![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
282 Cards in this Set
- Front
- Back
- 3rd side (hint)
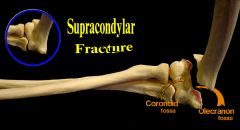
What artery should we be concerned a/b in supracondylar humerus fracture?
Check pulse of _ artery |
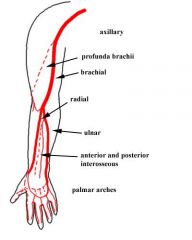
Brachial artery
Check radial artery pulse |
|
|
|
Peripheral neuropathy
Microcytic anemia |
B6 (pyridoxine) deficiency
|
|
|
|
What dz is this?
Ass'd c/ thyrotoxicosis, thymoma Thymoma resection may be curative Must avoid aminoglycosides and beta-blockers Proximal muscle weakness Fatigable ptosis, double-vision |
Myasthenia gravis
|
|
|
|
Diarrhea
Dementia Dermatitis |
B3 (niacin deficiency):
Diarrhea Dementia Dermatitis |
|
|
|
there are 2 disease types that cause the following:
demyelination of dorsal columns, lateral corticospinal tracts, spinocerebellar tracts -> ataxia, hyperreflexia, impaired position/vibrtion sense |
B12 deficiency and Friedreich's ataxia
(corticospinal dz causes hyperreflexia, which is not present in tertiary syphilis) Friedrich's ataxia: AR, trineucleotide repeat in tocopherol transfer protein -> progressive neuropathy, cardiomyopathy |
|
|
|
Oxytocin administration can cause what electrolyte disturbance in pregnant women?
|
Oxytocin administration can cause hyponatremia in pregnant women
|
|
|
|
Hypertension
Abdominal mass Hematuria Hepatic cysts |
Adult polycystic kidney disease:
Hypertension Abdominal mass Hematuria Hepatic cysts Treat hypertensionm kidney failure risk of cerebral berry aneurysm |
|
|
|
Hgb > 17, Hct > 50
WBC > 10,000/uL, Plt > 350,000/uL Low erythropoeitin redness, itching, splenomegaly Dz Tx Prognosis |
Polycythemia vera:
LOW epo (unlike other primary polycythemia) Tx: Cytoreductive drugs: hydroxyurea, interferon ASA to reduce thrombi Survival 7-10 yrs |
|
|
|
dyspnea
pleuritic chest pain tachycardia |
PE
Dx: V/Q scan most common; pulm angiography is gold standard 90% 2/2 DVT (dx by duplex US) Tx: heparin + long-term warfarin |
|
|
|
sinusitis
pneumonitis glomerulonephritis necrotizing vasculitis Dz Tx |
Wegener's granulomatosis
classic triad: sinusitis, pneumonitis, glomerulonephritis c-ANCA (+) usually Tx: cytotoxic agents e.g. cyclophosphamide, high-dose prednisone |
|
|
|
30-50 y/o
recurrent sinus infections hemoptysis SOB cough |
Wegener's granulomatosis
classic triad: sinusitis, pneumonitis, glomerulonephritis c-ANCA (+) usually Tx: cyclophosphamide, prednisone |
|
|
|
small-medium artery vasculitis
kidney failure high p-ANCA (-) c-ANCA |
Polyarteritis nodosa
small-medium artery vasculitis -> small aneurysms kidney failure high p-ANCA (-) c-ANCA tx: cyclophosphamide, prednisone |
|
|
|
young male smoker
claudication in limbs |
Thromboangiitis obliterans
young male smoker c/. claudication in limbs tx: stop smoking |
|
|
|
Dermatophyte _ causes tinea pedis/ cruris/ corporis/ captitis, along c/ Trichophyton and Epidermophyton
Pets = reservoir, can be treated c/ azoles |
Microsporum
enterocytozoon, encephalitozoon Spores in stool |
|
|
|
respiratory alkalosis
metabolic acidosis tinnitus vomiting mental status changes what dz? what tx? |
Asa overdose:
respiratory alkalosis metabolic acidosis tinnitus vomiting mental status changes IV bicarb to alkalinize urine |
|
|
|
GI sx, polyuria, neurologic sx
shortened QT problem is _ 2/2 to 3 main diseases _ tx _ |
hypercalcemia:
2/2 cancer, hyperparathyroidism, sarcoidosis GI sx, polyuria, neurologic sx shortened QT tx: saline, furosemide |
|
|
|
Pt c/ hemolysis, ARF, proteinuria, CNS changes
Dz 2 therapies Avoid _ b/c _ |
TTP
NSAIDS, plasmapheresis No platelets (can form clots) |
|
|
|
GI sx, polyuria, neurologic sx
shortened QT bilateral hilar lymphadenopathy |
sarcoidosis:
hypercalcemia sx + lymphadenopathy, non-caseating granulomas |
|
|
|
muscle spasms
lip tingling prolonged QT |
hypocalcemia:
muscle spasms lip tingling prolonged QT 2/2 hypoparathyoidism, renal dz, vit D deficiency |
|
|
|
Delivery of baby = definitive tx for HELLP after _ weeks
Pharm tx otherwise is 2 drug types for HTN... |
Delivery of baby = definitive tx for HELLP after 34 weeks
Pharm tx: hydralazine, beta blockers |
|
|
|
Middle-aged woman c/ priuritus, jaundice, steatorhhea
anti-mitochondrial Ab's, high bili, high alk phos +/- xanthomas, xanthelesmas, osteoporosis Dz Tx: _ slows dz progression _ for pruritus Definitive tx is _ |
primary BILIARY CIRRHOSIS 2/2 destruction of INTRA-hepatic bile ducts
Tx: Ursodeoxycholic acid slows dz progression Cholestyramine for pruritus Liver transplant = only other effective tx |
|
|
|
metabolic alkalosis
HTN high Na+ low K+ what disease? #1 cause |
Hyperaldosteronism:
Conn's (adrenal adenoma) = #1 cause high aldosterone, low renin (normal pathway: low blood volume or high K -> AT2 -> aldosterone -> DCT reabsorbs Na, secretes K, H) metabolic alkalosis, HTN, high Na+, low K+ |
|
|
|
skin darkening
weakness weight loss GI symptoms low Na+, high K+ hypotension |
Addison's = hypoaldosteronism
adrenal cortex insufficiency -> low cortisol, low aldosterone, high ACTH skin darkening weakness weight loss GI symptoms low Na+, high K+ hypotension |
|
|
|
euvolemic hyponatremia
urine osmolarity >300 mmol/Kg despite fluid challenge normal BP, no edema what dz? mechanism tx |
SIADH
tx = fluid restriction, demeclocyline euvolemic hyponatremia urine > serum osmolarity normal BP, no edema |
|
|
|
extreme polydipsia, polyuria
dilute urine +/ - high Na+ what 2 diseases? how is each treated? |
Diabetes insipidus
Posterior pituitary dz = ADH deficiency (2/2 tumor, ischemia/Sheehan's, trauma, ...) -> tx is desmopressin Nephrogenic = kidneys not responding to vasopressin (2/2 to lithium, demeclocycline = ADH blocker) Tx: Thiazides => mild volume depletion, stim prox absorbtion of Na, H20) Na restriction, water intake. |
|
|
|
symmetric ulnar deviation @ MCP joints
"swan neck", "boutonniere" deformaties @ PIP joints disease therapy |
Rheumatoid arthritis
tx = NSAIDS, anti-malarials, methotrexate, gold salts symmetric ulnar deviation @ MCP joints "swan neck", "boutonniere" deformaties @ PIP joints |
|
|
|
"Heberden's" nodes @ DIP joints
"Bouchard's" nodes @ PIP jointd Hip, spine pain Disease Tx |
Osteoarthritis
tx = NSAIDS, weight reduction "Heberden's" nodes @ DIP joints "Bouchard's" nodes @ PIP jointd Hip, spine pain |
|
|
|
abrupt onset of steady, severe pain that radiates to the back
no guarding, rebound AXR: "sentinel loop" or "colon cutoff sign" +/ - hypocalcemia Dz Can be 2/2 to 2 drugs... Tx Give IV abx, resp support, debridement if _ |
Acute pancreatitis:
2/2 gallstones, alcoholism, hypercalcemia, hypertriglyceridemia, VALPROIC ACID, THIAZIDES, virus, s/p ERCP, scorpion bite Tx: supportive Necrotizing sx => IV abx, resp support, debridement |
|
|
|
middle aged male c/:
malabsorbtion fever arthritis CNS manifestations Disease Tx |
Whipple's dz:
tx = Pen, Amp, or Tetracycline x 4-6 mo malabsorbtion fever arthritis CNS manifestations |
|
|
|
Anti-hypoglycemic ass'd c/ SIADH
(also a tx for central DI) |
Chlorpropamide = anti-hypoglycemic ass'd c/ SIADH
(also a tx for central DI) |
|
|
|
brown/gray rings in cornea
cirrhosis psych problems What is the mnemonic to remember 4 main sx of this dz? What is the tx? |
Wilson's dz
Cu accumulates in liver, brain, eye -> cirrhosis, psych problems ABCD: Asterixis Basal ganglia dz Ceruloplasmin low, Cu high Choreiform mvmts Carcinoma (hepatocellular) RF Dementia Tx: Restrict Cu (fish, liver, legumes) Penicillamine = Cu chelator, increases Cu in urine (already high as part of the dz) +/- oral zinc to increase fecal Cu excretion |
|
|
|
Sore throat
lymphadenopathy hepatosplenomegaly (+) heterophil Ab test Atypical lymphocytes Virus is _ ~ 1/3 have coexisiting illness of _ Avoid antibiotic _ |
Epstein Barr virus:
sore throat lymphadenopathy hepatosplenomegaly (+) heterophil Ab test Atypical lymphocytes ~1/3 have coexisting strep pharyngitis Avoid ampicillin => rash complications = splenic rupture, hepatitis |
|
|
|
elevated venous pressure
hypotension muffled heart sounds Dz Echo finding |
BECK'S TRIAD: cardiac tamponade
elevated venous pressure hypotension (most reliable) muffled heart sounds Echo: RA, RV diastolic collapse. CXR: enlarged, globular heart EKG: electrical alternans is diagnostic 2D US best to confirm dx |
|
|
|
CABG indications
|
CABG indications:
L main proximal LAD Mid-LAD + LCX 3-vessel disease |
|
|
|
CXR showing:
widened mediastinum obliteration of aortic knob |
Aortic tear => CXR showing:
widened mediastinum obliteration of aortic knob |
|
|
|
hypotension
distended neck veins decreased pulse P muffled heart sounds pulsus paradoxus = fall in BP on inspiration decreased EKG voltage |
Cardiac tamponade:
hypotension distended neck veins decreased pulse P muffled heart sounds pulsus paradoxus = fall in BP on inspiration |
|
|
|
How does one use the dexamthasone supression test?
