![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
349 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
How many days after surgery does myocardial ischemia occur?
|
The highest incidence is w/in 48hrs post-op
|
|
|
|
The following factors have the greatest incidence of pulmonary complications?
|
Abdominal/Thoracic site of surgery -- Pre-existing disease: severity of pulmonary dz; smoking hx w/productive cough; hypercapnia; obesity; advanced age -- Emergency surgery -- Long duration surgery (> 2hrs)
|
|
|
|
What are the 5-W’s IRT post-op fever & their etiologic considerations?
|
Day-1 = Wind = Pulmonary; Day-2 = Water = Urinary; Day-3 = Wound = Surgical site; Day-4 = Walking = Thrombophlebitis (legs/IV site); Day-5 = Wonder drug = Abx, chemo Rx, dilantin, Quinidine, Barb’s
|
|
|
|
What are the different types of surgical infections & incidences?
|
"A. “Clean”- elective, non-traumatic, w/o acute inflammation & is usually closed w/o use of drains. 1) 1%-2% -- 2) tx- close wound B. “Clean-contaminated”- operation on GI, or Resp.tract w/o unusual contamination, or entry into the biliary/urinary tract. Hollow viscous organ opened. 1) 5%-15% 2) tx- close wound C. “Contaminated”- acute inflammation, traumatic wound, GI-tract, spillage, or major break in sterile technique 1) 10%-20%. Stab wound or ruptured appendix 2) tx- leave wound open D. “Dirty”- pus present, perforated viscus (internal organ enclosed
|
|
|
|
What is the clinical presentation of surgical infection?
|
Pyrexia (fever), sweats, chills, induration (the act of hardening), cellulitis, drainage, dehiscence (bursting open of a wound)
|
|
|
|
What is the tx of surgical infections?
|
I & D will treat most post-op infections; Deeper infections req., extensive necrosis, or debridement
|
|
|
|
What are the causes of intra-abdominal abscesses
|
Extrinsic- penetrating trauma & surgery. Intrinsic- perforation of hollow viscus, seeding of bacteria from source outside abdomen, ischemia/infarct of tissue w/in abdomen
|
|
|
|
What are the commonest sites of intra-abdominal abscesses?
|
Subphrenic, Subhepatic spaces, lateral gutters along posterior, peritoneal cavity, pelvis, periappendical, or pericolonic areas
|
|
|
|
What are the s/sx of intra-abdominal abscesses?
|
infection, fever (large spiking T°), leukocytosis
|
|
|
|
What can happen if there is a delay in dx’g intra-abdominal abscess?
|
Pt., may present w/generalized sepsis, or septic hypotension, Post-op abscess usually present as fever the 2nd post-op week, GI-bleeding, pulmonary, renal, or hepatic failure may occur
|
|
|
|
What is the tx for intra-abdominal abscesses?
|
Deep infections need I & D w/irrigation & w/o contaminating the general peritoneal cavity. Pelvic abscesses drained = trans-rectally. Subphrenic abscesses drained = posteriorly through 12th rib approach
|
|
|
|
How is the mortality rate affected in post-op myocardial ischemia?
|
It ’s 32-fold
|
|
|
|
What are the most common post-op pulmonary complications?
|
Atelectasis (collapsed airless lung), Pneumonia, Respiratory Failure, Pulmonary Embolism
|
|
|
|
Which conditions could contribute to a post-op surgical infection?
|
The result of surgery, Any injury/condition req’g surgery, Combo of the prevous 2
|
|
|
|
What perioperative factor has the highest incidence of post-op complications?
|
Abnormal PFT/normal PFT w/incidence of 23/1
|
|
|
|
What are the major issues in regards to pulmonary concerns for the post-op period?
|
Ventilatory function, Bronchial hygiene, Analgesia
|
|
|
|
What are the general measures which may reduce the incidence of pulmonary complications?
|
Early ambulation, Bronchial hygiene, Effective Analgesia
|
|
|
|
What volume of urine is characteristic of acute oliguria?
|
Urine output < 0.5ml/kg/hr, or < 20ml/hr)
|
|
|
|
What is the most common cause of extrinsic “pre-renal" fluid loss post-op?
|
A) External loss (ie- hemorrhage, dehydration, diarrhea) B)Internal loss (ie- 3rd spacing, bowel obstruction, pancreatitis, hematoma)
|
|
|
|
What is best tx for post-op oliguria?
|
Rehydration thru fluid replacements; Fluid challenges: if pt., isn’t volume overloaded give 250-1000cc’s; N.S., or R.L./hr & eval response.(Monitor pt., closely for volume overload)
|
|
|
|
What controls & governs normal peristalsis of the GI-tract?
|
The enteric nervous system
|
|
|
|
What can cause a decrease in normal propulsion of the gut, or post-op ileus?
|
Anesthesia, or surgical manipulation
|
|
|
|
In what order & time frame does the GI-tract return to normal function following abdominal surgery?
|
Small bowel = 24hrs; Stomach = 48hrs; Large bowel = 72hrs *assuming there was no intestinal surgery, or obstruction present.
|
|
|
|
What factors can worsen, or prolong a post-op ileus?
|
Meds (ie- opiates); Electrolyte abnormalities; Inflammatory conditions; Pain
|
|
|
|
What are the classes of mechanical obstruction?
|
Simple-one obstructing point; Strangulated-blood flow reduced; Closed loop-afferent and efferent limbs effected; Intussusception-currant jelly. Polypoid lesion; Perforating
|
|
|
|
What are the causes of mechanical obstruction?
|
Adhesions (most common); Hernias; Intestinal tumors; Intussusception; Volvulus
|
|
|
|
What are the intrinsic causes of mechanical obstruction?
|
Congenital: webs, malrotations, atresias, Crohn’s Dz, Diverticulitis, Ulcerative Colitis, Luminal foreign bodies: bezoars (hair ball), parasites, gallstones
|
|
|
|
What imaging studies can be used to I.D. bowel obstructions?
|
Radiograph “picture frame outline”, Haustral markings-lg intestine, BE may help w/ID obstruction, Endoscopy (judiciously)
|
|
|
|
What are the tx’s for mechanical obstruction?
|
adhesions = surgical lysis, Hernias = reduced & repaired, Intestinal tumors = resection & bypass, Extrinsic / intrinsic lesions = depend on lesion
|
|
|
|
What is a functional obstruction?
|
Intestinal flow blockage resulting from impaired motility (ie-paralytic, or adynamic ileus)
|
|
|
|
How are functional obstructions treated?
