![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
209 Cards in this Set
- Front
- Back
|
What are the five general functions of blood? |
1. Transporting dissolved gases, nutrients, hormones and metabolic wastes 2. Regulating the pH and ion concentration in interstitial fluid 3. Restricting fluid loss at injury sites through clotting. 4. Defending against toxins in pathogens via white blood cells and antibodies 5. Stabilizing body temperature |
|
|
What is the volume of blood in an adult male in an adult female respectively |
5-6 L in a male, 4-5L in a female |
|
|
What is the hematocrit |
The percentage of formed elements in a sample of blood |
|
|
What is a normal hematocrit, or packed cell volume, (PCV) |
Males 46% Females 42% This difference reflects the fact that androgens stimulate red blood cell production where as estrogens do not |
|
|
What are formed elements in blood? |
Blood cells and cell fragments suspended in plasma. There are three types, platelets, white blood cells, and red blood cells |
|
|
Which cells are responsible for the production of formed elements? |
Myeloid stem cells and lymphoid stem cell |
|
|
What are platelets |
Small membrane-bound cell fragments that contain enzymes and other substances important for clotting |
|
|
What are white blood cells and what are the five classes |
Also known as leukocytes, they play a role in the body's defense mechanisms. 1. Neutrophils 2. Eosinophils 3. Basophils 4. Lymphocytes 5. Monocytes |
|
|
What are the three types of plasma proteins |
1. Albumins – most abundant proteins, major contributors to osmotic pressure, transporting fatty acids, thyroid hormones and some steroid hormones. 2. Globulins – 35% of proteins. Include antibodies, or immunoglobulins, and transport globulins, which bind ions and hormones 3. Fibrinogen – functions and clotting. 4% of plasma proteins |
|
|
What is the pH of blood |
Between 7.35 and 7.45 |
|
|
What is a metalloprotein |
A globulin protein in plasma which transports metal ions |
|
|
What is an apolipoprotien |
A plasma globulin which carries triglycerides and other lipids in the blood. When bound to lipids it is known as a lipoprotein |
|
|
What is a steroid binding protein |
A plasma globulin which transports steroid hormones in the blood |
|
|
What is serum |
A plasma without clotting proteins (fibrinogen) |
|
|
Which organ synthesizes most of the plasma protient |
Liver |
|
|
What is a normal red blood cell count in males and females respectively |
Males 4.5–6.3 million/microliter Females 4.2–5.5 million/microliter |
|
|
What are three effects of the biconcave shape of red blood cells |
1. Increases surface area to volume ratio 2. Enables red blood cells to form stacks (roulex) that smooth the flow through narrow blood vessels 3. Increases flexibility of red blood cells |
|
|
Why is the lifespan of a red blood cell relatively short |
Red blood cells lack nuclei and most organelles including mitochondria |
|
|
What are the normal ranges of hemoglobin content of whole blood |
Males, 14 – 18 g/dL Females, 12 – 16 g/dL |
|
|
Describe the structure of hemoglobin |
Two alpha chains and two beta chains, Each with a single molecule of heme which holds an iron ion which interacts with an oxygen molecule |
|
|
What is oxyhemoglobin |
HbO2, hemoglobin with oxygen |
|
|
What is deoxyhemoglobin |
Hemoglobin molecules who's iron is not bound to oxygen |
|
|
How does oxygen-carbon dioxide exchange occur |
When oxygen levels are low as in the capillaries, hemoglobin releases oxygen and Under these conditions carbon dioxide levels are elevated and the alpha and beta chains of hemoglobin bind carbon dioxide forming carbaminohemoglobin |
|
|
What is hemoglobinuria |
The presence of alpha and beta chains from hemoglobin in urine which gives it a red or brown color. This is caused by an abnormally large number of hemolyzed RBCs |
|
|
What is hematuria, and what does it indicate |
The presence of intact RBCs in urine. Indicates kidney damage or damage to a vessel along the urinary tract |
|
|
What happens when a phagocytic cell engulfs a broken down rbc |
The globular proteins are broken apart into amino acids which are either metabolized by the cell or are released into the bloodstream. Each heme unit is converted to Biliverdin, A green colored compound which gives bad bruise its greenish tint, then to Bilirubin which is excreted in the bile |
|
|
What is jaundice |
The inability of the liver to excrete Bilirubin which results in diffusion into peripheral tissues giving them a yellow color |
|
|
How is iron carried in the blood and why is this transport mechanism necessary |
Large quantities of free iron are toxic to the cell so Iron is transported on the protein transferrin. |
|
|
Where does erythropoiesis take place |
In adults it takes place in the red bone marrow, or myeloid tissue. From the 2nd to 5th months of development The liver and spleen are the primary site |
|
|
What is pernicious anemia |
Anemia caused by deficiency of vitamin B 12, which is necessary for stem cell division |
|
|
Erythropoietin |
A glycoprotein formed by the kidneys and liver when exposed to low oxygen which stimulates erythropoiesis. |
|
|
What are the two effects of EPO |
Increases Cell division rates in erythroblasts and speeds up the maturation of RBCs by accelerating hemoglobin synthesis. |
|
|
What is mean corpuscular volume |
MCV, average volume of one red blood cell. Normal is 82–101µm³. Elevated levels are macrocytic, depressed levels are microcytic. |
|
|
Mean corpuscular hemoglobin concentration |
(MCHC) average weight of hemoglobin in one red blood cell.
