![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
147 Cards in this Set
- Front
- Back
|
What is upper GI bleeding? |
Bleeding into the lumen of the proximal GI tract, proximal to the ligament of Treitz |
|
|
What are the signs/symptoms of upper GI bleeding? |
- Hematemesis - Melena - Syncope - Shock - Fatigue - Coffee-ground emesis - Hematochezia - Epigastric discomfort / tenderness - Signs of hypovolemia - Guaiac positive stools |
|
|
Why is it possible to have hematochezia with upper GI bleeds? |
Blood is a cathartic and hematochezia usually indicates a vigorous rate of bleeding from UGI source |
|
|
Are stools melenic or melanotic with upper GI bleeding? |
Melenic (melanotic is incorrect) |
|
|
How much blood do you need to have melena? |
>50 cc of blood |
|
|
What are the risk factors for upper GI bleeding? |
- Alcohol - Cigarettes - Liver disease - Burn/trauma - Aspirin / NSAIDs - Vomiting - Sepsis - Steroids - Previous UGI bleeding - Hx of PUD - Esophageal varices - Portal HTN - Splenic vein thrombosis - AAA repair (aortoenteric fistula) |
|
|
What is the most common cause of significant UGI bleeding? |
PUD: duodenal and gastric ulcers (50%) |
|
|
What is the common differential diagnosis of UGI bleeding? |
1. Acute gastritis 2. Duodenal ulcer 3. Esophageal varices 4. Gastric ulcer 5. Esophageal 6. Mallory-Weiss tear |
|
|
What is the uncommon differential diagnosis of UGI bleeding? |
- Gastric cancer - Hemobilia - Duodenal diverticula - Gastric volvulus - Boerhaave's syndrome - Aortoenteric fistula - Paraesophageal hiatal hernia - Epistaxis - NGT irritation - Dieulafoy's ulcer - Angiodysplasia |
|
|
Which diagnostic tests are useful for diagnosing upper GI bleeding? |
- History - NGT aspirate - Abdominal x-ray - Endoscopy (EGD) |
|
|
What is the diagnostic test of choice with UGI bleeding? |
EGD (>95% diagnosis rate) |
|
|
What are the treatment options for upper GI bleeding with an endoscope during EGD? |
- Coagulation - Injection of epinephrine (for vasoconstriction) - Injection of sclerosing agents (varices) - Variceal ligation (banding) |
|
|
Which lab tests should be performed in a patient with upper GI bleeding? |
- Chem 7 - Bilirubin - LFTs - CBC - Type and cross - PT / PTT - Amylase |
|
|
Why is BUN elevated in upper GI bleeding? |
Because of absorption of blood by GI tract |
|
|
What is the initial treatment for upper GI bleeding? |
1. IVFs (16G or larger peripheral IVs x2), Foley catheter (to monitor fluid status) 2. NGT suction (determine rate and amount of blood) 3. Water lavage (use warm H2O - will remove clots) 4. EGD: endoscopy (determine etiology / location of bleeding and possible treatment - coagulate bleeders) |
|
|
Why irrigate in an upper GI bleed? |
To remove the blood clot so you can see the mucosa |
|
|
What test may help identify the site of massive UGI bleeding when EGD fails to diagnose cause and blood continues per NGT? |
Selective mesenteric angiography |
|
|
What are the indications for surgical intervention in UGI bleeding? |
Refractory or recurrent bleeding and site known, >3U of PRBCs to stabilize or >6U PRBCs overall |
|
|
What percentage of patients require surgery for upper GI bleeding? |
~10% |
|
|
What percentage of patients with upper GI bleeding spontaneously stop bleeding? |
~80-85% |
|
|
What is the mortality of acute UGI bleeding? |
- Overall: 10% - 60-80 years of age: 15% - >80 years of age: 25% |
|
|
What are the risk factors for death following UGI bleed? |
- Age older than 60 years - Shock - >5U of PRBC transfusion - Concomintant health problems |
|
|
What is peptic ulcer disease (PUD)? |
Gastric and duodenal ulcers |
|
|
What is the incidence in the US? |
