![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
268 Cards in this Set
- Front
- Back
|
What does VATS stand for? |
Video-Assisted Thoracic Surgery (VATS) |
|
|
What is thoracic outlet syndrome? |
Compression of the: - Subclavian artery - Subclavian vein OR - Brachial plexus at the superior outlet of the thorax |
|
|
What are the causes of thoracic outlet syndrome? |
1. Various congenital anomalies, including cervical rib or abnormal fascial bands to the first rib, or abnormal anterior scalene muscle 2. Trauma: fracture of clavicle or first rib, dislocation of humeral head, or crush injuries 3. Repetitive motor injuries (baseball pitchers) |
|
|
What are the symptoms of thoracic outlet syndrome? |
- Paresthesias (neck, shoulder, arm, hand); 90% are in ulnar nerve distribution - Weakness (neural/arterial) - Coolness of involved extremity (arterial) - Edema, venous distention, discoloration (venous) |
|
|
What are the most common types of symptoms with thoracic outlet syndrome? |
Neurologic |
|
|
Which nerve is most often involved in thoracic outlet syndrome? |
Ulnar nerve |
|
|
What are the signs of thoracic outlet syndrome? |
- Paget-von Schroetter syndrome (Venous thrombosis leading to edema, arm discoloration, and distention of superficial veins) - Weak brachial and radial pulses in the involved arm - Hypesthesia/anesthesia - Occasionally, atrophy in the distribution of ulnar nerve - Positive Adson maneuver / Tinel's sign - Edema |
|
|
What is the Adson maneuver? |
Evaluates for arterial compromise (sign of thoracic outlet syndrome)
Patient: 1. Extends neck (lifts head) 2. Takes a deep breath and holds 3. Turns head toward examined side
Physician: - Monitors radial pulse on examined side - Test finding is positive if the radial pulse decreases or disappears during maneuver |
|
|
What is Tinel's test? |
Tapping of the supraclavicular fossa producing paresthesias |
|
|
What is the treatment of thoracic outlet syndrome? |
- Physical therapy (vast majority of cases) - Decompression of the thoracic outlet by resecting the first rib and cervical rib (if present) if PT fails and as a last resort |
|
|
What are the most common types of benign chest wall tumors? |
1. Fibrous rib dysplasia (posterolateral rib) 2. Chondroma (at costochondral junction) 3. Osteochondroma (any portion of rib) |
|
|
What is the treatment of benign chest wall tumors? |
Wide excision and reconstruction with autologous or prosthetic grafts |
|
|
What are the most common malignant chest wall tumors? |
1. Fibrosarcoma 2. Chondrosarcoma 3. Osteogenic sarcoma 4. Rhabdomyosarcoma 5. Myeloma 6. Ewing's sarcoma |
|
|
What is the treatment of malignant chest wall tumors? |
Excision with or without radiation |
|
|
What is Tietze's syndrome? |
Non-infectious costochondral cartilage inflammation |
|
|
What is a pleural effusion? |
Fluid in the pleural space |
|
|
What are the causes of pleural effusions? |
1. Pulmonary infections (pneumonia) 2. Congestive heart failure (CHF) 3. SLE or rheumatoid arthritis 4. Pancreatitis (sympathetic effusion) 5. Trauma 6. Pulmonary embolism 7. Renal disease 8. Cirrhosis 9. Malignancy (mesothelioma, lymphoma, metastasis) 10. Post-pericardiotomy syndrome |
|
|
What are the symptoms of pleural effusions? |
- Dyspnea - Pleuritic chest pain |
|
|
What are the signs of pleural effusions? |
- Decreased breath sounds - Dullness to percussion - Egophony at the upper limit |
|
|
What are the properties of a transudative pleural effusion? |
- Specific gravity <1.016 - Protein <3 g/dL - Few cells |
|
|
What are the properties of an exudative pleural effusion? |
- Specific gravity >1.016 - Protein >3 g/dL - Many cells |
|
|
What is the key diagnostic test for pleural effusions? |
Thoracentesis (needle drainage) with studies including cytology |
|
|
What is the treatment of pleural effusions? |
1. Pigtail catheter or thoracostomy (chest tube) 2. Treat underlying condition 3. Consider sclerosis |
|
|
What is an empyema? |
- Infected pleural effusion; must be drained, usually with chest tube(s) - Decortication may be necessary if the empyema is solid |
|
|
What is decortication? |
Thoracotomy and removal of an infected fibrous rind from around the lung (think of it as taking off a fibrous "cortex" from the lung) |
|
|
What are the signs/symptoms of a lung abscess? |
- Fever - Sputum - Sepsis - Fatigue |
|
|
What are the associated diagnostic studies for a lung abscess? |
- CXR: air-fluid level - CT scan to define position and to differentiate from an empyema - Bronchoscopy (looking for cancer / culture) |
|
|
What is the treatment for a lung abscess? |
- Antibiotics - Bronchoscopy for culture and toilet - With or without surgery |
|
|
What are the indications for surgery in a patient with a lung abscess? |
- Underlying cancer / tumor - Refractory to antibiotics |
|
|
What are the surgical options for a lung abscess? |
- Lobectomy of lobe with abscess - Tube drainage |
|
|