Normal is 27–34 µg per red blood cell (Normochromic) Elevated levels are turned hyperchromic, depressed levels are hypochromic |
|
|
Antigens |
Substances that can trigger a protective defense mechanism called in the immune response |
|
|
How is blood type determined |
By the presence or absence of surface antigens in rbc plasma membrane |
|
|
What constitutes type a blood type |
Surface antigen A only |
|
|
What constitutes a type B blood type? |
Surface antigen B only |
|
|
What constitutes type AB blood |
Red blood cells with both A and B antigens |
|
|
What constitutes type O blood type |
Red blood cells have neither A nor B surface antigens |
|
|
What is RH |
A surface antigen on red blood cells. Blood is either RH positive or Rh negative. |
|
|
Agglutinogens |
A collective term for surface antigens on RBCs |
|
|
If a person had a type a B blood what anti-bodies would we expect to see |
Anti-A antibodies |
|
|
What happens if a inappropriate blood type is used in a blood transfusion |
The cross-reaction. Antibodies will interact with surface antigens and cause red blood cells to clump or break up. These can cause obstruction in small vessels of the kidneys, lungs, heart and brain. |
|
|
What is the most common blood type |
O positive |
|
|
What are the four characteristics of circulating white blood cells |
1. All can migrate out of the bloodstream. Once activated adhere to walls in a process called margination. There they squeeze between endothelial cells and enter the surrounding tissue in a process called emigration 2. All are capable of amoeboid movement. 3. All are attracted to specific chemical stimuli. (Positive chemotaxis) 4. Neutrophils, eosinophils and monocytes are capable of phagocytosis
|
|
|
What is hemolytic disease of the newborn |
A red blood cell related disorder caused by cross reaction between fetal and maternal blood types. |
|
|
Neutrophils |
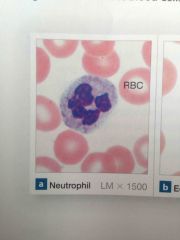
Also called PMNs. Highly mobile nonspecific white blood cells. Cytoplasm packed with granules containing lysosomal enzymes and bactericidal compounds. Neutrophils also release prostaglandins and leukotrienes which increase Capillary permeability and inflammation. |
|
|
Eosinophils |
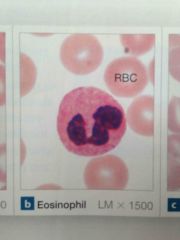
Generally stain red and have a bilobed nucleus.
Primary mode of attack is exocytosis of toxic compounds such as nitric oxide and cytotoxic enzymes.
Especially effective against parasitic infection.
Also sensitive to allergens and sites injury where they release enzymes that reduce inflammation produced by mast cells and neutrophils |
|
|
Basophils |
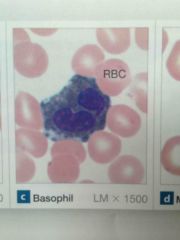
Discharge granules which contain histamine, which dilates blood vessels, and heparin, a compound that prevents blood clotting |
|
|
Monocytes |

Kidney shaped nucleus. Monocytes enter peripheral tissues and become macrophages |
|
|
Lymphocytes |
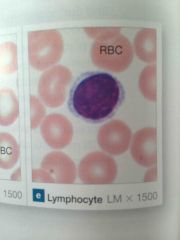
Have three functional classes 1. T cells – cell mediated immunity 2. B cells – humoral immunity (activated B cells differentiate into plasma cells) 3. Natural killer cells- perform immune surveillance, detection and subsequent destruction of abnormal cells. |
|
|
What is cell mediated immunity |
The defense mechanism against invading foreign cells |
|
|
What is humoral immunity |
A specific defense mechanism that involves the production of antibodies. These antibodies are distributed by blood, limph and interstitial fluid and are capable of attacking foreign antigens throughout the body |
|
|
What is leukopenia |
Inadequate numbers of WBCs |
|
|
What is leukocytosis |
Excessive WBCs. Modest leukocytosis is normal during infection but extreme leukocytosis generally indicates the presence of some form of leukemia |
|
|