|
2nd LINE (after 24-hr free cortisol to dx cause of hyperadrenalism)
Normal: low dose => decreases cortisol ACTH-producing tumor: low dose => increases cortisol high dose => decreases cortisol Cortisone-producing tumor: low OR high dose => increases cortisol |
|
|
|
woman in teens-twenties c/:
solitary, encapsulated, freely movable mass |
Fibroadenoma:
woman in teens-twenties solitary, encapsulated, freely movable mass no increased cancer risk |
|
|
|
sudden severe pain radiating to the back
hx of syphilis, atherosclerosis, Marfan's, HTN, trauma, congenital heart defect Disease Dx Tx |
Dissecting aortic aneurysm:
hx of HTN > syphilis, atherosclerosis, Marfan's, trauma, congenital heart defect Dx: differing BPs in upper extremities -> confirm c/ CT Tx: nitroprusside, beta blockers -> hypotension ASCENDING (type II or A) or AORTIC ARCH -> SURGERY immediately DESCENDING (type I=ace/desc, III=desc or B)-> MEDICAL TX -> surgery if HTN or sx continue or aneurysm develops |
|
|
|
workup and tx for blunt spinal cord trauma
|
Get plain films + CT
(MRI = best to assess cord injury, compression) steroids improve outcome Surgery for incomplete neuro injury + a correctable external compression, e.g spine subluxation or bone chip |
|
|
|
tx for Wegener's granulomatosis
|
Wegener's granulomatosis
Tx: cyclophosphamide, prednisone classic triad: sinusitis, pneumonitis, glomerulonephritis c-ANCA (+) usually |
|
|
|
tx for Polyarteritis nodosa (PAN)
|
Polyarteritis nodosa
tx: cyclophosphamide (alkylating agent, aka Cytoxan), prednisone ass'd c/ HepB, cryoglobulinemia medium artery autoimmune vasculitis -> small aneurysms kidney failure, neuropathy, ab pain, fever, wt loss high p-ANCA, (-) c-ANCA |
|
|
|
tx for Thromboangiitis obliterans
|
Thromboangiitis obliterans
young male smoker c/. claudication in limbs tx: stop smoking |
|
|
|
Treatment for ITP:
adult vs. child cases |
Idiopathic thrombocytopenia purpura:
Child or young lady c/ isolated thrombocytopenia 2/2 auto-ab's against platelets Peds cases often follow viral infection, usually self-limited Adult and severe peds cases require prednisone ± splenectomy Platelet transfusion not indicated |
|
|
|
tx for essential hypertension
|
ABCD:
ACEI/ARB: esp. for DM β blockers reduce mortality, esp. important for CAD (+/- Ca-channel blocker) Diuretics reduce mortality, esp. important for Af Am |
|
|
|
tx for malignant HTN
|
tx for malignant HTN =
sodium nitroprusside |
|
|
|
drug toxicity associated c/ T wave inversion
|
digoxin
|
|
|
|
tx for hypercalcemia
|
hypercalcemia:
tx: saline, furosemide (not thiazides) 2/2 cancer, hyperparathyroidism, sarcoidosis GI sx, polyuria, neurologic sx shortened QT |
|
|
|
tx for hyperthyroidism
|
hyperthyroidism:
tx: propranolol, radioactive iodine ablation 2/2 Grave's (diffuse toxic goiter) > vital thyroiditis, toxic adenoma |
|
|
|
tx for Klebsiella pneumonia
|
3G cephalosporin = ceftriaxone
or fluoroquinolone |
|
|
|
B12 deficiency is causesd by 5 things:
|
B12 deficiency is caused by 5 things:
1. stomach or ileal resection 2. diet 3. overgrowth of bacteria in blind loop of bowel or Meckel's diverticulum 4. atrophic gastritis 5. diphyllobothrium latum = fish tapeworm |
|
|
|
Pt has FEV1/FVC <0.7
Destruction of alveolar capillary membrane, decreased lung distensibility What is the tx regimen? |
COPD:
#1: anti-cholinergic = ipratropium, tiotropium + pneumococcal, flu vaccines -> Beta-2 agonists = albuterol -> O2 if resting PaO2 <66mmHg or SaO2 <90% -> corticosteroids |
|
|
|
Beriberi is deficinecy of vitamin ____ aka __
Wet beriberi = _ Dry beriberi = _ |
Beriberi is deficinecy of vitamin B1 aka thiamine
Wet beriberi = high-output heart failure Dry beriberi = symmetric neuropathy c/ pain |
|
|
|
dendriform corneal ulcers
vesicular ulcers in a dermatomal distribution dz tx |
Herpes zoster opthalmicus
tx = ORAL acyclovir, famiclovir, valacyclovir |
|
|
|
Antihypertensive drug good for pts c/:
Raynaud's Atrial tachyarrhythmias |
Ca channel blockers = good antihypertensive for pts c/:
Raynaud's Atrial tachyarrhythmias nifedipine, verapamil, diltiazem |
|
|
|
B6 (pyridoxine) deficiency
|
B6 (pyridoxine) deficiency:
Peripheral neuropathy Microcytic anemia |
|
|
|
bacterial meningitis in child 3 months old - adulthood
2 common organisms empiric tx |
Pneumococcus
Meningococcus IV vanc + ceftriaxone or cefotaxime rifampin for contacts if meningococcal meningitis |
|
|
|
Pt c/ recent virus
Now c/ decreased platelets No kidney sx, anemia, or hemolysis Dz Dx: test for _ Tx |
ITP
(+) anti-platelet Ab's Steroids if bleeding or Plt < 20,000 Splenectomy |
|
|
|
Pt > 40 y/o
Bloody nose, nasal perforation, hemoptysis, pleurisy Dz Dx (lab finding) Tx |
Wegener's: granulomatous inflamm of resp tract + kidney, necrotizing vasculitis
(+) cANCA Tx: corticosteroids, cyclophosphamide (alkylating agent) Pt > 40 y/o Bloody nose, nasal perforation, hemoptysis, pleurisy |
|
|
|
Vitamin D deficiency
|
Vitamin D deficiency:
Children -> defective bone growth, leg bowing Adults -> osteopenia, bone tenderness |
|
|
|
What vitamin deficiency?
RBC fragility muscle weakness/ataxia hyporeflexia Opthalmoplegia/blindness |
Vitamin E deficiency
|
|
|
|
TB drug regimen
|
TB drug regimen = RIPE:
Rifampin (turns body fluid orange) INH + B6 (peripheral neuritis, hepatitis) Pyrazinamide Ethambutol (optic neuritis) |
|
|
|
thyroid function tests:
best indicator of thyroid state most commonly used indicator of thyroid state 3 things that are low in hypothyroid, high in hyperthyroid |
thyroid function tests:
free thyroxine (t4) = best indicator of thyroid state free thyroxine index (FTI) = most commonly used indicator of thyroid state FTI, free T4, triiodothyronine (T3) = low in hypothyroid, high in hyperthyroid |
|
|
|
lab changes in hypothyroidism:
thyroid fx tests antibodies |
lab changes in hypothyroidism:
low FTI, free T4, triiodothyronine (T3) anti-thyroglobulin, anti-microsomal antibodies |
|
|
|
4 common causes of hyperthyroidism
|
hyperthyroidism:
Grave's = #1 = diffuse toxic goiter. Pretibial myxedema. Vital thyroiditis Toxic adenoma Plummer's dz = toxic multinodular goiter |
|
|
|
Graves' Disease:
Mechanism Tx |
Graves' Disease:
ab's against TSH receptors -> thyroid hyperfx Tx: propranolol, radioactive I |
|
|
|
round face
short digits mental retardation hypocalcemia high PTH what disease? mechanism |
Pseudohypoparathyroidism
2/2 tissue resistance to PTH round face short digits mental retardation hypocalcemia high PTH |
|
|
|
Lady c/ short stature
Short 4th, 5th metacarpals Hypocalcemia |
Albright's hereditary osteodystrophy aka
pseudohypoparathyroidism Autosomal D Kidneys unresponsive to PTH |
|
|
|
What is the #1 pituitary tumor?