What is middle lobe syndrome? |
Recurrent right middle lobe pneumonia caused most commonly by extrinsic bronchial obstruction |
|
|
What is hemoptysis? |
Bleeding into the bronchial tree |
|
|
What are the causes of hemoptysis? |
1. Bronchitis (50%) 2. Tumor mass (20%) 3. TB (8%)
Other: bronchiectasis, pulmonary catheters, trauma |
|
|
Define MASSIVE hemoptysis? |
>600 cc / 24 hours |
|
|
What comprises the workup for hemoptysis? |
- CXR - Bronchoscopy - Bronchial A-gram |
|
|
What is the treatment for massive hemoptysis? |
- Bronchoscopy - Intubation of unaffected side - Fogarty catheter occlusion of bleeding bronchus - Bronchial A-gram with or without embolization - Surgical resection of involved lung |
|
|
What is the treatment of mild to moderate hemoptysis? |
- Laser coagulation - +/- Epinephrine injection |
|
|
What is a spontaneous pneumothorax? |
Atraumatic spontaneous development of a pneumothorax |
|
|
What are the causes of spontaneous pneumothorax? |
- Idiopathic (primary) - Bleb disease - Emphysema |
|
|
What body habitus is associated with spontaneous pneumothorax? |
Thin and tall |
|
|
How do you diagnose spontaneous pneumothorax? |
CXR |
|
|
How do you treat a spontaneous pneumothorax? |
Chest tube |
|
|
What are the options if refractory, recurrent, or bilateral spontaneous pneumothoraces? |
Pleurodesis: scar the lung to the parietal pleura with a sclerosant (talc) via chest tube / thoracoscopy, or by thoracotomy and mechanical abrasion |
|
|
Who might also need a pleurodesis after the first episode of spontaneous pneumothorax? |
Those whose lifestyle places them at increased risk for pneumothorax (eg, pilots, scuba divers) |
|
|
What is a catamenial pneumothorax? |
Pneumothorax due to intrathoracic endometriosis |
|
|
What is malignant mesothelioma? |
Primary pleural neoplasm |
|
|
What are the types of malignant mesothelioma? |
1. Localized 2. Diffuse (highly malignant) |
|
|
What are the risk factors for malignant mesothelioma? |
- Exposure to asbestos - Smoking |
|
|
What are the symptoms of malignant mesothelioma? |
- Dyspnea and pain = 90% - Localized: pleuritic pain, joint pain and swelling, dyspnea - Diffuse: chest pain, malaise, weight loss, cough |
|
|
What are the signs of malignant mesothelioma? |
Pleural effusions: - Localized (10-15%) - Diffuse (>75%) |
|
|
What are the radiographic tests for detecting malignant mesothelioma? |
- CXR may reveal a peripheral mass, often forming an obtuse angle with the chest wall - CT scan is also performed |
|
|
How do you diagnose malignant mesothelioma? |
Pleural biopsy, pleural fluid cytology |
|
|
What is the treatment of malignant mesothelioma if localized? |
Surgical excision |
|
|
What is the treatment of malignant mesothelioma if diffuse? |
- Early stages may be resected, followed by radiation - For more advanced stages, radiation, chemotherapy, or both are done |
|
|
What is the prognosis for malignant mesothelioma? |
- Localized: poor - Diffuse: dismal (average life span after diagnosis is about 1 year) |
|
|
What is benign mesothelioma? |
Benign pleural mesothelioma |
|
|
What pleura is usually involved in a benign mesothelioma? |
Visceral pleura |
|
|
What is the gross appearance of benign mesothelioma? |
Pedunculated "broccoli or cauliflower" tumor on a stalk coming off of the lung |
|
|
What is the treatment for benign mesothelioma? |
Surgical resection with at least 1 cm clear margin |
|
|
What is the prognosis for benign mesothelioma? |
In contrast to malignant mesothelioma, the benign mesothelioma has an excellent prognosis with cure in the vast majority of cases |
|
|
What is the annual incidence of lung cancer in the US? |
170,000 new cases / year |
|
|
What is the number of annual deaths from lung cancer? |
150,000 - most common cancer death in the US in men AND women |
|
|
What is the #1 risk factor for bronchogenic carcinoma? |
Smoking (85%) |
|
|
Does asbestos exposure increase the risk of bronchogenic carcinoma in patients who smoke? |
Yes |
|
|
What type of lung cancer arises the most in non-smokers? |
Adenocarcinoma |
|
|
Cancer arises more often in which lobes of the lung? |
Right > Left
Upper lobes > Lower lobes |
|
|
What are the signs/symptoms of bronchogenic carcinoma? |
- Change in a chronic cough - Hemoptysis, chest pain, dyspnea - Pleural effusion (suggests chest wall involvement) - Hoarseness (recurrent laryngeal nerve involvement) - Superior vena cava syndrome - Diaphragmatic paralysis (phrenic nerve involvement) - Symptoms of metastasis / paraneoplastic syndrome - Finger clubbing |
|
|
What is Pancoast's tumor? |
Tumor at the apex of the lung or superior sulcus that may involve the brachial plexus, sympathetic ganglia, and vertebral bodies, leading to pain, upper extremity weakness, and Horner's syndrome |
|
|
What is Horner's syndrome? |
Injury to the cervical sympathetic chain; Think: "MAP" 1. Miosis (small pupil) 2. Anhydrosis of ipsilateral face 3. Ptosis |
|
|
