![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
234 Cards in this Set
- Front
- Back
|
What word describes the phenomenon of a single gene having more than one effect on an individual's phenotype?
|
Pleiotropy
|
|
|
A patient has inherited a mutation in a tumor suppressor gene. Mutation of the remaining (previously normal) copy of the tumor suppressor gene represents a loss of _____, which may lead to the development of cancer.
|
Heterozygosity; the patient was previously a heterozygote for the lost tumor suppressor gene
|
|
|
A genetic disease that shows _____ _____ will have mutations at different loci that produce the same phenotype.
|
Locus heterogeneity
|
|
|
What term describes the presence of both normal and mutated mitochondrial DNA (mtDNA), resulting in variable expression in mitochondrial inherited diseases?
|
Heteroplasmy
|
|
|
Name the genetic phenomenon that occurs when the offspring receives 2 copies of a chromosome from 1 parent and no copies from the other parent.
|
Uniparental disomy
|
|
|
In Leber's hereditary optic neuropathy, vision loss is _____ (central/peripheral).
|
Central (like macular degeneration)
|
|
|
What is the pattern of inheritance of hypophosphatemic rickets?
|
X-linked dominant
|
|
|
Autosomal-recessive patterns of inheritance are often found in diseases caused by defects in _____.
|
Enzymes
|
|
|
Autosomal-dominant patterns of inheritance are often found in diseases caused by defects in _____ genes.
|
Structural
|
|
|
Fatty acid oxidation occurs in the _____ (mitochondria/cytoplasm), whereas fatty acid synthesis occurs in the _____ (mitochondria/cytoplasm).
|
Mitochondria; cytoplasm
|
|
|
Name the three pathways that occur in both the cytoplasm and the mitochondria.
|
Heme synthesis, the Urea cycle, and Gluconeogenesis; remember the mnemonic: HUGs take two
|
|
|
Four pathways that occur in the mitochondria
|
Fatty acid oxidation, acetyl-CoA production, Krebs cycle, and oxidative phosphorylation
|
|
|
What is the rate-determining enzyme of de novo pyrimidine synthesis?
|
Carbomyl phosphate synthetase II
|
|
|
What is the rate-determining enzyme of de novo purine synthesis?
|
Glutamine-PRPP amidotransferase
|
|
|
What is the rate-determining enzyme of glycolysis?
|
PFK-1
|
|
|
What is the rate-determining enzyme of gluconeogenesis?
|
Fructose-1,6-bisphosphatase (F-1,6-BP)
|
|
|
What is the rate-determining enzyme of the TCA cycle?
|
Isocitrate dehydrogenase
|
|
|
What is the rate-determining enzyme of glycogen synthesis?
|
Glycogen synthase
|
|
|
What is the rate-determining enzyme of glycogenolysis?
|
Glycogen phosphorylase
|
|
|
What is the rate-determining enzyme of the HMP shunt?
|
G6PD
|
|
|
What is the rate-determining enzyme of fatty acid synthesis?
|
Acetyl-CoA carboxylase
|
|
|
What is the rate-determining enzyme of fatty acid oxidation?
|
Carnitine acetyltransferase I
|
|
|
What is the rate-determining enzyme of ketogenesis?
|
HMG-CoA synthase
|
|
|
What is the rate-determining enzyme of cholesterol synthesis?
|
HMG-CoA reductase
|
|
|
What is the rate-determining enzyme of the urea cycle?
|
Carbamoyl phosphate synthetase
|
|
|
How many ATP molecules are produced from the aerobic metabolism of glucose via the malate-aspartate shuttle?
|
32; occurs in the heart and liver
|
|
|
How many ATP molecules are produced from the aerobic metabolism of glucose via the glyceraldehyde-3-phosphate shuttle?
|
30; this occurs in the muscle
|
|
|
What compounds are used as single-carbon donors in various reactions?
|
Tetrahydrofolates (THFs)
|
|
|
What vitamin is the donor of the carboxyl group used in many biochemical reactions in the body?
|
Biotin
|
|
|
What molecule donates methyl groups?
|
S-adenosylmethionine (SAM)
|
|
|
What enzyme deficiency is seen in Fabry's disease?
