![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
149 Cards in this Set
- Front
- Back
Case 1:
- 46 yo male non-smoker presents w/ swelling in L neck for 2 weeks - Attorney, runner, decreased stamina, shortness of breath while running - Good appetite, stable weight - Occasional loose stools - Some back pain (lifting heavy couch) - BP: 115/78, HR: 68, T: 99 - Exam: firm mobile, non-tender lymph nodes, measure 2-3 cm in L lower cervical region of posterior triangle; liver and spleen non-palpable; voluntary guarding in LUQ Which additional information regarding this patient's history would you like to have? |
- Fevers?
- Weight loss? - Medications? - Sick contacts? - Pets (especially cats)? - Travel? - At risk behaviors (drug abuse and sexual behavior)? - Pesticide exposure? - Pre-existing auto-immune disease or immunosuppressive medication? |
|
|
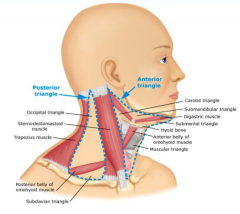
What are the borders of the posterior triangle of the neck?
|
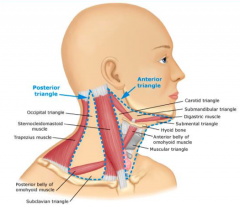
- Sternocleidomastoid muscle
- Trapezius muscle - Clavicle - Made of Occipital triangle and Subclavian triangle |
|
|
What are the borders of the anterior triangle of the neck?
|
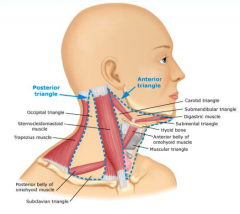
- Sternocleidomastoid muscle
- Midline of neck - Mandible |
|
|
Which lymph nodes drain the cheek, side of nose, lower lip, gums, and anterior tongue?
|
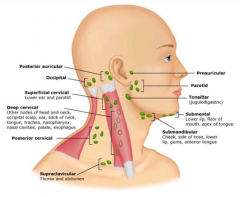
Submandibular lymph nodes
|
|
|
Which lymph nodes drain the lower lip, floor of mouth, and apex of tongue?
|
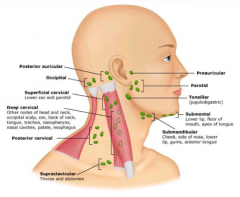
Submental lymph nodes
|
|
|
Which lymph nodes drain the occipital scalp, ear, back of neck, tongue, trachea, nasopharynx, nasal cavities, palate, and esophagus?
|
Deep cervical lymph nodes
|
|
|
Which lymph nodes drain the lower ear and parotid gland?
|
Superficial cervical lymph nodes
|
|
|
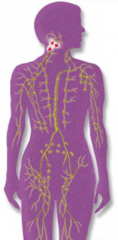
What is the typical distribution of lymphadenopathy?
|
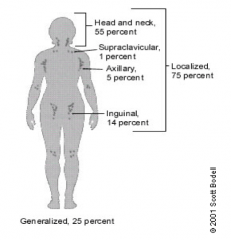
75% localized:
- 55% in head and neck - 1% in supraclavicular region - 5% in axillary region - 14% in inguinal region 25% generalized |
|
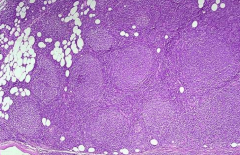
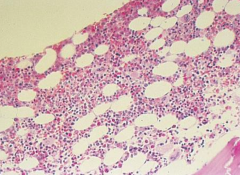
What is this?
|
A normal lymph node
|
|
|
What are the components of a lymph node?
|
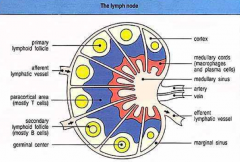
- Cortex: lymphoid follicles, secondary lymphoid follicles (mostly B cells), germinal center
- Paracortical area (mostly T cells) - Medullary cords (macrophages and plasma cells) - Medullary sinus |
|
|
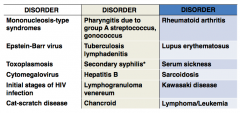
What are some causes of lymphadenopathy?
|
|
|
|
What are the medications that may cause lymphadenopathy?
|
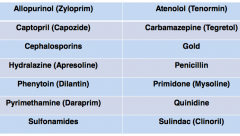
|
|
|
What factors about a patient with lymphadenopathy makes you want to biopsy it?
|
- Age >40 years
- Supraclavicular node location (suggests stomach or ovarian cancer) - Size (diameter) >2cm - Tenderness absent - Consistency rock-hard, fixed, or matted - Persistence >2 weeks |
|
|
What factors about a patient with lymphadenopathy makes you want to observe it (no biopsy)?
|
- Age ≤40 years
- Cervical, inguinal, or axillary node location - Size (diameter) ≤ 2cm - Tenderness present - Consistency rubbery - Persistence ≤ 2 weeks |
|
|
How does a patient's age affect your management of their lymphadenopathy?