What are the four most common sites of extrathoracic metastases of bronchogenic carcinoma? |
1. Bone 2. Liver 3. Adrenals 4. Kidney |
|
|
What are paraneoplastic syndromes? |
Syndromes that are associated with tumors but may affect distant parts of the body; they may be caused by hormones released from endocrinologically active tumors or may be of uncertain etiology |
|
|
Name five general types of paraneoplastic syndromes? |
1. Metabolic: Cushing's, SIADH, hypercalcemia 2. Neuromuscular: Eaton-Lambert, cerebellar ataxia 3. Skeletal: hypertrophic osteoarthropathy 4. Dermatologic: acanthosis nigricans 5. Vascular: thrombophlebitis |
|
|
What are the radiographic tests used to diagnose bronchogenic carcinoma? |
- CXR - CT scan - PET scan |
|
|
How do you diagnose bronchogenic carcinoma? |
1. Sputum cytology 2. Needle biopsy (CT or fluoro guidance) 3. Bronchoscopy w/ brushings, biopsies, or both 4. With or without mediastinoscopy, mediastinotomy, scalene node biopsy, or open lung biopsy for definitive diagnosis |
|
|
What is the usual site in the lung and the natural course of squamous cell carcinoma? |
- 66% occur centrally in lung hilus; may also be a Pancoast's tumor - Slow growth, late metastasis - Associated with smoking
Think: Squamous = Sentral |
|
|
What is the usual site in the lung and the natural course of adenocarcinoma? |
- Peripheral - Rapid growth with hematogenous / nodal metastasis - Associated with lung scarring |
|
|
What is the usual site in the lung and the natural course of small (oat) cell? |
- Central, highly malignant - Usually not operable |
|
|
What is the usual site in the lung and the natural course of large cell? |
- Usually peripheral - Very malignant |
|
|
What is the definition of carcinoma of the lungs AJCC stage IA? |
Tumor <3 cm, no nodes, no metastases |
|
|
What is the definition of carcinoma of the lungs AJCC stage IB? |
Tumor 3-5 cm, no nodes, no metastases |
|
|
What is the definition of carcinoma of the lungs AJCC stage IIA? |
1. Tumor <5 cm and positive nodes to lung or ipsilateral hilum; no metastases OR 2. Tumor 5-7 cm, no nodes, no metastases |
|
|
What is the definition of carcinoma of the lungs AJCC stage IIB? |
1. Tumor 5-7 cm and positive nodes in lung or ipsilateral hilum OR 2. Tumor that invades chest wall, diaphragm, mediastinal pleura, phrenic nerve, pericardial sac, or bronchus (not carina) and no nodes, no metastases |
|
|
What is the definition of carcinoma of the lungs AJCC stage IIIA? |
1. Tumor <7 cm and positive nodes in ipsilateral mediastinum or subcarina with NO metastases OR 2. Tumor >7 cm or extends into chest wall, parietal pleura, diaphragm, phrenic nerve, or pericardium and positive lymph node metastases to ipsilateral, mediastinal, or subcarinal nodes OR 3. Any size tumor that invades heart, great vessels, trachea, esophagus, carina, or ipsilateral lobe, or positive nodes peribronchial and/or ipsilateral hilum, or intrapulmonary nodes |
|
|
What is the definition of carcinoma of the lungs AJCC stage IIIB? |
- Any tumor, positive lymph node metastases to contralateral hilum or mediastinum - Supraclavicular / scalene nodes, NO distant metastases |
|
|
What is the definition of carcinoma of the lungs AJCC stage IV? |
Distant metastases |
|
|
What are the surgical contraindications for NON-small cell carcinoma? |
- Stage IV - Stage IIIB - Poor lung function (FEV1 <0.8 L) |
|
|
What is the treatment for NON-small cell lung carcinoma stage I? |
Surgical resection |
|
|
What is the treatment for NON-small cell lung carcinoma stage II? |
Surgical resection |
|
|
What is the treatment for NON-small cell lung carcinoma stage IIIA? |
Chemotherapy and XRT +/- surgical resection |
|
|
What is the treatment for NON-small cell lung carcinoma stage IIIB? |
Chemotherapy and XRT |
|
|
What is the treatment for NON-small cell lung carcinoma stage IV? |
Chemotherapy +/- XRT |
|
|
What is the treatment for isolated brain metastasis from lung cancer? |
Surgical resection |
|
|
What is the approximate prognosis (5-year survival) after treatment of NON-small cell lung carcinoma stage I? |
50% |
|
|
What is the approximate prognosis (5-year survival) after treatment of NON-small cell lung carcinoma stage II? |
30% |
|
|
What is the approximate prognosis (5-year survival) after treatment of NON-small cell lung carcinoma stage III? |
<10% |
|
|
What is the approximate prognosis (5-year survival) after treatment of NON-small cell lung carcinoma stage IV? |
1% |
|
|
How is small cell carcinoma treated? |
Chemotherapy +/- XRT (very small isolated lesions can be surgically resected) |
|
|
What are the contraindications to surgery for lung cancer? |
Think: "STOP IT" - Superior vena cava syndrome - Supraclavicular node metastasis - Scalene node metastasis - Tracheal carina involvement - Oat cell carcinoma (treat with chemo +/- radiation) - Pulmonary function tests show FEV1 <0.8L - Infarction (myocardial); aka cardiac cripple - Tumor elsewhere (metastatic disease) |