|
α-Galactosidase A
|
|
|
A patient presents with progressive neurodegeneration, hepatosplenomegaly, and a cherry-red spot on his macula. Histologic examination reveals cells containing lipid droplets, confirming a lysosomal storage disease. What are these cells called?
|
Foam cells; seen in Niemann-Pick disease
|
|
|
A patient presents with peripheral neuropathy, developmental delay, and optic atrophy. Histologic examination reveals multinucleated macrophages, confirming your diagnosis of a lysosomal storage disease. What are these cells called?
|
Globoid cells; seen in Krabbe's disease
|
|
|
A deficiency of the enzyme α-galactosidase A leads to what disease?
|
Fabry's disease
|
|
|
What substrate is accumulated in Fabry's disease?
|
Ceramide trihexose
|
|
|
A patient shows mild symptoms similar to Hurler's syndrome, but no corneal clouding; what kind of behavior patterns do you expect?
|
Aggressive behavior; seen in Hunter's syndrome
|
|
|
What type of inheritance does Fabry's disease demonstrate?
|
X-linked recessive
|
|
|
A patient has peripheral neuropathy of the hands and feet, angiokeratomas of the skin, and both cardiovascular and renal disease. These characteristics are typical of which lysosomal storage disease?
|
Fabry's disease
|
|
|
Name six types of sphingolipidosis.
|
Fabry's disease, Gaucher's disease, Niemann-Pick disease, Tay-Sachs disease, Krabbe's disease, metachromatic leukodystrophy
|
|
|
What enzyme deficiency leads to Gaucher's disease?
|
β-Glucocerebrosidase
|
|
|
What is the most common lysosomal storage disease?
|
Gaucher's disease
|
|
|
What three lysosomal storage disorders are Ashkenazi Jews at increased risk for?
|
Tay-Sachs, Niemann-Pick, and some forms of Gaucher's disease
|
|
|
A patient has hepatosplenomegaly, aseptic necrosis of the femur, bone crises, and abnormal macrophages on histologic examination. These characteristics are typical of which lysosomal storage disease?
|
Gaucher's disease
|
|
|
What enzyme deficiency leads to Niemann-Pick disease?
|
Sphingomyelinase
|
|
|
A child has progressive neurodegeneration, hepatosplenomegaly, and a cherry-red spot on his macula. These characteristics are typical of which lysosomal storage disease?
|
Niemann-Pick disease
|
|
|
What substrate is accumulated in Tay-Sachs disease?
|
GM2 ganglioside
|
|
|
A child has progressive neurodegeneration, developmental delay, cherry-red spots on the macula, and lysosomes with onion skin. These characteristics are typical of which lysosomal storage disease?
|
Tay-Sachs disease
|
|
|
Name two lysosomal storage diseases that may present with a cherry-red spot on the macula.
|
Niemann-Pick disease and Tay-Sachs disease
|
|
|
What enzyme deficiency leads to Krabbe's disease?
|
Galactocerebrosidase
|
|
|
A patient has peripheral neuropathy, developmental delay, and optic atrophy. These characteristics are typical of which lysosomal storage disease?
|
Krabbe's disease
|
|
|
What are the names of the cells that may serve as histologic confirmation of Niemann-Pick disease?
|
Foam cells
|
|
|
What are the names of the cells that may serve as histologic confirmation of Krabbe's disease?
|
Globoid cells
|
|
|
What enzyme deficiency leads to metachromatic leukodystrophy?
|
Arylsulfatase A
|
|
|
What substrate is accumulated in metachromatic leukodystrophy?
|
Cerebroside sulfate
|
|
|
A patient has central and peripheral demyelination with ataxia and dementia. These characteristics are typical of which lysosomal storage disease?
|
Metachromatic leukodystrophy
|
|
|
What enzyme deficiency leads to Hurler's syndrome?
|
α-L-iduronidase
|
|
|
A patient has developmental delay, gargoylism, airway obstruction, and corneal clouding. These characteristics are typical of which lysosomal storage disease?
|
Hurler's disease
|
|
|
What substances accumulate in mucolipodosis?
|
Heparan sulfate and dermatan sulfate
|
|
|
What enzyme deficiency leads to Hunter's syndrome?
|
Iduronate sulfatase
|
|
|
What pattern of inheritance does Hunter's syndrome demonstrate?
|
X-linked recessive
|
|
|
A patient has mild developmental delay, gargoylism, and airway obstruction but no corneal clouding. These characteristics are typical of which lysosomal storage disease?