|
Observation & fluid/nutritional support,Fluid/electrolyte resuscitation, NG tube, Rectal tube, ID cause, Endoscopy, Cecostomy
|
|
|
|
What does P.E.C.K. stand for?
|
Proteus, E.Coli, Klebsiella
|
|
|
|
What class of abx covers P.E.C.K.?
|
1st Gen Cephalosporins (Kefzol, Cefazolin, Cephalexin, Cefadroxil, Cephalothin, Cephapirin, Cephradine)
|
|
|
|
What does H.E.N.P.E.C.K. stand for?
|
H.Influenza, Enterobacter, N.Gonococci, Proteus, E.Coli, Klebsiella
|
|
|
|
What class of abx covers H.E.N.P.E.C.K.?
|
2nd Gen Cephalosporins: Cefaclor, Cefprozil, Cefonocid, Cefuroxime, Cefotetan, Cefoxitan, Cefmetazole
|
|
|
|
What does C.A.M.P.P.S. stand for?
|
Citrobacter, Actinobacter, Morganella, Pseudomonas, Providencia, Serratia
|
|
|
|
What class of abx covers C.A.M.P.P.S.?
|
3rd Gen Cephalosporins: Cefoperazone, Cefotaxime, Ceftazidimme, Ceftriaxone
|
|
|
|
Which class of drugs is best against Bacteroides?
|
2nd Generation Cephalosporins: Cefaclor, Cefprozil, Cefonocid, Cefuroxime, Cefotetan, Cefoxitan, Cefmetazole
|
|
|
|
Which class of drugs are antipseudomonal?
|
3rd Gen Cephalosporins: Cefoperazone, Cefotaxime, Ceftazidime, Ceftriaxone
|
|
|
|
Which class of drugs has the largest spectrum of coverage for (G-) & (G+) obligages & facultative organisms?
|
Carbapenams; Imipenem, Meropenem
|
|
|
|
What class of abx is used for surgical prophylaxis of a foreign body?
|
1st Gen Cephalosporins: Spefically Kefzol (cheap, readily available & covers most organisms)
|
|
|
|
What is the Drug of Choice (D.O.C.) for a pt., w/a documented anaphylactic rxn to PCN & cephalosporins?
|
Vancomycin
|
|
|
|
What’s the most important consideration for a pre-op bowel prep?
|
Remove all solid waste & most liquid from bowel; Reduce bacterial population in anticipation of procedures / complications of procedures that may contaminate the wound & peritoneal cavity.
|
|
|
|
What organism causes Gas Gangrene?
|
Clostridium
|
|
|
|
If a catheter cultures S.aureus, or the culture is (+) in blood, bile, burns, or UTI, how long should tx be?
|
Full 14 days
|
|
|
|
In a complicated skin infection, what needs to be present?
|
Compromised host; Polymicrobial infection; Septra not drug of choice.
|
|
|
|
What conditions require surgical anti-microbial prophylaxis?
|
High risk pt’s by CDC definition (ASA class 3,4,or 5); Long duration procedure; Clean-contaminated gastric surgery where the gastric acid production has been altered by H2 blockers, GI-bleed, gastric outlet obstruction; Biliary surgery; Colon surgery; Intra-abdominal infection
|
|
|
|
What is an “Acute abdomen”?
|
Undiagnosed abdominal pain, that arises suddenly < 7 days & usually < 48hrs. Greater than 6 hrs surgical signficance
|
|
|
|
IRT acute abdominal pain, how many pt’s will have a “non-surgical” abdomen?
|
2/3’s
|
|
|
|
Of those pt’s req’g surgical intervention for “acute abdominal” pain, what conditions comprise the majority of cases req’s surgery?
|
Acute appendicitis = 42.6%; Acute cholecystectomy = 14.7%
|
|
|
|
What condition is the most common surgical emergency?
|
Acute abdominal pain
|
|
|
|
What condition is the most common non-trauma-related surgical admission?
|
Acute abdominal pain (1%)
|
|
|
|
What key components should be covered in the clinical hx IRT acute abdominal pain?
|
CV, Pulmonary, GU, OB/GYN
|
|
|
|
What coditions comprise the majority of acute abdominal pain conditions for pt’s < 50yrs in the OMGE study?
|
Non-specific abdominal pain (39.5%); Appendicitis (32%)
|
|
|
|
What conditions comprise the majority of acute abdominal pain conditions for pt’s > 50yrs in the OMGE study?
|
Cholecystis (20.9%); Non-specific abdominal pain (15.7%)
|
|
|
|
What components of an abdominal exam should be included for evaluation of acute abdominal pain?
|
Unimanual & bimanual palpation of loins, Determine iliopsoas rigidity, Liver dullness, Free fluid (wave), Thigh rotation test (obturator test)- internal rotation
|
|
|
|
The basic investigative lab studies for evaluation of acute abdominal pain are?
|
CBC, UA, Chem-7, LFT, Amylase & Lipase, Pregnancy test (females)
|
|
|
|
What medical conditions would require an immediate emergent laparotomy?
|
Ruptured AAA, or visceral aneurysm, Ruptured ectopic pregnancy, Hepatic, or splenic rupture, Major blunt, or penetrating abdominal trauma, Hemoperitoneum (bleeding into peritoneal cavity)
|
|
|
|
When would an urgent (w/in 1-2hrs) laparotomy be indicated?
|
Perforated hollow viscus, Appendicitis, Meckel Diverticulitis, Strangulated hernia, Mesenteric ischemia, Ectopic pregnancy(unruptured)
|
|
|
|
What are the indications for an “early”, or “elective” laparotomy (ie- usually w/in 24-48hrs)
|
Uncomplicated acute cholecystitis, Non-strangulated hernia, Needs for resuscitation prior to surgery
|
|
|
|
IRT to a pt., w/an acute abdomen, what is the most important part of the work-up?
|
History and physical
|
|
|
|
When should a pt., be hospitalized if they are (+) for an acute abdomen?
|
There is an extracellular fluid deficit, Electrolyte imbalance, S/sx of sepsis, Unexplained abdominal pain w/o improvement > 24hrs
|
|
|
|
When can a pt. be worked-up as an out-pt.
|
This depends on: Overall condition of pt, PCP capabilities, Hospital distance & capabilities, Pt., reliability & support structures
|
|
|
|
How many pt’s have a work-up for acute abdominal pain as an out-pt?
|
2/3’s
|
|
|
|
What are the considerations for bowel obstruction in pediatrics?
|
Congenital deformities, Intussusception (1st yr of life to 10yrs), Strangulated hernia (most common cause), Adhesions
|
|
|
|
IRT mechanical bowel obstruction, what age of pt., are hernias most common?