|
|
What post-op FEV1 must you have to have surgery for lung cancer? |
- FEV1 >800 cc; thus, a pre-op FEV1 >2L is usually needed for a pneumonectomy - If FEV1 is <2L, a ventilation perfusion scan should be performed |
|
|
What is hypertrophic pulmonary osteoarthropathy? |
Periosteal proliferation and new bone formation at the end of long bones and in the bones of the hand (seen in 10% of patients with lung cancer) |
|
|
What are solitary pulmonary nodules (coin lesions)? |
Peripheral circumscribed pulmonary lesions |
|
|
What is the differential diagnosis for solitary pulmonary nodules (coin lesions)? |
- Granulomatous disease - Benign neoplasms - Malignancy |
|
|
What percentage of solitary pulmonary nodules (coin lesions) are malignant? |
Overall, 5-10% (but >50% are malignant in smokers >50 years old) |
|
|
Is there a gender risk for solitary pulmonary nodules (coin lesions)? |
Yes; the incidence of coin lesions is 3-9x higher and malignancy is nearly twice as common in men as in women |
|
|
What are the symptoms of solitary pulmonary nodules (coin lesions)? |
Usually asymptomatic with solitary nodules, but may include coughing, weight loss, chest pain, and hemoptysis |
|
|
What are the signs of solitary pulmonary nodules (coin lesions)? |
- Physical findings are uncommon - Clubbing is rare - Hypertrophic osteoarthropathy implies >80% chance of malignancy |
|
|
How is the diagnosis of solitary pulmonary nodules (coin lesions) made? |
- CXR - Chest CT |
|
|
What is the significance of "popcorn" calcification? |
Most likely benign (ie, hamartoma) |
|
|
What are the risk factors for malignancy with solitary pulmonary nodules (coin lesions)? |
1. Size: lesions >1 cm have a significant chance of malignancy, and those >4 cm are very likely to be malignant 2. Indistinct margins (corona radiata) 3. Documented growth on follow-up x-ray (if no change in 2 years, most likely benign) 4. Increasing age |
|
|
What are the lab tests that should be used to evaluate patients with solitary pulmonary nodules (coin lesions)? |
1. TB skin tests, etc 2. Sputum cultures 3. Sputum cytology (diagnostic in 5-20% of cases) |
|
|
Which method of tissue diagnosis is used for solitary pulmonary nodules (coin lesions)? |
- Chest CT scan with needle biopsy - Bronchoscopy (+/- transtracheal biopsy) - Excisional biopsy (open or thoracoscopic) |
|
|
What is the treatment of solitary pulmonary nodules (coin lesions)? |
- Surgical excision is the mainstay of treatment - Excisional biopsy is therapeutic for benign lesions, solitary metastasis, and for primary cancer in patients who are poor risks for more extensive surgery - Lobectomy for centrally placed lesions - Lobectomy with node dissection for primary cancer (if resectable by pre-op evaluations) |
|
|
Which solitary nodule can be followed without a tissue diagnosis? |
- Popcorn calcifications - Mass unchanged for 2 years on previous CXR |
|
|
What is the prognosis of solitary pulmonary nodules (coin lesions)? |
For malignant coin lesions <2 cm, 5-year survival is ~70% |
|
|
What if the patient has a solitary pulmonary nodule and pulmonary hypertrophic osteoarthropathy? |
>75% chance of carcinoma |
|
|
What is hypertrophic pulmonary osteoarthropathy? |
Periosteal proliferation and new bone formation at the end of long bones and in bones of the hand |
|
|
What is the incidence of hypertrophic pulmonary osteoarthropathy? |
~7% of patients with lung cancer (2-12%) |
|
|
What are the signs of hypertrophic pulmonary osteoarthropathy? |
- Associated with clubbing of fingers - Diagnosed by x-ray of long bones, revealing periosteal bone hypertrophy |
|
|
What is a carcinoid tumor? |
APUD (Amine-Precursor Uptake and Decarboxylation) cell tumor of the bronchus |
|
|
What is the natural course of carcinoid tumor in the lung? |
Slow growing (but may be malignant) |
|
|
What are the primary local findings of carcinoid tumor? |
Wheezing and atelectasis caused by bronchial obstruction / stenosis |
|
|
What condition can carcinoid tumors be confused with? |
Asthma |
|
|
How do you diagnose carcinoid tumor of the lung? |
Bronchoscopy reveals round red-yellow-purple mass covered by epithelium that protrudes into bronchial lumen |
|
|
What is the treatment of carcinoid tumor? |
- Surgical resection (lobectomy with lymph node dissection) - Sleeve resection is also an option for proximal bronchial lesions) |
|
|
What is a sleeve resection? |
Resection of a ring segment of bronchus (with carcinoid tumor inside) and then end-to-end anastomosis of the remaining ends, allowing salvage of lower lobe |
|
|
What is the prognosis (5-year survival) after complete surgical resection of carcinoid tumor with negative nodes? |
>90% alive at 5 years |
|
|
What is the prognosis (5-year survival) after complete surgical resection of carcinoid tumor with positive nodes? |
66% alive at 5 years |
|
|
What is the most common benign lung tumor? |