|
Hunter's syndrome
|
|
|
Name the two lysosomal storage diseases that show x-linked recessive inheritance.
|
Fabry's disease and Hunter's syndrome
|
|
|
In which direction does the citrate shuttle move acetyl coenzyme A between the cytoplasm and the mitochondria?
|
From the mitochondria to the cytoplasm
|
|
|
What is the intracellular location of the citrate shuttle?
|
The inner mitochondrial membrane
|
|
|
In acyl-CoA dehydrogenase deficiency, dicarboxylic acid levels _____ (increase/decrease) and glucose and ketone levels _____ (increase/decrease).
|
Increase; decrease
|
|
|
What two blood vessels and one nerve run along the spine at the level of the umbilicus?
|
aorta, IVC, sympathetic trunk
|
|
|
True or False: The latissimus dorsi is more superficial than the quadratus lumborum.
|
true
|
|
|
True or False: The transversalis fascia runs superficially to the transversus abdominis muscle.
|
false
|
|
|
True or False: The rectus sheath wraps around the outside of the rectus abdominis.
|
true
|
|
|
What is the most superficial muscle group making up the lateral abdominal wall?
|
external oblique
|
|
|
What is the deepest muscle group making up the lateral abdominal wall?
|
transversus abdominis
|
|
|
What lies between the bilateral rectus abdominis muscles, formed by the rectus sheath?
|
linea alba
|
|
|
Name two major organs that lie completely in the retroperitoneal space.
|
kidneys and adrenal glands
|
|
|
What part of the pancreas is not found in the retroperitoneal space?
|
the tail
|
|
|
True or False: The rectum lies in the retroperitoneal space.
|
true
|
|
|
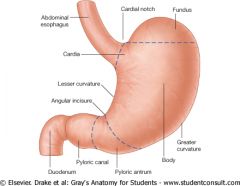
Keep the lesser and greater curvatures of the stomach straight!
|
|
|
|
Which two parts of the urinary system are retroperitoneal?
|
kidneys and ureters
|
|
|
Which parts of the colon are found in the retroperitoneal space?
|
ascending and descending colon
|
|
|
In the gastrointestinal tract, the falciform ligament connects which two structures?
|
liver and anterior abdominal wall
|
|
|
In the gastrointestinal tract, the gastrohepatic ligament connects which two structures?
|
liver and LESSER CURVATURE of the stomach
|
|
|
In the gastrointestinal tract, the gastrocolic ligament connects which two structures?
|
TRANSVERSE colon and GREATER CURVATURE of the stomach
|
|
|
In the gastrointestinal tract, the splenorenal ligament connects which two structures?
|
spleen to the POSTERIOR ABDOMINAL WALL (remember that the kidneys are retroperitoneal not within the abdominal cavity itself!)
|
|
|
The hepatoduodenal ligament contains what structures?
|
portal artery, portal vein and common bile duct (the hepatic TriaD, hepaToDuodental)
|
|
|
The gastrohepatic ligament contains what structures?
|
gastric arteries
|
|
|
The gastrocolic ligament contains what structures?
|
gastroepiploic arteries
|
|
|
The splenorenal ligament contains what structures?
|
splenic artery and vein
|
|
|
Name the ligament in the gastrointestional tract which is dervived from the fetal umbilical vein.
|
falciform ligament
|
|
|
The portal triad can be compressed through what opening to control bleeding?
|
omental foramen (also known as the epiploic foramen of Winslow)
|
|
|
What gastrointestinal ligament can be cut to access the lesser sac during surgery?
|
gastrohepatic ligament (it separates the RIGHT greater and lesser sacs)
|
|
|
The gastrosplenic ligament separates what two structures?
|
LEFT greater and lesser sacs
|
|
|
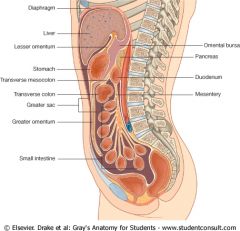
Don't forget where the greater and lesser sacs are! And, remember that the lesser sac may also called the omental bursa.
|
|
|
|
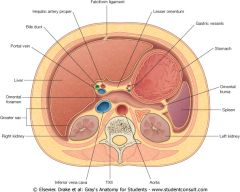
You must pound this abdominal cross-section into your head...especially the important GI ligaments!
