![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
126 Cards in this Set
- Front
- Back
|
Most common cause of endocarditis in a native valve |
Strep viridans
|
|
|
most common cause of early (within 60 days of surgery) endocarditis on a prosthetic valve? late (>60 days after surgery) endocarditis?
|
early--> staphylococci (e.g. staph epidermidis- skin bact)
late--> streptococci |
|

Atrial fibrillation
|
irregularly irregular rhythm with absent p waves
|
|
|
most common cause of right sided endocarditis
|
S. aureus (often seen in IV drug users)
|
|
|
complications of endocarditis
|
1. cardiac failure
2. myocardial abscess 3. various solid organ damage from showered emboli 4. glomerulonephritis |
|
|
What should you always suspect in a patient with fever and new onset murmur?
|
endocarditis
|
|
Janeway lesions vs oslers nodes
|
Janeway lesions- painless erythematous lesions on palms and soles-- symptom of endocarditis
Osler's nodes- painful raised lesions on fingers, toes and feet |
|

Roth spots
|
oval, retinal hemorrhages with clear, pale center seen in endocarditis
|
|
|
Is TEE or TTE better in the diagnosis of endocarditis?
|
Transesophageal Echo (TEE)
|
|
|
What should be given to any patient with cardiac valve disease undergoing GI/GU/dental procedures?
|
amoxicillin as endocarditis prophylaxis
|
|
|
Diagnosis of endocarditis (Duke's Criteria)
|
Need 2 Major, 1 major + 3 minor or 5 minor
Major = sustained bacteremia, endocardial involvement (vegetation, abscess, valve perforation) or New onset valve regurgitation Minor = predisposing condition (abnormal valve), fever, vascular phenomena (septic arterial or pulmonary emboli, mycotic aneurysms, Janeway lesions), immune mediate phenomena (glomerulonephritis, oslers nodes, roth spots), positive blood cultures, positive echo |
|
|
Tx for endocarditis
|
IV (parenteral) antibiotics based on culture results for extended periods (4-6 weeks)
If culture negative, but high clinical suspicion, treat empirically with penicillin or vancomycin plus an aminoglycoside (e.g. gentamycin, neomycin etc) until organism can be isolated. |
|
|
4 parts to Tetralogy of Fallot
|
1. Pulmonary Stenosis
2. Right Ventricular Hypertrophy (secondary pulm stenosis) 3. Overriding Aorta 4. Ventricular Septal Defect (VSD) |
|
|
Non-bacterial thrombotic endocarditis (Marantic endocarditis)
|
associated with debilitating disease such as metastatic cancer
- sterile deposits of fibrin and platelets form along the closure line of cardiac valve leaflets - vegetation can embolize to brain or periphery - heparin may be used but NOT proven effective |
|

Nonbacterial Verrucous Endocarditis (Libman Sacks Endocarditis)
1. associations 2. what is it? 3. treatment |
- typically involves the AV valves in individuals with SLE
- characterized by formation of small warty vegetations on BOTH sides of valve leaflets +/- regurgitation murmurs - rarely gives rise to infective endocarditis but can be a source of systemic emboli - Tx: treat underlying SLE + anticoagulation |
|
|
5 congenital cyanotic Heart Diseases
|
early cyanosis- Terrible Ts
1. Truncus Arteriosus- one trunk arising from RV and LV 2. Transposition of Great Vessels- Pulmonary artery and aorta arise from wrong sides of the heart 3. Tricuspid Atresia 4. Tetralogy of Fallot 5. Total Anomalous Pulmonary Venous Connection |
|
|
Atrial Septal Defect
1. most common type 2. pathophysiology |
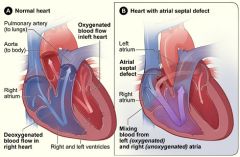
1. ostium secundum- central portion of the septum
2. oxygenated blood from the LA goes thru ASD into RA which leads to increased pulm. blood flow and inc work of right side of heart. As the shunt size inc, RA and RV dilatation occur. Pulm HTN is a serious sequelae, but RARE in ASD |
|
|
Clinical course of ASD
|
Patients are usually asymptomatic until middle age (age 40). thereafter sx may begin-- exercise intolerance, dysnpea on exertion, and fatigue
- if mild patients may have a normal life span |
|
|
Luetic Heart
1. Cause 2. demographic 3. features 4. treatment |
1. complication of syphilitic aortitis-- usually affecting men in the 4th to 5th decade of life.