Hamartoma (normal cells in a weird configuration) |
|
|
What is pulmonary sequestration? |
Abnormal benign lung tissue with separate blood supply that DOES NOT communicate with the normal tracheobronchial airway |
|
|
What is an "interlobar" pulmonary sequestration? |
Sequestration in normal lung tissue covered by normal visceral pleura |
|
|
What is an "extralobar" pulmonary sequestration? |
Sequestration not in normal lung covered by its own pleura |
|
|
What are the signs/symptoms of pulmonary sequestration? |
Asymptomatic, recurrent pneumonia |
|
|
How do you diagnose pulmonary sequestration? |
- CXR - Chest CT - Angiogram - U/S with Doppler flow to ascertain blood supply |
|
|
What is the treatment of extralobar pulmonary sequestration? |
Surgical resection |
|
|
What is the treatment of intralobar pulmonary sequestration? |
Lobectomy |
|
|
What is the major danger during surgery for pulmonary sequestration? |
- Anolamous blood supply from below the diaphragm (these can be cut and retract into the abdomen resulting in exsanguination!) - Always document blood supply by A-gram or U/S with Doppler flow |
|
|
What structures lie in the superior mediastinum? |
- Aortic arch - Great vessels - Upper trachea - Esophagus |
|
|
What structures lie in the anterior mediastinum? |
- Thymus - Ascending aorta - Lymph nodes |
|
|
What structures lie in the middle mediastinum? |
- Heart - Lower trachea and bifurcation - Lung hila - Phrenic nerves - Lymph nodes |
|
|
What structures lie in the posterior mediastinum? |
- Esophagus - Descending aorta - Thoracic duct - Vagus and intercostal nerves - Sympathetic trunks - Azygous and hemizygous veins - Lymph nodes |
|
|
What is the major differential diagnosis for tumors of the anterior mediastinum? |
Classic "four T's": - Thyroid tumor - Thymoma - Terrible lymphoma - Teratoma
Also parathyroid tumor, lipoma, vascular aneurysms |
|
|
What is the major differential diagnosis for tumors of the middle mediastinum? |
- Lymphadenopathy (eg, lymphoma, sarcoid) - Teratoma - Fat pad - Cysts - Hernias - Extension of esophageal mass - Bronchogenic cancer |
|
|
What is the major differential diagnosis for tumors of the posterior mediastinum? |
- Neurogenic tumors - Lymphoma - Aortic aneurysm - Vertebral lesions - Hernias |
|
|
What is the most common type of tumor arising in the mediastinum? |
Neurogenic (most commonly in posterior mediastinum) |
|
|
What is the most common type of tumor arising in the mediastinum? |
Neurogenic (most commonly in posterior mediastinum) |
|
|
What is the differential diagnosis for a neurogenic tumor? |
- Schwannoma (aka neurolemmoma) - Neurofibroma - Neuroblastoma - Ganglioneuroma - Ganglioneuroblastoma - Pheochromocytoma |
|
|
Where are thymomas found in the mediastinum? |
Anterior |
|
|
How do you diagnose a thymoma? |
CT scan |
|
|
What is the treatment for thymoma? |
All thymomas should be surgically resected via midline sternotomy |
|
|
What are the indications for POST-op radiation therapy in treatment of thymomas? |
Invasive malignant tumors |
|
|
What are the indications for PRE-op chemo therapy for thymoma? |
Tumor >6 cm and CT scan with invasion |
|
|
What percentage of thymomas are malignant? |
~25% |
|
|
How is a malignant thymoma diagnosed? |
At surgery with invasion into surrounding structures (not by histology!) |
|
|
What is myasthenia gravis? |
Auto-immune disease with antibodies against the muscle acetylcholine receptors |
|
|
What percentage of patients with myasthenia gravis patients have a thymoma? |
~15% |
|
|
What percentage of patients with thymoma have or will have myasthenia gravis? |
~75% |
|
|
What are teratomas? |
Tumors of branchial cleft cells; the tumors contain ectoderm, endoderm, and mesoderm |
|
|
What is a dermoid cyst? |
Teratoma made up of ectoderm derivatives (eg, teeth, skin, hair) |
|
|
Which age group is affected by teratomas? |
Usually adolescents but can occur at any age |
|
|
Where in the mediastinum do teratomas occur? |
Anterior mediastinum |
|
|
What are the characteristic x-ray findings of teratomas? |
Calcifications or teeth; tumors may be cystic |
|
|
What percentage of teratomas are malignant? |
~15% |
|
|
What is the treatment of benign dermoid cysts? |
Surgical excision |
|
|
What is the treatment of malignant teratomas? |
Pre-op chemo until tumor markers are normal, then surgical resection |
|
|
Which tumor markers are associated with malignant teratomas? |
- AFP - CEA |
|
|
What is the incidence of neurogenic tumors? |
Most common mediastinal tumors in all age groups |
|
|
Where in the mediastinum do neurogenic tumors occur |
Posterior, int he paravertebral gutters |
|
|
What percentage of neurogenic tumors are malignant? |
50% in children 10% in adults |
|
|
What are the histologic types of neurogenic tumors? (note cells of origin and whether benign or malignant) |