~10% of the population will suffer from PUD during their lifetime |
|
|
What are the possible consequences of PUD? |
- Pain - Hemorrhage - Perforation - Obstruction |
|
|
What percentage of patients with PUD develop bleeding from the ulcer? |
~20% |
|
|
Which bacteria are associated with PUD? |
H. pylori |
|
|
What is the treatment of PUD? |
Treat H. pylori with MOC or ACO
2-week antibiotic regimens: - MOC: Metronidazole, Omeprazole, Clarithromycin - ACO: Ampicillin, Clarithromycin, Omeprazole |
|
|
What is the name of the sign with RLQ pain/peritonitis as a result of succus collecting from a perforated peptic ulcer? |
Valentino's Sign |
|
|
In which age group are duodenal ulcers most common? |
40-65 years of age (younger than patients with gastric ulcer) |
|
|
What is the ratio of male to female patients? |
Men > Women (3:1) |
|
|
What is the most common location? |
Most are within 2 cm of the pylorus in the duodenal bulb |
|
|
What is the classic pain response to food intake? |
Food classically relieves duodenal ulcer pain (Duodenum = Decreased with food) |
|
|
What is the cause of duodenal ulcers? |
Increased production of gastric acid |
|
|
What syndrome must you always think of with a duodenal ulcer? |
Zollinger-Ellison Syndrome |
|
|
What are the associated risk factors of duodenal ulcers? |
- Male gender - Smoking - ASA / NSAIDs - Uremia - Zollinger-Ellison syndrome - H. pylori - Trauma - Burn injury |
|
|
What are the symptoms of duodenal ulcers? |
- Epigastric pain - burning / aching, usually several hours after a meal (food, milk, or antacids initially relieve pain) - Bleeding - Back pain - Nausea, vomiting, anorexia - Decreased appetite |
|
|
What are the signs of duodenal ulcers? |
- Tenderness in epigastric area (possibly) - Guaiac-positive stool - Melena - Hematochezia - Hematemesis |
|
|
What is the differential diagnosis for duodenal ulcers? |
- Acute abdomen - Pancreatitis - Cholecystitis - All causes of UGI bleeding - Zollinger-Ellison syndrome - Gastritis - MI - Gastric ulcer - Reflux |
|
|
How is the diagnosis of duodenal ulcer made? |
- History - Physical exam - EGD - UGI series (if pt is not actively bleeding) |
|
|
When is surgery indicated with a bleeding duodenal ulcer? |
Most surgeons use: >6U PRBC transfusions, >3U PRBCs needed to stabilize, or significant rebleed |
|
|
What EGD finding is associated with rebleeding of duodenal ulcer? |
Visible vessel in the ulcer crater, recent clot, active oozing |
|
|
What is the medical treatment of duodenal ulcers? |
- PPIs or H2 blockers - heal ulcers in 4-6 weeks in most cases - Treat H. pylori if applicable |
|
|
When is surgery indicated for duodenal ulcers? |
"I HOP": - Intractability (hard to control) - Hemorrhage (massive or relentless) - Obstruction (gastric outlet obstruction) - Perforation |
|
|
How is a bleeding duodenal ulcer surgically corrected? |
- Opening of duodenum through the pylorus - Oversewing of the bleeding vessel |
|
|
What artery is involved with bleeding duodenal ulcers? |
Gastroduodenal artery |
|
|
What are the common surgical options for truncal vagotomy? |
Pyloroplasty |
|
|
What are the common surgical options for duodenal perforation? |
- Graham patch (poor candidates, shock, prolonged perforation) - Truncal vagotomy and pyloroplasty incorporating ulcer - Graham patch and highly selective vagotomy - Truncal vagotomy and antrectomy (higher mortality rate, but lowest recurrence rate) |
|
|
What are the common surgical options for duodenal obstruction resulting from duodenal ulcer scarring (gastric outlet obstruction)? |
- Truncal vagotomy, antrectomy, and gastrduodenostomy (BI or BII) - Truncal vagotomy and drainage procedure (gastrojejunostomy) |
|
|