|
- Biopsy: >40 years
- Observe: ≤ 40 years |
|
|
How does the location of a patient's lymphadenopathy affect your management?
|
- Biopsy: supraclavicular
- Observe: cervical, inguinal, axillary |
|
|
How does the size of a patient's lymphadenopathy affect your management?
|
- Biopsy: >2 cm
- Observe: ≤ 2 cm |
|
|
How does the tenderness of a patient's lymphadenopathy affect your management?
|
- Biopsy: absent tenderness
- Observe: tenderness present |
|
|
How does the consistency of a patient's lymphadenopathy affect your management?
|
- Biopsy: rock-hard, fixed, matted
- Observe: rubbery |
|
|
How does the persistence of a patient's lymphadenopathy affect your management?
|
- Biopsy: >2 weeks
- Observe: ≤ 2 weeks |
|
|
A malignancy is suspected and needs to be ruled out. A biopsy of the cervical lymph nodes is performed. What are the major malignancies to be considered?
|
- Squamous cell cancer of head and neck
- Metastatic cancer (lung, esophageal, GI, melanoma, etc) - Lymphoid malignancy (lymphoma, leukemia) |
|
|
What are the types of biopsies that can be performed on lymphadenopathy? Which is better?
|
- Needle aspirate
- Excisional biopsy: if you suspect a lymphoma or leukemia you want this type, important because it gives you architecture |
|
Pathologic diagnosis of cervical lymph node biopsy:
• Sections show: sheets of tumor cells characterized by lymphocytes with large cell size, round to irregular nuclear contours, vesicular chromatin, multiple distinct eosinophilic nucleoli, and moderate amounts of eosinophilic cytoplasm. • Flow cytometry revealed a monoclonal B-cell population of large size which was CD10(+) and lambda light chain restricted. • Immunohistochemical stains: The tumor cells show diffuse strong positivity for CD20 and BCL-2. The Cyclin D1 stain is negative in tumor cells. A Ki-67 stain shows a proliferative index of approximately 80% in the tumor cells. Diagnosis? |
Diffuse Large B-cell Lymphoma
|
|
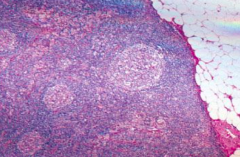
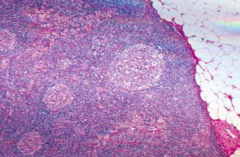
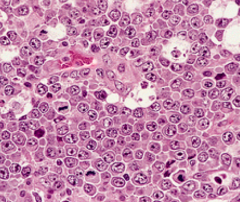
What do you notice about this lymph node?
|
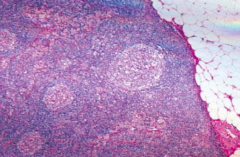
Normal lymph node
|
|
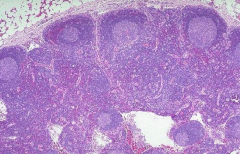
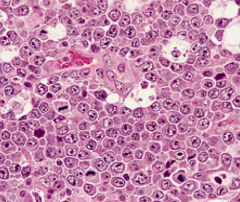
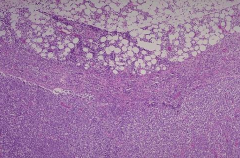
What do you notice about this lymph node?
|
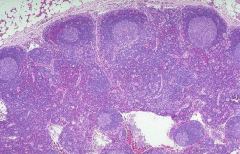
Benign, "reactive" lymph node - they may develop a malignancy in many years
|
|
What do you notice about this lymph node?
|
Follicular Lymphoma
|
|
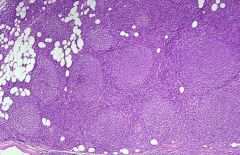
What do you notice about this lymph node?
|
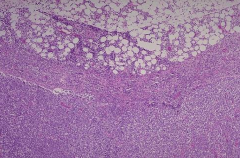
Diffuse Large B-cell Lymphoma
|
|
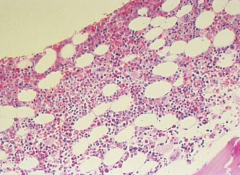
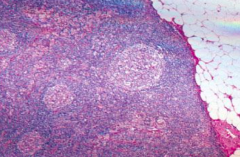
What do you notice about this bone marrow biopsy?
|
Normal bone marrow
|
|
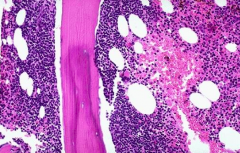
What do you notice about this bone marrow biopsy?
|
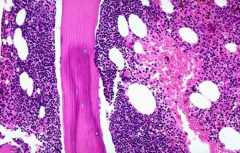
Bone marrow involved by lymphoma
|
|
|
How do B cells develop in the bone marrow?
|
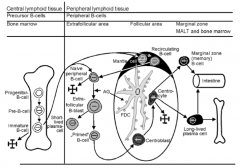
Progenitor B-cell → Pre B-cell → Immature B-cell → Leaves BM to peripheral lymphoid tissue
|
|
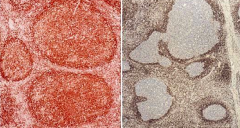
How are these cells stained? What is the difference between L & R slides?