|
Pt’s < 35yrs
|
|
|
|
IRT mechanical bowel obstruction, what age of pt., are intestinal tumors most common?
|
Pt’s > 65yrs
|
|
|
|
A tumor on L-side will result in ________________, whereas an obstruction on the R-side will result in ________________.
|
Obstruction, Anemia
|
|
|
|
The clinical findings of a “high/proximal” small bowel obstruction are?
|
Frequent emesis seldom feculent smell, No distention, Intermittent, non-crescendo type pain
|
|
|
|
The clinical findings of a “middle” small bowel obstruction are?
|
Frequent emesis seldom feculent smell, Moderate distention, Intermittent pain, crescendo-colicky type pain w/free intervals
|
|
|
|
The clinical findings of a “low” small bowel obstruction are?
|
Late emesis, feculent smell, Marked distention, Variable pain that may not be classic crescendo type
|
|
|
|
Which type of bowel obstruction has a “jelly-currant” appearance?
|
Intussusception in pediatrics
|
|
|
|
What is the tx of a small bowel obstruction?
|
Depends on underlying etiology, IV-fluids, NG-tube, Correct the cause (if mechanical then surgery)
|
|
|
|
What are the clinical findings in a large bowel obstruction?
|
Constipation/obstipation (no stool), Abdominal distention & sometimes tenderness, Abdominal pain, N/V (late), Characteristic X-ray findings
|
|
|
|
The primary causes of colonic obstruction in adults are?
|
CA of colon 65%; Diverticulitis 20%
|
|
|
|
The ddx for bowel obstruction should include the following?
|
Small vs large bowel, Paralytic ileus, Pseudo-obstruction (Ogilvie’s Syndrome)- massive idiopathic non-obstructive dilation of the colon
|
|
|
|
Which bowel obstruction condition has a palpable “olive” tumor typically located in the midepigastrium to RUQ?
|
Pyloric Stenosis
|
|
|
|
1- Vagotomy & Pyloroplasty
2- Roux-en-Y (Gastrojejunostomy) 3- Gastrojejunostomy 4- Gastroduodenostomy A. 4 B. 3 C. 1 D. 3 E. 1 F. 2 |
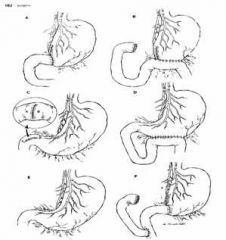
Match the following gastric surgeries with the respective letter.
|
|
|
|
Why should prophylactic Abx only be given for 6-24 hours?
|
Increase risk of superinfection
|
|
|
|
How are prophylactic Abx defined?
|
Abx given 1 hour prior to surgery and no more thatn 24 hr post-op. Cardiac surgery is an exception in which Abx can be given 48 hours prior to surgery
|
|
|
|
What organisms cause abscesses?
|
Staphylococci (S. Aureus, S. epidermidis)
|
|
|
|
What are furuncles and what organism causes them?
|
Thear are cutaneous staph abscesses (boils)
|
|
|
|
Carbuncles are common in what disease population?
|
Diabetics
|
|
|
|
What is hidradenitis suppurative?
|
Infection of apocrine sweat glands in axillary, inguinal and perineal regions.
|
|
|
|
How are cutaneous abscesses treated?
|
1) Drian 2) Irrigate 3) Abx (usually erythromycin or cephalosporin 4) debride
|
|
|
|
What are the signs and symptoms of cellulitis?
|
Redness, edema, pain, fever, leukocytosis. If bacteria enters lymphatics, red streaks develop on extremity
|
|
|
|
What is the causative organism and treatment of cellulitis?
|
1) Streptococcus 2) Penicillin
|
|
|
|
What are the signs and symptoms of necrotizing fasciitis?
|
Hemorrhagia bullae, edema and redness, crepitus usually present although skin may appear normal. Also see fever, tachycardia and foul serrous drainage
|
|
|
|
What organisms are commonly involved in necrotizing fasciitis?
|
Facultative Streptococci, Staphyloccoci
|
|
|
|
What is the treatment for necrotizing fasciitis?
|
Debridement and high doses of clindamycin and an aminoglycoside
|
|
|
|
What organisms cause Fourniers Gangrene?
|
1) E. Coli, Bacteroides, Strep, Staph, Clostridia
|
|
|
|
What characteristics lend themselves to devleoping Gas Gangrene?
|
Severe tissue destruction, areas of impaired blood supply, immunologic in compotence as see in corticosteroid drug therapy
|
|
|
|
What are the clinical presenations of Gas Gangrene?
|
Symptoms start within 48 hours of injury: pain at injury site -- rapid, weak pulse; pale and sweaty; brown serous fluid with foul smell drainind from wound. Crepitus may appear much later.
|
|
|
|
What lab studies should be done for gas gangrene?
|
1) Blood - show falling HCT and rising bilirubin due to hemolysis; 2) Gram Stain - large gram (+) bacilli and numerous RBC but few WBCs 3) X-Ray - may show air in the soft tissues
|
|
|
|
How is gas gangrene treated?
|
A) Debridement and penicillin G (3-4 million units) Q 4 hours plus tentanus prophylaxis
|
|
|
|
When is prophylactic Abx indicated?
|
Gastric CA, achlorhydria, H2 Blockers, Gastic surgery when obstruction, hemorrhage or perforation present, pts over 70, hysterectomy, and elective pulmonary resections (many surgeons use but not demonstrated useful), orthopedic surgery
|
|
|
|
When is prophylactic Abx not indicated?
|
elective gastric surgery; elective cholecystectomy
|
|
|
|
What is the most important factor in decreasing post-op infections?
|
mechanical removal of feces
|
|
|
|
Mechanical bowl prep should be used in all elective bowel surgeries except when this is present?
|
obstruction
|
|
|
|
True or False: Chronic indwelling catheters are usually colonized with bacteria and DO NOT require Abx Tx?
|
True. Unless symptomatic local infection, generalized sepsis or catheter obstruction present
|
|
|
|
Second and third degree burns are prone to this organism and should be Tx with what Abx?
|
Group A Strep. Penicillin G
|
|
|
|
What Abx should be used in human bites?
|
Pencillin
|
|
|
|
What organisms are common to the GI tract?
|
Bacteroides, E.Coli, Enterobacter, Peptostreptococcus, Streptococcus
B.E.E.P.S. |
B-Bacteroides
E- E.Coli E- Enterobacter P- Peptostreptococcus S- Streptococcus |
|
|
Which penicillin is IV only?
|
Penicillin G
|
|
|
|
What organisms does Penicillin treat?