|
|
|
|
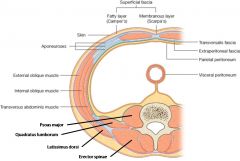
Pound the layers of the abdominal wall into your brain!
|
|
|
|
What structure attaches the digestive tract to the abdominal wall?
|
the mesentery
|
|
|
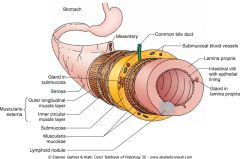
remember the histological layers of the GI tract!
|
|
|
|
Which layer of the muscularis externa is closer to the lumen: the circular layer or the longitudinal layer?
|
the circular layer
|
|
|
What is another name for the serosa?
|
the adventitia
|
|
|
List three components of the gut wall mucosa.
|
epithelium, lamina propria, muscularis muscosa
|
|
|
What is the primary function of the lamina propria of the gut wall mucosa?
|
support
|
|
|
What structure is found within the submucosa of the gut wall?
|
Meissner's plexus
|
|
|
What lies between the inner circular and outer longitudinal layers of the muscularis externa?
|
the myenteric nerve (Auerbach's) plexus
|
|
|
List the four main layers of the gut wall, starting from the inside and going out.
|
mucosa, submucosa, muscularis externa, serosa
|
|
|
What is the rate of basal electrical rhythm in the duodenum?
|
12 waves/min
|
|
|
What is the rate of basal electrical rhythm in the stomach?
|
3 waves/min
|
|
|
What is the rate of basal electrical rhythm in the ileum?
|
8-9 waves/min
|
|
|
In what portion of the gut does the myenteric plexus coordinate motility?
|
along the entire gut wall
|
|
|
The submucosal plexus is located between what two layers?
|
mucosa and the innner (circular) layer of smooth muscle
|
|
|
True or False: The vagus nerve innervates structures at the L3 vertebral level.
|
False; the L3 vertebral level is innervated by the pelvic parasympathetics (hindgut region)
|
|
|
What is the parasympathetic innervation for the liver, gallbladder and pancreas?
|
vagus nerve (CN X)
|
|
|
Where is the division between the foregut and the midgut?
|
Middle of the duodenum, the proximal duodenum is part of the foregut, the distal duodenum is part of the midgut
|
|
|
Where is the division between the midgut and the hindgut?
|
2/3rds of the way through the transverse colon it changes from midgut to hindgut
|
|
|
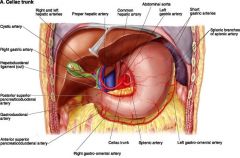
Name the 3 brances of the celiac trunk.
|
Common hepatic artery, splenic artery, and left gastric artery
|
|
|
True or False: The cystic artery is a branch of the hepatic artery proper.
|
False, the cystic artery is a branch of the right hepatic artery
|
|
|
What are the two branches of the gastroduodenal artery?
|
Superior pancreaticoduodenal and right gastroepiploic arteries
|
|
|
True or False: The right and left gastroepiploic arteries anastamose along the lesser margin of the stomach.
|
False, they anastamose along the greater margin
|
|
|
The short gastric arteries have poor anastomoses if the _____ artery is blocked.
|
Splenic
|
|
|
Strong anastomoses exist between what two sets of arteries of the celiac trunk?
|
L & R gastroepicloics and L & R gastrics
|
|
|
Know the branches of the celiac trunk
|
|
|
|
The internal thoracic/mammary (subclavian) can anastamose with the inferior epigastric (external iliac) via what arterial connection?
|
superior epigastric (internal thoracic)
|
|
|
If the abdominal aorta is blocked, the superior pancreaticoduodenal (celiac trunk) artery can anastamose with what vessel?
|
inferior pancreaticoduodenal (SMA)
|
|
|
If the abdominal aorta is blocked, which artery can anastamose with the left colic artery (IMA)?
|
middle colic artery (SMA)
|
|
|
The superior rectal artery (IMA) can anastamose with what artery?
|
middle rectal artery (internal iliac)
|
|
|
Esophageal varices result from anastomoses between the _______ vein and the _______ vein.
|
left gastric vein; esophageal vein
|
|
|
Caput medusae results from anastomoses between the ____ vein and ____/_____ veins.