|
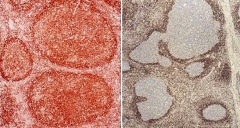
- Stained with bcl-2
- Left: Follicular Lymphoma (strong immunostaining for bcl-2) - Right: Reactive Lymphadenopathy (negative for bcl-2) |
|
|
How can you determine the cell markers on leukocytes?
|
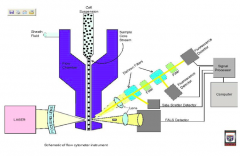
Flow cytometry and Immunohistochemistry
|
|
|
Which lymphoid malignancy is CD5+, CD23-, and FMC7+?
|
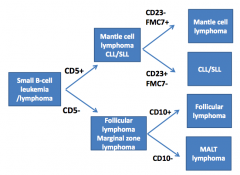
Mantle Cell Lymphoma
|
|
|
Which lymphoid malignancy is CD5+, CD23+, and FMC7-?
|
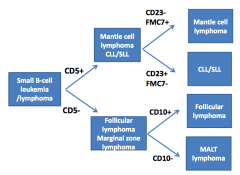
CLL / SLL
|
|
|
Which lymphoid malignancy is CD5- and CD10+?
|
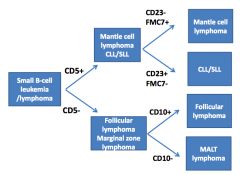
Follicular Lymphoma
|
|
|
Which lymphoid malignancy is CD5+ and CD10-?
|
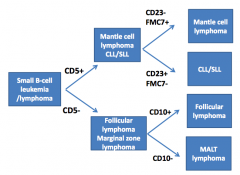
MALT Lymphoma
|
|
|
What is the immunophenotype of Mantle Cell Lymphoma?
|
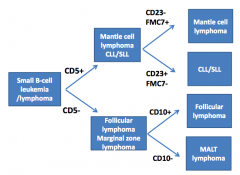
- CD5+
- CD23- - FMC7+ |
|
|
What is the immunophenotype of CLL/SLL?
|
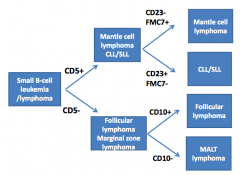
- CD5+
- CD23+ - FMC7- |
|
|
What is the immunophenotype of Follicular Lymphoma?
|
- CD5-
- CD10+ |
|
|
What is the immunophenotype of MALT Lymphoma?
|
- CD5-
- CD10- |
|
|
What translocation is responsible for the pathogenesis of Follicular Lymphoma? What genes are translocated?
|
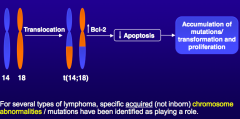
t(14;18): ↑ Bcl-2 → ↓ apoptosis → accumulation of mutations / transformation and proliferation
|
|
|
What translocation is responsible for the pathogenesis of Mantle Cell Lymphoma? What genes are translocated?
|
t(11;14): Cyclin D1 activated
|
|
|
What translocation is responsible for the pathogenesis of CLL? What genes are translocated?
|
t(11;19): NF-κB inhibitor activated
|
|
|
What translocation is responsible for the pathogenesis of Burkitt's Lymphoma? What genes are translocated?
|
t(8;14) - myc transcription factor activated
|
|
|
How common is Non-Hodgkin's Lymphoma?
|
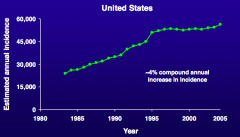
~4% compound annual increase in incidence
|
|
|
What are the most common non-Hodgkin's Lymphoma subtypes?
|
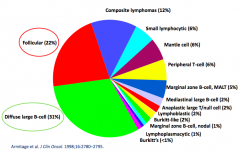
- 31% Diffuse Large B-Cell Lymphoma
- 22% Follicular Lymphoma - 12% Composite Lymphomas - Others <10% |
|
|
What are the different prognoses for non-Hodgkin's Lymphoma?
|
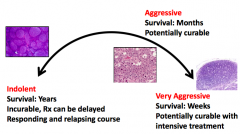
- Indolent (survive for years)
- Aggressive (survive for months) - Very aggressive (survive for weeks) |
|
|
How long does a patient with "indolent" non-Hodgkin's Lymphoma typically live? How is it treated?
|
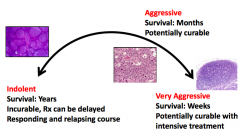
- Survival: years
- Incurable, treatment can be delayed - Responding and relapsing course |
|
|
How long does a patient with "aggressive" non-Hodgkin's Lymphoma typically live? How is it treated?
|
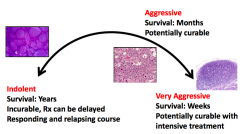
- Survival: months
- Potentially curable |
|
|
How long does a patient with "very aggressive" non-Hodgkin's Lymphoma typically live? How is it treated?
