![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
PVD (LL Arterial) - Risk factors for atherosclerosis?
|
Major Risk Factors:
1) Smoking 2) DM 3) HTN 4) FHx IHD/CVA 5) Hypercholersterolemia / hLipidemia Minor: 1) Obesity 2) Sedentery lifestyle 3) Hyperhomocysteinemia |
Non Modifiable:
- Age - Sex (men, older women) - FHx |
|
|
PVD (LL Arterial) - Lower limb occlusive disease - Presentation
|
1) Asymptomatic
2) Intermittent claudication 3) Rest pain (critical limb ischaemia) 4) Acute occlusion |
|
|
|
PVD (LL Arterial) - Common Sites of occlusive disease on LL
|
1) Superficial femoral artery (SFA)
2) Aorto-iliac region 3) Popliteal artery |
1) Superficial femoral artery (SFA)
- 15cm below inguinal ligament - Calf pain 2) Aorto-iliac region - Buttock, thigh, calf pain 3) Popliteal artery |
|
|
PVD (LL Arterial) - Difference between intermittent claudication and rest pain?
|
Intermittend Claudication:
WHAT? Cramp like pain WHERE? SFA (=calf pain), iliac A (butt, thigh, calf) WHEN? On ambulation WHAT RELIEVES? Rest OTHER: Claudication distance is usually constant DDx: Neurogenic claudication, sciatica, OA PROGNOSIS: 5% Limb loss @ 5y |
Rest pain (critical limb ischaemia)
WHAT? Pain at rest WHERE? Foot, toes WHEN? At night, at rest WHAT RELIEVES? Hanging foot over side of bed, standing/walking OTHER: Ulceration and gangrene may be present PROGNOSIS: Indicates imminent loss of limb (50%+ amputation) |
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - O/E
|
Look:
1) Skin Atrophy 2) Allopecia 3) Onycholysis 4) Muscle Atrophy 5) Ulceration (toes/feet) 6) Venous guttering Feel: 1) Cool skin 2) Capillary refill >3s 3) Peripheral pulses reduced/absent 4) Buerger's sign Listen: - Auscultate main vessels: Systolic bruit indicates stenosis |
Buerger's sign - eleveation of leg causes pallor
Affected limb regains color more slowly, followed by rubur due to reactive hyperaemia |
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Types of Gangrene
|
1) Gangrene - necrosis due to compromised blood supply
2) Dry gangrene: dry necrosis w/o infection (mummified) 3) Wet gangrene: moist necrotic tissue w/ infection |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Features of Gangrene
|
- Well demarcated
- Patch to entire limb - Gangrene = soft & boggy dead tissue w/ pus @ line of demarcation - Starts distally on toes and extends proximally - Senseless and painless |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Ulceration
|
- Begins in a pressure area on foot
- Dead tissue is present - Granulation tissue absent |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Ix
|
Assess extent of PVD:
1) ABI - SBP ankle:brachial (N=>1, 0.6-0.9=claudication, 0.3-0.6=rest pain) 2) Duplex USS 3) DSA - gold standard but invasive (contrast digital subtraction angiography) Look for a cause: 4) FBC, U&E, lipids, glucose, syphilis |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Performing a DSA - Checklist?
|
1) Allergies to contrast?
2) Medications? 3) Coagulopathies? Correct w/ FFP 4) Peripheral pulses - check and document 5) Baseline studies - PT, aPTT, U&E, FBC 6) Withhold aspirin, warfarin, metformin |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Performing a DSA - Pre, intra, post-procedure?