|
paraumbilical vein; superior and inferior epigastric veins
|
|
|
Hemorrhoids result from anastomoses between the ______ vein and _____ and _____ veins.
|
superior rectal vein; middle and inferior rectal veins
|
|
|
Portocaval shunt placement between the ______ _____ and ______ _____ veins relieves portal hypertension by shunting blood from the ______ circulation to the ______ circulation.
|
splenic vein; left renal vein; portal; systemic
|
|
|
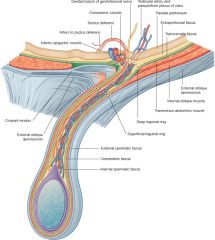
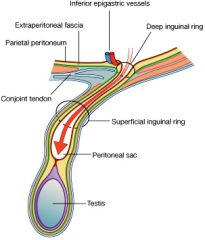
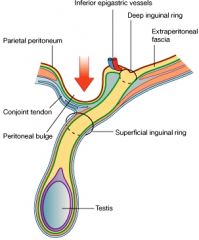
Be sure to know all the layers involved in the inguinal canal
|
|
|
|
What fluid drains through the space of Disse?
|
lymph (in the liver)
|
|
|
In the liver, bile flows from zone ___ (centrilobular zone) to zone _____ (periportal zone).
|
zone III; zone I
|
|
|
In the liver, venous blood flows from the ___ zone to the ___ zone.
|
periportal; centrilobular - remember it enters via the portal vein
|
|
|
In the liver, hepatocytes secrete bile into the bile _____, which drain into the bile _____ leading to the central hepatic duct.
|
canaliculi; ductules
|
|
|
Are the zones of the liver numbered according to the flow of venous blood or of bile
|
According to the flow of venous blood - zone I is where the blood enters (periportal region) and zone III is where the blood exits the liver (centrilobular region)
|
|
|
True or False: Zone I (periportal zone) of the liver is affected first by viral hepatitis.
|
True - remember that viral hepatitis is a BLOOD-BORNE illness
|
|
|
Zone III (pericentral zone/centrilobular zone) is the first site affected by ______ (alcoholic/viral) hepatitis.
|
centrilobular zone; ALCOHOLIC hepatitis (most sensitive to toxins)
|
|
|
Name two characteristics of the sinusoids of the liver that make them "irregular capillaries."
|
fenestrated epithelium and lack of a basement membrane
|
|
|
En route from the liver sinusoids to the hepatocytes, plasma macromolecules must pass through what space?
|
the perisinusoidal space (space of Disse)
|
|
|
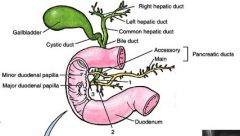
A patient presents with right upper quadrant abdominal pain. Further work-up reveals a gallstone obstructing the common bile duct. Which two biliary ducts drain directly into the common bile duct?
|
cystic duct and common hepatic duct
|
|
|
Know the anatomy of the bile ducts
|
|
|
|
What is the name of the structure formed by the common bile duct and the pancreatic duct as they empty into the duodenum?
|
the ampulla of Vater
|
|
|
What structure forms the lateral border of the femoral triangle?
|
the sartorius muscle
|
|
|
What structure forms the medial border of the femoral triangle?
|
the adductor longus muscle
|
|
|
What three main structures are contained within the femoral sheath?
|
femoral artery, femoral vein, femoral canal
|
|
|
What does the femoral canal contain?
|
the deep inguinal lymph nodes
|
|
|
What femoral triangle structure lies outside of the femoral sheath?
|
the femoral NERVE
|
|
|
What acronym do you use to remember the structures in the femoral triangle?
|
NAVEL - lateral to medial contents of the femoral triangle - Nerve, Artery, Vein, Empty space, Lymphatics - remember the Venous near the Penis
|
|
|
Know indirect inguinal hernias
|
|
|
|
Know direct inguinal hernias
|
|
|
|
What acronym do you use for the contents of the carotid sheath?
|
VAN - think of someone with VAN Morrison tattooed on their neck - Vein, Artery, Nerve
|
|
|
What structure is described in relation to inguinal hernias?
|
inferior epigastric artery
|
|
|
What acronym do you use for the contents of the carotid sheath?