What types of white blood cells are classified as granulocytes |
Neutrophils, basophils, and eosinophils. |
|
|
What are the functions of platelets |
1. Release enzymes and factors at appropriate times to initiate and control process 2. Forming a temporary patch in the walls of damage vessels 3. Platelets contain filaments of actin and myosin which contract to shrink the clot and the size of the break in the vessel wall |
|
|
How do platelets form |
Megakaryocytes manufacture structural proteins enzymes and membranes. They begin shedding cytoplasm and small membrane enclosed packets within the red bone marrow |
|
|
What three substances influence the rate of platelet formation |
1. Thrombopoeitin - A peptide hormone produced in the kidneys that accelerates platelet formation and stimulates production of megakaryocytes 2. Interleukin 6 - a hormone that stimulates platelet formation 3. Multi CSS – stimulates platelet production promoting formation growth of megakaryocytes. |
|
|
Hemostasis |
Stopping of bleeding |
|
|
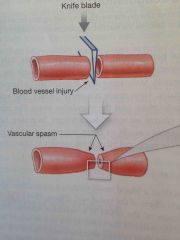
What are the three phases of hemostasis? |
Vascular phase, the platelet phase, the coagulation phase, |
|
|
What is a vascular spasm |
Local contraction of smooth muscle fibers of the vessel wall caused by cutting the wall of the blood vessel |
|
|
Describe the vascular phase |
Endothelial cells contract and release endothelins, which stimulates smooth muscle contraction and endothelial division. Endothelial cells become sticky and Adhere to platelets and each other |
|
|
Describe the platelet phase |
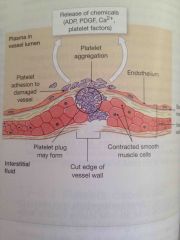
Platelets adhere to endothelial surfaces and form a platelet plug. They release ADP, which stimulates platelet aggregation, thromboxane A2 and serotonin, which stimulate vascular spasm, clotting factors, platelet derived growth factor and calcium ions |
|
|
How is growth of the platelet plug regulated? |
Prostacyclin, a prostaglandin that inhibits platelet aggregation is released by endothelial cells.
WBCs entering the area release inhibitory compounds.
|
|
|
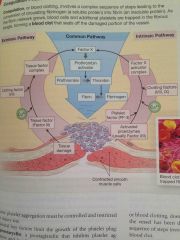
Describe the coagulation phase of hemostasis |
Complex sequence leading to the conversion of circulating fibrinogen into fibrin which traps blood cells and additional platelets to form a blood clot |
|
|
What are pro enzymes |
Proenzymes are inactive enzymes which can be converted to active enzyme |
|
|
Describe the extrinsic pathway of the coagulation phase of hemostasis |
The extrinsic ipathway begins outside the bloodstream in the vessel wall
Damaged endothelial cells release factor 3, also known as tissue factor.
Tissue factor then combines with calcium ions and clotting factor 9 to form an enzyme complex capable of activating factor X |
|
|
Describe the intrinsic pathway of the coagulation phase of hemostasis |
Intrinsic pathway begins in the bloodstream.
Activation of factor 12 in conjunction with PF-3 leads to activation of factors 8 and 9 which form an enzyme complex capable of activating factor 10 |
|
|
Describe the common pathway of the coagulation phase of hemostasis |
Factor X, Activate's Prothrombin activator, which converts prothrombin into thrombin which completes the clotting process by converting fibrinogen into fibrin |
|
|
What kind of feedback loop is blood clotting |
Positive feedback loop |
|
|
How would low calcium ion levels or vitamin K levels affect clotting |
A calcium deficiency would impair blood clotting as all three pathways require calcium to proceed.
Vitamin K deficiency would prevent the liver from synthesizing four of the clotting factors including prothrombin |
|
|
Fibrinolysis |
The process of dissolving a clot.
Thrombin and tissue plasminogen activator Activate the proenzyme plasminogen, which turns it into plasmin.