1. Neurilemmoma or schwannoma (benign) - arise from Schwann cell sheaths of intercostal nerves 2. Neurofibroma (benign) - arise from intercostal nerves; may degenerate into: 3. Neurosarcoma (malignant) 4. Ganglioneuroma (benign) - from sympathetic chain 5. Neuroblastoma (malignant) - also from sympathetic chain |
|
|
Where in the mediastinum does a lymphoma occur? |
Anywhere, but most often in the anterosuperior mediastinum or hilum in the middle mediastinum |
|
|
What percentage of lymphomas involve mediastinal nodes? |
~50% |
|
|
What are the symptoms of lymphoma? |
- Cough - Fever - Chest pain - Weight loss - SVC syndrome - Chylothorax |
|
|
How do you diagnose lymphoma? |
1. CXR, CT scan 2. Mediastinoscopy or mediastinotomy with node biopsy |
|
|
What is the treatment of lymphoma? |
Non-surgical (chemo, radiation, or both) |
|
|
What is acute mediastinitis? |
Acute suppurative mediastinal infection |
|
|
What are the six etiologies of acute mediastinitis? |
1. Esophageal perforation (Boerhaave's syndrome) 2. Post-op wound infection 3. Head and neck infections 4. Lung or pleural infections 5. Rib or vertebral osteomyelitis 6. Distant infections |
|
|
What are the clinical features of acute mediastinitis? |
- Fever - Chest pain - Dysphagia (especially with esophageal perforation) - Respiratory distress - Leukocytosis |
|
|
What is the treatment for acute mediastinitis? |
1. Wide drainage 2. Treatment of primary cause 3. Antibiotics |
|
|
What is chronic mediastinitis? |
Mediastinal fibrosis secondary to chronic granulomatous infection |
|
|
What is the most common etiology of chronic mediastinitis? |
Histoplasma capsulatum |
|
|
What are the clinical features of chronic mediastinitis? |
- 50% are asymptomatic - Symptoms are related to compression of adjacent structures: SVC syndrome, bronchial and esophageal strictures, constrictive pericarditis |
|
|
How do you diagnose chronic mediastinitis? |
CXR or CT scan may be helpful, but surgery / biopsy often makes the diagnosis |
|
|
What is the treatment for chronic mediastinitis? |
- Antibiotics - Surgical removal of the granulomas is rarely helpful |
|
|
What is superior vena cava syndrome? |
Obstruction of the superior vena cava, usually by extrinsic compression |
|
|
What is the #1 cause of superior vena cava syndrome? |
- Malignant tumors cause ~90% of cases; lung cancer is by far the most common - Other tumors include thymoma, lymphoma, and Hodgkin's disease |
|
|
What are the clinical manifestations of superior vena cava syndrome? |
1. Blue discoloration and puffiness of the face, arms, and shoulders 2. CNS manifestations may include headache, nausea, vomiting, visual distortion, stupor, and convulsions 3. Cough, hoarseness, and dyspnea |
|
|
What is the treatment for superior vena cava syndrome? |
1. Diuretics and fluid restriction 2. Prompt radiation therapy +/- chemotherapy for any causative cancer |
|
|
What is the prognosis for superior vena cava syndrome? |
SVC obstruction itself is fatal in <5% of cases; mean survival time in patients with malignant obstruction is ~7 months |
|
|
What are the primary functions of the upper and lower esophageal sphincters? |
- UES: swallowing - LES: prevention of reflux |
|
|
The esophageal venous plexus drains inferiorly into the gastric veins. Why is this important? |
Gastric veins are part of the portal venous system; portal HTN can thus be referred to the esophageal veins, leading to varices |
|
|
What type of muscle is in the proximal 1/3 of the esophagus? |
Skeletal muscle |
|
|
What type of muscle is in the middle 1/3 of the esophagus? |
Smooth muscle > skeletal muscle |
|
|
What type of muscle is in the distal 1/3 of the esophagus? |
Smooth muscle |
|
|
What is the blood supply to the proximal 1/3 of the esophagus? |
Inferior thyroid, anterior intercostals |
|
|
What is the blood supply to the middle 1/3 of the esophagus? |
Esophageal arteries, bronchial arteries |
|
|
What is the blood supply to the distal 1/3 of the esophagus? |
Left gastric artery, left inferior phrenic artery |
|
|
What is the length of the esophagus? |
~25 cm in the adult (40 cm from teeth to LES) |
|
|
Why is the esophagus notorious for anastomotic leaks? |
Esophagus has no serosa (same as distal rectum) |
|
|
What nerve runs with the esophagus? |
Vagus nerve |
|
|
What is a Zenker's diverticulum? |
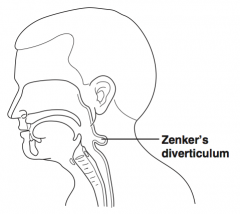
Pharyngoesophageal diverticulum; a false diverticulum containing mucosa and submucosa at the UES at the pharyngoesophageal junction through Killian's triangle |
|
|
What is Zenker's diverticulum's claim to fame? |
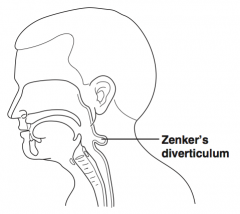
Most common esophageal diverticulum |
|
|
What are the signs/symptoms of Zenker's diverticulum? |
- Dysphagia - Neck mass - Halitosis - Food regurgitation - Heartburn |
|
|
How do you diagnose Zenker's diverticulum? |
Barium swallow |
|
|
What is the treatment for Zenker's diverticulum? |
1. Diverticulectomy 2. Cricopharyngeus myotomy, if >2 cm |
|
|
What is achalasia? |