What are the common surgical options for duodenal ulcer intractability? |
- PGV (highly selective vagotomy) - Vagotomy and pyloroplasty - Vagotomy and antrectomy BI or BII (especially if there is a coexistant pyloric / prepyloric ulcer) but associated with a higher mortality |
|
|
Which ulcer operation has the highest ulcer recurrence rate and the lowest dumping syndrome rate? |
Vagotomy and antrectomy |
|
|
Why must you perform a drainage procedure (pyloroplasty, antrectomy) after a truncal vagotomy? |
Pylorus will not open after a truncal vagotomy |
|
|
Which duodenal ulcer operation has the lowest mortality rate? |
- PGV (1/2000 mortality), truncal vagotomy and pyloroplasty (1-2/200), vagotomy and antrectomy (1-2% mortality) - Thus, PGV is the operation of choice for intractable duodenal ulcers with the cost of increased risk of ulcer recurrence |
|
|
What is a "kissing" ulcer? |
Two ulcers, each on opposite sides of the lumen so that they can "kiss" |
|
|
Why may a duodenal rupture be initially painless? |
Fluid can be sterile, with a non-irritating pH of 7.0 initially |
|
|
Why may a perforated duodenal ulcer present as lower quadrant abdominal pain? |
Fluid from stomach/bile drains down paracolic gutters to lower quadrants and causes localized irritation |
|
|
In which age group are gastric ulcers most common? |
- 40-70 years old (older than duodenal ulcer population) - Rare in patients younger than 40 years |
|
|
How does the incidence in men compare to women for gastric ulcers? |
Men > Women |
|
|
Which is more common overall: gastric or duodenal ulcers? |
Duodenal ulcers are more than twice as common as gastric ulcers (think: Duodenal = Double rate) |
|
|
What is the classic pain response to food in patients with gastric ulcers? |
Food classically increases gastric ulcer pain |
|
|
What is the cause of gastric ulcers? |
Decreased cytoprotection or gastric protection (ie, decreased bicarb / mucus) |
|
|
Is gastric acid production high or low in gastric ulcers? |
Gastric acid production is normal or even low! |
|
|
Which gastric ulcers are associated with increased gastric acid? |
- Prepyloric - Pyloric - Coexist with duodenal ulcers |
|
|
What are the associated risk factors for gastric ulcers? |
- Smoking - Alcohol - Burns - Trauma - CNS tumor / trauma - NSAIDs / steroids - Shock - Severe illness - Male gender - Advanced age |
|
|
What are the symptoms of gastric ulcers? |
- Epigastric pain - ± Vomiting, anorexia, and nausea |
|
|
How is the diagnosis of gastric ulcers made? |
- History - Physical exam - EGD with multiple biopsy (looking for gastric cancer) |
|
|
What is the most common location for gastric ulcers? |
~70% are on the lesser curvature ~5% are on the greater curvature |
|
|
When and why should biopsy be performed of a gastric ulcer? |
- With all gastric ulcers, to rule out gastric cancer - If the ulcer does not heal in 6 weeks after medical treatment, rebiopsy (always biopsy in OR also) must be performed |
|
|
What is the medical treatment for gastric ulcers? |
Similar to duodenal ulcers: PPIs or H2 bockers, H. pylori treatment as indicated |
|
|
When do patients with gastric ulcers need to have an EGD? |
1. For diagnosis with biopsies 2. 6 weeks post diagnosis to confirm healing and rule out gastric cancer! |
|
|
What are the indications for surgery for gastric ulcers? |
I CHOP: - Intractability - Cancer (rule out) - Hemorrhage (massive or relentless) - Obstruction (gastric outlet) - Perforation
Note: surgery is indicated if gastric cancer cannot be ruled out |
|
|
What is the common operation for hemorrhage, obstruction, and perforation? |
Distal gastrectomy with excision of the ulcer WITHOUT vagotomy unless there is duodenal disease (ie, BI or BII) |