Plasmin digests the fibrin strands and erodes the clot |
|
|
Right atrium |
Receives blood from the systemic circuit and passes it to the right ventricle |
|
|
Right ventricle |
Receives blood from the right atrium and pumps blood into the pulmonary circuit |
|
|
Left atrium |
Receives blood from the pulmonary circuit and pumps Blood into the left ventricle |
|
|
Left ventricle |
Receives blood from the left atrium and pumps blood into the systemic circuit |
|
|
Pericarditis |
Inflammation of percardial services. The two surfaces can be heard rubbing against each other with the stethoscope |
|
|
Cardiac tamponade |
Increased fluid in the pericardial cavity which restricts movement of the heart |
|
|
What are the three layers of the heart? |
1. Epicardium 2. Myocardium 3. Endocardium |
|
|
Epicardium |
The visceral pericardium covering the outer surface of the heart. Consists of exposed mesothelium and underlying loose areolar connective tissue |
|
|
Myocardium |
Muscular wall of the heart. Concentric layers of cardiac muscle tissue |
|
|
Endocardium |
The simple squamous epithelium which covers the inner surfaces of the heart and heart valves. |
|
|
Describe the structure of an intercalated discs |
Interlocking membranes are held together by desmosomes and linked by gap junctions |
|
|
What are four histological characteristics that distinguish cardiac muscle cells from skeletal muscle cells |
1. Small size 2. A single central nucleus 3. Branching interconnections between cells 4. The presence of intercalated discs. |
|
|
What 3 veins open into the right atrium and which parts of the body do they service |
1. Superior vena cava – delivers blood from the head, neck, upper limbs and chest 2. Inferior vena cava – delivers blood from the trunk, viscera, and lower limbs. 3. Coronary sinus – delivers blood from the cardiac means draining the myocardium |
|
|
Foramen ovale |
A structure present in embryonic development that penetrates the interatrial septum and connects the two atria of the fetal heart. This permits blood flow between the atria while the lungs are developing. * usually sealed off within three months of delivery leaving the fossa ovalis. |
|
|
Where would you find pectinate muscles |
The anterior atrial wall and inner surface of the auricle |
|
|
How does blood travel from the right atrium to the right ventricle |
Via the right atrioventricular valve, also known as the tricuspid valve. The free edges of each cusp are anchored by Chordae tendineae which originate at papillary muscles. This prevents backflow during ventricular contraction |
|
|
What happens to blood during contraction of the right ventricle? |
What is forced through the conus arteriosus, a cone shaped pouch at the superior end of the right ventricle, which ends at the pulmonary valve. It then enters the pulmonary trunk which is the start of the pulmonary circuit. |
|
|
Where does the left atrium receives blood from? |
Via the left and right pulmonary veins |
|
|
Through what structures does blood pass in route from the left atrium to the left ventricle |
The bicuspid (or mitral) valve |
|
|
Blood leaves the left ventricle through which valve |
The aortic semilunar valve |
|
|
What is the function of the atrioventricular valves |
Prevents the backflow of blood from the ventricles to the atria when the ventricles are contracting. |
|
|
What is the function of the semilunar valves |
Prevent the backflow of blood from the pulmonary trunk and the aorta |
|
|
What are aortic sinuses |
Saclike expansions at the base of the ascending aorta that prevent individual cusps of the aortic valve from sticking to the wall of the aorta |
|
|
Where do the right and left coronary arteries originate |
At the left and right aortic sinuses. |
|
|
What is rheumatic fever? |
And inflammatory autoimmune response to infection by streptococcal bacteria that can lead to carditis which in turn can lead to valvular heart disease |
|
|
What is the cardiac skeleton |
Four bands of tough elastic tissue that encircle the heart valves and the bases of the pulmonary trunk aorta. The bands stabilize the positions of the valves and ventricular muscle cells |
|
|
Where is the right coronary artery and what does it service |
Follows the coronary sulcus around the heart. Services the right atrium, portions of both ventricles, portions of the conducting system of the heart, including the SA node in the AV node
Supplies the posterior interventricular artery |
|
|
Where is the posterior interventricular artery and what does it service |
Travels toward the apex of the heart within the posterior interventricular sulcus.
Services the interventricular septum and adjacent portions of the ventricles. |
|
|
What does the left coronary artery service |
Left ventricle, left atrium, and interventricular septum |
|
|
Describe the SA node |
The SA node is embedded in the posterior wall of the right atrium. Contains pacemaker cells which establish the heart rate. Generally depolarizes at a rate of 80–100/min |
|
|
Describe impulse conduction through the heart |
1. SA node depolarizes 2. Stimulus spreads across atrial surfaces and reaches AV node 3. Atria contract 4. Action potential travels along the intraventricular septum to Purkinje fibers and the moderator band. 5. Impulse is distributed by Purkinje fibers and ventricular contraction begins |
|
|
What is an ectopic pacemaker |
If a abnormal conducting cell or ventricular muscle cell begins generating action potentials at a higher rate and overrides the SA or AV nodes |
|
|
Describe the components of an EKG |
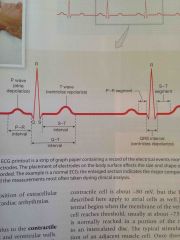
P- wave, Depolarization of the atria QRS complex – ventricular depolarization. Ventricles begin contracting shortly after the peak of the R wave. T-wave – ventricular repolarization |
|
|
What is the PR interval on an EKG |
Time measurement from the start of atrial depolarization to Q, the start of the QRS complex. Extension of the PR interval to more than 200 ms can indicate damage to the conducting pathways or AV node |
|
|
What is the Q – T interval in an EKG |
Time for ventricles to Depolarize and repolarize.