|
- Survival: weeks
- Potentially curable with intensive treatment |
|
|
What are the presenting symptoms of non-Hodgkin's Lymphoma?
|
• Presence of “B symptoms”
– Fevers – Night sweats – Weight loss • Painless enlargement of lymph nodes • Unexplained pain, particularly back / abdominal • Cough • Swelling, especially in ankles or legs • Severe fatigue • Loss of appetite • Less common, but serious, complications: – Low blood counts, kidney failure, liver failure, neurological symptoms (brain or spinal cord), blood clots, bowel obstruction, high calcium levels. |
|
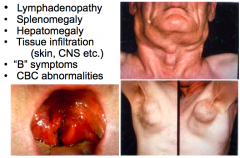
Case 2:
- Patient presents with lymphadenopathy, splenomegaly, hepatomegaly, tissue infiltration (skin, CNS, etc), "B" symptoms (fevers, night sweats, weight loss), and CBC abnormalities What should you do to work up this patient? |
• Physical examination
• CT scans of the chest, abdomen and pelvis • PET scan • Bone marrow biopsy +/- • Lab – CBC, LFTs, Basic chemistries, uric acid, LDH, beta-2 microglobulin and serum protein electrophoresis • Look for infectious agents – HIV, Hepatitis C, H. pylori |
|
|
What are the "B" symptoms?
|
- Fevers
- Night sweats - Weight loss |
|
|
What infectious agents should you check for in a patient who appears to have symptoms of non-Hodgkins Lymphoma?
|
- HIV
- Hepatitis C - H. pylori |
|
|
What labs should you check in a patient who appears to have symptoms of non-Hodgkins Lymphoma?
|
- CBC
- LFTs - Basic chemistries - Uric acid - LDH - β-2 microglobulin - Serum protein electrophoresis |
|
|
What are the characteristics of stage 1 lymph nodes?
|
- Localized disease
- Single lymph node region - Single organ outside of lymph nodes |
|
|
What are the characteristics of stage 2 lymph nodes?
|
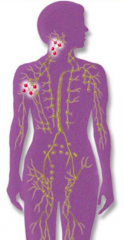
Two or more lymph node regions near to each other
|
|
|
What are the characteristics of stage 3 lymph nodes?
|

Two or more lymph node regions in different parts of the body
|
|
|
What are the characteristics of stage 4 lymph nodes?
|
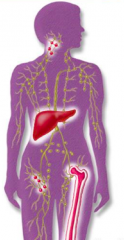
- Widespread disease
- Multiple organs - With or without lymph node involvement |
|
|
What is the function of PET-CT scans in patients with lymphoma?
|
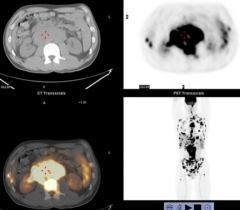
Can look for distribution of malignancy elsewhere - cervical lymphadenopathy may be the tip of the iceberg
|
|
|
How should you treat a patient with diffuse large B-cell lymphoma?
|
Chemo-immunotherapy:
• Cyclophosphamide (Cytoxan) • Doxorubicin (Adriamycin) • Vincristine (Oncovin) • Prednisone • Rituximab (Rituxan) Referred to as R-CHOP (or CHOP-R) Administered every six weeks x 6 cycles |
|
|
Of the drugs in the R-CHOP regimen, which of the following are most likely to put the patient at risk for both hemorrhagic cystitis and dilated cardiomyopathy?
a) Vincristine, rituximab b) Cyclophosphamide, doxorubicin c) Doxorubicin, vincristine d) Cyclophosphamide, rituximab e) Prednisone, doxorubicin |
Cyclophosphamide, doxorubicin
|
|
|
Which R-CHOP drug for diffuse large B-cell lymphoma causes cardiotoxicity, myelosuppression, GI issues, and alopecia?
|
Doxorubicin (Adriamycin)
|
|
|
Which R-CHOP drug for diffuse large B-cell lymphoma causes GI issues, alopecia, myelosuppression, and hemorrhagic cystitis?
|
Cyclophosphamide
|
|
|
Which R-CHOP drug for diffuse large B-cell lymphoma causes Na+/water retention, K+ depletion, increased appetite, weight gain, elevated glucose, hypertension, and increased infection risk?
|
Prednisone
|
|
|
Which R-CHOP drug for diffuse large B-cell lymphoma causes peripheral neuropathy, neurotoxicity, alopecia, and constipation?
|
Vincristine
|
|
|
Which R-CHOP drug for diffuse large B-cell lymphoma causes infusion reactions, fevers, chills, lymphopenia, and tumor lysis syndrome?
|
Rituximab
|
|
|
Of the drugs in the R-CHOP regimen, which one best fits the description of a prodrug?
a) Rituximab b) Cyclophosphamide c) Doxorubicin d) Vincristine e) Prednisone |
Cyclophosphamide
(pro-drug is a drug that is not active and must be activated by the body) |
|
|
How is Cyclophosphamide activated from its pro-drug form? What does it form?