Tx What if a pituitary tumor is calcified? |
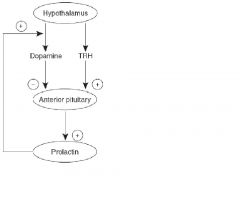
Prolactinoma = #1 pituitary tumor
tx = bromocriptine calcified pituitary tumor => craniopharyngioma |
|
|
|
Pituitary tumor that is calcified
|
Craniopharyngioma = Pituitary tumor that is calcified
|
|
|
|
Thyroid cancer:
presentation most common type |
Thyroid cancer:
women > men usually euthyroid often c/ enlarged cervical LN's papillary carcinoma = #1 type |
|
|
|
Thyroid cancer c/ elevated calcitonin
main RF |
Medullary carcinoma of thyroid:
elevated calcitonin ass'd c/ MEN2,3 |
|
|
|
Workup for a thyroid nodule (4 steps)
|
Cancers are usually "cold" and solid
1. TFTs to r/o hyperfx 2. US => solid vs. cystic 3. Radioactive scan => hot vs. cold 4. Cold nodule => FNA to r/o malignancy - high sensitivity, med specificity ("hot" nodules are never cancerous, should not be biopsied) |
|
|
|
Tx for thyroid cancer
|
Tx for thyroid cancer:
surgery (spare recurrent laryngeal nerve, at least 1 parathyroid gland) +/ - post-op radioactive I, radiotherapy, thyroid replacement |
|
|
|
Tx for parathyroid adenoma
|
Parathyroid adenoma:
usual cause of primary hyperparathyroidism Tx: neck exploration, excison |
|
|
|
3 possible causes of pseudotumor cerebri
Tx |
large dose Vitamin A
large dose tetracyclines withdrawal from corticosteroids tx: acetazolamide (inhibits choroid plexus carbonic anhydrase to decrease CSF) -> corticosteroids -> repeat LPs |
|
|
|
#1 cause of secondary HTN in ladies
|
#1 cause of secondary HTN =
oral contraceptives |
|
|
|
physical exam finding of bilateral renal artery stenosis
|
physical exam finding of bilateral renal artery stenosis =
abdominal bruit |
|
|
|
Tx for Crohn's, UC:
First line: _ +/- _ Severe dz, flares: _ Do NOT use _ b/c can precipitate _ Surgery |
Tx for Crohn's, UC:
First line: 5-ASA +/- sulfa drug, e.g. sulfasalazine Severe dz, flares: corticosteroids, other immunosupressants e.g. infliximab, azathioprine Do NOT use anti-diarrheals b/c can precipitate toxic megacolon UC can be treated c/ protocolectomy + ileoanal anastomosis |
|
|
|
Infantile spasms
hypopigmented macules MR red nodules on nose + cheeks rough papule on sacrum Dz (remember mnemonic) Inheritance Increased risk of neoplasms... |
Tuberous sclerosis: AD
Affects skin, heart, retina, kidneys "Zits, Fits, Deficits" RF for cardiac rhabomyoma, astrocytoma > renal hamartoma/angiomyolipoma, other benign tumors Tx: infantile spasms => ACTH Seizures => clonazepam, valproate Surgery if dev delay, high ICP, ... |
|
|
|
3 sequelae of malignant HTN
tx for malignant HTN |
malignant HTN ->
nephropathy papilledema encephalopathy tx = sodium nitroprusside |
|
|
|
child has unilateral replacement of long bones c/ fibrous tissue
precocious puberty cafe au lait spots c/ irregular serpigenous borders |
McCune-Albright
Polyostotic fibrous dysplasia Pigment:cafe au lait spots Precocious Puberty unlike tuberous sclerosis and neurofibromatosis, this is not a phakomatosis |
|
|
|
physical findings of mitral regurgitation:
murmur +/- echo, CXR findings... |
mitral regurgitation:
holosystolic murmur @ apex radiating to axilla LA enlargement, pulmonary congestion/HTN. LVH Soft S1 |
|
|
|
Skin cancer on chin tends to be _
Skin cancer on eyelid tends to be _ Sq cell carcinoma is more likely to metastasize if it arises from _ or _; less likely if it arises from _ |
Basal cell => Eyelid
Sq cell => Chin from lip or ulcer => metastasis more likely from actinic keratosis => metastasis less likely |
|
|
|
physical findings of aortic regurgitation:
murmur Echo finding seen c/ 2 diseases… |
aortic regurgitation:
pandiastolic decrscendo murmur @ sternal border Waterhammer pulse, pistol-shot femoral pulse LV enlargement Marfan's, syphilis |
|
|
|
Juvenile RA: 3 types are...
1. Pauciarticular complication _ ANA _, RF _ joint type _ 2. Polyarticular ANA _, RF _ joint type _ 3. Still's dz systemic sx ANA _, RF_ |
Pauciarticular: <5 weight-bearing joints
Risk of iridocyclitis = uveitis ANA (+), RA (-) Polyarticular: >5 small joints ANA, RA (-) Still's = acute febrile/systemic: daily high fevers, salmon-colored rash, H/S-megaly, pericarditis Tx: NSAIDS. Corticosteroids for severe cases, if carditis present 2nd line: methotrexate Must occur in <16 y/o, last >6 wks 95% goes away by puberty ANA, RA (-) |
|
|
|
early-diastolic decrescendo murmur @ apex
wide pulse P, LVH, LV dilation , S3 ass'd c/ what 2 diseases? |
Aortic regurgitation
Marfan's, Syphilis |
|
|
|
_ % of AAA rupture is retroperitoneal, _% anterior to peritoneal cavity
|
80 % of AAA rupture is retroperitoneal, 20% anterior to peritoneal cavity
|
|
|
|
most AAA rupture is below renal arteries b/c _
|
most AAA rupture is below renal arteries b/c vasa vasorum is lacking there
|
|
|
|
what disease process?
middle to outer part of aorta elastic tissue fragmentation cleftlike spaces containing acid mucopolysaccharides most commonly in 2 genetic diseases _ |
Cystic medial degeneration:
middle-outer aorta elastic tissue fragmentation cleftlike spaces containing acid mucopolysaccharides Marfans (fibrillin) Ehlers-Danlos (elastin) |
|
|
|
cystic medial degeneration is involved in AAA dissection 2/2 to _ in elderly men and _ in younger individuals
occurs in _ part of aorta |
cystic medial degeneration is involved in AAA dissection 2/2 to hypertension in elderly men and CT disorders in younger individuals
occurs in middle/outer part of aorta |
|
|
|
Sclerosing mediastinitis is most commonly 2/2 to _
Tx is _ other sx: calcified nodes in lung, mediastinum, spleen, liver yeast on silver stain Urine and serum polysaccharide Ag test = sensitive |
Sclerosing mediastinitis is most commonly 2/2 to histoplasmosis
Tx: amphotericin B x 3-10 days, then itraconzaole x 12 weeks HIV opportunistic pathogen when CD4+ <50,000/uL |
|
|
|
dilated scrotal veins on L
no retching/vomiting scrotal pain dz tx |
varicocele involving pampiniform plexus of veins => RENAL CARCINOMA (L testicular vein drains into L renal)
Renal adenocarcinoma ~85% => resection (15-30% response to chemo) dilated scrotal veins on L no retching/vomiting scrotal pain |
|
|
|
increased plasma volume
increased RBC mass tendency for venous thrombosis Dz Dx: test level of _ Tx |
polycythemia rubra vera:
clonal proliferation of a pluripotent marrow stem cell Excess RBC, WBC, Plt Low EPO!!!!!!!!!!!!!!!!!! Tx: cytoreductive drugs: hydroxyurea, interferon Aspirin to prevent thrombosis Survival c/ tx is 7-10 yrs |
|
|
|
__ = #1 sign ass'd c/ traumatic dissection of thoracic aorta
2/2 blood collecting subjacent to _ |
wide mediastinum => traumatic dissection of thoracic aorta
2/2 blood collecting subjacent to the adventitia (intima, media are fractured; adventia intact) => a PSEUDOaneurysm |
|
|
|
Myocardial contusion 2/2 chest trauma tends to involve:
_ ventricle EKG finding _ most sensitive test for dx _ |
Myocardial contusion 2/2 chest trauma tends to involve:
R ventricle EKG finding new RBBB most sensitive test for dx radionuclide angiography |
|
|
|
Shock c/:
low CO high PCWP high PVR low SvO2 |
Cardiogenic shock:
low CO high PCWP high PVR low SvO3 |
|
|
|
2 diabetes drugs not appropriate for pts c/ liver failure (okay for kidney failure)
(1 is short-acting) |
Glipizide = short-acting
Rosiglitazine |
|
|
|
Shock c/:
low CO low PCWP low PVR low SvO2 |
Neurogenic shock:
low CO low PCWP low PVR low SvO5 |
|
|
|
Shock c/:
high CO low PCWP low PVR high SvO2 high SaO2 |
Septic shock:
high CO low PCWP low PVR high SvO2 high SaO3 |
|
|
|
Carotid artery stenosis - surgery is indicated if:
1. TIA 2. asymptomatic + >_% stenosis or _ plaque 3. hx of _ |
Carotid artery stenosis - surgery is indicated if:
1. TIA 2. asymptomatic + >75% stenosis or complex, ulcerated plaque 3. good fx s/p CVA 2/2 carotid occlusion |
|
|
|
After MI, don't give beta blocker in 3 circumstances...