Measured from the end of the P – R interval to the end of the T-wave. Longer than normal indicates electrolyte disturbances, conduction problems, coronary ischemia, or myocardial damage |
|
|
Describe the action potential in cardiac muscle cells |
1. At threshold, voltage gated fast sodium channels open and the sarcolemma is rapidly depolarized. 2. Fast sodium channels close as slow voltage gated calcium channels are opening. This maintains the membrane potential near 0 mV for an extended period. 3. Repolarization – slow calcium channels clothes and slow potassium channels open which restores resting potential |
|
|
Systole |
Contraction phase of heart muscle |
|
|
Diastole |
Relaxation phase of heart muscle. Chamber fills with blood |
|
|
What is end – diastolic volume |
The amount of blood in each ventricle after atrial systole.
Usually 130 mL in a resting adult |
|
|
Isovolumetric contraction |
The early stage of ventricular contraction when the semi lunar valves remain closed |
|
|
What is stroke volume |
The amount of blood ejected from each ventricle during systole.
Roughly 60% of end diastolic volume, approximately 70 to 80 mL of blood |
|
|
Isovolumetric relaxation |
The ventricles are in diastole, but blood cannot flow into them as pressure in the ventricles remains higher then the atria |
|
|
What is the primary method of ventricular filling |
Low pressures in the ventricles during diastole allow blood to pour freely through the atria and into the ventricles |
|
|
What are the S1 and S2 heart sounds |
S1 - Occurs at the beginning of ventricular contraction when the atrioventricular valves close. S2- Occurs at the beginning of ventricular filling when the semilunar valves close |
|
|
What is a heart murmur |
A sound made when heart valves do not close properly and AV valve regurgitation occurs during ventricular systole |
|
|
What is cardiac output |
The amount of blood pumped by the left ventricle in one minute |
|
|
What two factors affect heart rate |
Autonomic innervation, and hormones |
|
|
What is the cardioaccelatory center and where is it found? |
Control sympathetic neurons that increase the heart rate and is found in the medulla oblongata |
|
|
What is the cardio inhibitory center and where is it found? |
Controls parasympathetic neurons that slow the heart rate and is found in the medulla oblongata. |
|
|
What is the atrial (Bainbridge) reflex? |
Also known as the Bainbridge reflex. When the walls of the right atrium are stretched, stretch receptors trigger a reflexive increase in heart rate by stimulating sympathetic activity |
|
|
What is the Frank-Starling principal |
Increasing the end diastolic volume results in a corresponding increase in the stroke volume |
|
|
What are three factors that influence end systolic volume |
Preload, contractibility of the ventricle, and after load |
|
|
What is contractibility? |
The amount of force produced during a contraction at a given preload. Factors that increase contractibility have a positive inotropic action. Factors that decrease contractibility have a negative inotropic action. |
|
|
Describe the Tunica media |
Smooth muscle and loose connective tissue which is mostly elastic fibers in arteries and collagen fibers in veins. The external elastic membrane is present in arteries and separates the Tunica media from the tunica externa |
|
|
Tunica externa |
The connective tissue sheath. In veins it contains some smooth muscle cells. |
|
|
What are vaso vasorum |
Small arteries and veins that supply the smooth muscle cells and fibroblasts of the Tunica media and tunica externa |
|
|
Elastic arteries |
Carry large volumes of blood away from the heart. High concentration of elastic fibers make these arteries extremely resilient to the pressure waves that accompany ventricular contraction |
|
|
Muscular arteries |
Thick Tunica media. Distribute blood to the body skeletal muscles and internal organs. Includes external carotid artery's, brachial arteries, and femoral arteries |
|
|
What are the two types of capillaries |
Continues Capillaries – The endothelium is a complete lining. Found in all tissue except cartilage and epithelium
Fenestrated capillaries - endothelium contains pores which allow rapid exchange of water and solutes between blood and interstitial fluid. Fenestrated capillaries are found the choroid plexus of the brain and in a variety of endocrine organs and along the digestive tract. |
|
|
What is afterload? |
Amount of tension that the contracting ventricle must produce to open the semilunar valve and eject blood.
As afterload increases stroke volume decreases |
|
|
Coronary artery disease |
Partial or complete blockage of coronary circulation generally caused by the build up of artherosclerotic plaque or a thrombus |
|
|
What diagnostic tests would be used to diagnose a myocardial infarction |
Elevated cardiac troponin T, elevated cardiac troponin I, and a special form of creatine phosphokinase CK – MB |
|
|
Cardiomyoplasty |
Surgical procedure that uses stimulated latissimus dorsi muscle to assist with cardiac function. |
|
|
Commotio cordis |
Sudden cardiac arrest as a result of a blunt hit or impact to the chest |
|
|
Congestive heart failure |
Condition of weakness, edema, and shortness of breath caused by the inability of the heart to maintain adequate circulation in the peripheral tissues and the lungs |
|
|
Cor pulmonale |
Weakness of the right ventricle due to prolonged hypertension in the pulmonary artery. |
|
|
What are the three layers of the walls of the arteries and veins |
The Tunica intima, Tunica media, and tunica externa |
|
|
Describe the Tunica intima |
The inner layer. Includes an endothelial lining which appears rippled in arteries and smooth in veins. The internal elastic membrane is present in arteries. |
|
|
Collaterals and arterial anastomosis |
Collaterals are when multiple arteries supply a capillary bed. they fuse before giving rise to arterioles which is called arterial anastomosis |
|
|
What is an arteriovenus anastomoses and what happens when it is dilated |
Direct connections between arterioles and venules that when dilated allow blood to bypass the capillary beds.