|
Pre:
1) Shave and prep groin 2) Clear liquids 8h 3) IV fluids Intra: 1) Seldinger technique via femoral or brachial artery Cannula > Guide wire > Catheter Post: 1) Supine 2) Compress wound 3) Distal pulses check |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Performing a DSA - Complications
|
Contrast:
1) Anaphylaxis 2) Nephrotoxicity Vascular access: 1) Bleeding 2) Infection 3) Thromboembolic event 4) AV fistula 5) Perforation 6) Nerve damage 7) Pseudoaneurysm 8) Dissection Tx: Surgery, or amputate |
|
|
|
PVD (LL Arterial) - Lower Limb Ischaemia - Mx
|
Conservative("PACE"):
1) Pentoxifylline (-- blood viscosity) 2) Aspirin 3) Cessation of smoking 4) Exercise Surgical: 1) Angioplasty - balloon +/- stent 2) Endarterectomy - intima and media 'cored out' 3) Bypass graft - Fem-Pop; Fem-distal (peroneal, ant tib, post tib) ** Note Fem=SFA |
|
|
|
Acute limb ischaemia - 5 causes
|
Intraluminal
- Atheroma - Thrombus - Embolis (AF, MI, IE) Vessel wall: - Aneurysm, intimal dissection, AV fistula Extraluminal: - Compartment syndrome - Tumour |
1) Embolization (AF, MI, endocarditis)
2) Thrombosis 3) Atheromatous lesion 4) Aneurysm (aorta, femoral, popliteal) 4) Vascular trauma 5) Compartment syndrome; fracture, circumferential burns |
|
|
Acute Limb Ischaemia - Clinical features
|
P's:
1 (Look)) Pallor 2 (Feel)) Perishing cold 3 (Feel)) Parasthesia 4 (Feel)) Pulse decreased/absent 5 (Feel)) Perishing cold 6 (Move)) Paralysis |
|
|
|
Acute Limb Ischaemia - Ix
|
1) Angiogram
2) ECG 3) USS |
|
|
|
Acute Limb Ischaemia - Emergency Mx
|
1) Heparin bolus + infusion
2) Embolectomy / thrombolysis |
<4-6 hours, otherwise irreversible tissue damage = amputation
1) Anticoagulate w/ IV heparin - Bolus followed by constant infusion (prevents further thrombosis) Definitive Mx: 1) Surgical embolectomy (fogarty baloon catheter) 2) Thrombolysis (tPA) |
|
|
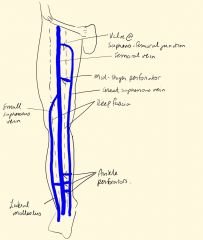
Draw the Lower Limb Venous System
|
|
|
|

What is the lesion? Describe it
|
Venous Ulcer
Site: Gaiter of leg? Size: 10mm? Shape: round Edge: Sloping with new epithelium Base: Clear and pink (granulation tissue) Surrounding tissue: normal |
|
|
|
Leg Ulcers - Types and their locations
|
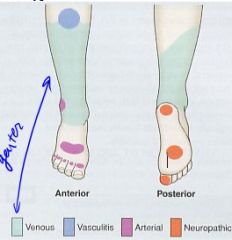
Arterial - Dorsum of foot, tips of toes, lateral malleolus
Venous - Gaiter area, medial side Neuropathic - Weight bearing areas (plantar) Neoplastic - Sun exposed areas |
|
|
|
Leg Ulcers - Edge characteristics
|

Punched out - arterial (indicates rapid death and minimal healing)
Everted - SCC (rapid growth, carcinoma) Rolled - BCC (slow growth, ROdent) Sloping - Venous (indicates healing) |
|
|
|
Leg Ulcers - Describing
|
1) Site (eg. gaiter=venous)
2) Size, shape, color & tenderness 3) Edge 4) Base/floor 5) Depth 6) Discharge 7) Surrounding skin 8) Regional lymph nodes |
1) Site (eg. gaiter=venous)
2) Size, shape, color & tenderness 3) Edge (eg. punched out=arterial) 4) Base/floor - Ischaemic = dry or necrotic eschar - Venous - superficial w/ fibrinous exudate & ooze - Color: Black=necrosis, yellow=sloguh, red=granulation, pink=epithelium 5) Depth (mm, structures involved) 6) Discharge (quantity, type=serous, sanguinous, purulent) 7) Surrounding skin (color, pulses, previous ulcers) 8) Regional lymph nodes (enlargement due to infection or neoplasia) |
|
|
Leg Ulcers - Causes
|
1) Venous (75%)
2) Arterial 3) Neuropathic 4) Traumatic 5) Neoplastic 6) Hematological 7) Infective 8) Misc (pyoderma gangrenosum, insect bites) |
1) Venous (75%) - varicose veins, post-thrombophelbitis
2) Arterial - Ischaemic (DM, therosclerosis, embolism); Vasculitic (Buerger's disease) 3) Neuropathic - DM, EtOH, spinal cord lesion 4) Traumatic - Pressure sores (decubitius) 5) Neoplastic - SCC, BCC, melanoma, Kaposi's sarcoma 6) Hematological -spherocytosis, sickle cell 7) Infective - Mycobacterial, post-cellulitis, chronic infected isius 8) Misc (pyoderma gangrenosum, insect bites) |
|
|
Leg Ulcers - Hx
|
- Onset and duration