|
After MI, don't give beta blocker if:
R coronary distribution (2, 3, aVF) in heart failure increased PR interval |
|
|
|
pt c/ decreased pain and temp sensation over the lateral aspects of both arms
+/- slow involvement of motor + sensory deficits |
syringomyelia:
central pathologic cavitation of spinal cord idiopathic or c/ arnold-chiari or trauma usually affects lateral spinothalamic tracts first |
|
|
|
Type A aortic aneurysm is …
Tx is ... |
Type A aortic aneurysm:
ascending or involving aortic arch -> immediate surgery Marfan's: fibrillin defect -> type A aneurysm +/- aortic annular dilatation => higher dissection risk |
|
|
|
Type B aortic aneurysm is …
Tx is _ Surgical indication is _ |
Type B aortic aneurysm:
descending -> medical tx -> surgery if HTN continues or aneurysm develops, or pt stays symptomatic |
|
|
|
_ supplies the SA and AV nodes, His bundle, posterior LV
also supplies the inferior LV via the PD artery 80% of the time infarction causes EKG changes... |
RCA supplies the SA and AV nodes
also supplies the inferior LV via the PD artery 80% of the time Acute posterior infarct => ST dep. in V1, V2, V3 Acute inferior infarct => ST elev in II, III,AVF |
|
|
|
LAD supplies …
look for Q waves, T inversion in _ |
LAD
EKG changes in V1-4 anterior 2/3 of the interventricular septum anterior wall of the LV anterior papillary muscle |
|
|
|
_ supplies the lateral and posterior superior LV
|
LCX supplies the lateral and posterior superior LV
|
|
|
|
In a child c/ VSD, consider 3 congenital diseases/conditions...
(see hint) |
In a child c/ VSD, consider:
fetal alcohol syn TORCH Down's syn |
in utero chemical exposure
in utero micro exposure genetic disease |
|
|
|
|
|
|
|
80 y/o male c/ systolic crescendo-decresendo murmur
|
Aortic stenosis:
81 y/o male c/ systolic crescendo-decresendo murmur |
|
|
|
5 y/o c/ systolic murmur + wide, fixed split S2
|
ASD:
5 y/o c/ systolic murmur + wide, fixed split S2 often asymptomatic until adulthood +/- palpitations Secundum type is most common only large defects require surgery |
|
|
|
late diastolic blowing murmur @ apex
opening snap loud S1 A fib, L atrial enlargement, PH |
Mitral stenosis: late diastolic blowing murmur @ apex
opening snap loud S1 A fib, L atrial enlargement, PH |
|
|
|
holosystolic murmur radiating to axilla
soft S1 LAE, PH, LVH |
Mitral regurgitation: holosystolic murmur radiating to axilla
soft S1 LAE, PH, LVH |
|
|
|
harsh systolic ejection murmur in aortic area, radiating to carotids
slow pulse upstroke S3/S4 ejection click LVH, cardiomegaly syncope c/ angina, CHF |
Aortic stenosis: harsh systolic ejection murmur in aortic area, radiating to carotids
slow pulse upstroke S3/S4 ejection click LVH, cardiomegaly syncope c/ angina, CHF |
|
|
|
early-diastolic decrecendo murmur @ apex
widened pulse P LVH, LV dilation S3 |
Aortic regurgitation: early-diastolic decrecendo murmur @ apex
widened pulse P LVH, LV dilation S4 |
|
|
|
mid-systolic click or late-systolic murmur
ass'd c/ panic disorder |
Mitral valve prolapse: mid-systolic click or late-systolic murmur
ass'd c/ panic disorder |
|
|
|
child c/ constant machine-like murmur in upper L sternal border
dyspnea +/ - CHF 4 RFs Tx |
PDA = L -> R shunt from aorta -> pulm artery
Hx of 1st trimester rubella, prematurity, female gender, high altitude Close c/ indomethacin (keep open c/ prostaglandin E1 in case of transposition of the great vessels, Tet of Fal, hypoplastic L heart) |
|
|
|
child c/ holosystolic murmur next to the sternum
#1 congenital heart defect |
VSD: child c/ holosystolic murmur next to the sternum
#1 congenital heart defect usually resolves spontaneously |
|
|
|
Congenital heart defect
Usually asymptomatic until adulthood Fixed, split S2 + palpitations most common type is _ |
ASD: congenital heart defect
Usually asymptomatic until adulthood Fixed, split S2 + palpitations most common type is secundum |
|
|
|
#1 cyanotic heart defect in CHILDREN
maternal RFs Tx |
Tetralogy of Fallot = PROVe
Pulm stenosis RVH Overriding aorta VSD Maternal RFs: PKU, CATCH22 Initial tx = PGI2; surgery later Cyanosis increases in 1st 2 yrs, reflects pulm stenosis severity (transposition of the great vessels = #1 cyanotic heart dz in newborns) |
|
|
|
Turner's syn is ass'd c/ congenital heart defect _
|
Turner's syn is ass'd c/ congenital heart defect: coarcation of the aorta
systolic murmur heard over mid-upper back rib notching on CXR radiofemoral delay |
|
|
|
Adult pt develops maculopapular drug rxn (or erythema multiforme) -> widespread erythema including mucous membrane-> sheds large sheets of skin
What are the 4 drugs that may have caused this? tx Unlike staph scalded skin syndrome... |
TEN = toxic epidermal necrolysis
2/2 CAPS: Carbamazepine Allopurinol Phenytoin Sulfonamides Tx: skin coverage, fluids Controversial - early steroids, IVIG Unlike SSSS, TEN involves full-thickness epidermal damage |
|
|
|
Drugs causing cholestasis:
if pt is a young woman: if pt has epilepsy... |
Drugs causing cholestasis:
OCPs (or pregnancy) Phenothiazines = class of neuroleptic antipsychotic drugs (Chlorpromazine, Thioridazine, Fluphenazine, Prochlorperazine) |
|
|
|
Urethritis
Conjunctivitis Arthritis |
Reiter's
2/2 Chlamydia trachomatis Doxycycline 100 mg PO BID x 7 days or Azithromycin 1g PO x1 day Erythromycin if pregnanct |
|
|
|
Prolonged bleeding time
+/ - prolonged aPTT => _ due to _ Diagnostic test Tx |
Prolonged bleeding time
+/ - prolonged aPTT => von Willebrand's dz WVF carries factor 8, mediates platelet adhesion Ristocetin cofactor assay: can vWF agglutinate platelets in vitro? Bleeding => DDAVP Menorrhagia => OCPs Avoid Asa, other anti-platelet drugs |
|
|
|
Prolonged aPTT, normal PT
Dz most likely to be _ Dx via _ Tx |
Hemophilia A = 90%
X-linked factor 8 defic MIXING STUDY: pt's plasma + normal plasma => corrects coagulopathy Mild dz=> desmopressin (DDAVP) + fluid restriction to prevent hyponatremia, release factor 8 Bleeding => clotting factors or cryo to 40% of normal concentration Dose BID for hemophilia A, QD for hemophilia B |
|
|
|
4 causes of microcytic hypochromic anemia
|
5 causes of microcytic hypochromic anemia:
1. Fe deficiency 2. thalassemia 3. lead poisoning 4. sideroblastic anemia (may be related to myelodysplasia or future blood dyscrasia) |
|
|
|
Ferritin <20 ug/L
MCV <100 |
Fe deficinecy anemia:
Ferritin <20 ug/L MCV >100 Absent Fe stores in bone marrow #1 cause = GI bleed |
|
|
|
Low TIBC
MCV >100 |
anemia of chronic dz:
low TIBC MCV >101 |
|
|
|
goal for fasting glucose during pregnancy
|
75-90
|
|
|
|
high Hct
redness itching HIGH erythropoeitin splenomegaly |
secondary polycythemia:
1. high Hct 2. redness 3. itching 4. HIGH erythropoeitin 5. splenomegaly Tx = phlebotomy |
|
|
|
African-American soldier is in Vietnam, gets sick after taking quinine.
possible explanation... |
G6PD deficiency -> RBCs susceptible to oxidative stress
X-linked R infection, metabolic acidosis, fava beans, antimalarials, nitrofurantoin, salicylates, sulfa drugs/dapsone -> hemolysis -> anemia, jaundice, dark urine heinz bodies, bite cells |
|
|
|
Heinz bodies
Bite cells Anemia Jaundice |
G6PD deficiency:
Heinz bodies Bite cells Anemia Jaundice |
|
|
|
Bacterial meningitis in pt <1 month old:
Organisms Tx |
Bacterial meningitis in pt <1 month old:
Grp B strep, E. coli/GNRs, Listeria ampicillin AND cefotaxime(3G) or gentamycin |
|
|
|
bacterial meningitis in baby <1 month old:
3 most common organisms empiric tx if no rash, assume organism is _ |
GBS => no rash
E coli/GNRs Listeria Amp + 3G (e.g. Cefotaxime) or Gent |
|
|
|
Arthritis:
Synovial WBC 10,000-50,000 suggests _ Synovial WBC >50,000 suggests _ |
Crystal arthritis -> synovial WBC 10,000-50,000
Septic arthritis -> synovial WBC >50,000 (staph, gonococcus, pneumococcus, strep viridans, strep pyogenes, gram (-) ...) |
|
|
|
What is wrong c/ this person?