|
|
What are the options for concomitant duodenal and gastric ulcers? |
Resect (BI, BII) and truncal vagotomy |
|
|
What is a common option for surgical treatment of a pyloric gastric ulcer? |
Truncal vagotomy and antrectomy (ie BI or BII) |
|
|
What is a common option for a poor operative candidate with a perforated gastric ulcer? |
Graham patch |
|
|
What must be performed in every operation for gastric ulcers? |
Biopsy looking for gastric cancer |
|
|
What is a Cushing's ulcer? |
PUD/gastritis associated with neurologic trauma or tumor |
|
|
What is a Curling's ulcer? |
PUD/gastritis associated with a major burn injury (curling iron burn) |
|
|
What is a marginal ulcer? |
Ulcer at the margin of a GI anastomosis |
|
|
What is a Dieulafoy's ulcer? |
Pinpoint gastric mucosal defect bleeding from an underlying vascular malformation |
|
|
What are the symptoms of a perforated peptic ulcer? |
ACUTE onset of upper abdominal pain |
|
|
What causes pain in lower quadrants in patients with a perforated peptic ulcer? |
Passage of perforated fluid along colic gutters |
|
|
What are the signs of a perforated peptic ulcer? |
- Decreased bowel sounds - Tympanic sound over liver (air) - Peritoneal signs - Tender abdomen |
|
|
What are the signs of posterior duodenal erosion / perforation? |
Bleeding from gastroduodenal artery (and possibly acute pancreatitis) |
|
|
What sign indicates anterior duodenal perforation? |
Free air (anterior perforation is more common than posterior) |
|
|
What is the differential diagnosis for a patient you suspect of having a perforated peptic ulcer? |
- Acute pancreatitis - Acute cholecystitis - Perforated acute appendicitis - Colonic diverticulitis - MI - Any perforated viscus |
|
|
Which diagnostic tests are indicated for a patient you suspect of having a perforated peptic ulcer? |
X-ray: free air under diaphragm or in lesser sac in an upright CXR (if upright CXR is not possible, then left lateral decubitus can be performed because air can be seen over the liver and not confused with the gastric bubble) |
|
|
What are the associated lab findings for a patient you suspect of having a perforated peptic ulcer? |
- Leukocytosis - High amylase serum (secondary to absorption into the blood stream from the peritoneum) |
|
|
What is the initial treatment for a patient with perforated peptic ulcer? |
- NPO: NGT (decrease contamination of the peritoneal cavity) - IVF/Foley catheter - Antibiotics/PPIs - Surgery |
|
|
What is a Graham patch? |
Piece of omentum incorporated into the suture closure of perforation |
|
|
What are the surgical options for treatment of a duodenal perforation? |
- Graham patch (open or laparoscopic) - Truncal vagotomy and pyloroplasty incorporating ulcer - Graham patch and highly selective vagotomy |
|
|
What are the surgical options for a perforated gastric ulcer? |
Antrectomy incorporating perforated ulcer, Graham patch or wedge resection in unstable/poor operative candidates |
|
|
What is the significance of hemorrhage and perforation with duodenal ulcer? |
May indicate two ulcers (kissing); posterior is bleeding and anterior is perforated with free air |
|
|
What type of perforated ulcer may present just like acute pancreatitis? |
Posterior perforated duodenal ulcer into the pancreas (ie, epigastric pain radiating to the back; high serum amylase) |
|
|
What is the classic difference between duodenal and gastric ulcer symptoms as related to food ingestion? |
- Duodenal = decreased pain - Gastric = increased pain |
|
|
What is a Graham patch? |
- For treatment of duodenal perforation in poor operative candidates / unstable patients - Place viable omentum over perforation and tack into place with sutures |
