![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Define cellulitis. |
|
|
|
What are the hallmark characteristics of cellulitis? |
Pain |
|
|
What are the most common sites for cellulitis? |
- Lower extremities |
|
|
What are the most common bugs causative of cellulitis? |
- Staphylococcus aureus |
|
|
List risk factors for cellulites. |
|
|
|
Are diabetes, alcohol misuse and smoking risk factors for cellulites? |
- No |
|
|
What is Ludwig’s angina? |
- Cellulitis of the submandibular spaces bilaterally |
|
|
Why is Ludwig’s angina important to recognize? |
- Potential for airway and respiratory compromise as the swelling of the floor of the mouth can cause elevation of the tongue and airway obstruction |
|
|
What is the most common cause of Ludwig’s angina? |
- Local spread of odontogenic infection/oral bacteria (i.e. 2nd and 3rd lower molars) |
|
|
What does fever suggest in the patient with cellulitis? |
- Associated bacteremia |
|
|
List management steps on cellulites. |
- Immobilization, Elevation, Heat or warm moist packs (no evidence) |
|
|
List options for oral therapy for Soft Tissue infections. |
Group A Streptococcus Penicillin V (phenoxymethylpenicillin)250–500 mg qid First-generation cephalosporin250–500 mg qid Erythromycin250–500 mg qid Azithromycin500 mg × 1 dose then 250 mg qd × 4 Clarithromycin500 mg bid
Staphylococcus aureus (not MRSA) Dicloxacillin125–500 mg qid Cloxacillin250–500 mg qid First-generation cephalosporin250–500 mg qid Erythromycin (variable effectiveness)250–500 mg qid Azithromycin500 mg × 1 dose then 250 mg qd × 4 Clarithromycin500 mg bid Clindamycin150–450 mg qid Amoxicillin/clavulanate875/125 mg bid or 500/125 mg tid Ciprofloxacin500 mg bid
Haemophilus influenzae Amoxicillin/clavulanate250–500 mg tid Cefaclor250–500 mg tid Trimethoprim (TMP)/sulfamethoxazole160 mg TMP/800 mg (SMX)SMX bid Azithromycin500 mg × 1 dose then 250 mg qd × 4 Clarithromycin500 mg bid |
|
|
List indications for admission for cellulitis. |
Systemic toxicity/sepsis
Failure of out patient therapy |
|
|
What is the venous drainage of the orbital and periorbital tissues? |
- Venous cavernous sinuses (intracranial) |
|
|
List clinical features of periorbital cellulitis. |
Swelling of the lid |
|
|
What is the most common cause of orbital cellulites? |
- Sinus infection |
|
|
List clinical features that suggest orbital cellulitis. |
- Proptosis |
|
|
What is the diagnostic procedure of choice if concerned about orbital cellulites? |
CT orbits |
|
|
What additional test should be considered in someone with orbital cellulites? |
- Blood cultures |
|
|
What are the treatments for periorbital and orbital cellulites? |
- Periorbital cellulites – Oral antibiotic with close follow up |
|
|
List indications for operative management of orbital cellulites. |
- Failure of IV antibiotics |
|
|
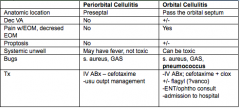
Compare and contrast orbital cellulitis and preseptal cellulitis |
|
|
|
What is erysipelas? |
Acute superficial cellulites with sharply demarcated border surrounding skin that is raised, deeply erythematous, indurated, painful |
|
|
What layers are involved in erysipelas? How do patients with erysipelas appear? |
- Toxic |
|
|
|
S pyogenses S aureus |
|
|
List antibiotics for erysipelas. |
IV Pen G Cephalosporins |
|
|
Compare and contrast erisypelas and cellulitis |
CellulitisErysipelas
Tissue Layers involvedExtends into subQ tissueSuperficial, cutaneous
Physical exam features -Erythema, blanching, flat, poorly demarcated -Indurated, clearly demarcated, raised
Most likely organism Staph aureus GAS
Specific TxPRP (i.e. ancef/keflex)PCN G |
|
|
What is Staphylococcal Scalded Skin Sydrome (Staphylococcal Epidermal Necrolysis)? |
Toxin producing staphylococcus aureus |
|
|
What are is most affected by staphylococcal scalded skin? |
- Children 6 month – 6 years |
|
|