Fever, chills w/in 12 hrs of transfusion Caused by _ Tx _ |
Leukoagglutinin reaction
Fever, chills w/in 12 hrs of transfusion Caused by antigens on WBCs > cytokines formed during blood storage Tx = acetaminophen, diphenydramine Corticosteroids in severe cases |
|
|
|
Elderly pt c/
Raynaud's Neuro changes (AMS, periph neuropathy, blurred vision) Elevated ESR, uric acid, LDH, alk phos Dz Mechanism is _ Precursor is _ Dx by _ Tx _ |
Waldenstrom's macroglobulinemia
= a malignant monoclonal gammopathy HIGH IgM -> hyperviscosity, cold agglutinin dz Causes auto-immune hemolysis, amyloidosis MGUS = precursor to Waldenstrom's and mult myeloma Dx: BM bx => abnl plasma cells, PAS(+) IgM deposits = Dutcher bodies Tx: plasmapheresis to reduce IgM Chemotx |
|
|
|
Dilated cardiomyopathy:
3 main causes |
Dilated cardiomyopathy is 2/2:
Alcohol abuse Myocarditis Doxorubicin |
|
|
|
Elevated neutrophils, metamyelocytes
WBC >100,000 Low Alk Phos High LDH, uric acid, B12 Splenomegaly t[9;22] ± acute blast crises or hyperviscosity sx |
CML
Philadelphoia chromosome = t[9;22] High neutrophils, metamyelocytes Low alk phos may accelerate to AML via "blast crisis" |
|
|
|
Tx for trigeminal neuralgia
|
carbamazepine
|
|
|
|
middle aged woman c/ vaginal complaint
hyperkeratotic, erosive, or papulosquamous lesion(s) flat-topped polygonal papules lesions @ sites of trauma lesions on mucous membranes have white stripes Intense pruritus, soreness discharge |
vulvar lichen planus
band of T-lymphocytes @ dermal-epidermal junction c/ damage to basal layer Tx: mild => topical steroids Severe => systemic steroids Oral mucosa => tretinoin gel |
|
|
|
Abx causing peripheral neuropathy
|
Isoniazid
Ethambutol Aminoglycosides |
|
|
|
elevated D-dimers
low fibrinogen low platelets elevated PT |
DIC:
elevated D-dimers low fibrinogen low platelets elevated PT |
|
|
|
tx for herpetic neuralgia
|
acyclovir
|
|
|
|
SLE:
2 lab tests that are most specific can be caused by 2 drugs __ lab test that indicates a drug etiology |
SLE:
anti-dsDNA, anti-Sm Ab's = most specific can be caused by procainamide = class 1a = mod Na channel blocker to prolong purkinje repolarization (A flutter/fib, PSVT, V tach) Hydralazine = arteriolar dilator to decrease afterload (CHF or to prevent reflex tachycardia c/beta blocker) anti-histone Ab's => drug etiology |
|
|
|
Pancreatitis:
main causes presentation lab changes _ correlates c/ poor prognosis |
Pancreatitis:
EtOH, gallstones > hypertriglyceridemia, hypercalcemia, drugs (steroids, azothioprine), virus (coxsackie, mumps) abrupt onset of steady, severe pain that radiates to the back s/ guarding, rebound +/ - hypocalcemia Amylase rises before lipase Hypocalcemia => poor prognosis |
|
|
|
Malabsorbtion
(+) fecal D-xylose |
Malabsorbtion c/ (+) fecal D-xylose => intestinal etiology
(not pancreatic insufficiency) |
|
|
|
Celiac sprue is diagnosed via _
|
Celiac sprue is diagnosed via biopsy
|
|
|
|
Charcot's triad is ...
If you add Raynaud's pentad... |
Charcot's triad = acute cholangitis:
1. Fever 2. Severe jaundice 3. RUQ pain Raynaud's pentad = suppurative cholangitis/sepsis 4. AMS 5. Hypotension |
|
|
|
What are the RFs for CAD?
|
Male >44
Female >54 HTN Cigarettes HDL <40 (>60 is neg. RF) Fam hx CAD in M<55, F<65 |
|
|
|
Elderly pt c/ LLQ pain, rebound tenderness , guarding , diminished bowel sounds, fever
Dz Dx Tx: for inflamation, bleeding, or perforation |
Diverticulitis
Diagnosed by AXR to r/o free air, ileus, obstruction; other options are barium enema, colonoscopy No colon/sigmoidoscopy in early dz b/c of perforation risk NPO, NG tube, broad-spec abx (metronidazole+ fluoroquinolone or gen 2/3 cephalosporin) Bleeding => usually stops. If not, angiography + embolization or surgery Perforation => resection + temporary colostomy c/ Hartmann's pouch + mucus fistula |
|
|
|
RLQ pain
early abdominal pain, nausea later focal pain c/ rebound tenderness, vomiting, mild fever Etiology: 2 most common Tx: what to do under certain circumstances |
Appendicitis:
RLQ pain early abdominal pain, nausea later focal pain c/ rebound tenderness, vomiting, mild fever Tx: NPO, IVF, abx c/ gram (-), anaerobic coverage Perforation => abx until pt afebrile + normal WBC -> close wound via delayed primary closure Appendectomy -> explore abdomen if appendicitis not found Abcess => broad-spec abx, percutaneous drainage, elective appy 6-8 wks later |
|
|

Indurated, erythematous, painful lesions (often pretibial)
Heal spontaneously s/ ulceration +/- fever, joint pain Dz Causes |
Erythema nodosum = a panniculitis 2/2:
Infection: Strep, Coccidioides, Yersinia, TB Drugs: sulfonamides, abx, OCPs Chronic inflamm dz: sarcoid, Crohn's, UC, Behcet's Indurated, erythematous, painful lesions (often pretibial) Heal spontaneously s/ ulceration +/- fever, joint pain |
|
|
|
Pt has fluctuant cervical LN.
What 2 organisms are most likely? Do I+D followed by what antibiotic? (3 options) |
Strep vs. Staph
Dicloxacillin Cephalexin Clindamycin |
|
|
|
vomiting does not relieve abdominal pain => 2 possibilities
|
vomiting does not relieve abdominal pain =>
GU disease strangulated bowel |
|
|
|
constant epigastric pain that worsens with eating => 2 possibilities
|
constant epigastric pain that worsens with eating =>
chronic gastric ulcer gastric carcinoma |
|
|
|
Hereditary spherocytosis:
inheritance test MCV is _ MCHC is > _% |
AD
osmotic fragility test (not specific) MCV normal to slightly low MCHC> 37% |
|
|
|
abdominal pain that increases while reclining, decreases when sitting up suggests the lesion is located _
|
RETROPERITONEAL abdominal pain increases while reclining, decreases when sitting up suggests…
|
|
|
|
abdominal causes of neck/shoulder pain
|
diaphragmatic irritation -> neck/shoulder pain:
liver abscess perforated gastric ulcer |
|
|
|
diabetes drug that contributes to lactic acidosis => not appropriate for renal failure or liver failure pts
|
metformin
|
|
|
|
What are the 3 causes of microangiopathic hemolytic anemia?
How to tell them apart... |
1. HUS:
<2 y/o or pregnant Previous E. coli diarrhea Hematuria High Cr Severe: dialysis, transfuse 2. TTP Young adult Proteinuria tx: NSAIDS, plasmapheresis NO platelets 3. DIC PT >15 sec, aPTT >25 sec |
|
|
|
pt c/ bacterial meningitis is >60 years old, an alcoholic, or chronically ill
4 common organisms empiric tx |
Pneumococcus
GNRs Listeria Meningococcus Amp + Vanc + Cefotaxime or Ceftriaxone |
|
|
|
Pt c/ fever, cough, malaise, arthritis, uveitis.