|
pneumococci, meningococci, gonococci, and streptococci
|
|
|
|
What drugs are classified as aminopenicillins and what orgnaisms do they treat?
|
Ampicillin and Amoxicillin. Pneumococci, meningococci, gonococci, streptococci and several Gram (-) bacilli
|
|
|
|
What drugs are classified as antipseudomonal penicillins?
|
Mezlocillin, Piperacillin, Azlocillin
|
|
|
|
What organisms do Kefzol, Cefazolin and Cephalexin treat?
|
PECK (Proteus, E. coli, Klebsiella)
|
|
|
|
Second generation cephalosporins treat what organisms? (Cefotetan, Cefuroxione, Cefoxifin)
|
HENPECK (H. influ, Enterobacter, N. gonococci, Proteus, E. coli, Klebsiella)
|
|
|
|
Which generation Cephalosporin is most effective against Bactorides fragalis?
|
Second generation (cefoxitin)
|
|
|
|
Third generation Cephalosporins treat what organisms (Cefotaxime, Ceftazidime, Ceftriaxone)?
|
CAMPPS (Citrobacter, Actinobacter, Morganella, Pseudomonas, Providencia, Serratia)
|
|
|
|
Which class of Abx has the broadest spectrum of coverage?
|
Carbapenems (Imipenem, Meropenem)
|
|
|
|
What side effects do aminoglycosides have?
|
Ototoxicity and Nephrotoxicity
|
|
|
|
What class of Abx have a cross allergenicity with penicillin?
|
Cephalosporins
|
|
|
|
What Abx is commonly used in surgeries involving mesh, valves, grafts and artificial joints?
|
Kefzol. Use Vancomycin if allergic to pen/chphalo
|
|
|
|
In complicated skin infections (compromised host, polymicrobial) , what drugs can be used?
|
3rd and 4th generation cephalosporins; Augmentin; Unasyn; Timentin; Zosyn; Not Septra
|
|
|
|
What are some physiological effects of anesthesia and surgery?
|
Increased oxygen demand →myocardial ischemia, Atelectasis, pneumonia, hypo/hypertension, major fluid shifts
|
|
|
|
What is the evaluation emphasis in an asymptomatic patient?
|
Functional status, exercise tolerance, cardiopulmonary Si/Sx and bleeding hx
|
|
|
|
What is classified as high risk surgery?
|
emergency, anticipated blood loss, aortic surgery
|
|
|
|
What is classified as intermediate risk surgery?
|
abdominal, head & neck, carotid, orthopedic, prostate
|
|
|
|
What is classified as low risk surgery?
|
breast, cataract, endoscopy
|
|
|
|
What is the management of intermediate risk pts with CAD?
|
stabilize CHF (diuretics), MUGA scan to examine ejection fraction (normal > 55%). Keep all cardiac meds periop period
|
|
|
|
At what blood pressure levels should surgery be delayed?
|
> 180 mmHg systolic; >110 mmHg diastolic
|
|
|
|
How may cc/Kg is normal for Forced Vital Capacity?
|
10
|
|
|
|
What are possible surgical complications secondary to liver disease?
|
hemorrhage, infection, renal failure, encephalopathy, increased mortality
|
|
|
|
What components make up an hematologic evaluations?
|
family Hx, previous surgeries, current meds, sickle cell status, anemia status, PTT, PT, INR
|
|
|
|
What are the components of a neurological evaluation?
|
Neurological Hx, listen to carotids, look in retina for Hollin-Horse plague (white speck in back of retina)
|
|
|
|
When should the use of metformin be discontinued before surgery?
|
1 day prior to surgery. Resume when PO
|
|
|
|
What are risk factors for the development of post-op acute renal failure?
|
aortic surgery, cardiac surgery, PVD, age>70
|
|
|
|
How is acute abdominal pain defined?
|
undiagnosed abdominal pain that arises suddenly and is of less than 7 days (usually less than 48 hours) duration
|
|
|
|
Of those requiring surgical intervention for abdominal pain, what are the top 2 conditions?
|
Acute appendicitis, acute cholecystectomy
|
|
|
|
True or False. Pneumonia can cause upper abdominal pain?
|
True
|
|
|
|
What is the most important part of a acute abdominal pain workup?
|
Hx & PE
|
|
|
|
In what circumstances should radioactive dye not be used?
|
Perforated bowel. Use gastrographin instead
|
|
|
|
When is laparoscopy indicated vs laparotomy?
|
Acute appendicitis and perforated ulcers
|
|
|
|
What laparotomy surgeries are elective?
|
Uncomplicated acute cholecystitis; nonstrangulated hernia; needs for resuscitation prior to surgery
|
|
|
|
When should a patient be hospitalized for an acute abdomen?
|
EC fluid deficit, lytes imbalance, sepsis, unexplained abdominal pain w/o improvement >24 hours
|
|
|
|
What percentage of pts with abdominal pain are non-surgical?
|
2/3
|
|
|
|
Bowel obstruction in pediatric patients is most commonly due to?
|
strangulated hernia
|
|
|
|
Pyloric stenosis is identified by what?
|
olive size lump in epigastric area
|
|
|
|
What produces currant jelly stools?
|
Intussception
|
|
|
|
What is the most common cause of colon obstruction in adults?
|
Colon cancer
|
|
|
|
What are the clinical findings of large bowel obstruction?
|
constipation or obstipation; abdominal distension/pain; N/V (occurs later)
|
|
|
|
What is a Hartman Procedure Colostomy?
|
An end colostomy where the colon is divided. One free end is left in pelvic cavity while the other is brought to outside of body and connected to colostomy bag.
|
|
|
|
What is the no-touch technique in colon surgery?
|
Tie vessels and lymph at pedestal, then tie off bowel, then cut section of bowel to remove.
|
|
|
|
Which type of suture is difficult to work with due to "memory"?
|
Polypropylene (Prolene)
|
|
|
|
What are the principles of would closure?
|
1) close wound in layers 2) match landmarks 3) proper suture placement
|
|
|
|
In suturing, what is "dead space"?
|
Space that occurs when a suture is placed in the skin does not encompass the entire wound.
|
|
|
|
What type of hernia is more common in females?
|
Femoral
|
|
|
|
Which type of hernia is most common?
|
Indirect
|
|
|
|
Which hernia is often congenital related?
|
Indirect & umbilical
|
|
|
|
By what age are congenital hernias repaired?
|
5 years
|
|
|
|
What events can lead to "acquired" hernias?