- Evolution? - Suspected cause? - Pain - ischaemic=painful, venous=some pain, neuropathic=painless - Bleeding/discharge - PHx: Venous=DVT,PE,varicose veins,previous surgery Arterial=Intermittent claudication,rest pain,CVD Other:DM, RA, Vasculitis, IBD, chronic skin ulcers Medications: B-Blockers,ergotamine,corticosteroids,NSAID SHx - Smoking, EtOH |
|
|
|
Venous vs Arterial vs Neuropathic vs Pressure Ulcers
Hx |
Venous: Chronic
Ischaemic: Intermittent claudication, rest pain, IHD, CVD Neuropathic: DM, EtOH Pressure: Bed bound, immobilized |
|
|
|
Venous vs Arterial vs Neuropathic vs Pressure Ulcers
Site |
Venous: Medial side, gaiter area
Arterial: Dorsum of foot, toes, lateral malleolus Neuropathic: Weight bearing areas (plantar) Pressure Sores: Bony prominences - heels, malleoli, sacrum, hips |
|
|
|
Venous vs Arterial vs Neuropathic vs Pressure Ulcers
Pain |
Venous: Nil to mild
Arterial: Very painful Neuropathic: Painless Pressure: Painful |
|
|
|
Venous vs Arterial vs Neuropathic vs Pressure Ulcers
Ulcer features |
Venous: Depth=superficial; Edge=sloping; Base=granulation; Discharge=Seropurulent; Healing=some
Arterial: Depth=deep; Edge=punched out; Base=grey-yellow slough,dry; Healing=none Neuropathic: Depth=Deep, Edge=Punched out, Base=infected Pressure: Necrotic slough and granulation |
|
|
|
Venous vs Arterial vs Neuropathic vs Pressure Ulcers
Rest of limb |
Sensation/Pulses/Temp/Oedema
Venous: Present / Normal / Hot & tender / Present Arterial: Painful / -- ABI / Cold / Absent Neuropathic: Absent / Bounding / Warm / Absent Pressure: Variable |
|
|
|
Venous vs Arterial vs Neuropathic vs Pressure Ulcers
Other features |
Venous: Varicose veins, lipodermatosclerosis, stasis eczema, atrophie blanch
Arterial: Allopecia, atrophy of skin, onycholysis Neuropathic: Charcot's joints, high arch & clawing of toes Pressure: Erythema at pressure site |
|
|
|
Diabetic Foot
Aetiology and Pathogenesis |
"DAMN"
Diabetes Atherosclerosis Microangiopathy Neuropathy Peripheral neuropathy >> lack of sensation >> trauma to MT and heels >> ischaemia >> pressure ulceration >> angiopathy + infection >> impaired healing |
"DAMN"
Diabetes = Glucose ++ infection Atherosclerosis = Vessel occlusion Microangiopathy = Thickening of BM in arterioles and caps Neuropathy = Sensory, motor, autonomic |
|
|
Diabetic Foot
Sequelae |
Gangrene
Infection Ulceration Deformity - Charcot joints |
|
|
|
Diabetic Foot
Vs Ischaemic |

|
|
|
|
DVT
Risk Factors |
Surgery
Travel OCP Hypercoagulable state Immobility Malignancy |
Prior DVT/PE
Thrombophilia Major medical illness Age >60y |
|
|
DVT
Prevention |
Cease OCP
Early mobilization post-op Aspirin for 3/52 Mechanical support (TED, GCS) Elevate foot Anti-coagulants: - SC Heparin 2hrs pre-op, 7-10d post - High MW: 5000U BD: INR 2-3 - Low MW: enoxaprin 20mg/OD SC - Warfarin |
|
|
|
DVT
Clinical Features |
1) Homan's Sign
2) Calf tenderness 3) Warmth and erythema 4) Swelling of calf and leg 5) Venous distension (superficial) 6) Fever & tachycardia 7) Chest signs: PE / MI |
|
|
|
DVT
How can heparin be administered? What to monitor? |
Administration:
- IV or SC - Unfractionated (heparin) or LMW (enoxaparin) - Monitor aPTT (intrinsic pathway) for unfractionated heparin |
|
|
|
DVT
Unfractionated Heparin |
- 5000-10000U IV lodaing dose
- Continuous infusion @ 1000-2000U/hr - monitor APTT (target 1.5-2.5x normal) - Duration: 5-10d - Contraindications: pregnancy, PUD - Complications: haemorrhage |
|
|
|
DVT
LMW Heparin (enoxaprin, SC) |
- 1 mg/kg BD for >5d
- No need for monitoring |
|
|
|
Varicose Veins
O/E.Inspection |
Look:
- Visible superficial veins (not site, size, course) - Medial = great saphenous vein - Posterior calf = short saphenous vein - Oedema - Venous stasis signs: induration, pigmentation, eczema & ulceration |
|
|
|
Varicose Veins
O/E.Palpation |
- Harvey's Test
- Cough impulse at sapheno-femora & sapheno-popliteal junctions; pulse=incompetent SC valves - Pitting oedema, thickening/tenderness of SC tissues - Tourniquet test - Brodie-Trendelenburg test - Perthe's test - Tap test |
|
|
|
Varicose Veins
Harvey's test |
(Varicose Veins)