Increased serum ACE, Ca2+ Dz Tx |
Sarcoidosis = GRUELING
Granulomas, aRthritis, Uveitis, Erythema nodosum, Lymphadenopathy, Interstitial fibrosis, Negative TB test, Gammaglobulinemia Tx: corticosteroids for constitutional sx, hypercalcemia, extrathoracic dz |
|
|
|
mucosal inflammation affecting rectum +/ - colon
pseudopolyps increased risk of colon cancer Disease Tx |
Ulcerative colitis:
mucosal inflammation affecting rectum +/ - colon pseudopolyps increased risk of colon cancer Surgery is curative |
|
|
|
remove colon polyps found on colonoscopy if:
shape size other characteristics |
remove colon polyps found on colonoscopy if:
>1 cm pedunculated villous adenoma dysplastic ulcerative |
|
|
|
most common locations for colon cancer
|
sigmoid colon, rectum = most common locations for colon cancer
|
|
|
|
male pt c/o recurrent oral and genital ulcers, ocular inflamm
hx of R-sided colitis, auto-immune dz |
Behcet's:
M>F. Triad of recurrent oral and genital ulcers, ocular inflamm Colitis in 30% Dermatitis, erythema nodosum, thrombophlebitis, cerebral involvement Ass'd c/ auto-immune dz, arthritides, vasculitites |
|
|
|
#1 solid tumor in men 15-35 y/o
Tx (and how this depends on type) |
testicular = #1 solid tumor in men 15-35
Seminoma = most common AND radiosensitive otherwise => unilateral orchiectomy +/- rad, chemo main RF = cryptorchidism Lymphatics -> retroperitoneal LNs near renal veins AFP => yolk sac tumor betaHCG => choriocarcinoma Leydig tumors secrete testosterone |
|
|
|
#1 primary testicular tumor
Tx prognosis |
germ cell seminoma = #1 primary testicular tumor
Tx: unilateral orchiectomy + radiation Good prognosis |
|
|
|
_ -> testicular aching, infertility, dragging sensation
etiology Tx |
Varicocele
= varicosity of pampiniform venous flexus testicular aching, infertility, dragging sensation Tx: surgery |
|
|
|
HIV prophylaxis:
add anti-retrovirals when CD4 count < _ Regimen is ... |
HIV prophylaxis: when CD4 count < 350 or pt symptomatic
3 drugs: Nucleoside/tide RTIs Non-nucleoside RTIs Protease inhibitors |
|
|
|
HIV prophylaxis:
add trimethoprim-sulfamethoxazole or inhaled pentamidine for _ when CD4 count < _ |
HIV prophylaxis:
add trimethoprim-sulfamethoxazole or inhaled pentamidine for Pneumocystis carinii when CD4 count < 200 |
|
|
|
HIV prophylaxis:
add ganciclovir or foscarnet for _ when CD4 count < _ Retinitis -> floaters, field changes, retinal detachment AIDS cholangiopathy Pneumonitis CNS: polyradiculopathy, transverse myelitis, subacute encephatitis, periventricular califications |
HIV prophylaxis:
add ganciclovir for CMV when CD4 count < 50 |
|
|
|
PPD thresholds for:
HIV+ Otherwise ill Healthy, <35 y/o |
PPD thresholds for:
HIV+: >5mm Otherwise ill: >10mm Healthy, <35 y/o: >15 mm |
|
|
|
Tx for (+) PPD c/ (-) CXR
2 drug side effects, way to prevent one |
Tx for (+) PPD c/ (-) CXR => Isoniazid alone
SE's: hepatitis, peripheral neuropathy (prevent c/ B6 = pyridoxine) |
|
|
|
#1 pneumonia in teens, young adults
|
Mycoplasma pneumoniae = #1 pneumonia in teens, young adults
|
|
|
|
Parkinson's:
Substantia nigra has overactive _ neurons and underactive _ neurons What is the classic tetrad? Tx: 1st line in early disease: _ mainstays are _ MAOB _ is neuroprotective COMT inhibitor _ increases amt of _ to brain For temor sx: _ |
1. bradykinesia, inc. shuffling gait
2. postural instability 3. resting tremor 4. rigidity (cogwheeling is 2/2 rigidity + tremor) Tx: 1st line dopamine agonists: ropinerole, pramipexole Mainstays: levodopa, carbidopa Entacapone increases levodopa to brain, may decrease motor fluxuations Selegiline is neuroprotective Anti-cholinergic = benztropine decreases tremor |
|
|
|
Young male c/ hemoptysis, dyspnea, renal failure
Dz _ seen on kidney bx Tx (2 drugs) |
Goodpasture's
anti-GBM Ab's tx: steroids, cyclophosphamide Young male c/ hemoptysis, dyspnea, renal failure |
|
|
|
#1 cause of aspiration pneumonia
Tx |
anaerobes, e.g. Bacteroides
Tx: clindamycin, ceftriaxone + azithromycin |
|
|
|
Epstein Barr virus:
Dx |
Epstein Barr virus:
Dx: (+) hetrophil Ab test sore throat lymphadenopathy hepatosplenomegaly Atypical lymphocytes |
|
|
|
Antibiotic prophylaxis started for ladies c/ _ UTI's/ year
|
Antibiotic prophylaxis started for ladies c/ 3 UTI's/ year
|
|
|
|
Sporadic phakomatosis that involves MR, seizure, visual impairment, port wine stain in trigeminal distribution
|
Surge Weber:
bridging veins from sagital sinus absent on one side sporadic phakomatosis = CNS dz that has skin + retina sx (others; Neurofibromatosis, Tuberous sclerosis, Ataxia telangiectasia, von Hippel-Lindau disease) |
|
|
|
Organism most likely to cause:
surgical wounds |
Staph aureus = most likely to cause:
surgical wounds |
|
|
|
Organism most likely to cause:
post-surgical parotiditis |
Staph aureus = most likely to cause:
post-surgical parotiditis 20% mortality |
|
|
|
Organism most likely to cause:
heart murmur in IV drug user |
Staph aureus = most likely to cause:
heart murmur in IV drug user |
|
|
|
Pt c/ MR, apnea, deafness, holoprosencephaly (fusion of cerebral hemispheres), myelomeningocele, CV abnormalities, rocker-bottom feet.
Disease Prognosis |
Patau = trisomy 13
Early pediatric death MR, apnea, deafness, holoprosencephaly (fusion of cerebral hemispheres), myelomeningocele, CV abnormalities, rocker-bottom feet. |
|
|
|
Organism most likely to cause:
red ear canal or ear |
Pseudomonas = most likely to cause:
red ear canal or ear |
|
|
|
test used to confirm Hep C diagnosis in pt c/ anti-HCV Ab's, esp. a pt c/ hypergammaglobulinemia (high false postitive rate)
|
RIBA = recombinant immunoblot assay confirms HepC dx in pt c/ (+) enzyme immunoassay test (which only has 50% specificity)
|
|
|
|
Organism most likely to cause:
infected bite from cat or dog |
Pasturella = most likely to cause:
infected bite from cat or dog |
|
|
|
Organism most likely to cause:
infected human bite |
Eikenella = most likely to cause:
infected human bite |
|
|
|
2 Organisms most likely to cause cellulitis
Empiric tx |
Group A Strep > Staph aureus
Beta-lactamase R pen: nafcillin, cloxacillin H flu coverage for < 5 y/o 3rd gen cephalosporin? |
|
|
|
3 Organisms most likely to cause:
infection after splenectomy |
Strep pneumo, H. influenzae, Neisseria meningidis = most likely to cause:
infection after splenectomy |
|
|
|
Asian female 15-30 y/o
unable to feel a pulse on arms concern a/b neurologic changes Dz complications in 2 systems... tx |
Takayasu's arteritis:
vasculitis of aortic arch + branches Carotid dz => neuro signs, stroke CHF Tx: corticosteroids +/- cyclophosphamide |
|
|
|
Pt c/ chest pain, increased JVP
Systolic BP drops >10 mmHg on inspiration ECG: PR depression and diffuse ST elevation -> T wave inversion Virus most likely to cause this is _ Would be treated with _ |
Coxsackie B virus
Aspirin/NSAIDS PERICarditis: Pulsus paradoxus ECG changes Rub Increased JVP Chest pain |
|
|
|
Chronic osteomyelitis => 3 organisms
|
S. aureus
Pseudomonas Enterobacteriaceae |
|
|
|
(+) HepBsAg => _
|
(+) HepBsAg => infectivity, active disease
|
|
|
|
(+) anti-HepB Ab => _
|
(+) anti-HepB Ab => immunity
|
|
|
|
Boy 5-20 y/o c/ fam hx "kidney problems"
Nerve deafness Asymptomatic hematuria Eye disorder e- microscopy => GBM splitting Dz Prognosis |
Alport's = a hereditary GBM nephritis
Progresses to renal failure Anti-GBM nephritis may occur after transplant |
|
|
|
Pt c/ at least 3 tetanus toxoid shots over a lifetime gets toxoid if...
|
clean wound, last shot >10 yrs ago
dirty/severe wound, last shot >5 yrs ago |
|
|
|
Do Rh Ab testing on...
|
1st prenatal visit AND
28 weeks in unsensitized mother c/ Rh(+)/unk partner |
|
|
|
HTN in pregnancy:
start @ BP of _ or if pt already on anti-HTN meds 2 drugs to use... |
start tx @ 150/95
Labetalol: blocks alpha1, beta1/2. lowers BP s/ increase in HR Methyldopa: pre-synaptic adrenergic blocker. SE = coombs (+) hemolytic anemia, hepatitis |
|
|
|
Impetigo:
Common is usually located @ _ and can be complicated by _ Bullous is usually 2/2 _ and located @ _ and can evolve into _ |
Impetigo:
Common: pustules, crusts on face. Ass'd c/ strep acute glomerulonephritis. Bullous: fingers, toes. usually S. aureus. Can evolve into SSSS cephalexin treats both Grp A Strep and Staph aureus |
|
|
|
What is pickwickian syndrome?