|
Cyclophosphamide --CYP450s--> phosphoramide mustard + acrolein
|
|
|
How does Cyclophosphamide cause hemorrhagic cystitis?
|
Acrolein is a highly reactive aldehyde - associated with sterile hemorrhagic cystitis (drink lots of water!)
|
|
|
Is there an agent to prevent / lessen the hemorrhagic cystitis associated with Cyclophosphamide?
|
2-mercaptoethanesulfonate (MESNA)
• scavenges acrolein |
|
|
All of the following are mechanisms of action associated with doxorubicin, EXCEPT:
a) Binds DNA/topoisomerase II complex b) Causes lipid peroxidation and free radical damage c) Bind tubulin, blocking microtubule assembly d) Intercalates in DNA, distorts DNA helix Which drug does have that mechanism? |
Bind tubulin, blocking microtubule assembly is not an action of Doxorubicin - this is a mechanism of Vincristine
|
|
|
What is the mechanism of Cyclophosphamide?
|
• Once activated, phosphoramide mustard is an alkylating agent
• Alkylates DNA causing strand breaks, adducts, crosslinks |
|
|
What is the mechanism of Rituximab?
|
• Monoclonal Ab that binds to CD20 on cell surface of B lymphocytes (>90% of non-Hodgkins lymphomas)
• Blocks cell cycle initiation, differentiation • Bound antibody recruits immune cells --> cell lysis |
|
|
What is the mechanism of Vincristine?
|
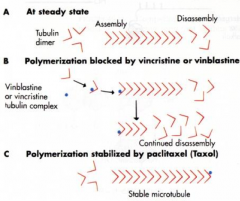
Binds tubulin, blocks assembly of microtubules, mitotic spindle
|
|
|
What is the mechanism of Prednisone?
|
• Binds to steroid receptors, can decrease expression of growth- related genes
• Can induce nucleases which modulate lymphocytic lysis • Anti-inflammatory, stimulates appetite, anti-emetic |
|
|
What are the favorable prognostic factors for the outcome in diffuse large cell lymphoma?
|
- Age < 60 years
- Performance status: 0-2 - Lactate dehydrogenase: normal - Extra-nodal sites: <2 sites - Stage: 1-2 |
|
|
What are the unfavorable prognostic factors for the outcome in diffuse large cell lymphoma?
|
- Age > 60 years
- Performance status: 3-4 - Lactate dehydrogenase: increased - Extra-nodal sites: >2 sites - Stage: 3-4 |
|
|
How does age affect the prognosis for diffuse large cell lymphoma?
|
- Favorable: <60 years
- Unfavorable: >60 years |
|
|
How does performance status (how functional they are) affect the prognosis for diffuse large cell lymphoma?
|
- Favorable: 0-2
- Unfavorable: 3-4 0= completely normal, functional 4= bedridden, non-functional |
|
|
How does lactate dehydrogenase affect the prognosis for diffuse large cell lymphoma?
|
- Favorable: normal LDH
- Unfavorable: increased LDH |
|
|
How do extra-nodal sites affect the prognosis for diffuse large cell lymphoma?
|
- Favorable: <2 sites
- Unfavorable: >2 sites |
|
|
How does stage affect the prognosis for diffuse large cell lymphoma?
|
- Favorable: stage 1-2
- Unfavorable: stage 3-4 |
|
|
Case 1:
- Patient with diffuse large B-cell lymphoma did well for about 18 months without evidence of disease on R-CHOP regimen - He then started to develop night sweats, three weeks later noted enlarged lymph nodes in left lower neck - PET-CT scan showed 2-2.5 cm enlarged neck nodes in R cervical region and 3.5 cm lymph node in superior mediastinum - No other sites of FDG uptake were noted What should be done next? |
High-dose chemotherapy followed by autologous stem cell transplant
- 3 cycles of chemotherapy with: Rituxan, Ifosfamide, Carboplatin, and Etoposide (RICE) There was total resolution of lymphadenopathy on PET scan after 2nd cycle!! He successfully underwent an autologous stem cell line transplant and remains in remission 5 years later!! |
|
|
What is the mechanism of action of Carboplatin?
|

• Platinum coordination complex that causes DNA crosslinks
• Cisplatin analog • Intrastrand crosslinks |
|
|
What is the mechanism of action of Etoposide?
|
Irreversibly binds/stabilizes DNA- topoisomerase II complexes
|
|
|
What is the mechanism of action of Ifosfamide?
|
• Cyclophosphamide analog
• Ifosfamide ---> nitrogen mustard + acrolein |
|
|
What is the side effects of Ifosfamide?
|
• Like cyclophosphamide (GI, alopecia, myelosuppression)
• Additional: nephrotoxicity, neurotoxicity (encephalopathy) - related to chloroacetaldehyde metabolite |
|
|
What is the side effects of Carboplatin?
|
• Cisplatin analog
• Myelosuppression, GI upset • Less nephrotoxicity, neurotoxicity, ototoxicity than cisplatin |
|
|
What is the side effects of Etoposide?