|
Enlarged foramen; loss of tissue strength and elasticity; trauma; increase in intra-abdominal pressure
|
|
|
|
How can you distinguish between a reducible hernia and strangulated hernia?
|
Strangulated won't reduce when patient lays down; and it is painful
|
|
|
|
What is a sliding hernia?
|
Bowel is adhered to abdominal wall and often becomes strangulated
|
|
|
|
What is a Richter's hernia?
|
Portion of bowel wall incorporated into hernia. If you reduce it, there will be a weak spot in the bowel that can rupture.
|
|
|
|
What are the ventral hernias?
|
Incisional, Epigastric, Umbilical, Spigelian -- occur at lateral borders of rectus muscle where posterior sheath absent
|
|
|
|
List the inguinal hernias?
|
A) Indirect (congenital) B) Direct (acquired) C) Pantaloon (direct and indirect) D) Recurrent E) Femoral
|
|
|
|
In relation to the epigastric vessels where do indirect and direct hernias originate?
|
Indirect - lateral to epigastric; Direct - medial to epigastric
|
|
|
|
Which hernia goes through Hesselbach's triangle?
|
Direct and spigelian
|
|
|
|
Where does femoral hernia lie in relation to the femoral artery and vein?
|
Medial
|
|
|
|
Medial
|
|
|
|
|
What characteristics make a hernia an emergency?
|
Patient has decreased appetite, nausea or emesis
|
|
|
|
What is the preferred laparoscopic repair technique for hernias?
|
TAPP - Transabdominal Preperitoneal
|
|
|
|
Name 2 types of "open repair" techniques for hernias?
|
Bassini & Lichtenstein
|
|
|
|
What is the recurrnece rate for "open repair" hernias?
|
10%
|
|
|
|
Name the types of anesthesia?
|
Local with sedation/analgesic; general; regional
|
|
|
|
Define the American Society of Anesthesiologists (ASA) classifications:
|
Class I - normal healthy; Class II - milde to moderate disease; Class III - severe systemic disease; Class IV - severe disease that is life threatening; Class V - moribund
|
|
|
|
What is another name for "field block" anesthesia?
|
Local
|
|
|
|
What drug is commonly used for a local anesthesia?
|
Lidocaine. 7 mg/Kg is toxic→periorbital numbness
|
|
|
|
Which anesthesia has the least amount of drug for the body to metabolize?
|
Local
|
|
|
|
What sedative and analgesic are commonly used with a local?
|
Sedative - versed; Analgesic - Fentanyl; This combination makes the pt. more comfortable, but can lead to respiratory depression and hypotension
|
|
|
|
Total Intravenous Anesthesia (TIVA) and Inhalation are two types of which kind of anesthesia?
|
General Anesthesia
|
|
|
|
Induction, Maintenance and Emergence are part of what type of anesthesia?
|
General
|
|
|
|
Depolarizers (Curare and Anectine) and Non-Depolarizers are what type of drug class?
|
Muscle relaxant
|
|
|
|
What depolarizer has rapid onset and can trigger bradycardia?
|
Anectine
|
|
|
|
Which drug (Depolarizer or Non-Depolarizer) can trigger malignant hyperthermia?
|
Depolarizer (Anectine) →Use Dantrolene
|
|
|
|
What drug may potentiate Curare (Depolarizer)?
|
Aminoglycoside
|
|
|
|
Which muscle relaxant may be the anesthetic of choice?
|
Propofol
|
|
|
|
What Inhalational Anesthetic is good for kids?
|
Halothane - total anesthesia, amnesia, muscle relaxation
|
|
|
|
A Bier Block is what type of anesthesia?
|
Regional (IV Nerve block for arms)
|
|
|
|
How do regional anesthetics work?
|
Anesthetic deposited in general area - subarachnoid, epidural, axillory sheath or specific neural sheath
|
|
|
|
What is the average onset time and average duration of time for Bupivacaine (Marcaine)?
|
onset = 2-30 minutes
duration = 2-4 hours (avg) = 4-12- per.nrv.blk |
|
|
|
How does the administration of epinephrine with Bopivacaine (Marcain) effect its duration?
|
The vasconstructive action doubles the length of anesthetic
|
|
|
|
As a rough rule, shorter duration drugs have quicker onset times … True or False.
|
TRUE
|
|
|
|
What type of anesthesia would not be used in a hernia repair?
|
Local (field block)
|
|
|
|
What impact does smoking have on blood vessel disease?
|
Increases blood viscosity, fibrinogen, & LDL & decreases HDL and elastin
|
|
|
|
What is "critical arterial stenosis"?
|
Degree of narrowing sufficient to produce pressure drop (cross sectional area of vessel is reduced by more than 75%)
|
|
|
|
What are the 5 P's of Acute Arterial Occlusion?
|
Pain, Palor, Pulselessness, Paralysis, Paresthesia
|
|
|
|
What is the most common cause of chronic arterial occlusion?
|
Atherosclerosis
|
|
|
|
What are the common sites of Chronic Arterial Occlusion?
|
Infrarenal Aorta, Illiac Artery, Superficial femoral Artery
|
|
|
|
How are the gastric neoplasms treated?
|
Surgical excision
|
|
|
|
Which area of the intestinal tract is commonly affected by diverticular disease?
|
Large bowel, esp sigmoid
|
|
|
|
What are the distinguishing clinical features of diverticulosis and diverticulitis?
|
Diverticulosis does not cause pain but does cause bleeding; Diverticulitis causes pain, fever and hypotension
|
|
|
|
How is diverticulosis and diverticulitis diagnosed?
|
Do a colonoscopy on a bleedng diverticulosis and a CT scan for diverticulitis
|
|
|
|
How do you treat diverticulosis and diverticulitis?
|
Bleeding diverticulosis → blood transfusion, surgery if unstable; Diverticulitis → fluids, NPO, Abx
|
|
|
|
What procedure is used to treat complicated diverticulitis?
|
Hartman's Procedure
|
|
|
|
In the Duke classification for colonic neoplasms, what is the survior rate for class C & D?
|
C → 35%; D → < 5%
|
|
|
|
If a person has a family hx of colon cancer, at what age should they begin colonoscopy screening?
|
5 years earlier than the diagnosed age of the family member
|
|
|
|
True or False. The deeper the penetration of the colon tumor, the more severe it is?
|
TRUE
|
|
|
|
What is the clinical presentation of colon cancer?
|
intermittent abdominal pain, guarding, wt. loss, bleeding
|
|
|
|
How can you diagnose colon cancer?
|
DRE and colonoscopy (5% of tumors have tumors someplace else)
|
|
|
|
What are the normal values for carinembryonic antigen (CEA) and how is it used?