|
obesity hypervent. syn c/ hypercapnia, acidosis 2/2 low lung compliance
tx: vent support, wt loss, O2, progestins (resp stimulant) |
|
|
|
3 main causes of Ca > 10.2 mg/dL (hypercalcemia)
main signs of hypercalcemia Tx Do not use _ |
1. Hyperparathyroid
2. Malignancy: breast, sq cell, mult myeloma sarcoidosis -> fractures, kidney stones, anorexia/constipation, weakness/fatigue, AMS Short QT tx: saline, furosemide Severe cases: calcitonin, bisphosphonate, glucocorticoid, dilaysis NOT thiazides => increase Ca absorbtion |
|
|
|
Pt c/ cystic brown bone tumors
PTH >25 pg/mL Underlying dz is _ Ass'd c/ genetic syndromes _ Skeletal complication mentioned above is _ Psych drug _ or diuretic _ may aggravate this condition |
Hyperparathyroidism
Primary: 80% adenoma, 15% hyperplasia, 5% caricinoma (but PTH usually <25 pg/mL in cancer) Ass'd c/ MEN1, 2A Secondary: most common cause is phosphate retention in chronic renal failure Osteitis fibrosa cystica = Recklinghausen's dz of bone = osteoclastic bone resorption 2/2 excess PTH -> paratrabecular fibrosis, cystic brown tumors |
|
|
|
low Ca2+
high PO4- |
hypoparathyroidism:
usually s/p thyroidectomy low Ca2+ c/ high PO4- |
|
|
|
Alk phos is produced in 3 places …
|
Alk phos is produced in:
Bile ducts Bones Placenta |
|
|
|
3 groups of people are expected to have:
elevated alk phos normal AST, ALT |
Kids, pregnant women, and elderly:
elevated alk phos normal AST, ALT |
|
|
|
AST, ALT both > 250 IU/L => _
|
AST, ALT both > 250 IU/L => infectious hepatitis
|
|
|
|
Young pt c/ recent URI
Now has rash on extensor surfaces + buttocks, abdominal pain +/- arthralgias of hips/knees/ankles, melena, hematuria Bx: granulocytes in walls of small vessels Dz = a _-type nephropathy Tx |
HSP => supportive tx; steroids for renal or severe dz
IgA nephropathy (normal C3) + systemic vasculitis 2 of 4 criteria: 1. palpable purpura 2. age <21 3. bowel angina 4. bx: granulocytes in arteriole/venule walls |
|
|
|
Young adult c/ hx of UC (less commonly has Crohn's)
C/o jaundice, pruritus, fatigue MRCP/ERCP => multiple bile duct strictures "onion-skinning" on bx Dz Tx Increased risk of _ |
Primary sclerosing cholangitis
Tx: high-dose ursodeoxycholic acid Endoscopic dilation + short-term stenting of bile duct strictures Liver tx RF for cholangiocarcinoma |
|
|
|
Pt c/ recurrent HSV infection of the lip
Now c/ annular, erythematous, pruritic rash Has plaques, papules, and target appearance On palms and soles +/- mucous membranes |
Erythema multiforme
2/2 HSV infection of lip > mycoplasma, drugs Tx: symptomatic - antipruritics for minor cases; treat severe cases like a burn. NO benefit to systemic cortiosteroids.HSV => acyclovir supression therapy may decrease rash frequency |
|
|
|
Hyaline casts in urine => _
WBC casts +/- hyaline casts => _ |
Hyaline casts => pre-renal azotemia, e.g. volume depletion
WBC casts +/- hyaline casts => pyelonephritis = post-renal failure |
|
|

tx for septic arthritis in a child
if it is in the hip... |
nafcillin
Hip = surgical emergency 2/2 risk of avascular necrosis |
|
|
|
Child c/ recent e. coli diarrheal illness
now c/ acute renal failure, hematuria hemolytic anemia thrombocytopenia Dz, Tx |
Hemolytic uremic syndrome:
Child c/ recent e. coli diarrheal illness now c/ acute renal failure, hematuria hemolytic anemia thrombocytopenia tx: supportive |
|
|
|
Pt c/ hx of autoimmune dz (pernicious anemia, vitiligo, SLE)
Sx of hypothyroidism (+) anti-_ Ab's, anti-_ Ab's Dz Type _ hypersensitivity Tx: _ Myexedema coma => IV _ + IV _ if _ has not been excluded |
Hashimoto's thyroiditis
type 4 hypersensitivity: T cell infiltration (+) anti-TPO Ab's, anti-microsomal Ab's Tx: levothyroxine Myexedema coma => IV levothyroxine + IV hydrocortisone if adrenal insufficiency has not been excluded |
|
|
|
_ toxicity causes hepatic necrosis
Tx = _ |
Acetaminophen toxicity causes hepatic necrosis
Tx = N-Acetylcysteine |
|
|
|
Anion gap equation = _
Normal anion gap is _ 8 main causes of anion gap metabolic acidosis (remember mnemonic) |
Anion gap = Na - Cl - HCO3
Normal = 8-12 mEq/L MUDPILES: Methanol Uremia DKA Paraldehyde Intoxicaiton Lactic acidosis Ethylene glycol Salicylates resp compensation: pCO2 decrease = 1.5(HCO3) + 8 |
|
|
|
_ toxicity causes muscarinic agonism
Tx = 2 drugs |
Organophosphate toxicity causes muscarinic agonism
Tx = Pralidoxime, Atropine = acetylcholinesterase ACTIVATORS |
|
|
|
heaped-up verrucous genital lesions that are flat, velvety
Dz Tx |
Condyloma lata
Secondary syphilis Tx: penicillin |
|
|
|
Tx for diverticulitis flare not requiring surgery
Avoid _ |
NPO, NG
Broad spec abx: metronizazole + fluoroquinolone or 2/3G cephalosporin Avoid barium enema, flex sig |
|
|
|
surgically elevate skull fractures that _
|
surgically elevate skull fractures that are depressed >1 cm
|
|
|
|
fracture to _ region of skull ->
Battle's sign = bruising over mastoid process behind ear periorbital bruising CSF leak +/ - blood behind eardrums |
Basilar skull fracture->
Battle's sign = bruising over mastoid process behind ear periorbital bruising CSF leak +/ - blood behind eardrums |
|
|
|
surgically explore a penetrating wound to neck zone _, which is located _
|
surgically explore a penetrating wound to neck zone 2 = b/w clavicle and lower mandible
|
|
|
|
appropriate imaging for blunt head trauma
|
blunt head trauma =>
head CT to r/o hemorrhage +/ - LP to r/o occult bleed lateral C-spine films |
|
|
|
Amlodipine is a _= acting drug in the _ class
Used for HTN, angina Preferentially affects _, not _ |
Amlodipine
dihydropyradine Ca-channel blocker Relaxes arterial sm muscle, does not act on heart Reduces BP, improves blood flow to heart |
|
|
|
Tx for flail chest
|
Tx for flail chest:
analgesia pulmonary toilet |
|
|
|
40-60 y/o M weekend warrior
movement involving sudden push-off c/ foot -> pain in calf radiating to knee and ankle |
tear of plantar flexor muscles (gastricnemius, soleus)
40-60 y/o M weekend warrior movement involving sudden push-off c/ foot -> pain in calf radiating to knee and ankle pain c/ compression of muscle bellies plantar flexion still possible, c/ pain |
|
|
|
bowel obstruction
abdominal mass elevated amylase s/p trauma |
Duodenal hematoma:
bowel obstruction abdominal mass elevated amylase s/p trauma Dx by CT |
|
|
|
Tx for pelvic fracture c/ stable pelvic hematoma
|
NO exploration for pelvic fracture c/ stable pelvic hematoma
|
|
|
|
20 y/o man presents with idiopathic mild unconjugated hyperbilirubinemia.
what dz? |
Gilbert's dz
|
|
|
|
Volkmann's contracture
= contraction of fingers or wrist 2/2 vascular insufficiency 2 causes tx |
Volkmann's contracture
= contraction of fingers or wrist 2/2 vascular insufficiency 2/2 severe elbow injury, improper tourniquet use tx = immediate decompression |
|
|
|
_ = pulp space infection of distal finger pad
tx |
Felon = pulp space infection of distal finger pad
tx = incise + drain |
|
|
|
2-3 day old baby c/ purulent eye discahrge, swollen eyelids
|
gonococcal conjunctivitis
|
|
|
|
Diminished distal pulses after posterior knee dislocation
|
Popliteal artery occlusion =>
diminished distal pulses s/p posterior knee dislocation Dx: angiogram |
|
|
|
Humerus fracture complication
|
Humerus fracture can cause radial nerve injury -> wrist drop
|
|
|
|
Tx for simple closed femur fracture
|
Simple closed femur fracture => traction only
|
|
|
|
#1 carpal fracture
presentation complication tx |
Scaphoid = #1 carpal fracture
"snuffbox" tenderness risk of avascular necrosis -> osteoarthritis tx = immobilization, repeat x-ray in 3 wks |
|
|
|
fracture 2/2 "fall onto outstretched hand"
|
"fall onto outstretched hand" -> colles fracture
#1 wrist/distal radius fracture tx: closed reduction, splinting |
|
|
|
tx for cancer-associated anorexia
|
megestrol acetate = a progestin
|
|
|
|
Coomb's test:
(+) direct Coomb's means ... (+) indirect Coomb's meanss... |
(+) direct Coomb's => Ab's are bound to the surface of pt's RBCs
Indirect Coomb's is done in pregnant pts and prior to transfusion . (+) test => Ab's against RBCs of a particular antigenicty are present in pt's SERUM |
|
|
|
pink-red-brown scaly spots on the back in a "Christmas tree" distribution
larger patch -> general eruption Dz Etiology Tx |
Pityriasis rosea:
HSV infection (HHV-7) Dx: clinical exam, KOH Usually heals c/ tx in 2-3 wks Can use skin lubrication, topical antipruritic, antihistamine Severe cases: corticosteroids oval/round red-brown spots on back "Christmas tree" distribution larger patch -> general eruption |
|
|
|
Correction of Ca2+ for albumin:
for each drop of _ g/dL in albumin from _ g/d, expect Ca2+ to decrease by _ mg/dL (_% of Ca2+ is albumin-bound, _% is ionized) |
for every decrease in albumin of 1 g/dL from 4 g/dL, expect Ca2+ to decrease 0.8 mg/dL.