|
VAN - think of someone with VAN Morrison tattooed on their neck - Vein, Artery, Nerve
|
|
|
What structure is described in relation to inguinal hernias?
|
inferior epigastric artery
|
|
|
What is the site of protrusion of an indirect hernia in the inguinal canal?
|
the INternal inguinal ring is the structure through which an INdirect inguinal hernia protrudes
|
|
|
Which runs more medially, the medial umbilical ligament or the median umbilical ligament?
|
the mediaN umbilical ligament - think about how the median of a road is it's dead center
|
|
|
Name the layers that compose the spermatic cord, from the most superficial to the deepest layer.
|
external spermatic fascia, cremasteric muscle, internal spermatic fascia
|
|
|
True or False: The rectus abdominis muscle is deep to the pyramidalis muscle and superficial to the medial/median umbilical ligaments.
|
TRUE
|
|
|
From the most superficial layer to deep, what are the three muscles that cover the internal (deep) inguinal ring?
|
external oblique, internal oblique, rectus abdominis
|
|
|
What cells produce the hormone gastrin?
|
G cells
|
|
|
Where within the gastrointestinal tract are G cells located?
|
the antrum of the stomach
|
|
|
What hormone causes the following three effects: increased hydrogen secretion, increased growth of the gastric mucosa, and increased gastric motility?
|
gastrin
|
|
|
The presence of what substance within the stomach leads to increased gastrin release?
|
amino acids (or peptides) - especially phenylalanine and tryptophan
|
|
|
What cells in the gastrointestinal tract make cholecystokinin?
|
I cells
|
|
|
In cholelithiasis, the worsened pain experienced after the ingestion of fatty foods is the result of the increased release of what substance?
|
CCK - increases contraction of the gallbladder
|
|
|
Secretin is produced by what cells?
|
S cells
|
|
|
Where in the gastrointestinal tract are S cells located?
|
duodenum
|
|
|
What two types of GI hormone secreting cells are found in the duodenum and jejunum but not in the ileum
|
I cells (secrete cholecystokinin, CCK) and K cells (secrete glucose-dependent insulinotropic peptide, GIP)
|
|
|
Secretin has what effect on the pancreas?
|
increased bicarbonate secretion
|
|
|
Which two substances stimuate secretin release within the duodenum?
|
acid and fatty acids
|
|
|
True or False: There are clinically useful inhibitors for the gastrin receptors on the parietal cells.
|
false
|
|
|
Acetylcholine and gastrin act through which second messenger system in parietal cells?
|
Gq / IP3 / Ca signaling
|
|
|
What transporter is required for glucose and galactose uptake?
|
SGLT1 and it's Na+ dependent
|
|
|
What transporter is required for fructose uptake?
|
GLUT-5
|
|
|
What is the only monosaccharide with Na independent uptake?
|
fructose
|
|
|
What transporter is required for monosaccharide transport into the blood?
|
GLUT-2
|
|
|
Fracture of the surgical neck of the humerus damages what nerve?
|
axillary nerve - may also hit the posterior circumflex humoral artery
|
|
|
Fracture of the midshaft of the humerus damages what nerve?
|
radial nerve (lies in the radial groove) - may also hit the profunda brachial/brachii artery
|
|
|
Fracture of the supracondylar humerus damages what nerve?
|
median nerve
|
|
|
Fracture of the medial epicondyle of the humerus damages what nerve?
|
ulnar nerve
|
|
|
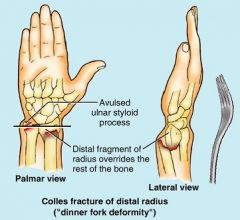
Know where a "Colles" fracture is...most common fracture seen in little only ladies w/ osteoporosis...distal 2 cm of the radius
|
|
|
|
Know your humeral fractures and what arteries and nerves may be damaged with each
|

|
|
|
Match these up correctly: Apolipoproteins B-100 and B-48 / Liver and Intestine
|
B-100 in the liver, B-48 in the intestine - remember apo B-48 in on chylomicrons while apo B-100 is on VLDL and chylomicrons transport dietary TGs while VLDL transports TG synthesized in the liver
|
|
|
Can the liver use ketones for fuel?
|
NO! it's missing a key enzyme in the mito
|
|
|
What congenital defect produces a similar symptom to those seen in an infant with PKU who consumes phenylalanine?