3. aneurysm of aortic arch with retrograde extension that causes Aortic Regurg plus stenosis of aortic branches 4. IV penicillin and surgical repair |
|
|
Mycotic aneurysm
1. definition 2. Blood Cultures 3. Treatment |
1. aneurysm resulting from damage to the vessel wall secondary to infection
2. Blood cx are positive in most cases 3. IV abx plus surgical excision |
|
|
Acute Arterial Occlusion
1. Pathophysiology 2. Most common site |
1. Acute occlusion is usually caused by an embolus, although rarely from an in situ thrombosis
2. most common site = common femoral artery |
|
|
most common sources of emboli in acute arterial occlusion
|
1. Heart - 85% (Afib is the most common cause, post-MI stasis, endocarditis, myxoma)
2. Aneurysms 3. Atheromatous plaque |
|
|
Clinical Features of Acute Arterial Occlusion
|
6 Ps
1. Pain 2. Pallor 3. Polar 4. Pulselessness (use doppler US to assess) 5. Paresthesia 6. Paralysis |
|
|
Diagnosis of Acute arterial Occlusion
|
1. Arteriogram to define site
2. ECG to look for MI or Afib (sources) 3. Echo to evaluate heart valves, clots, MI |
|
|
Compartment Syndrome
1. definition 2. treatment |
Compression of nerves, blood vessels, muscle etc inside an enclosed space/compartment within the body
tx: fasciotomy to relieve pressure |
|
|
Treatment of Acute Arterial Occlusion
1. main goal 2. how long can skeletal muscle survive without perfusion? 3. What if there is paralysis or paresthesia? |

Immediate anticoagulation with IV Heparin and emergent embolectomy via cutdown or fogarty balloon-- if this fails then bypass. Treat compartment syndrome as necessary
1. main goal it to assess viability of tissues and salvage the limb 2. skeletal muscle can tolerate 6 hours of ischemia- perfusion should be re-established within this time 3. if paralysis or paresthesia are present then amputation is probably necessary |
|
|
Treatment of Rheumatic Fever
1. prevention 2. acute treatment 3. pts with h/o RF 4. rheumatic heart dz |
1. Treat strep pharyngitis with penicillin or erythromycin (if pen allergy) to prevent it
2. Acute Rheumatic Fever = NSAIDs 3. pts with h/o RF should get abx before all GI/GU/dental procedures-- amoxicillin or erythromycin 4. treat valvular disease as indicated |
|
|
Diagnosis of Acute Rheumatic Fever
|

Jones criteria: 2 major, 1 major and 2 minor
Major 1. Migratory polyarthritis 2. Eyrthema marginatum- pink rings on the trunk that come and go 3. cardiac involvement- pericarditis, CHF, valve disease 4. subQ nodules- Aschoff nodules 5. chorea Minor 1. fever 2. inc ESR 3. polyarthralgias 4. h/o s. pyogenes infection (positive ASO titer -antistreptolysin O antibodies) 5. h/o rheumatic fever 6. prolonged PR |
|
|
Causes of hypertensive emergency
|
1. Medication non-compliance
2. cocaine, LSD, methamphetamine 3. Alcohol withdrawal 4. hyperaldosteronism- inc aldo --> inc reabsorption of sodium and water, inc secretion of K+ 5. Cushings syndrome- inc cortisol secretion 6. eclampsia- seizure in pre-eclampsia 7. vasculitis 8. pheochromocytoma 9. Non-compliance with dialysis |
|
|
Treatment of aortic dissection
1. Medical for all 2. Type A vs Type B |
Initiate medical treatment- IV Beta blockers to decrease HR and force of LV Ejection, Nitropusside or Nitroglycerin to decrease blood pressure to below 120 mmHg
2. For Type A (proximal aorta dissections) - surgery is indicated as cardiac tamponade may develop For Type B (distal dissections)- medical management only unless pt is unstable |
|
|
Best Tests for Aortic Dissection
1. stable pt 2. unstable pt |
1. TEE and CT
2. TEE at the bedside |
|
|
Aortic Dissection
1. definition 2. types-- Stanford |
1. tear in the inner wall of the aorta causes blood to flow between vessel/intimal wall layers, forcing them apart
2. Type A- involves ascending aorta +/- arch- may spread retrograde into heart--> tamponade Type B- involves descending aorta or arch |
|
|
Hypertensive Emergency Treatment
1. over 1st 1-2 hours 2. if severe? (how do you define severe?) 3. if less immediate danger? |
1. reduce MAP by 25% in the 1st 1-2 hours. The goal is NOT immediately to achieve normal BP, but to get the patient out of danger and then gradually reduce it
2. if SEVERE (DBP > 130 mmHg) or hypertensive encephalopathy --> IV agents such as nitroglycerin, nitroprusside, or labetalol (alpha and beta antagonist) are appropriate 3. If in less immediate danger - oral agents such as captopril, clonidine, labetalol, or diazoxide |
|
|
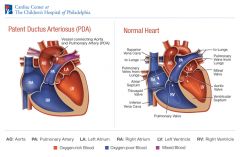
Clinical features of Patent Ductus Arteriosus (PDA)
|
1. Maybe asx
2. signs of HF 3. loud P2- sign of pulm HTN 4. LVH ( L--> R shunt)--> Left heart has to pump against increased PVR 5. continuous machinery murmur at 2nd ICS (both systolic and diastolic) 6. Wide Pulse pressure (SBP-DBP) 7. Differential cyanosis- lower extremity clubbing- toes are more likely to be cyanotic than fingers |
|
|
Complications of VSD
|
1. Heart Failure
2. Endocarditis 3. Progressive Aortic Regurgitation 4. pulm HTN and shunt reversal (R-->L) = Eisenmenger's syndrome |
|
|
Symptoms of hypertensive emergency
|
severe headache, visual disturbances, and altered mental status (AMS)
|
|
|
Complications of aortic coarctation
|
1. Severe HTN
2. rupture of cerebral aneurysms (inc flow/pressure above coarctation) 3. infective endocarditis 4. aortic dissection |
|
|
Treatment of PDA
1. if pulm HTN absent 2. if PHTN present or R--> L shunt |
1. surgical ligation if there is NO PHTN
2. if severe PHTN or R-->L shunt do not correct PDA-- this is a contraindication |
|
|
What are the leading causes of death in adults with a PDA (2)?