1. Failure of LES to relax during swallowing 2. Loss of esophageal peristalsis |
|
|
What are the proposed etiologies of achalasia? |
1. Neurologic (ganglionic degeneration of Auerbach's plexus, vagus nerve, or both); possibly infectious in nature 2. Chagas' disease in South America |
|
|
What are the associated long-term conditions with achalasia? |
Esophageal carcinoma secondary to Barrett's esophagus from food stasis |
|
|
What are the symptoms of achalasia? |
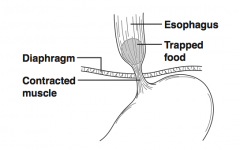
- Dysphagia for both solids and liquids, followed by regurgitation - Dysphagia for liquids is worse |
|
|
What are the diagnostic findings for achalasia? |
- Radiographic contrast studies reveal dilated esophageal body with narrowing inferiorly - Manometry: motility studies reveal increased pressure in the LES and failure of the LES to relax during swallowing |
|
|
What are the treatment options for achalasia? |
1. Balloon dilation of the LES 2. Medical treatment of reflux vs. Belsey Mark IV 270 degree fundoplication (do not perform 360 degree Nissen) 3. Myotomy of lower esophagus and LES |
|
|
What is a diffuse esophageal spasm? |
Strong, non-peristaltic contractions of the esophageal body; sphincter function is usually normal |
|
|
What condition is associated with diffuse esophageal spasm? |
GERD |
|
|
What are the symptoms of diffuse esophageal spasm? |
Spontaneous chest pain that radiates to the back, ears, neck, jaw, or arms |
|
|
What is the differential diagnosis of diffuse esophageal spasm? |
- Angina pectoris - Psychoneurosis - Nutcracker esophagus |
|
|
What are the diagnostic tests associated with diffuse esophageal spasm? |
- Esophageal manometry: motility studies reveal repetitive, high-amplitude contractions with normal sphincter response - Upper GI may be normal, but 50% show segmented spasms or corkscrew esophagus - Endoscopy |
|
|
What is the classic finding of diffuse esophageal spasm on esophageal contrast study (UGI)? |
"Corkscrew esophagus" |
|
|
What is the treatment for diffuse esophageal spasm? |
- Medical (anti-reflux measures, calcium channel blockers, nitrates) - Long esophagomyotomy in refractory cases |
|
|
What is Nutcracker esophagus also known as? |
Hypertensive peristalsis |
|
|
What is Nutcracker esophagus? |
Very strong peristaltic waves, aka hypertensive peristalsis |
|
|
What are the symptoms of Nutcracker esophagus? |
Spontaneous chest pain that radiates to the back, ears, neck, jaw, or arms |
|
|
What is the differential diagnosis of Nutcracker esophagus? |
- Angina pectoris - Psychoneurosis - Diffuse esophageal spasm |
|
|
What are the associated diagnostic tests? |
1. Esophageal manometry: motility studies reveal repetitive, high-amplitude contractions with normal sphincter response 2. Results of UGI may be normal (rule out mass) 3. Endoscopy |
|
|
What is the treatment of Nutcracker esophagus? |
- Medical (anti-reflux measures, calcium channel blockers, nitrates) - Long esophagomyotomy in refractory cases |
|
|
What is esophageal reflux? |
Reflux of gastric contents into the lower esophagus resulting from the decreased function of the LES |
|
|
What are the causes of esophageal reflux? |
1. Decreased LES tone 2. Decreased esophageal motility 3. Hiatal hernia 4. Gastric outlet obstruction 5. NGT |
|
|
What are four conditions / factors associated with esophageal reflux? |
1. Sliding hiatal hernia 2. Tobacco and alcohol 3. Scleroderma 4. Decreased endogenous gastrin production |
|
|
What are the symptoms of esophageal reflux? |
- Substernal pain - Heartburn - Regurgitation - Symptoms are worse when patient is supine and after meals |
|
|
How is the diagnosis of esophageal reflux made? |
1. pH probe in the lower esophagus reveals acid reflux 2. EGD shows esophagitis 3. Manometry reveals decreased LES pressure 4. Barium swallow |
|
|
What is the initial treatment for esophageal reflux? |
- Medical: H2-blockers, antacids, metoclopramide, omeprazole - Elevation fo the head of the bed, small / multiple meals |
|
|
Which four complications of esophageal reflux require surgery? |
1. Failure of medical therapy 2. Esophageal strictures 3. Progressive pulmonary insufficiency secondary to documented nocturnal aspiration 4. Barrett's esophagus |
|
|
What is a "Nissen" surgery? |
360 degree fundoplication: wrap fundus of stomach all the way around the esophagus |
|
|
What is a "Belsey Mark IV" surgery? |
270 degree fundoplication: wrap fundus of stomach, but not all the way around |
|
|
What is a "Hill" surgery? |
Tighten arcuate ligament around esophagus and tack stomach to diaphragm |
|
|
What is a "Lap Nissen" surgery? |
Nissen (360 degree fundoplication: wrap fundus of stomach all the way around the esophagus) via laparoscope |
|
|
What is a "Lap Toupet" surgery? |
Lap fundoplication posteriorly with less than 220-250 degree wrap used with decreased esophageal motility; disadvantage is more post-op reflux |
|
|
What is Barrett's esophagus? |