|
0-4. Monitor recurrence of cancer
|
|
|
|
How is colonic cancer treated?
|
Polyps are removed endoscopically; if deeper into the tissue → surgical resection
|
|
|
|
What percent of colonic volvulus occurs in the cecum and sigmoid colon?
|
Cecum → 80%; Sigmoid → 20%
|
|
|
|
What is the clinical presenation of colonic volvulus?
|
Abd. Distension, crampy abd. Pain, constipation/obstipation, fever
|
|
|
|
How do you treat colonic volvulus?
|
Sigmoidoscopy and tub placement. Hartman procedure may need to be done, if so → get fluids on board
|
|
|
|
What age range has the greatest risk of appendicitis?
|
8-15 years
|
|
|
|
What are signs/symptoms of appendicitis?
|
Fever, N/V, loss of appetite, McBurney's point tenderness, Psoas/obturator sign, elevated WBC
|
|
|
|
How can you diagnose an appendicitis?
|
Ultrasound
|
|
|
|
How do you treat appendicitis?
|
Fluid resuscitation, Abx (cephalosporin - unperforated) if perforated, give Abx that covers E. coli and Bacteroides. Surgery - Laparoscopic or open
|
|
|
|
True or False. Ulcerative colitis can be cured with surgery?
|
TRUE
|
|
|
|
True or False. Crohn's disease can be cured with surgery?
|
False
|
|
|
|
What are the signs and symptoms of ulcerative colitis?
|
12-30 yr. olds, ulceration of mucosa and submucosa of colon and rectum, bloody diarrhea, wt. loss, pallor, look very sick
|
|
|
|
How do you diagnose ulcerative colitis?
|
R/O other causes of bloody diarrhea, use a flexible sig → exudates on mucosa located in one area WITHOUT skip lesions
|
|
|
|
How do you treat ulcerative colitis?
|
Medications: Sulfasalazine and steroids. Surgery: Total proctocolectomy. If recturm is kept → use sleeve procedure to strip mucosa
|
|
|
|
What are the signs/symptoms of Crohn's Disease?
|
Occurs in both young and old, penetrates entire wall of digestive tract and occurs throughout the entire GI tract (mouth to anus), colick pain. Often develop oxalate stones
|
|
|
|
How do you diagnose Crohn's disease?
|
Colonoscopy and biopsy. Cobblestone appearance of mucosa with skip lesions
|
|
|
|
How do you treat Crohn's disease?
|
Medications: Sulfasalazine and steroids. Surgery just controls it → not a cure
|
|
|
|
Where is the ligament of Treitz located?
|
First part of the jejunum
|
|
|
|
In the case of rectal bleeding, where does dark blood, bright blood, and melena originate respectively?
|
Dark blood = before transverse colon; Bright blood (hematochezia)= left side of colon; Melena = before ligament of Treitz
|
|
|
|
What is the major cause of rectal bleeding in adults?
|
Diverticular disease (60%)
|
|
|
|
During NG aspirate you notice it to be positive for blood where did the blood originate?
|
Above ligament of Treitz
|
|
|
|
Upon examination of NG aspirate you notice no blood but it is positive for bile. What the hell does this mean?
|
>85% chance that there is an upper GI bleed
|
|
|
|
What imging studies would you do for rectal bleeding?
|
Nuclear Scintigraphic, Helical CT, Colonoscopy
|
|
|
|
How do you treat rectal bleeding?
|
Vasopression v doesn't work well in older adults; Surgery → if identify bleed → resect it; → If can't identify bleed → subtotal colectomy with distal ileorectal anastomosis
|
|
|
|
What complications exist with surgery for rectal bleeding?
|
Anastomosis bleeding, mechanical bowel obstruction
|
|
|
|
What type of needle is used in mucosa sugery?
|
Taper
|
|
|
|
What type of suture is used on fascia?
|
Nylon
|
|
|
|
#10 blade is commonly used for what?
|
Emergency procedures
|
|
|
|
A #11 blade is commonly used for what?
|
stabbing → I & D
|
|
|
|
A #15 blade is used for what?
|
Delicate dissection. Look like duck bill
|
|
|
|
A #12 blade is used for what?
|
ENT. It is hooked
|
|
|
|
What does a Poole suction device look like and what is it used for?
|
Disposable type has tube-inside-a-tube within inside tube full of holes. Used to sock fluid from abdomen
|
|
|
|
What does a Yankhouer suction look like and what is it used for?
|
Has suction a the tip and used for oral suctioning
|
|
|
|
True or False. The sterile field in surgery is from your testicles to your chest?
|
False. Table top and up to 2 inches above elbow
|
|
|
|
When changing positions with another person in surgery, how should you maneuver yourself?
|
Pass either facing each other or with backs facing
|
|
|
|
What position in surgery is used for appendectomy?
|
Supine
|
|
|
|
What use is the Trendelenberg position in surgery?
|
Installation of central line
|
|
|
|
What position is used for laparoscopic gall bladder surgery
|
Reverse Trendelenberg
|
|
|
|
What surgery uses the Fowler's and sitting position?
|
Craniotomy
|
|
|
|
What position is used for perineal surgery?
|
Lithotomy position
|
|
|
|
What surgery uses the prone position?
|
Back
|
|
|
|
What position is best for hemorrhoidal surgery?
|
Jacknife or knee to chest
|
|
|
|
To make a flank incision, what position should the patient be in?
|
Lateral
|
|
|
|
Ethibond is what type of suture?
|
Nylon
|
|
|
|
When should you operate on a Fistula?
|
If there is an infection or foreign body
|
|
|
|
How much sodium does the average blue whale need per day?
|
Who gives a shit!!!!
|
|
|
|
How much sodium does the average human need per day?
|
1.2 mEq/kg
|
|
|
|
Sodium chloride contains how many mEg of sodium?
|
154 mEq
|
|
|
|
What is the formula for determining the amount of water needed per day for maintenance?
|
100/50/20; 100 cc per first 10 kg of bwt; 50 cc per 2nd 10 kg of bwt; 20 cc per each kg of bwt beyond 20 kg
|
|
|
|
What information is contained in a preoperative note?
|
Documentation of what procedure is, its consequences and informated consent. Need separate consent for blood (often good for 30 days).
|
|
|
|
What information is found in a post operative note?
|
Procedure performed, findings, who did surgery, blood loss, fluids given, complications, conditions, and patient disposition
|
|
|
|
What is the most common complication of lung, breast or prostate cancer?
|
Spinal cord compression
|
|
|
|
How does spinal cord compression pain differ from benign back pain?