|
Heart failure and infective endocarditis
|
|
|
What is PDA associated with (3)?
|
Congenital rubella syndrome
High altitude Premature births |
|
|
Treatment of VSD
1. when indicated 2. what needs to be given as ppx 3. for asx pts with a small defect? |
1. surgical repair when pulmonary to systemic blood flow ratio is greater than 1.5:1 or 2:1 (same as with ASD)
2. endocarditis prophylaxis (amoxicillin, or erythromycin if allergy) 3. surgery is not indicated |
|
|
Non-cyanotic congenital heart diseases (4)
|
1. ASD
2. VSD 3. PDA 4. Coarctation of the Aorta - narrowing of the aorta |
|
|
Signs of VSD
1. type of murmur 2. what happens to murmur with valsalva 3. other sx 4. what happens to pulm component of S2 as Pulmonary Vascular Resistance inc? 5. What causes AR when a VSD is present? |
1. harsh, blowing holosystolic murmur with thrill (blood crossing VSD)-- the smaller the defect, the louder the murmur
2. murmur decreases with valsalva and handgrip (decreased return of blood to heart- decreased preload) 3. sternal lift from RV enlargement 4. As PVR increases the pulm component of s2 increases in intensity 5. Aortic Regurgitation- flow through VSD creates low pressure zone leading to AV prolapse by venturi effect |
|
|
Clinical features of superficial thrombophlebitis vs chronic venous insufficiency vs DVT
|
superficial thrombophlebitis- local tenderness and erythema along course of superficial vein
CVI- aching of lower extremities worse at end of day, relieved by elevation of the lefts and worsened by recumbency. May see edema, pigmentation and ulcers DVT- usually asymptomatic, but may calf pain, and unilateral swelling |
|
|
Diagnosis of superficial thrombophlebitis vs chronic venous insufficiency vs DVT
|
superficial thrombophlebitis- clinical dx
CVI- clinical dx DVT- duplex US, D-Dimer to r/o |
|
|
Treatment of superficial thrombophlebitis vs chronic venous insufficiency vs DVT
|
superficial thrombophlebitis- analgesics, monitor for spread or cellulitis
CVI- leg elevation, avoid long periods of standing, elastic stockings, and if ulcers present then Unna boot and wet to dry dressings DVT- anticoagulation |
|
|
Systemic Inflammatory Response Syndrome (SIRS)
1. criteria 2. sepsis 3. septic shock 4. multi-organ dysfunction syndrome (MODS) |
Characterized by 2 or more of the following
Temperature >38 or <36 C (fever or hypothermia) HR >100 or <60 bpm hyperventilation (rate >20 bpm or PaCO2 > 32 mmHg) tachycardia (HR >90 bpm) inc WBC count (>12,000 cell/hpf) or dec WBC count (<4,000 cell/hpf) or >10% band form (immature cells) Sepsis- when blood cultures are positive + SIRS (two sets of blood cultures must be taken from two sites before abx are given) Septic shock- decreased blood pressure due to sepsis despite fluid resuscitation Multiorgan dysfunction syndrome- usually leads to death |
|
|
What is the most common primary cardiac neoplasm?
|
atrial myxoma
|
|
|
Atrial myxoma
1. definition 2. benign or malignant? 3. complications 4. causes 5. protypical presentation 6. tx |

1. benign gelatinous growth that is usually pedunculated and usually arising from the interatrial septum in the region of the fossa ovalis
2. benign 3. can embolize leading to metastatic disease or can cause relative valvular dynfunction 4. most are sporadic put some autosomal dominant cases have been reported 5. fatigue, fever, syncope, palpitations, malaise, low pitched diastolic murmur that changes with body position (diastolic plop) 6. tx- surgical excision |
|
|
patient presents with fatigue, fever, syncope, palpitations, and malaise. On exam you hear a low pitched diastolic murmur that changes with body position. What do they most likely have?