|
• Myelosuppression, alopecia
• GI upset (mild-moderate) • Allergic reactions (low %) |
|
|
The mechanism of action of etoposide is best described as:
a) Metal coordination complex that causes DNA crosslinks b) Metal-containing glycopeptide that causes oxidative DNA damage c) Irreversibly binds/stabilizes DNA-topoisomerase II complexes d) DNA alkylating agent |
Irreversibly binds/stabilizes DNA-topoisomerase II complexes
|
|
|
Which of the following drugs are associated with myelosuppression?
a) Ifosfamide b) Carboplatin c) Etoposide d) All of the above |
All of the above
|
|
|
What can you expect for survival after autologous transplants for diffuse large B-cell lymphoma?
|
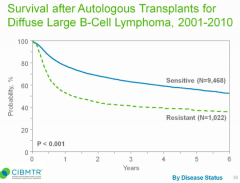
- 60% of patients sensitive to treatment will survive 6 years
- 40% of patients resistant to treatment will survive 6 years |
|
|
Case 2:
- 4 yo boy presents w/ 4-days of fever, runny nose, cough, and sore throat - Pre-kindgerden, several classmates with unspecified illness - New kitten at home; grandparents from rural Mexico visiting for last 2 months - T: 38.6°C, HR 92, RR 16, BP 96/64 - Multiple non-tender sub-cm nodes palpated in submandibular area and bilateral anterior cervical chains - Everything else on exam is normal What is the most likely etiology of this child’s illness? a) Group A streptococcal pharyngitis b) Viral upper respiratory infection c) Epstein-Barr virus infection d) Parinaud’s oculoglandular syndrome d) Kawasaki disease |
Viral upper respiratory infection
|
|
|
What is the meaning of lymphadenopathy?
|
Abnormality in size or consistency of a lymph node
|
|
|
What can cause lymph node enlargement?
|
- Cellular hyperplasia
- Cellular infiltration - Reactive tissue edema |
|
|
How should you evaluate pediatric lymphadenopathy?
|
- Thorough history
- Comprehensive physical exam - Past medical history - Family history - Social history (exposures - other people, exotic locales, animals) - Review of systems |
|
|
An initial diagnostic impression of pediatric lymphadenopathy will be more refined when considering what additional details?
|
– Patient age
– Size of the nodes – Location of the nodes (anatomic location and laterality) – Distribution (localized or generalized) – Quality of the nodes – Time course of lymphadenopathy and associated symptoms |
|
|
How does lymph tissue change with age?
|
- Volume increases with age
- Overall maturity of immune system as an aggregate antigenic exposure increases |
|
|
What should be the characteristics of lymph nodes in a newborn? What should you consider if they are abnormal?
|
- Newborns should not have palpable lymph nodes, though may have congenital lesions that could mimic a node (eg, cystic hygroma, thyroglossal duct cyst)
- Enlarged nodes in neonates should prompt consideration of congenital infections such as toxoplasmosis or CMV |
|
|
What should be the characteristics of lymph nodes in older infants and younger children? What should you consider if they are abnormal?
|
- They will frequently have "shotty" nodes in the head, neck, axillary, or inguinal regions, even when otherwise healthy
- These children are constantly bombarded by viruses |
|
|
What should be the characteristics of lymph nodes in a school-aged child or adolescent? What should you consider if they are abnormal?
|
Less frequently have palpable nodes
- Teenagers start exploring opportunities to develop communicable causes of inguinal adenopathy (and generalized adenopathy) - eg, STIs, EBV, CMV |
|
|
How does the size and location of a lymph node in a pediatric patient affect what you think about it?
|
- A size that could be considered pathologic in one anatomic region may be physiologic in another
- In general, head and neck region nodes should be subcentimeter, inguinal nodes should less than 1.5 centimeters, and most other regions should be less than half a centimeter (In adults, it should concern you if >2cm) |
|
|
What is the function of the lymphatic system?
|
Open circulatory system responsible for circulating lymph through lymphatic vessels, nodes, the spleen, and other lymphoid tissues
|
|
|
What do you need to consider if there is supraclavicular adenopathy?
|
Malignancy should always be high on the differential for supraclavicular adenopathy
- Could also be TB or sarcoidosis! |
|
|
Which lymph node drains the posterior scalp?
|
Occipital LN
|
|
|
Which lymph node drains the temporal and parietal scalp?
|
Post-auricular LN
|
|
|
Which lymph node drains the anterior and temporal scalp, anterior ear canal and pinna, and conjunctiva?
|
Pre-auricular LN
|
|
|
Which lymph node drains the forehead and temporal scalp, midface, external ear canal, middle ear, gums, and parotid gland?
|
Parotid LN
|
|
|
Which lymph node drains the cheek, nose, lips, tongue, submandibular gland, and buccal mucosa?
|
Submandibular LN
|
|
|
Which lymph node drains the lower lip and floor of mouth?