generally occurs during sympathetic activation |
|
|
What triggers angiogenesis |
Vascular endothelial growth factor |
|
|
What is vasomotion |
Rhythmic contraction and relaxation of precapillary sphincter's which occurs perhaps 12 times per minute. |
|
|
Describe venous valves |
Folds of the Tunica intima that project from the vessel wall and point in the direction of blood flow.
Blood is then squeezed toward the heart by skeletal muscles. |
|
|
What is capacitance |
The ability of a blood vessel to expand at higher pressures. Veins have a higher capacitance than arteries, and can accommodate large changes in blood volume or pressure |
|
|
What happens during hemorrhaging |
Vasomotor center of the medulla oblongata stimulate sympathetic nerves which innervate smooth muscles in medium sized veins. 1. Venoconstriction decreases the blood volume within the venous system. 2. Constriction of veins in the liver, skin and lungs redistributes a significant proportion of the total blood volume. |
|
|
What is venous reserve? |
Amount of blood that can be shifted from veins in the liver, skin, and lungs to the general circulation. |
|
|
How is the mean arterial pressure calculated |
MAP = diastolic pressure + pulse pressure/3
*pulse pressure is the difference between systolic and diastolic pressure |
|
|
Distinguish between stage one hypertension and pre-hypertension |
Stage one hypertension is systolic blood pressure's from 140-159 or diastolic pressures 90–99
Prehypertension - systolic blood pressure is 120 - 139, diastolic pressures 80-89 |
|
|
What two factors contribute to venous return to the heart? |
Muscular compression, and the respiratory pump |
|
|
What are the four functions of water movement from the capillaries to the lymphatic system |
1. Keeps plasma and interstitial fluid in constant contact 2. Accelerates distribution of nutrients, hormones, and gases 3. Assist in transport of insoluble lipids and tissue proteins that cannot enter the bloodstream via capillary walls 4. Carries toxins to lymphatic tissues |
|
|
What three factors affect tissue perfusion |
1. Cardiac output 2. Peripheral resistance 3. Blood pressure |
|
|
What are vasodilators. |
Factors that promote the dilation of precapillary sphincters |
|
|
Describe the process of autoregulation in regards the cardiovascular system |
Autoregulation involves changes in the pattern of blood flow within capillary beds as precapillary sphincters open and close in response to chemical changes in the interstitial fluid. |
|
|
Describe the process of autoregulation in regards the cardiovascular system |
Autoregulation involves changes in the pattern of blood flow within capillary beds as precapillary sphincters open and close in response to chemical changes in the interstitial fluid. |
|
|
Describe central regulation in regards to the cardiovascular system |
Central regulation involves both neural and endocrine mechanisms. Cardioacceleratory center, and vasomotor center stimulate the heart and constrict vessels. Endocrine response produces long term increases in blood volume and blood pressure |
|
|
Control vasoconstriction by the vasomotor center |
Neurons and everything peripheral blood vessels are adrenergic, they release norepinephrine, which stimulates smooth muscles causing constriction. |
|
|
Control vasoconstriction by the vasomotor center |
Neurons and everything peripheral blood vessels are adrenergic, they release norepinephrine, which stimulates smooth muscles causing constriction. |
|
|
Describe the control of vasodilation by neurons of the vasomotor center |
Cholinergic neurons release ACH, which stimulates endothelial cells to release NO causing relaxation of the vascular smooth muscle cells. |
|
|
Diagram the baroreceptor reflexes of the carotid and aortic sinuses |

|
|
|
Chemoreceptor reflex |

|
|
|
Diagram hormonal regulation which compensates for decreasing blood pressure or volume. |
Back (Definition) |
|
|
Diagram hormonal regulation of factors which compensate for increasing blood pressure or volume. |

Back (Definition) |
|
|
What are the carotid sinus |
Expanded Chambers near the basis of the internal carotid artery's |
|
|
What are the aortic sinuses |
Pockets in the walls of the ascending aorta adjacent to the heart. |
|
|
What are baroreceptors and where are they found in the cardiovascular system? |