|

Atrial myxoma- benign primary cardiac tumor
|
|
|
General characteristics of cardiac neoplasms
1. primary vs metastatic more likely? 2. if metastatic where are the most likely primaries? |
1. primary cardiac neoplasms are rare, 75% are from mets
2. sites of primaries = lungs, breast, skin, kidney, lymphomas, kaposi's sarcoma (HHV-8) in AIDS pts |
|
|
Treatment of neurogenic shock
|
1. judicious use of IV Fluids = mainstay
2. vasoconstrictors but be cautious 3. put patient supine or in trendelenburg position (head down) 4. maintain body temp |
|
|
Clinical features of neurogenic shock
- skin - Urine output - HR and BP? - CO, SVR and PCWP |
- warm, well perfused skin (vasodilation)
- decrease urine output or nl - decreased HR and BP (but can be tachy) - C.O. is nl to decreased, dec SVR, PCWP is nl to decreased |
|
|
Neurogenic shock- general characteristics
1. mechanism 2. causes |
failure of the sympathetic nervous system to maintain adequate vascular tone (sympathetic denervation leading to decreased epi and norepi)
- causes include spinal cord injury, severe head injury, spinal anesthesia, pharmacologic sympathetic blockade - characterized by peripheral vasodilation with dec SVR - dec CO, SVR, and PCWP |
|
|
Definition of cardiogenic shock
1. SBP and Urine output criteria |
SBP <90mmHg and urine output <20 cc/hr with adequate LV filling pressure
|
|
|
What is the most common cause of death in the ICU?
|
septic shock
|
|
|
1. diagnosis of septic shock
2. treatment of septic shock |
1. clinical diagnosis, confirmed by blood culture but blood cultures are commonly negative
2. IV antibiotics broad spectrum at max doses, surgical drainage if necessary (depending on source of infection), fluids to inc BP, pressors if BP remains low despite aggressive fluid fluids (1st dopamine, 2nd norepi) |
|
|
Clinical features of septic shock
1. skin |
- manifestations related to the cause of sepsis (pneumonia, UTI, peritonitis etc)
- signs of SIRS - dec BP, oliguria, lactic acidosis - fever or hypothermia - hypothermia is more common in the very young, elderly or debilitated or ICH- don't have immune response that leads to the fever |
|
|
Septic shock
1. definition 2. causes 3. progression 4. presentation 5. complications |
1. decreased BP induced by sepsis that persists despite adequate fluid resuscitation
2. causes- pneumonia, pyelonephritis, meninigitis, abscess, cholangitis, cellulitis, peritonitis 3. Progression- SIRS --> sepsis--> septic shock --> multiorgan dysfunction 4. Severe decrease in SVR secondary to peripheral vasodilation, nl to increased C.O. (due to inc HR and maintained SV), warm extremities, dec EF secondary to decreased contractility 5. complications- ARDS, acute tubular necrosis (ATN), Disseminated Intravascular Coagulopathy (DIC)--form a bunch of clots then start hemorrhaging because you have used up all your clotting factors, multi-organ failure, death |
|
|
Treatment of hypovolemic shock
|
1. Airway and Breathing- pts in severe shock and circulatory collapse generally require intubation and mechanical ventilation
2. Circulation- if hemorrhage- apply direct pressure +/- transfusion. IV hydration - pts with class I usually do not require IV fluids, class II benefits, and class III and IV require fluid resuscitation. Give fluid bolus and continuous infusion and then reassess 3. For non-hemorrhagic shock- do not transfuse. Crystalloids with electrolyte replacement is adequate |
|
|
What is the only type of shock where PCWP/LA filling pressure is increased?
|
cardiogenic shock
|
|
|
Clinical features of cardiogenic shock
|
1. Altered mental status (AMS)
2. dec BP 3. inc HR 4. engorged neck veins (JVD) - inc venous pressure 5. pulmonary congestion (LVF) |
|
|
Cardiogenic shock
1. general characteristics 2. causes |
1. occurs when the heart is unable to generate enough C.O. to maintain tissue perfusion. Defined as SBP< 90 mmHg with urine output <20 cc/hr + adequate PCWP/LA filling pressure
2. After acute MI - most common cause - cardiac tamponade (compression of the heart) - tension pneumothorax (compression of the heart) - arrhythmias - massive PE --> RVF - myocardial disease (cardiomyopathies, myocarditis) |
|
|
What is the most effective method of monitoring response to treatment in hypovolemic shock?