|
congenital pyloric stenosis - will have projectile vomiting
|
|
|
Into what two monomers is lactose degraded?
|
glucose + galactose
|
|
|
Into what two monomers is sucrose degraded?
|
glucose + fructose
|
|
|
A patient has an anterior hip dislocation and can no longer adduct the thigh. She has a sensory deficit along the medial thigh. What nerve has been damaged?
|
obturator n.
|
|
|
A patient has a pelvic fracture. He can no longer flex his thigh or extend his leg. He has a sensory deficit along the anterior thigh and medial leg. What nerve has been damaged?
|
femoral n.
|
|
|
A patient has a pelvic fracture and has damaged his femoral nerve. On physical exam one would expect that he can no longer _____ (flex/extend) his thigh, nor can he _____ (flex/extend) his leg.
|
flex; extend
|
|
|
A patient has a pelvic fracture and has damaged his femoral nerve. On physical exam one would expect decreased sensation along the _____ (anterior/posterior/medial) thigh and along the _____ (anterior/posterior/medial) leg.
|
anterior thigh; medial leg
|
|
|
A patient experiences trauma to his lateral leg and can no longer evert or dorsiflex his foot, nor can he extend his toes. What nerve has been injured, and what sign is evident on physical exam?
|
common peroneal nerve; foot drop
|
|
|
A patient has damaged his common peroneal nerve. What sensory deficit would be expected on physical exam in the foot?
|
decreased sensation in the DORSUM of the foot
|
|
|
A patient has damaged his tibial nerve. What sensory deficit would be expected on physical exam in the foot?
|
decreased sensation in the SOLE of the foot
|
|
|
A patient has had trauma to his knee and can no longer invert or plantar flex his foot, nor can he flex his toes. He has decreased sensation in the sole of his foot. What nerve has been damaged?
|
tibial n.
|
|
|
A patient has a posterior hip dislocation and cannot abduct his thigh (positive Trendelenburg sign). What nerve has been damaged?
|
superior gluteal n.
|
|
|
A patient has a posterior hip dislocation. She can't jump, climb stairs, or rise from a seated position. What nerve has been damaged?
|
inferior gluteal n.
|
|
|
What two nerves may be damaged if a patient sustains a posterior hip dislocation?
|
superior gluteal and inferior gluteal nerves
|
|
|
Loss of foot eversion is due to damage of the _____ _____nerve, while loss of foot inversion is due to damage of the _____ nerve.
|
common peroneal; tibial
|
|
|
Loss of dorsiflexion of the foot is due to damage of the _____ _____nerve, while loss of plantar flexion of the foot is due to damage of the _____ nerve.
|
common peroneal; tibial
|
|
|
If a patient has foot drop, his ______ _____nerve is damaged; but if a patient cannot stand on his tiptoes, then the _____ nerve is damaged.
|
common peroneal; tibial
|
|
|
What nerve innervates the posterior compartment of the lower extremity?
|
tibial n.
|
|
|
During skeletal muscle signal conduction, postsynaptic ligand binding leads to the depolarization of what type of cell?
|
muscle cell in the motor end plate
|
|
|
Where are Dihydropyridine receptors located? Where are Ryanodine receptors located?
|
Dihydropyridine receptors in on the skeletal muscle membrane deep in the T-tubules; Ryanodine receptors are in the sarcoplasmic reticulum membrane
|
|
|
During skeletal muscle contraction, which band(s) of the sarcomere shorten in length?
|
H, I & Z bands - think HIZ shrinkage
|
|
|
During skeletal muscle contraction, which bands of the sarcomere remain(s) the same length?
|
A band - think A is Always the same length
|
|
|
In the sarcomere, does the A-band correspond to the length of actin or myosin?
|
myosin
|
|
|
In the sarcomere, does the I band correspond to the area that is only actin or only myosin?
|
only actin
|
|
|
In the sarcomere, does the H-band correspond to the area that is only actin or only myosin?
|
only myosin
|
|
|
In the sarcomere, is the Z line the site of actin or myosin attachment?
|
actin
|
|
|
In the sarcomere, is the M line the site of actin or myosin attachment?
|
myosin
|
|
|
A sarcomere is defined as the area between one ______ _____to the next ______ _____.
|
z line; z line
|
|
|
In skeletal muscle contraction, ATP binds to what molecule?