|
Gets worse with recumbent position
|
|
|
|
What physical exam signs exist with spinal cord compression?
|
Percussion directly on spine causes pain, weakness, bowel/bladder incontinence, decreased rectal tone
|
|
|
|
How do you diagnose a spinal cord compression?
|
MRI and myelogram
|
|
|
|
How do you treat a spinal cord compression?
|
Pain control → NSAIDS and Narcotics (Daladid or Morphine). Don't use Demerol → causes seizures; Steroids → give 100mg Decadron before MRI, the 10mg IV qhr x 24 hours; Radiation therapy
|
|
|
|
What causes hypercalcemia in cancer patients?
|
Tumor secretes PTH - related proteins that activate osteoclasts 85% of cases are either primary hyper parathyroidism or tumor
|
|
|
|
What is a normal calcium level?
|
8.5 - 10.5
|
|
|
|
What are some signs/symptoms of hypercalcemia
|
Apathy, fatigue, polyuria, anorexia
|
|
|
|
Most of our calcium is bound to serum albumin. What can cause albumin to be low?
|
Liver mets ↓ albumin, Poor nutrition ↓ albumin
|
|
|
|
True or False. Serum calcium is a good indicator of calcium level in the body?
|
False. A corrected calcium formula that incorporates serum albumin should be used
|
|
|
|
What is the treatment for hypercalcemia?
|
Hydrate (IVF can drop calcium 1.6-2.4 mg/dl); increase renal calcium excretion via Lasix (↑ calcium excretion at ascending loop of Henle by 30%). Start 6 hours after hydration. Do not use in dehydrated patients and avoid thiazides. Inhibit bone resorption (Didronel, Aredia, Calcimar) - add in with lasix. Calcimar acts in couple of hours the others in 2 days; Correct malignancy; Monitor renal, calcium, electrolytes → 2x/dy
|
|
|
|
What type of lung cancer commonly results in superior vena cava syndrome?
|
Small cell or squamous cell
|
|
|
|
What is the etiology of superior vena cava syndrome?
|
Brachiocephalic veins get obstructed compression from mediastinal tumors
|
|
|
|
What are signs/symptoms of superior vena cava syndrome?
|
Dyspnea, cough, neck/face swelling (all get worse with lowering of head), dilated chest wall and neck veins
|
|
|
|
How do you diagnose superior vena cava syndrome?
|
Cinical findings; CXR (mediastinal widening and right hilar mass); CT scan
|
|
|
|
How do you treat superior vena cava syndrome?
|
Need to tissue biopsy first. Then radiation therapy (5000 RADS), chemo
|
|
|
|
When excess formation of thrombin and plasmin exist in the circulation what results?
|
DIC; Thromin to fibrin = clotting; Plasmin breaks down fibrin = bleeding
|
|
|
|
Describe the last part of the coagulation pathway?
|
Prothrombin (FII) → Thrombin (FIIa) → Fibrinogin (FI) → Fibrin
|
|
|
|
What is the treatment for DIC?
|
Treat underlying cause; give heparin and FFP
|
|
|
|
What is the normal range of WBC?
|
5-10,000
|
|
|
|
Leukemia has what WBC count?
|
>100,000
|
|
|
|
What causes tumor lysis syndrome?
|
Rapid cell death from chemotherapy → byproduct overwhelms kidney → kidney failure
|
|
|
|
What lab findings exist with tumor lysis syndrome?
|
↑ BUN and Creatinine; Hyperuricemia (N/V, diarrhea); Hypophosphatemia (combines with calcium and precipitates out in kidneys); Hypocalcemia (muscle cramping); Hyperkalema (Peeked Twave arrythmias)
|
|
|
|
What is the treatment for tumor lysis syndrome?
|
Prevention → Allopurinol 1-2 days before chemo - prevents new uric acid formation; Hydration → 3-4 L/day; Alkalize urine with sodium bicarb - ↓ uric acid precipitation; Monitor electrolytes, BUN, creatinine, calcium, PO4, LDH
|
|
|
|
LDH is a marker for what?
|
cell death
|
|
|
|
Impaired bone marrow function in cancer patients results in what?
|
Neutropenia
|
|
|
|
How is neutropenic fever defined?
|
Fever in a neutropenic patient. Temp greater than 101 (38.3); absolute neutrophil count (ANC) <1000/mm2
|
|
|
|
What is the major cause of neutropenic fever?
|
Infection (60-75%). Tumors can also produce TNF → fever.
|
|
|
|
What is the most common serious infection associated with neutropenic fever?
|
Pneumonia
|
|
|
|
How do you treat neutropenic fever?
|
Abx - high risk patients (active cancer, diabetes) use vancomycin; If think organisms is S. aureus or S. epi use ceftazidime and mono therapy; Two drug therapy → Aminoglycoside and Anti-pseudomonas; If don't respond to Abx → consider candida; Use nupagin → WBC stimulator
|
|
|
|
What factors increase probability to convert from laparoscopic to laparotomy?
|
Acute cholecystitis; >65 years; male; obesity; severe pancreatitis; multiple gall bladder attacks; Thick GB wall
|
|
|
|
What are the risk factors for peripheral atherosclerosis?
|
Male, Advanced Age, HTN, Smoking, Hyperlipidemia, D.M.
|
|
|
|
True or False. Popliteal aneurysm is emergent?
|
TRUE
|
|
|
|
If you suspect AAA, what is the first test to conduct?
|
Dopplar of Abdomen
|
|
|
|
At what centimeter level does risk of AAA increase?
|
>5cm
|
|
|
|
What is the difference between a "leaking" aorta and "ruptured" aorta?
|
Leaking occurs into the aorta vessel layers whereas a rupture spills blood into abdominal cavity.
|
|
|
|
What are the risk factors for AAA?
|
Diastolic HTN, Initial aneurysm size, COPD
|
|
|
|
What percent of a person's body mass is water?
|
60%
|
|
|
|
What percent of a person's body water is found in the intracellular space?
|
40% (↓Na+, ↑K+, ↑Mg+)
|
|
|
|
What percent of a person's body water is found in the extracellular space?
|
20%→15% interstitial (↑Na+, ↓K+, ↓Mg+), 5% plasma
|
|
|
|
For every unit of blood lost, how many units of crystalloid should be used?
|
3
|
|
|
|
How does pH effect K+ levels?
|
High pH drives K+ into cell; low pH displaces K+ out of cell into plasma
|
|
|
|
What are the classes of blood loss?
|
Class I - up to 15%, Class II - 15-30%, Class III - 30-40%, Class IV->40%
|
|
|
|
What are the causes of edema?