|
measuring urinary output (UOP)
- also helpful are pulmonary catheter +/- central line |
|
|
Hypovolemic shock
1. general characteristics 2. causes |
1. Primary pathophysiology- dec effective circulatory volume (ECV) leads to dec preload and dec CO
2. Rate of volume loss is important- the slower the loss then the greater the compensatory mechanisms 3. patients with signs of medical commorbidities (esp cardiac) may be unable to compensate physiologically 4. there are 4 classes depending on the severity of the volume loss 5. causes - hemorrhage- trauma, GI bleed, retroperitoneal - non-hemorrhagic- lots of vomiting, severe dehydration, severe diarrhea, burns, 3rd spacing in bowel obstruction |
|
|
Treatment of the cardiogenic shock
|
1. ABCs- airway, breathing and circulation
2. Identify and treat underlying cause a. Acute MI- MONAH (standard), Aggressive revascularization with PTCA or CABG b. tamponade- periocardiocentesis/surgery c. surgery for valve issues d. treat arrythmias 3. Vasopressors - dopamine = 1st, dopamine and dobutamine = 2nd, Norepi and epi if severe 4. Afterload reduction - Nitroglycerin or Nitroprusside- not usually indicated because they exacerbate hypotension but may be used later with vasopressor 5. IV fluids are likely harmful because of elevated LV pressures. Patients may actually need diuretics 6. Intra-aortic balloon pump (IABP) - dec afterload, inc CO, dec myocardial demand |
|
|
Diagnosis of cardiogenic shock
|
1. ECG- ST elevation or arrythmia
2. Echo- mechanical compression of heart, valve disease, estimate EF, pericardial effusion 3. Hemodynamic monitoring-- Swan Ganz catheter (pulm artery catheter) to measure PCWP, PA pressure, CO, Cardiac Index, SVR, keep CO > 4 L/min (nl = 5 L/min), Cardiac Index > 2.2, and PCWP < 18 mmHg |
|
|
Surgical Treatment for peripheral vascular disease (PVD)
1. indications 2. methods |
1. rest pain, ischemic ulcerations (tissue necrosis), severe symptoms refractory to conservative treatment
2. options = surgical bypass graft is most common and has a 5 yr patency of 70% or angioplasty |
|
|
Causes of Abdominal Aortic Aneursym
|
MULTIFACTORIAL- most cases = atherosclerotic weakening of the aortic wall
- Predisposing factors = trauma, HTN, vasculitis, smoking, and a positive family history - syphilis + connective tissue abnormalities (E.g. Marfans, Ehler's Danlos) are associated with thoracic aneurysms but they may involve the lower aorta as well |
|
|
Rupture of AAA
1. triad of findings 2. Other symptoms |
1. Abdominal pain, hypotension, palpable pulsatile mass - ruptured AAA --> emergent laporotomy with further diagnostic tests
2. circulatory collapse, syncope, pre-syncope secondary to sudden hemorrhage, n/v |
|
|
Treatment of unruptured AAA vs ruptured AAA
- what is the normal size/diameter of the infrarenal Aorta? |
1. unruptured AAA- depends on the size. If the diameter > 5 cm or symptomatic then operate (synthetic graft). If asymptomatic and <5 cm diameter, treatment is controversial, but periodic imaging is recommended to F/U growth (NO SAFE SIZE EXISTS)
- consider life expectancy of patients vs risk of surgery and lengthy recovery 2. ruptured-- emergery laporotomy 3. nl = 2 cm |
|
|
Peripheral Vascular Disease (PVD)
1. definition 2. typical patients 3. sites of occlusion/stenosis |
1. PVD = atherosclerotic disease of the lower extremities
2. patients with PVD usually have co-existing CAD (with CHF, or h/o MI etc) plus other chronic medical problems like diabetes or lung disease 3. most common site is the superficial femoral artery (in Hunter's canal), popliteal artery, aortoiliac occlusive disease |
|
|
Prognosis of peripheral vascular disease (PVD)
|
1. If the patient has intermittent claudication- good prognosis
2. patients with rest pain or ischemic ulcers have the worst prognosis (especially if they are diabetic or are smokers) |
|
|
Treatment of Peripheral Vascular Disease (PVD)
|
- Diabetics have an amputation rate 4x higher than others
- Conservative management for intermittent claudication includes: 1) smoking cessation- cannot be over-emphasized), 2) graduated exercise program (walk to point of claudication, rest then continue), 3) foot care (especially in diabetics), 4) Atherosclerotic RF reduction (dec HLP, HTN, weight, and improve glycemic control), 5) avoid extremes of temperature (esp extreme cold), 6) aspirin, 7) Trental (pentoxyfylline)- lowers blood viscosity |
|
|
Diagnosis of Peripheral Vascular Disease
1. most common 2. other 3. gold standard |
1. Ankle-Brachial Index (ABI) - ratio of SBP at ankle vs arm (nl >/= 1.0, claudication ABI < 0.7, Rest pain ABI < 0.4)
2. pulse volume recordings - excellent assessment of segmental perfusion/non-invasive using pressure cuffs 3. gold standard - arteriography - contrast in vessels + radiographs- helps locate PVD- only needed if surgery/revascularization is being considered |
|
|
1. What is a normal ABI?
2. when does claudication begin (what ABI)? 3. When does rest pain begin (what ABI)? |
1. > 1.0 mmHg
2. <0.7 mmHg 3. < 0.4 mmHg ABI = ankle-branchial index = SBP in ankle/SBP in arm (brachial artery) |
|
|
Signs of peripheral vascular disease (PVD) on physical exam
|
1. dec or absent pulses
2. muscular atrophy 3. dec hair growth 4. thick toenails 5. dec skin temp 6. ischemic ulceration (usually on toes)- localized skin necrosis secondary to trauma that does NOT heal 7. tissue infarction/gangrene (end stage disease) 8. pallor of elevation and rubor of dependency |
|
|
Diagnosis of Atrial Septal Defect
|
1. Transesophageal Echo is diagnostic (better than TTE)
2. CXR - may show large pulmonary arteries (secondary to inc blood flow) - inc pulmonary vascular markings 3. ECG- RBBB, right axis deviation, atrial abnormalities such as AFib or Aflutter |
|
|
Complications of ASD
|
1. pulmonary HTN- common in > 40 yo
2. Eisenmenger's disease - irreversible pulmonary HTN leads to shunt reversal (R--> L shunt), HF and cyanosis 3. Right sided HF 4. atrial arrhythmias-- esp Afib 5. Stroke secondary to paradoxical emboli or afib |
|
|
Clinical features of ASD
|
1. Mild Systolic Ejection murmur at pulmonary area secondary to inc blood flow
2. wide fixed splitting of S2 due to inc pulm blood flow and delayed closure of the Pulm Valve 3. diastolic flow "rumble" murmur - inc blood flow across the tricuspid valve 4. if advanced - signs of RVF - ascites, hepatomegaly, JVD etc |
|
|
What does fixed splitting of S2 indicate?