|
|
What is a truncal vagotomy? |
Resection of a 1- to 2-cm segment of each vagal trunk as it enters the abdomen on the distal esophagus, decreasing gastric acid secretion |
|
|
What other procedures must be performed along with a truncal vagotomy? |
"Drainage procedure" (pyloroplasty, antrectomy, or gastrojejunostomy), because vagal fibers provide relaxation of the pylorus, and, if you cut them, the pylorus will not open |
|
|
What is a vagotomy and pyloroplasty? |
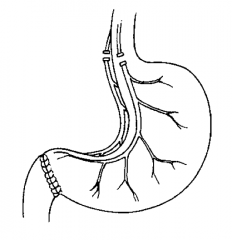
Pyloroplasty performed with vagotomy to compensate for decreased gastric emptying |
|
|
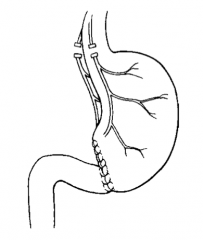
What is a vagotomy and antrectomy? |
Remove antrum and pylorus in addition to vagotomy; reconstruct as a Billroth I or II |
|
|
What is the goal of duodenal ulcer surgery? |
Decrease gastric acid secretion (and fix IHOP) |
|
|
What ist he advantage of proximal gastric vagotomy (highly selective vagotomy)? |
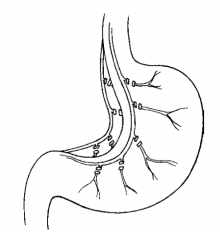
No drainage procedure is needed; vagal fibers to the pylorus are preserved; rate of dumping syndrome is low |
|
|
What is a Billroth I (BI)? |
Truncal vagotomy, antrectomy, and gastroduodenostomy (Think B1 = ONE limb off of the stomach remnant) |
|
|
What are the contraindications for a Billroth I? |
Gastric cancer or suspicion of gastric cancer |
|
|
What is a Billroth II (BII)? |
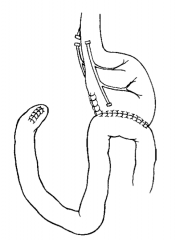
Truncal vagotomy, antrectomy, and gastrojejunostomy (Think BII = TWO limbs off of the stomach remnant) |
|
|
What is the Kocher maneuver? |
Dissect the left lateral peritoneal attachments to the duodenum to allow visualization of posterior duodenum |
|
|
What is stress gastritis? |
Superficial mucosal erosions in the stress patient |
|
|
What are the risk factors for stress gastritis? |
- Sepsis - Intubation - Trauma - Shock - Burn - Brain injury |
|
|
What is the prophylactic treatment for stress gastritis? |
- H2 blockers - PPIs - Antacids - Sucralfate |
|
|
What are the signs/symptoms of stress gastritis? |
NGT blood (usually), painless (usually) |
|
|
How is stress gastritis diagnosed? |
EGD, if bleeding is significant |
|
|
What is the treatment for gastritis? |
LAVAGE out blood clots, give a maximum dose of PPI in a 24-hour IV drip |
|
|
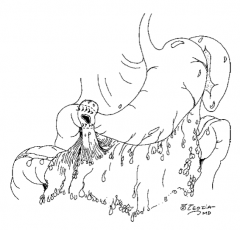
What is Mallory-Weiss Syndrome? |
Post-retching, postemesis longitudinal tear (submucosa and mucosa) of the stomach near the GE junction; approximately 3/4 are in stomach |
|
|
For what percentage of all upper GI bleeds does Mallory-Weiss Syndrome account for? |
~10% |
|
|
What are the causes of the tears in Mallory-Weiss Syndrome? |
Increased gastric pressure, often aggravated by hiatal hernia |
|
|
What are the risk factors for Mallory-Weiss Syndrome? |
- Retching - Alcoholism (50%) - >50% have a hiatal hernia |
|
|
What are the symptoms of Mallory-Weiss Syndrome? |
- Epigastric pain - Thoracic substernal pain - Emesis - Hematemesis |
|
|
What percent of patients with Mallory-Weiss Syndrome will have hematemesis? |
85% |
|
|
How do you diagnose Mallory-Weiss Syndrome? |
EGD |
|
|
What is the classic history for Mallory-Weiss Syndrome? |
Alcoholic patient after binge drinking - first vomit food and gastric contents followed by forceful retching and bloody vomitus |
|
|
What is the treatment for Mallory-Weiss Syndrome? |
Room temperature water lavage (90% of patients stop bleeding), electrocautery, arterial embolization, or surgery for refractory bleeding |
|
|
When is surgery indicated for Mallory-Weiss Syndrome? |
When medical/endoscopic treatment fails (>6U PRBC infused) |
|
|
Can the Sengstaken-Blakemore tamponade balloon be used for treatment of Mallory-Weiss Syndrome tear bleeding? |