Replacement of the lower esophageal squamous epithelium with columnar epithelium secondary to reflux |
|
|
Why is Barrett's esophagus significant? |
This lesion is pre-malignant |
|
|
What is the treatment of Barrett's esophagus? |
People with significant reflux should be followed with regular EGDs with biopsies, H2-blockers, and anti-reflux precautions
Many experts believe that patients with severe dysplasia should undergo esophagectomy |
|
|
Which agents may cause esophageal strictures if ingested? |
- Lye - Oven cleaners - Drain cleaners - Batteries - Sodium hydroxide tablets (Clinitest) |
|
|
How do you diagnose caustic esophageal strictures? |
- History - EGD is clearly indicated early on to assess the extent of damage (<24 hours) - Scope to level of severe injury (deep ulcer) only, water soluble contrast study for deep ulcers to rule out perforation |
|
|
What is the initial treatment for caustic esophageal strictures? |
1. NPO / IVF / H2-blockers 2. Do NOT induce emesis 3. Corticosteroids (controversial - probably best for shallow/moderate ulcers), antibiotics (penicillin / gentamicin) for moderate ulcers 4. Antibiotic for deep ulcers 5. Upper GI at 10-14 days |
|
|
What is the treatment of caustic esophageal strictures when stricture develops? |
- Dilation with Maloney dilator / balloon catheter - In severe refractory cases, esophagectomy with colon interposition or gastric pull-up |
|
|
What is the long-term follow-up for caustic esophageal strictures? |
Because of increased risk of esophageal squamous cancer (especially with ulceration), patients endoscopies every other year |
|
|
What is a Maloney dilator? |
Mercury-filled rubber dilator |
|
|
What are the two main types of esophageal carcinoma? |
1. Adenocarcinoma at GE junction 2. Squamous cell carcinoma in most of the esophagus |
|
|
What is the most common histology associated with esophageal carcinoma? |
- Worldwide: squamous cell carcinoma (95%) - USA: adenocarcinoma |
|
|
What is the age and gender distribution of esophageal carcinoma? |
Most common in the 6th decade of life; men predominate, especially black men |
|
|
What are the etiologic factors that contribute to esophageal carcinoma? |
1. Tobacco 2. Alcohol 3. GE reflux 4. Barrett's esophagus 5. Radiation |
|
|
What are the symptoms of esophageal carcinoma? |
- Dysphagia, weight loss - Other symptoms include chest pain, back pain, hoarseness - Symptoms of metastasis |
|
|
What comprises the workup for esophageal carcinoma? |
1. UGI 2. EGD 3. Transesophageal ultrasound (TEU) 4. CT scan of chest / abdomen |
|
|
What is the differential diagnosis of esophageal carcinoma? |
- Leiomyoma - Metastatic tumor - Lymphoma - Benign stricture - Achalasia - Diffuse esophageal spasm - GERD |
|
|
How do you diagnose esophageal carcinoma? |
1. Upper GI localizes tumor 2. EGD obtains biopsy and assesses resectability 3. Full metastatic workup (CXR, bone scan, CT scan, LFTs) |
|
|
What are the characteristics of adenocarcinoma esophageal cancer stage I? |
- Tumor: invades lamina propria, muscularis mucosa, or submucosa - Nodes: negative |
|
|
What are the characteristics of adenocarcinoma esophageal cancer stage IIA? |
- Tumor: invades muscularis propria (grade 3) - Nodes: negative |
|
|
What are the characteristics of adenocarcinoma esophageal cancer stage IIB? |
- Tumor invades up to muscularis propria with positive regional nodes OR - Tumor invades adventitia with negative nodes |
|
|
What are the characteristics of adenocarcinoma esophageal cancer stage III? |
- Tumor invades adventitia with positive regional nodes OR - Tumor invades adjacent structures |
|
|
What are the characteristics of adenocarcinoma esophageal cancer stage IV? |
Distant metastasis |
|
|
What is the treatment for esophageal carcinoma? |
Esophagectomy with gastric pull-up or colon interposition |
|
|
What is an Ivor-Lewis procedure? |
Laparotomy and right thoracotomy with gastro-esophageal anastomosis in the chest after esophagectomy |
|
|
What are the treatment options for esophageal carcinoma with metastatic disease? |
- Chemotherapy and XRT - +/- Dilation - +/- Stent - +/- Laser - +/- Electrocoagulation - +/- Photodynamic laser therapy |
|
|
What is a "blunt esophagectomy"? |
Esophagectomy with "blunt" transhiatal dissection of esophagus from abdomen and gastroesophageal anastomosis in the neck |
|
|
What is the operative mortality rate for esophageal carcinoma? |
~5% |
|
|
Has radiation therapy and/or chemotherapy been shown to decrease mortality for esophageal carcinoma? |
No |
|
|
What is the post-op complication rate of esophageal carcinoma? |
~33% |
|
|
What is the prognosis (5-year survival) for esophageal carcinoma stage I? |
66% |
|
|
What is the prognosis (5-year survival) for esophageal carcinoma stage II? |
25% |
|
|
What is the prognosis (5-year survival) for esophageal carcinoma stage III? |
10% |
|
|
What is the prognosis (5-year survival) for esophageal carcinoma stage IV? |
Basically 0% |