2 fingers on vein, slide proximal finger to empty, release distal finger to see which way the empty segment fills |
|
|
|
Varicose Veins
Tourniquet test |
(Varicose Veins)
1) Pt supine, elevate leg 90deg 2) Tourniquet upper 1/3 of thigh 3) Stand pt. If superficial veins above tourniquet RAPID fill = incompetent communicating vein. 4) Move vein distally to locate incompetent valve |
|
|
|
Varicose Veins
Brodie-Trendelenburg test (Tap test) |
(Varicose veins)
- Compress distal segment - Pulse proximal segment - If pulse felt distally = POSITIVE |
|
|
|
Varicose Veins
O/E.Auscultation |
- AV fistulae @ varicose veins produce bruits
|
|
|
|
Varicose Veins
Pathophysiology |
- Superficial to deep
- Pressure of superficial > deep - Calf pump - Incompetent perforator valves = engorged and dilated superficial veins |
- Blood flows superficial to deep
- When calf relaxed: Superficial pressure > Deep pressure - When calf contracted: Blood transmitted PROXIMALLY - Valves prevent retrograde flow - Incompetent PERFORATOR veins cause muscle pump to force blood into the superficial system >> engorgement and dilation |
|
|
Varicose Veins
Aetiology |
- Idiopathic
- Pregnancy (hormones, ++ intrabdo pressure) - Prolonged standing - Pelvic mass - AV fistula - Thrombosis - superficial or deep - Conginetally weak or absent valves (Klippel-Trelaunay syndrome) |
|
|
|
Varicose Veins
Ulceration pathogenesis |
- Hydrostatic pressure in superficial veins impair nutrition to SC and dermis
- Skin breakdown, ulceration, dermatitis |
|
|
|
Varicose Veins
Ix |
- Duplex USS (Gold standard)
- MR Venography - CT - Ambulatory venous pressures (needle measurement device) |
|
|
|
AAA
Aetiology |
1) Atherosclerosis (95%)
2) Degenerative aging 3) Congenital - Marfan's (CT disease) 4) Inflammatory / Infection (Syphillis) 5) FHx/genetic 6) ++ Collagenase/elastase activity 7) Trauma 8) Neoplastic 9) Metabolic / endocrine 10) Dissection |
Atherosclerotic (95%)
Congenital: 1) Marfan's Syndrome 2) Ehlers-Danlos syndrome 3) Behcet's disease Inflammatory 1) Mycotic - bacterial 2) Syphilitic |
|
|
AAA
Ehlers-Danlos syndrome |
CT disorder
|
|
|
|
AAA
Triad indicating emergency surgery for ruptured AAA |
3 P's
1) Pain in the abdomen 2) Pulsatile abdominal mass 3) Pressure low (hypotension) |
|
|
|
AAA
Mx based on sizes |
- 5 cm = threshold for surgery
- Fusiform more likely to rupture than saccular - Comorbidities: HTN, smoking, COPD |
|
|
|
AAA
Growth rates |
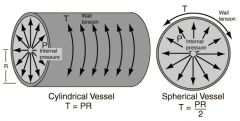
- <5cm = 4%/yr
- 5-7cm = 7%/yr - >7cm = 20%/yr - Larger aneurysms grow faster due to Laplace's law |
|
|
|
Laplace's Law
|
|
|
|
|
AAA
Causes for decrease in UO post AAA repair? |
Pre-renal
- Post-op ADH release - Hypovolemia - Hypotension - 3rd spacing - Pump failure: CCF, cardiogenic shock - Bleeding Intrarenal - Kidney parenchyma dysfunction - Tubular dysfunction: ATN - Glomerular dysfunction: rhabdomyolysis (myoglobinuria) Post-renal - Foley catheter obstruction - Ureteral/urethral injury - BPH - Bladder disfunction - iatrogenic - Calculi |
|
|
|
Carotid Arterial Disease
Significance of a carotid bruit? |
1/3 by stenosis of carotid or vertebral arteries
1/3 radiation from aortic valve 1/3 insignificant Other: Thyroid vessel bruits - Bruit will not always be heard over a significant carotid stenosis |
|
|
|
Carotid Arterial Disease
Ix |
- Carotid Doppler USS
- DSA gold standard - Angiography (risk of thrombus dislodging) - MR angiography - MRI/CT brain - space occupying lesion |
|
|
|
Carotid Arterial Disease
Mx |
General:
- Smoking cessation - Control DM, hyperlipidemia, HTN - Antiplatelet drugs Surgical: - Carotid endarterectomy - remove diseased intima + shunt |
|
|
|
Carotid Arterial Disease
Indications for endarterectomy |
- 70% stenosis +
- Recent TIA - Recovered stroke - amaurosis fugax |
|
|
|
Carotid Arterial Disease
Complications of endarterectomy |
- Bleeding (antiplatelet)
- Nerve damage; hypoglossal (CN12), facial (CN7, tongue deviates to ipsilateral side), Vagus (CN10, voice changes) - Reperfusion syndrome - Restenosis |
|