|
ASD
|
|
|
Treatment of ASD
|
1. surgical repair when pulm to systemic blood flow ratio > 1.5 : 1 or 2.0 : 1 OR if the patient is symptomatic
|
|
|
What is the most common congenital cardiac malformation?
|
VSD
|
|
|
What is a paradoxical embolus?
|
DVT forms and instead of traveling to the lungs and causing a PE is transverses the ASD to the brain causing stroke
|
|
|
Symptoms of Peripheral Vascular Disease (PVD)
|
1. Intermittent claudication- cramping leg pain that is reliably reproduced by the same walking distance (relieved by rest or dangling legs over the bed)
2. Rest pain (continuous) - usually felt over distal metatarsals, often prominent at night-- awakens patient from sleep. Hanging foot over the bed or standing relieves the pain due to extra perfusion to ischemic areas - using gravity. This suggests severe ischemia such that frank gangrene may occur without intervention |
|
|
Peripheral Vascular Disease (PVD) Risk Factors
|
1. Diabetes Mellitus - prevalence markedly increased
2. smoking 3. CAD 4. HLP 5. HTN 6. hyperhomocystinemia |
|
|
Diagnosis of AAA
|

1. US = test of choice to evaluation both location and size of aneurysm - 100% sensitive
2. CT Scan - 100% sensitive, but is more expensive and more time consuming- should only be used if patient is hemodynamically stable 3. Abd Xray - may show calcification of dilated segment -- allowing measurement of aortic diameter. Quick method of diagnosis but a negative study is not helpful-- cannot r/o |
|
|
Grey-Turner's sign vs Cullen's sign
|

Both are signs of acute pancreatitis or retroperitoneal bleed
Grey Turner's sign - ecchymosis on back or flanks Cullen's sign - ecchymosis around the umbilicus (U in cullens and umbilicus) |
|
|
Clinical features of AAA
|
- Usually asymptomatic and discovered incidentally on exam or radiologic study for another reason
- may have a sense of abd fullness - +/- pain, usually in hypogastrium (below umbilicus) + lower back- throbbing - pulsatile mass of exam - symptoms suggest expansion or impending rupture - sudden onset of severe pain in back or lower abd with radiation to groin or buttocks/legs --> rupture (may see grey turner's or cullen's signs) |
|
|
Abdominal Aortic Aneurysm
1. definition 2. where is it most common? 3. average age of diagnosis 4. women or men most likely afflicted? |
1. abnormal localized dilatation of the aorta
2. between the renal arteries and iliac bifurcation (infrarenal aorta) 3. incidence increase with age. They are rare before 50. Average age at the time of diagnosis is 65-70 yo 4. much more common in men |
|
|
Right-sided vs left-sided endocarditis
|
Right-sided is more likely in IV drug users (s. aureus)- due to injection into the venous system-- then infection goes back to the Right heart
Left-sided is more commonly due to infection of a damaged or prosthetic valve-- usually caused by s. viridans, a less virulent organism than s. aureus |
|
|
Infective Endocarditis
1. definition 2. acute vs subacute |
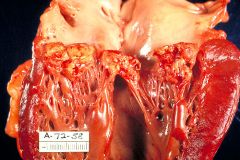
1. infection of heart valves that can be acute or subacute
2. acute- usually caused by s. aureus (virulent), on a normal heart valve, if no treatment then death occurs in < 6 weeks subacute- less virulent organisms (s. viridans or enterococcus), usually on damaged valves. If untreated then death may occur in > 6 weeks |
|
|
Rheumatic heart disease
|
Complication of untreated S. pyogenes pharyngitis - acute RF is immunologically mediated process that may progress to rheumatic heart disease with chronic valvular abnormalities
The most common valve problem = mitral stenosis, but there may be AV or TV issues as well |
|
|
Hemodynamic changes in hypovolemic shock by class (% blood lost, pulse inc, SBP dec, pulse pressure (SBP- DBP) dec, cap refill dec, RR inc, CNS sx, UOP)
1. Class I 2. Class II 3. Class III 4. Class IV |
1. Class I - 10-15% blood lost, normal pulse, normal SBP, normal pulse pressure, normal cap refill, normal RR, no CNS sx, UOP is normal
2. Class II - 20-30% of blood lost, pulse > 100, normal SBP, dec PP, delayed cap refill, mild inc in RR, anxious, UOP = 20-30 cc/hr 3. Class III - 30-40% blood lost, pulse > 120 bpm and weak, dec SBP, dec PP, delayed cap refill, marked tachypnea, confusion, UOP = 20 cc/hr 4. Class IV - > 40% blood lost, pulse > 140 bpm or non-palpable, marked decrease in SBP and PP, absent cap refill, marked tachypnea, lethargy/ coma, and negligible UOP |
|
|
Hypertensive Emergency
1. definition 2. vs urgency |
1. SBP > 220 +/- DBP > 120 mmHg in addition to end-organ damage- immediate treatment is indicated
2. urgency - inc BP alone without end-organ damage = hypertensive urgency rarely requires emergency treatment and can be managed with attempts to lower the BP over a 24 hour period |
|
|
When patients present with markedly inc blood pressure what is it critical to access for?