|
Submental LN
|
|
|
Which lymph node drains the lower larynx, lower ear canal, and parotid gland?
|
Superficial cervical LN
|
|
|
Which lymph node drains the tonsils, adenoids, posterior scalp and neck, tongue, larynx, thyroid, palate, nose, esophagus, and paranasal sinuses?
|
Deep cervical LN
|
|
|
Which lymph node drains the mediastinum and lungs?
|
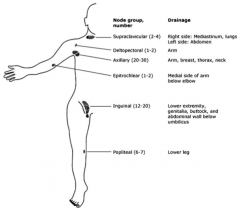
R supraclavicular LN
|
|
|
Which lymph node drains the abdomen?
|
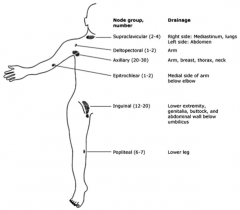
L supraclavicular LN
|
|
|
Which lymph node drains the arms?
|
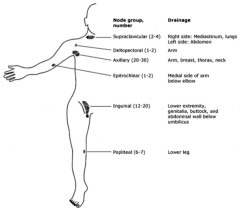
Deltopectoral LN
|
|
|
Which lymph node drains the arms, breasts, thorax, and neck?
|
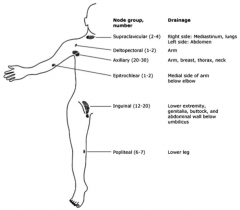
Axillary LN
|
|
|
Which lymph node drains the medial arm below the elbow?
|
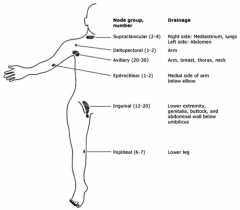
Epitrochlear LN
|
|
|
Which lymph node drains the lower extremity, genitalia, buttocks, and the abdominal wall below the umbilicus?
|
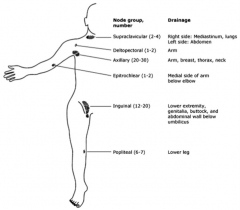
Inguinal LN
|
|
|
Which lymph node drains the lower leg?
|
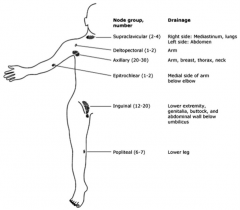
Popliteal LN
|
|
|
How do you define the distribution of lymphadenopathy?
|
• Involvement of one nodal group or contiguous nodal groups constitutes LOCALIZED or regional adenopathy.
• Involvement of two or more non-contiguous nodal groups constitutes GENERALIZED adenopathy |
|
|
What should your differential diagnosis be for systemic generalized lymphadenopathy in a neonate?
|
- Syphilis
- Toxoplasmosis - CMV - HIV (think TORCHES infections? |
|
|
What should your differential diagnosis be for systemic generalized lymphadenopathy in a child?
|
- Viral infection
- EBV - CMV - HIV - Toxoplasmosis |
|
|
What should your differential diagnosis be for systemic generalized lymphadenopathy in an adolescent?
|
- Viral infection
- EBV - CMV - HIV - Toxoplasmosis - Syphilis |
|
|
What are the qualities of normal nodes?
|
- Soft
- Compressible - Freely mobile |
|
|
If a node is tender, what does this usually indicate?
|
- Usually infection
- May be associated with overlying skin changes such as redness or swelling |
|
|
If a node is hard, what does this usually indicate?
|
Usually indicates fibrosis secondary to cancer or a previous infection
|
|
|
If a node is firm and rubbery, what does this usually indicate?
|
May indicate lymphomatous infiltration
|
|
|
If a node is fixing and matting (cluster that all moves together and seems like it is fixed to underlying tissue), what does this usually indicate?
|
Signs of infiltrative changes: could be infectious or malignant process
|
|
|
How does the time course of the lymphadenopathy influence your interpretation?
|
- Acute enlargements (<4 weeks) are more likely to be infectious
- Adenopathy lasting >4 weeks is considered chronic and is more likely to be related to malignancy for chronic infections |
|

Case 2:
- Your 4yo patient returns 2 weeks later w/ several days of progressive L neck swelling and discomfort - Recovered from recent illness, and had been doing well for subsequent 2 weeks - Then developed progressive tender swelling along L side of neck - Several days of fever, tenderness and swelling in neck - Skin around neck is red and he refuses to turn head - Febrile to 39°C, HR 110 (others normal) - Angle of jaw is obscured on L and he is tender to palpation - There is a 3x4 cm indurated area palpable in this region What is the most likely diagnosis? a) Post-viral lymph node syndrome b) Kawasaki disease c) Acute cervical lymphadenitis d) Infected branchial left cyst |

Acute Cervical Lymphadenitis
|
|
|
In a pediatric patient with cervical adenopathy, what are the potential categories? Why categorize?
|
- Acute Bilateral Lymphadenitis
- Acute Unilateral Lymphadenitis - Chronic Cervical Lymphadenopathy - Multiple causes for each, differentiating allows for a more deliberate diagnostic and therapeutic plan |
|
|
What typically causes Acute Bilateral Lymphadenopathy?