Specialized receptors that monitor the degree of stretch in the walls of expandable organs. Found in the carotid sinuses, aortic sinuses, and the wall of the right atrium. |
|
|
What are baroreceptors and where are they found in the cardiovascular system? |
Specialized receptors that monitor the degree of stretch in the walls of expandable organs. Found in the carotid sinuses, aortic sinuses, and the wall of the right atrium. |
|
|
What happens to baroreceptors when blood pressure rises? |
Cardiac output decreases due to Parasympathetic stimulation in the inhibition of sympathetic activity. Peripheral vasodilation due to inhibition of excitatory neurons in the vasomotor center |
|
|
What are baroreceptors and where are they found in the cardiovascular system? |
Specialized receptors that monitor the degree of stretch in the walls of expandable organs. Found in the carotid sinuses, aortic sinuses, and the wall of the right atrium. |
|
|
What happens to baroreceptors when blood pressure rises? |
Cardiac output decreases due to Parasympathetic stimulation in the inhibition of sympathetic activity. Peripheral vasodilation due to inhibition of excitatory neurons in the vasomotor center |
|
|
What effects are triggered by baroreceptors when blood pressure falls below normal |
Decreased baroreceptor activity, increases cardiac output through stimulation of sympathetic innervation in the cardioaccelatory center, as well as peripheral vasoconstriction caused by sympathetic vasoconstrictor neurons |
|
|
How can the Valsalva maneuver be used to check for normal cardiovascular responses to changes in arterial pressure and venous return |
The Valsalva maneuver causes increased inter-thoracic pressure which impedes venous return to the right atrium. The resulting drop in cardiac output and blood pressure stimulates the aortic and carotid baroreceptors causing a reflexive increase in heart rate and peripheral vasoconstriction.
When the maneuver ends blood pressure increases suddenly as does cardiac output, Which results in stretching of the baroreceptors. |
|
|
Where are chemo receptors located? |
In the carotid bodies, situated near the carotid sinus, and the aortic bodies, near the arch of the aorta. |
|
|
What four hormones are involved with long term regulation of blood volume |
1. Antidiuretic hormone 2. Angiotensin II 3. Erythropoietin 4. Natriuretic peptides |
|
|
What does antidiuretic hormone have on the cardiovascular system |
Stimulates water conservation by the kidneys, brings about vasoconstriction which elevates blood pressure. ADH release is stimulated by decrease in blood volume, increase in osmotic concentration of plasma, or by circulating angiotension 2 |
|
|
What effect does angiotensin II have on the cardiovascular system? |
1. Stimulates adrenal production of aldosterone, causing sodium retention and potassium loss in the kidneys. 2. Stimulate secretion of ADH 3. Stimulates thirst 4. Increases cardiac output and triggers constriction of arterials raising blood pressure. |
|
|
What effect does angiotensin II have on the cardiovascular system? |
1. Stimulates adrenal production of aldosterone, causing sodium retention and potassium loss in the kidneys. 2. Stimulate secretion of ADH 3. Stimulates thirst 4. Increases cardiac output and triggers constriction of arterials raising blood pressure. |
|
|
How is angiotensin II produced? |
Angiotensin II is produced when juxtaglomerular cells release renin in response to fall in renal blood pressure. Renin converts angiotensinogen to angiotensin 1. Angiotensin one is converted by angiotension – converting enzyme in the lungs to angiotension two. |
|
|
What are the effects of EPO on the cardiovascular system |
EPO causes vasoconstriction as well as stimulates production and maturation of red blood cells. |
|
|
What effect do natriuretic peptides have on the cardiovascular system? |
They reduce blood pressure and blood volume by. 1. Increasing sodium ion excretion 2. Increasing volume of urine produced 3. Reduce thirst 4. Block release of ADH, aldosterone, epinephrine, and norepinephrine. 5. Stimulate peripheral vasodilation |
|
|
Where are natriuretic peptide's produced and what triggers production? |
Atrial natriuretic peptide is produced in response to excessive stretching of the right atrium during diastole.