|
Signs of end-organ damage
1. Eyes- papilledema (swelling of the optic disc) 2. CNS - AMS or ICH -- hypertensive encephalopathy may develop (confusion etc) 3. Kidneys- renal failure or hematuria 4. Heart - unstable angina, MI, CHF with pulmonary edema, aortic dissection 5. Lungs- pulmonary edema |
|
|
Treatment of hypertensive URGENCY
|
Lower blood pressure gradually with ORAL agents over the course of 24 hours
|
|
|
Diagnosis of aortic coarctation
1. ECG findings 2. CXR findings |
1. ECG- LVH
2. CXR- notching of the ribs due to inc flow through the collaterals. Figure 3 appearance due to indentation of the aorta at the site of coarctation with dilation before and after the stenosis |
|
|
Diagnosis of PDA
1. CXR findings 2. Echo findings |
1. CXR- inc pulm vasc markings, dilated pulm arteries, enlarged cardiac silhouette, sometimes calcifications of the ductus arteriosus
2. Echo- PDA +/- turbulent blood flow` |
|
|
Pathophysiology of PDAs
|
- large L--> R shunt results in Right Hear volume overload, PHTN, and RHF (ascites, HSM, JVD etc)
- cyanosis is a late finding - may eventually see reversal of blood flow (R-->L) |
|
|
Treatment of Aortic Coarctation
|
- Standard treatment is surgical decompression
- percutaneous balloon aortoplasty is also an option in selected cases |
|
|
Coarcation of the Aorta
1. definition 2. associations |
1. narrowing/occlusion of aorta usually at origin of Left subclavian near the ligamentum arteriosum --> leads to obstruction between the proximal and distal aorta thus leading to inc afterload
2. associated with Turner syndrome |
|
|
Diagnosis of VSD
1. ECG findings 2. CXR 3. Echo findings |
1. biventricular hypertrophy predominates when the PVR is high
2. CXR- enlargement of the pulm artery, enlargement of the cardiac silhouette. As the PVR increases the L--> R shunt decreases and heart size decreases but PA size increases 3. VSD |
|
|
Pathophysiology of VSD
|
1.Blood flows from LV (high pressure) into the RV (low pressure) through the VSD. this leads to inc pulm blood flow. As long as pulmonary vascular resistance (PVR) is lower the systemic vascular resistance (SVR) then flow is L --> R. If PVR > SVR then shunt becomes R --> L
2. Large defects leads to PHTN |
|
|
Clinical features of aortic coarctation
|
- HTN in upper extremities and hypotension in the lower extremities
- well-developed upper body with under-developed lower hald - mid-systolic murmur heard best over the back - sx- HA, cold extremities, claudication with exercise and fatigue |
|
|
treatment of shock (general)
|
1. ABCs - airway, breathing and circulation
2. Except for cardiogenic and sometimes neurogenic shock-- give large boluses of IV Fluids |
|
|
What signs/symptoms are common to all forms of shock?
|
- decreased BP
- oliguria - tachycardia - compensatory due to low BP - AMS |
|
|
Initial approach to the patient in shock
1. findings supportive of different types of shock 2. initial steps to treatment |
1. Focused H & P - fever and infection site--> septic shock
- trauma, GI bleeding, vomiting--> hypovolemic shock - h/o MI, angina or heart disease --> cardiogenic shock - JVD --> cardiogenic shock - spinal injury or neuro deficits --> neurogenic shock 2. Stabilize and determine the cause- 2 large bore IVs, central line and art line, b. fluid bolus 500-1000cc, c. blood draw - CBC, elec, CR, BUN, PT/PTT, type and cross, d. ECG, CXR, e. pulse ox, f. vasopressors (dopamine or epi if unstable DESPITE fluids), g, if NOT sure what the cause is then do pulmonary catheter or echo |
|
|
Shock - general characteristics
1. definition 2. presentation 3. changes seen to what? |
1. underperfusion of tissues-- medical emergency. Supply does not meet demand
2. decreased BP plus malfunction of underperfused organ systems (lactic acidosis, renal -anuria/oliguria, CNS dysfunction (AMS) 3. C.O., SVR and volume status (assessed by JVP and PCWP) -- these vary depending on the type of shock |
|
|
treatment of superficial thrombophlebitis
1. need anticoag? 2. localized thrombophlebitis? 3. severe thrombophlebitis? 4. need for abx? if septic thrombophlebitis? |
1. No anticoagulation needed-- rarely causes PE
2. localized thrombophlebitis --< mild analgesic (aspirin) is all that is required-- continue activity 3. severe thrombophlebitis (with pain and cellulitis) - a. bed rest, elevation, hot compresses, b. onse symptoms resolve -- ambulation and elastic stockings, c. no abx unless suppurative-- need adequate drainage, d. septic thrombophlebitis-- usually due to infection of IV cannula -- remove and start IV abx |
|
|
Superficial thrombophlebitis
1. general characteristics 2. clinical features |