|
Usually secondary to head and neck infection, typical pathogens include:
- RSV, adenovirus, influenza, other viral upper respiratory tract pathogens - Occasionally EBV and CMV can cause a mononucleosis that presents with bilateral (typically posterior) cervical adenopathy |
|
|
What typically causes Acute Unilateral Lymphadenopathy?
|
Frequently bacterial in nature
- Usually either S. aureus or group A streptococcal species being implicated - Other important pathogens include oral flora, including anaerobes, from poor dentition - Presence of bacterial species in a lymph node incites a localized inflammatory reaction |
|
|
What typically causes Chronic Cervical Lymphadenopathy?
|
Frequently infections in children
- Tuberculosis - Atypical mycobacteria - Bartonella henselae infection (cat scratch disease) - Other |
|
|
What are the non-infectious etiologies of cervical lymphadenopathy?
|
- Malignant
- Immunologic - Endocrinologic - Miscellaneous |
|
|
How should you approach treatment of infectious cervical adenoapthy?
|
• Treatment should be based upon microbiologic testing whenever possible
• Oftentimes, empiric treatment will have to suffice and should be directed against the most likely pathogens • TREATMENT WITH GLUCOCORTICOIDS SHOULD BE AVOIDED AT ALL COSTS, UNLESS LIFE-THREATENING AIRWAY COMPROMISE IS PRESENT! |
|
|
Staphylococcus and Streptococcus are the most common causes of what type of cervical lymphadenitis? What drugs should be considered?
|
Acute Unilateral Cervical Lymphadenitis:
• Drug examples (Strep., MSSA): – Cephalexin, clindamycin, amoxicillin+clavulanate – Macrolides (e.g. erythromycin) – MSSA: oxacillin, dicloxacillin, cloxacillin • Drugs for community-acquired MRSA: – Linezolid, clindamycin (also cover Strep.) – Doxycycline; TMP/SMX (not good for Strep.) |
|
|
Which drugs can be used to treat Streptococcus and MSSA, causing acute unilateral cervical lymphadenitis?
|
– Cephalexin, clindamycin, amoxicillin+clavulanate
– Macrolides (e.g. erythromycin) – MSSA: oxacillin, dicloxacillin, cloxacillin |
|
|
Which drugs can be used to treat community-acquired MRSA, causing acute unilateral cervical lymphadenitis?
|
– Linezolid, clindamycin (also cover Strep.)
– Doxycycline; TMP/SMX (not good for Strep.) |
|
|
Bartonella can cause what type of cervical lymphadenitis? What drugs should be considered?
|
Subacute or chronic lymphadenitis due to cat-scratch disease:
• Azithromycin: a note of caution—if you are considering empiric treatment, get a PPD first! • Others: ciprofloxacin, rifampin, TMP/SMX • Generally resistant to β-lactams |
|
|
Which drugs can be used to treat Bartonella, causing subacute or chronic lymphadenitis due to cat-scratch disease?
|
• Azithromycin: a note of caution—if you are
considering empiric treatment, get a PPD first (TB skin test)! • Others: ciprofloxacin, rifampin, TMP/SMX • Generally resistant to β-lactams |
|
|
Mycobacterium Avium Intracellulare (MAC) can cause what type of cervical lymphadenitis? What drugs should be considered?
|
Cervical lymphadenitis due to atypical mycobacteria
• Clarithromycin, rifabutin • Others: ethambutol, amikacin, isoniazid |
|
|
Which drugs can be used to treat Mycobacterium Avium Intracellulare (MAC), causing cervical lymphadenitis?
|
• Clarithromycin, rifabutin
• Others: ethambutol, amikacin, isoniazid |
|
|
Case 2:
- 4 yo boy with acute unilateral cervical lymphadenitis Your patient is hospitalized for parenteral treatment of his lymphadenitis. You want to choose a regimen that will cover the most likely pathogens. Your choice should focus on all of the following bacteria except: a) Gram-positive cocci b) Oral anaerobes c) Gram-negative enteric rods d) None of the above |
G- enteric rods (usually wouldn't suspect these to cause unilateral cervical lymphadenitis)
|
|
|
What should you consider as the cause of regional lymphadenopathy?
|
- Infectious etiologies in the drainage area should be the first consideration
- Consider further studies and diagnoses if the lymphadenopathy fails to resolve with observation or empiric treatment - Non-infectious considerations: Kawasaki disease, malignancy, sarcoidosis |
|
|
What are the six key characteristics that should be described for involved lymph nodes?
|
- Age of patient
- Size - Location - Distribution - Quality (eg, soft, tender, hard, firm, etc) - Timing - |
|
|
What is the most frequent cause of cervical lymphadenopathy in pediatric patients?
|
Infection
|
|
|
What should you take into consideration when considering empiric treatment of lymphadenopathy?
|
- Risk of malignancy
- Tuberculosis - Atypical mycobacterial infection |