Brain Natriuretic peptide is produced when ventricular muscle cells are stretched during diastole |
|
|
How does exercise affect cholesterol levels? |
Exercise stimulates enzymes that move LDLs from the blood to the liver where they are converted to bile and excreted from the body. Exercise also increases the size of lipoprotein particles that carry cholesterol, making it harder for small proteins to lodge in vessel walls creating arthrosclerosis |
|
|
Diagram the cardiovascular responses to blood loss |

Back (Definition) |
|
|
What happens when compensatory mechanisms for blood loss fail? |
Shock |
|
|
Describe the short-term cardiovascular response to hemorrhaging |
As blood pressure begins to drop the carotid in the order reflexes increase cardiac output and cause peripheral vasoconstriction. Activation of the sympathetic nervous system triggers increase in vasomotor town as well as venoconstriction which mobilizes the venous reserve. Sympathetic activation also leads to the release of epinephrine and norepinephrine which increase cardiac output and extend vasoconstriction |
|
|
How does the body respond in the long term to blood loss |
Decrease in capillary blood pressure triggers recall of fluids from interstitial spaces. Aldosterone and ADH promote fluid retention and reabsorption by the kidneys. Thirst increases. EPO stimulates maturation and production of red blood cells |
|
|
How are blood and nutrients transported into a developing fetus |
Via a single umbilical vein which carries blood from the placenta into the ductus venous of the liver where it joins fetal circulation in the inferior vena cava |
|
|
How are blood and nutrients transported into a developing fetus |
Via a single umbilical vein which carries blood from the placenta into the ductus venous of the liver where it joins fetal circulation in the inferior vena cava |
|
|
What is the ductus arteriosus |
A small muscular vessel which connects the pulmonary and aortic trunks during development. |
|
|
Intermittent claudication |
A limp which results from cramping leg pain that is typically caused by obstruction of the arteries |
|
|
Raynaud's phenomenon |
Discoloration of the fingers or toes when a person is subject to changes in temperature or to emotional stress. |
|
|
Which kinds of white blood cells contribute to the bodies nonspecific defenses |
Eosinophils, basophils, neutrophils and monocytes |
|
|
Name the 3 types of lymphocytes and identify their functions. |
1. T cells - cell mediated immunity 2. B cells - humoral immunity 3. NK cells - immune surveillance |
|
|
Which of the following is longer, the refractory period of Skeletal muscles or the refractory period of cardiac muscle |
The refractory period of cardiac muscle |
|
|
Cardiac arrhythmias - premature atrial contractions, PACs. |
Normal atrial rhythm is momentarily interrupted by atrial contraction. Often occur in healthy hearts. Stress, caffeine, and various drugs may increase the incidence of PACs. Normal ventricular contraction follows |
|
|
Cardiac arrhythmias – paroxysmal atrial tachycardia |
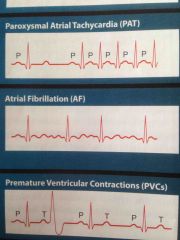
A premature atrial contraction triggers a flurry of atrial activity. Ventricles are still able to keep pace heart rate jumps to approximately 180 bpm |
|
|
Cardiac arrhythmias – paroxysmal atrial tachycardia |
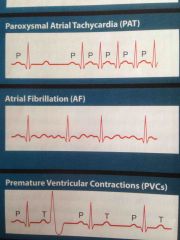
A premature atrial contraction triggers a flurry of atrial activity. Ventricles are still able to keep pace heart rate jumps to approximately 180 bpm |
|
|
Cardiac arrhythmias – atrial fibrillation |
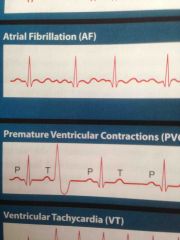
Atrial impulses are too fast for the ventricles to keep up, atrial's quiver rather than producing organized contraction and are nonfunctional. Because atrial contraction contribute so little to end diastolic volume The condition sometimes goes unnoticed, particularly in older individuals |
|
|
Cardiac arrhythmias – premature ventricular contractions |
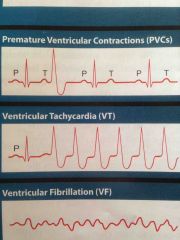
Occur when a purkinjebcell or ventricular myocardial cell depolarizes to threshold and triggers a premature contractions. Single PVCs are common and not dangerous, the responsible cell is in an ectopic pacemaker. |
|
|
Cardiac arrhythmias – ventricular tachycardia |
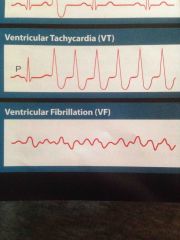
Four or more PVCs without intervening normal beats. May indicate a serious cardiac problem |
|
|
Cardiac arrhythmias – ventricular fibrillation |
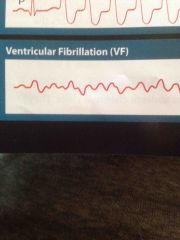
Ventricles quiver and stop pumping blood. Responsible for cardiac arrest |
|
|
What are the results of alpha receptor stimulation |
Systemic arteriolar constriction Epi and norepi stimulate |
|
|
What are the results of B1 receptor activation |
increased heart rate and force of contraction Epinephrine stimulates |
|
|
What are the results of B2 stimulation |
Dialation of some vascular beds such as skeletal muscle and bronchodialation |
|
|
How is the Renin-Angiotensin System activated and what is the process |
Macula Densa cells in the juxtaglomerular apparatus produce renin which combines with angiotensinogen produced in the liver to form angiotensin 1. Angiotensin 1 is converted to angiotensin 2 which is a powerful vasoconstrictor. It also triggers aldosterone secretion which in turn leads Sodium --> water retention. End result. Increased blood pressure. |
|
|
What is the Ejection Fraction and why is it important |
The percentage of the end diastolic volume pumped by the heart during each contraction. Indicates the hearts efficiency as a pump |