1. Vichow's triad is implicated (stasis, endothelial injury and hypercoaguable state). UE - at IV sites, LE - assoc with varicose veins (in greater saphenous system) - secondary to stasis of blood flow
2. pain and tenderness, induration, plus erythema long the course of vein. Tender cord may be palpated |
|
|
Perforating veins
|
- connect superficial and deep venous systems
- valves allow flow from superficial to deep systems but not vice versa |
|
|
Prognosis of VTach
|
- prognosis depends on presence of heart disease and whether VTach is sustained or non-sustained
- VTach after a MI leads to a poor prognosis especially if sustained - If there is no underlying heart condition, then there is a good prognosis. |
|
|
Non-Sustained VTach
|
-Brief self-limited runs of VTach
- usually asymptomatic - when CAD and LV dysfunction are present, it is an independent risk factor for sudden cardiac death so do a thorough cardiac work-up in patients with non-sustained VT |
|
|
Torsades de pointes (TdP)
|
- rapid polymorphic VT
- dangerous arrhythmia that often can lead to VFib - associated wtih many factors that prolong QT interval (e.g. congenital, TCAs, anticholinergics, electrolyte abnormalities, ischemia) - IV Magnesium stabilizes heart while you treat the underlying cause |
|
|
Sustained VTach definition
|
- persists in absence of intervention
- lasts longer than 30 seconds and is almost always symptomatic - often associated with marked hemodynamic compromise (dec BP or ischemia) - LIFE THREATENING - can progress to VFib |
|
|
Causes of VTach (6)- which is most common
|
1. CAD with prior MI = most common cause
2. Active ischemia, hypotension 3. cardiomyopathies 4. congenital defects 5. prolonged QT syndrome 6. Drug toxicity |
|
|
Ventricular Tachycardia definition
|
- rapid and repetitive firing of 3 or more PVCs in a row at a rate between 100-250 bpm
- AV dissocation present (i.e. sinus P waves continue with their cycle unaffected by Vtach) - originates below the bundle of His |
|
|
Treatment of Wolff-Parkinson-White Syndrome
|
1. Radio-frequency catheter ablation of one arm of the re-entrant loop
2. Avoid drugs active on the AV node (e.g. digoxin) because they may accelerate conduction through the accessory pathway (type IA + IC antiarrhytmics are better choices) |
|
|
ECG diagnosis of WPW syndrome
|
- narrow complex tachycardia, short PR interval + DELTA WAVE (upward deflection seen before the QRS complex)
|
|
|
Wolff-Parkinson-White (WPW) syndrome- definition
|
- accessory conduction pathway from atria to ventricles causes premature ventricular excitation because it lacks the delay seen in the AV node.
- May lead to paroxysmal tachycardia by 2 mechanisms a. orthodromic reciprocating tachy - impulse through AV node (anterograde) -- depolarizes ventricles -- retrograde impulse through accessory pathway redepolarizes the atrai -- re-entry loop (no delta waves) b. supraventricular tachy (afib or aflutter)-- usually AV node only allows certain impulses through accessory pathway but everything gets through allowing for inc HR and hemodynamic instability |
|
|
Treatment for paroxsymal SVT
|
1. Vagal maneuvers --> block re-entry mechanism by delaying AV conduction
2. Pharmacologic Treatment- IV adenosine - agent of choice. Short duration, that decreases sinoatrial activity and AV nodal activity. IV verapamil and IV esmolol or digoxin. 3. Direct Current Cardioversion if drugs are not effective or patient is unstable 4. Prevention- digoxin usually is the drug of choice. Verapamil or beta-blockers are alternatives. Radiofrequency catheter ablation of either the AV node or the accessory tract |
|
|
Side effects of adenosine
|
- Headache
- flushing - shortness of breath - chest pain - n/v |
|
|
Causes of paroxsymal Vtach (PVST)
|
1. ischemic heart disease
2. digoxin toxicity= PVST with 2:1 ratio is most common 3. AV node re-entry 4. atrial flutter with RVR 5. AV reciprocating tachy (accessory pathway) 6. excessive caffeine intake or EtOH |
|
|
Most common cause of Supraventricular Tachycardia (SVT)
|
AV nodal re-entrant tachycardia
|
|
|
Paroxsymal supraventricular tachycardia (PVST) pathophysiology (2 types)
|
1. most commonly due to re-entrant tachycardia. 2 pathways (one fast and one slow), within the AV node- re-entrant circuit is in AV node. It is initiated or terminated by PACs. ECG shows narrow QRS complexes with no discernable p-waves. The p-waves are buried in the QRS complex
2. orthodromic AV re-entrant tachycardia- an accessory pathway between atria and ventricles that conducts retrograde. Initiated or terminated by PACs and PVCs. ECG shows narrow QRS complexes with p-waves that may or may not be seen. Re-entrant circuit is longer |