|
myosin head - think "it's a SIN to give HEAD" .... and the head gets COCKED when it hydrolyzes ATP
|
|
|
The release of ADP allows for what process in actin/myosin cross-bridging?
|
release of the myosin head from it's binding site on actin
|
|
|
After a smooth muscle membrane is depolarized, voltage-gated _____ _____ will open.
|
calcium channels
|
|
|
In the process of smooth muscle cell contraction, calcium binds to what?
|
calmodulin
|
|
|
With the binding of calcium to calmodulin in smooth muscle contraction, the activation of _____ _____-_____ kinase takes place.
|
myosin light-chain kinase
|
|
|
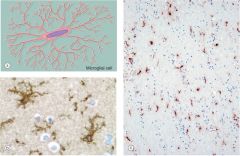
Don't forget what microglia look like!
|
|
|
|
Don't forget what an astrocyte looks like!
|
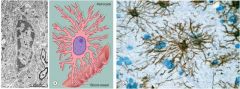
|
|
|
Don't forget what oligodendrocytes look like!
|
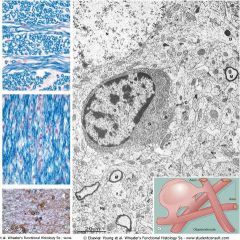
FRIED EGGS!!!
|
|
|
Know structures of the brain stem in a ventral view
|
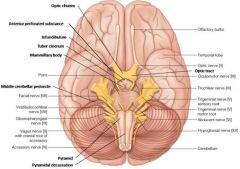
|
|
|
Know the structures of the brain stem in a dorsal view (with the cerebellum removed)
|
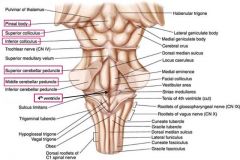
|
|
|
Know the structures that pass through the cavernous sinus
|
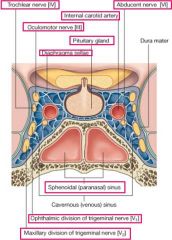
|
|
|
Know the structures of the inner ear
|
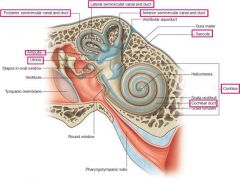
|
|
|
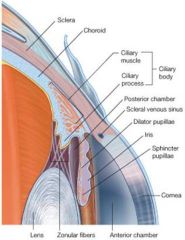
Know the structures of the eye and retina
|
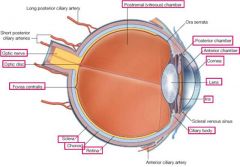
|
|
|
Know the locations of extraocular muscles and related nerves as they exit the bony ocular orbit
|
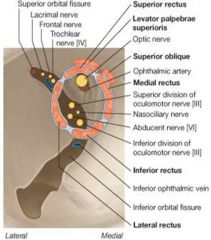
|
|
|
Know the pathway of aqueous humor secretion and reabsorption
|
|
|
|
What are the three first-line drug classes for the treatment of anxiety?
|
SSRIs, benzos, buspirone
|
|
|
What are the three first-line drug classes (all mood stabilizers) for the treatment of bipolar disorder?
|
Lithium, valproic acid, and carbamazepine; atypical antipsychotics can also be used
|
|
|
What are the three first-line drug classes for the treatment of depression?
|
NSRIs, SSRIs, TCAs
|
|
|
What are the two first-line drugs used for the treatment of depression with insomnia?
|
trazadone and mirtazapine
|
|
|
What two drug classes are used in the treatment of atypical depression?
|
MAOIs and SSRIs
|
|
|
What drug classes are used in the treatment of panic disorder?
|
SSRIs, TCAs and Benzos
|
|
|
What two drugs or drug types are used in the treatment of obsessive-compulsive disorder?
|
SSRIs and clomipramine
|
|
|
What two drugs or drug types are used in the treatment of obsessive-compulsive disorder?
|
Antipsychotics (Haloperidol)
|
|
|
Which has mainly neurological side effects, high or low potency antipsychotics?
|
High potency antipsychotics (haloperidol)
|
|
|
Which is better at addressing the negative S/S of schizophrenia, typical or atypical antipsychotics?
|
atypicals address both + and - symptoms; typicals address + symptoms only
|