Is there mucus membrane involvement in staph scalded skin? |
- No |
|
|
What is Nikolsky’s sign? |
Easy separation of the outer portion of the epidermis from the basil layer when pressure is applied |
|
|
What is the differential for Staphylococcal scalded skin syndrome? |
Toxic epidermal necrolysis |
|
|
List criteria for the diagnosis of staphylococcal scalded skin syndrome? |
|
|
|
What is the treatment of Staphylococcal scalded skin? |
- Antistaphylococcal penicillinase resistant peniciilin |
|
|
How haemophilus influenzae cellulites present? |
|
|
|
What are drugs for the treatment of Haemophilus cellulites? |
|
|
|
List the criteria for Toxic shock syndrome – this criteria is for staph or strep etiology |
Fever of 38.9° C (102° F) or higher Rash (diffuse macular erythema) that resembles the rash of scarlet fever Desquamation of skin 1 to 2 weeks after onset of disease Hypotension (systolic blood pressure less than 90 mm Hg, orthostatic drop of 15 mm Hg or more, or orthostatic dizziness of syncope) Clinical or laboratory abnormalities in at least three organ systems: Gastrointestinal: nausea and vomiting, diarrhea Muscular: myalgia or creatine phosphokinase at least two times normal level Mucous membrane: vaginal, oropharyngeal, or conjunctival hyperemia Renal: blood urea nitrogen or creatinine level at least twice normal or pyuria greater than five cells per high-power field Hepatic: bilirubin, serum transaminases at least twice normal level Hematologic: thrombocytopenia, <100,000/mm3 Neurologic: disorientation or altered consciousness with-out focal findings
Reasonable evidence for the absence of other cause of illness |
|
|
List criteria for Streptococcal Toxic Shock Syndrome. |
Must meet criteria from both 1 and 2 below: a. A normally sterile site such as blood or cerebrospinal fluid is a definite case. b. A normally nonsterile site such as sputum or skin lesion is a probable case. 2. Hypotension and at least two of the following: a. Renal impairment b. Coagulopathy c. Liver involvement d. Adult respiratory distress syndrome e. Generalized erythematous macular rash that may desquamate f. Soft tissue necrosis such as nec fasc, gangrene, myositis |
|
|
Staph TSS VS strep TSS |
both are caused by an exotoxin |
|
|
|
- Chicken pox |
|
|
What is the treatment of Streptococcal toxic shock syndrome. |
|
|
|
What are the effects of clindamycin in streptococcal toxic shock syndrome. |
|
|
|
What is impetigo? |
Superficial infection of the skin caused by GAS > staphylococcus aureus |
|
|
What are the 2 types of impetigo? |
|
|
|
Can post streptococcal glomerulonephritis follow impetigo? |
- Yes
- No |
|
|
What is a partial DDx for Impetigo? |
|
|
|
List treatments for impetigo? |
- Mupirocin ointment 2% |
|
|
Define abscess. |
|
|
|
List anatomic location common for abscesses. |
Head and neck - Perirectal area |
|
|
When is the loose packing removed? |
- 48 hours (24 hours incosmetically important areas) |
|
|
What is the management of a Bartholin Cyst Abscess? |
I and D and placement of a Word catheter |
|
|
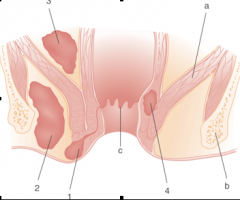
a- Levator ani PerianalI and D in Emergency department IsciorectalAttempted I and D in ED SuprealevatorOR I and D InterspinctericOR I and D |
|
|
Where do pilonidal abscesses occur? |
- Gluteal fold over coccyx |
|
|
What is a Furuncle? |
|
|
|
What is a carbuncle? |
|
|
|
What is hiradenitis suppurativa? |
· Chronic suppurative abscesses in the apocrine sweat glands |
|
|
NECROTIZING FASCIITIS |
|
|
|
List layers of tissue involved in fasciitis. |
|
|
|
List risk factors for fasciitis. |
- Diabetes |
|
|
List treatments for fasciitis? |
- Fluid resuscitation |
|
|
What are the two type of necrotizing fasciitis? |
- Type 1 – Polymicrobial – Nongroup A strep and anaerobes |
|
|
List specific fasciitis syndrome. |
|
|
|
List myonecrosis syndromes. |
|