|
Decreased oncontic pressure, increased hydrostatic pressure, increased permeability, increased sodium
|
|
|
|
How much fluid do we need per day for maintenance?
|
2000-2400cc/day
|
|
|
|
How much fluid do we need per day when under the stress of trauma?
|
3000cc/day
|
|
|
|
How many grams of glucose in a 1 Liter bag of 5% dextrose?
|
50 grams
|
|
|
|
How many calories are required to prevent the body from self catabolizing?
|
600 calories. This holds true for a couple of days
|
|
|
|
Distinguish between "acute" blood loss and "massive" blood loss.
|
Acute = 1000cc lost; Massive=1500cc lost→need blood transfusion
|
|
|
|
What is normal blood volume?
|
70ml/kg
|
|
|
|
What are the causes of bleeding in surgery?
|
Inadequate surgical hemostasis, Hypothermia, DIC, Circulating Heparin
|
|
|
|
A platelet count under what level will prevent clotting?
|
40,000
|
|
|
|
Spontaneous bleeding may occur at what platelet level?
|
10,000-20,000
|
|
|
|
One unit of platelets contains how many platelets?
|
10,000
|
|
|
|
What is the Hct/Hgb ratio?
|
3:1. One unit of blood raises Hgb 1 gram, so Hct goes up 3%
|
|
|
|
Distinguish "first" intention and "second" intention healing.
|
First (primary) - surgical closure; Second (secondary) - healing from bottom up
|
|
|
|
What is the delayed primary closure?
|
Wait 5-7 days then close.
|
|
|
|
What causes decubitus ulcers?
|
Prolonged pressure that robs tissue of its blood supply
|
|
|
|
What are the principles of treating pressure ulcers?
|
Eliminate pressure, debride, clean and disinfect, dress
|
|
|
|
The most common technical causes of dehiscence are?
|
Infection and Excessively tight sutures
|
|
|
|
Where are arterial ulcers found?
|
Distal ankle at pressure points (toes, heels, ankles). There will be muscle wasting, no pulse, cool to touch, fungal infection of nails, dry skin. May find most comfortable position by dangling limb
|
|
|
|
Where are venous ulcers found?
|
Medial and above ankle. May notice brownish/purple discoloration, edema, varicose veins and stinging pain
|
|
|
|
What type of suture is used on a heart valve?
|
Dacron
|
|
|
|
What type of suture and needle is used for closing skin?
|
Nylon. Cutting needle
|
|
|
|
What type of suture is used on subcutaneous tissue?
|
Dexon
|
|
|
|
When placing mesh inside the body what type of suture is used?
|
Nylon
|
|
|
|
What type of suture is used in infected areas?
|
Absorbable (PDS, Dexon, Vicryl)
|
|
|
|
What type of suture is used for fascia?
|
Nylon
|
|
|
|
What type of suture is used in mucosa?
|
Chromic
|
|
|
|
What type of renal obstruction gives a high circulating sodium and low urine sodium?
|
Post
|
|
|
|
What type of renal obstruction results in high circulating sodium and high urine sodium?
|
Pre-renal
|
|
|
|
How is the diameter (size or gauge) of the suture designated?
|
Descending sequence (heaviest to smallest diameter) 5,4,3,2,1,0, 00,1/0…11/0
|
|
|
|
What type of suture is used in prosthetic grafts?
|
Dacron
|
|
|
|
What are the total absorption days for the following sutures (Fast absorbing, Regular, chromic, PDS)?
|
Fast Absorbing (21-42 days), Regular (70 days), Chromic (60-90 days), PDS (180 days)
|
|
|
|
When would PDS suture use be ideal?
|
Muscle repair
|
|
|
|
What are the risk factors for PUD?
|
Smoking, NSAIDS, H.pylori infection
|
|
|
|
What portion of the stomach are peptic ulcers found?
|
1 inch pre and post pylorus
|
|
|
|
What are common characteristics associated with PUD?
|
Low bicarb secretion in proximal duodenum, increased basal gastric acid secretion, and increased gastric acid secretion with meals.
|
|
|
|
Where do most peptic ulcers perforate?
|
Anterior. Can use omental patch
|
|
|
|
True or False. PUD symptoms are relieved by food?
|
True. Person is often obese
|
|
|
|
How can you diagnose PUD?
|
Endoscopy
|
|
|
|
What is the medical treatment for PUD?
|
H2 receptor antagonist (Zantac & Tagament); PPI; Thermal therapy; Injection therapy
|
|
|
|
How is H.pylori treated?
|
Amoxicillin, Flagyl, PPI
|
|
|
|
What circumstances dictate surgery for PUD?
|
Cancer, bleeding, perforation, obstruction, intractable
|
|
|
|
What are the risk factors for Gastric Ulcer?
|
Smoking, NSAIDS, H.pylori infection
|
|
|
|
True or False. There are 4 classes of gastric ulcer and the first 3 classes result from under production of acid?
|
False. Due to overproduction of acid.
|
|
|
|
True or False. Food makes the symptoms of gastric ulcer worse?
|
TRUE
|
|
|
|
How can you diagnose gastric ulcer?
|
Barium swallow. Use gastrograffin if suspect perforation.
|
|
|
|
How do you treat gastric ulcer?
|
H2 receptor antagonist (Zantac & Tagament); PPI; Thermal therapy; Injection therapy
|
|
|
|
True or False. People with gastric ulcers are usually obese?
|
FALSE
|
|
|
|
What are the 3 common gastric neoplasms?
|
Adenocarcinoma (most common), Gastric Lymphoma, Leiomyosarcoma
|
|
|
|
What are the symptoms of gastric lymphoma?
|
Epigastric, non-radiating pain, wt. loss, fecal occult blood
|
|
|
|
How is gastric lymphoma diagnosed?
|
Endoscopy and CT scan
|
|
|
|
What age group is Leiomyosarcoma commonly seen in?
|
60-70
|
|
|
|
What are the expected lab values for DIC (Platelet, PT, aPTT Firbrinogen, FDP, d-dimer)
|
Platelet <100,000, PT >15 seconds,aPTT >37 seconds,fibrinogen <150mg/dl, FDP >20ug/ml, D-dimer (+)
Normal Values Platelets (150,000-400,000) PT 12-14 sec aPTT (25-38) Fibrinogen (150-350mg/dl) FDP (2-10ug/ml) D-Dimer (negative) |
|
|
|
What are the signs/syms DIC?
|
Petchiae, purpura, hematoma, intracranial bleed, massive bleeding, epistaxis, hematuria.
|
|