No, it makes bleeding worse; use the balloon only for bleeding from esophageal varices |
|
|
What is esophageal variceal bleeding? |
Bleeding from formation of esophageal varices from back up of portal pressure via the coronary vein to the submucosal esophageal venous plexuses secondary to portal hypertension from liver cirrhosis |
|
|
What is the "rule of two thirds" of esophageal variceal hemorrhage? |
2/3 of patients w/ portal HTN develop esophageal varices; 2/3 of patients with esophageal varices will bleed |
|
|
What are the signs/symptoms of esophageal variceal bleeding? |
- Liver disease - Portal HTN - Hematemesis - Caput medusa - Ascites |
|
|
How do you diagnose esophageal variceal bleeding? |
EGD (very important because only 50% of UGI bleeding in patients with known esophageal varices are bleeding from the varices; the other 50% have bleeding from ulcers, etc) |
|
|
What is the acute medial treatment of esophageal variceal bleeding? |
Lower portal pressure with somatostain and vasopressin |
|
|
In the patient with CAD, what must you given in addition to vasopressin to a patient with esophageal variceal bleeding? |
Nitroglycerin, to prevent coronary artery vasoconstriction that may result in an MI |
|
|
What are the treatment options for esophageal variceal bleeding? |
Sclerotherapy or band ligation via endoscope, TIPS, liver transplant |
|
|
What is the Sengstaken-Blakemore balloon? |
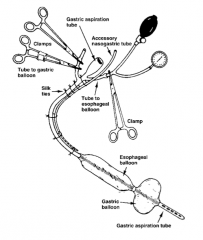
Tamponades with an esophageal balloon and a gastric balloon |
|
|
What is the problem with shunts? |
Decreased portal pressure, but increased encephalopathy |
|
|
What is Boerhaave's Syndrome? |
Post-emetic esophageal rupture |
|
|
Who was Dr. Boerhaave? |
Dutch physician who first described the syndrome in the Dutch Grand Admiral Van Wassenaer in 1724 |
|
|
Why is the esophagus susceptible to perforation and more likely to break down an anastomosis? |
No serosa |
|
|
What is the most common location of Boerhaave's Syndrome? |
Posterolateral aspect of the esophagus (on the left), 3-5 cm above GE junction |
|
|
What is the cause of rupture of the esophagus in Boerhaave's Syndrome? |
Increased intraluminal pressure, usually caused by violent retching and vomiting |
|
|
What is the associated risk factors for Boerhaave's Syndrome? |
Esophageal reflux disease (50%) |
|
|
What are the symptoms of Boerhaave's Syndrome? |
Pain post-emesis (may radiate to the back, dysphagia) |
|
|
What are the signs of Boerhaave's Syndrome? |
- Left pneumothorax - Hamman's sign - Left pleural effusion - Subcutaneous / mediastinal emphysema - Fever - Tachypnea - Tachycardia - Signs of infection by 24 hours - Neck crepitus - Widened mediastinum on CXR |
|
|
What is Mackler's triad? |
1. Emesis 2. Lower chest pain 3. Cervical emphysema (subQ air)
Boerhaave's Syndrome |
|
|
What is Hamman's sign? |
"Mediastinal crunch or clicking" produced by the heart beating against air-filled tissues
Boerhaave's Syndrome |
|
|
How do you diagnose Boerhaave's Syndrome? |
- History - Physical exam - CXR - Esophagram with water-soluble contrast |
|
|
What is the treatment for Boerhaave's Syndrome? |
Surgery within 24 hours to drain the mediastinum and surgically close the perforation and placement of pleural patch; broad-spectrum antibiotics |
|
|
What is the mortality rate for Boerhaave's Syndrome if LESS than 24 hours until surgery for perforated esophagus? |
~15% |
|
|
What is the mortality rate for Boerhaave's Syndrome if MORE than 24 hours until surgery for perforated esophagus? |
~33% |
|
|
Overall, what is the most common cause of esophageal perforation? |
Iatrogenic (most commonly cervical esophagus) |