(40% of Ca2+ is albumin-bound, 40% is ionized) |
|
|
|
Sudden severely blurred vision in one eye -> excrutiating pain
High intraocular P |
Acute glaucoma:
Sudden severely blurred vision in one eye -> excrutiating pain High intraocular P |
|
|
|
Sudden painless unilateral blindness
Called _ if it resolves in a few minutes Pale retina c/ red spot on macula _ may save pt's vision r/o _ |
Central retinal artery occlusion:
Sudden painless loss of all vision in one eye Amaurosis fugax if it resolves in a few minutes Pale retina c/ red spot on macula Tx: thrombolysis of opthalmic artery w/in 8 hrs of sx. Drainage of anterior chamber -> reduce intraocular P IV acetazolamide => improve retinal perfusion r/o temporal arteritis |
|
|
|
Appearance of gray cloud in visual field
Minimal to catastropic vision loss |
Retinal detachment:
Appearance of gray cloud in visual field Minimal to catastropic vision loss, depending on where retina detaches |
|
|
|
diabetes drug that increases in blood level if pt has renal failure (alright c/ liver failure pts)
|
Glyburide (longer-acting)
|
|
|
|
Resect non-small cell lung cancers unless: (3 reasons)
|
Resect non-small cell lung cancers unless:
bloody pleural effusion local invasion into major nerves, vessels distant metastases |
|
|
|
peripheral lung cancer
no smoking association cardiovascular sx _ type is ass'd c/ multiple nodules, insterstitial infiltrates, lots of sputum |
Adenocarcinoma
Bronchoalveolar type = sputum, interstitial infiltrates, multiple nodules Dx: FNA b/c of peripheral location |
|
|
|
lung mass:
male > 60 y/o peripheral location calcifications seen on CXR fat seen on CT |
Hamartoma:
male > 60 y/o peripheral location "popcorn" calcifications seen on CXR fat seen on CT |
|
|
|
Nasopharyngeal cancer:
typical population 2 RF's = population _, hx of _ Tx |
Nasopharyngeal cancer:
young adults RFs: Asians, Epstein Barr virus Tx: radiation tx, radical neck dissection if nodes palpable |
|
|
|
persistant hoarseness
hx of smoking, EtOH Disease Most common sub-type Tx (hoarseness is due to _) |
Laryngeal cancer
persistant hoarseness 2/2 recurrent laryngeal nerve involvement? 90% sq cell carcinoma 90% (+) hx of smoking, EtOH Tx: surgery or radiation |
|
|
|
Acute cholecystitis: RUQ pain, N/V, fever
workup what organisms can cause superinfection? therapy |
#1: do Ab US => stones, sludge, thickened wall, pericholecystic fluid, gas in gallbladder
if US is equivocal then -> #2: HIDA scan = radionuclide cholescintigraphy: nonvisualization on HIDA scan => acute cholecystitis If no stones => acalculous (debilitated pts, s/p trauma/burn) Superinfection: EEEK (E coli, Enterobacter cloacae, Enterococcus, Klebsiella) Tx: 1. IV abx, fluids 2. Cholecystectomy w/in 72 of sx c/ pre-op ERCP ot intra-op cholangiogram to r/o common bile duct stones Can wait 4-6 wks for stable pts w/ comorbidities - 50% will resolve s/ surgery |
|
|
|
one-sided hearing loss
tinnitus vertigo signs of cerebellar dysfx Disease location Tx If bilateral, then suspect _ |
Acoustic neuroma:
@ CN8, cerebellopontine angle Surgical resection Neurofibromatosis 2: AD. bilat acoustic neuromas OR 2 neurofibromas, meningiomas, gliomas, or schwannoma. +/- seizures, skin nodules, cafe au lait spots |
|
|
|
episodic vertigo
unilateral tinnitus, hearing loss |
Meniere's syndrome:
episodic vertigo unilateral tinnitus, deafness |
|
|
|
initial screening test for primary hyperaldosteronism
confirm dx c/ _ then do adrenal CT to look for adenoma |
plasma aldosterone/renin > 30
confirm dx c/ IV saline => aldosterone not suppressed then do adrenal CT to look for adenoma |
|
|
|
proximal muscle weakness => difficulty getting out of chair or up stairs
no effect on extraocular muscles elevated CPK Disease? Dx via … |
Polymyositis:
proximal muscle weakness no effect on extraocular muscles elevated CPK, irregular EMG Dx by muscle bx |
|
|
|
purple upper eyelids
red papules on the back of knuckes proximal muscle weakness no effect on extraocular muscles elevated CPK Disease? Increased risk of _ |
Dermatomyositis = polymyositis + skin manifestations
purple upper eyelids red papules on the back of knuckes proximal muscle weakness no effect on extraocular muscles elevated CPK increased risk of cancer |
|
|
|
large calves 2/2 pseudohypertrophy
Dz Life expectancy Western blot Mental fx |
Duchenne muscular dystrophy
X-linked absence of dystrophin look for large calves 2/2 pseudohypertrophy X-linked R Life expectancy in teens MR common Western => dystrophin in markedly low or absent |
|
|
|
woman 20-40 y/o
ptosis, diplopia general muscle fatigability esp. @ end of day Disease mechanism Dx Tx |
Myasthenia gravis
muscles fatigue quickly extraocular muscles affected 70% c/ hyperplastic thymus 10% c/ thymoma Auto-ab's to acetyl choline R's Dx: edrophonium improves sx Tx: anti-cholinesterase (pyridostigmine, neostigmine) Thymectomy |
|
|
|
muscles get stronger c/ repeated movement
extraocular muscles usually unaffected +/ - severe autonomic dysfx Disease mechanism Ass'd c/ cancer _ Tx |
Lambert-Eaton:
paraneoplastic syn c/ small cell lung cancer Ab's block voltage-gated Ca2+ channels -> LOWERS ACh RELEASE at NMJ -> Ach accumulates c/ movement Tx: plasmapheresis, immunosupression e.g. prednisone |
|
|
|
Baby c/
constipation weak cry + smile hypotonia c/ poor head control +/ - symmetric descending paralysis |
Botulism toxicity if baby c/
constipation weak cry + smile hypotonia c/ poor head control +/ - symmetric descending paralysis |
|
|
|
Extraocular muscle paralysis ->
Flaccid paralysis -> Respiratory failure |
Botulism toxicity:
Extraocular muscle paralysis -> Flaccid paralysis -> Respiratory failure mental status intact w/in 48 hrs of eating home-canned food |
|
|
|
Dermatomal pain over lower extremities c/ sensory changes
Pain exacerbated c/ straight leg raise Disease Localized most commonly at _ Tx |
Lumbar disk herniation
most commonly at L5-S1 Dermatomal pain over lower extremities c/ sensory changes Pain exacerbated c/ straight leg raise Tx: rest, NSAIDs, lumbar laminectomy c/ discectomy |
|
|
|
symmetric distal extremity pain, paresthesias, loss of vibration sense
Disease Tx |
Diabetic neuropathy:
symmetric distal extremity pain, paresthesias, loss of vibration sense Amitriptyline, desipramine may improve sx |
|
|
|
ascending peripheral paralysis
may lead to resp failure CSF protein >100 mg/dL disease tx |
Guillain-Barre:
vaccine or ~1 week before ascending peripheral paralysis slow nerve conduction velocity may lead to resp failure NO corticosteroids early plasmapheresis or IV Ig may speed recovery |
|
|
|
ipsilateral motor weakness or paralysis
c/ loss of tactile, vibratory sensation loss of contralateral pain, temp sensation |
Brown-Sequard syndrome:
2/2 unilateral hemisection of spinal cord ipsilateral motor weakness or paralysis c/ loss of tactile, vibratory sensation loss of contralateral pain, temp sensation |
|
|
|
cystic cavity in spinal cord
ass'd c/ mild cerebellar herniation in Chiari I malformation +/ - Brown-Sequard syndrome Disease Tx |
Syringomyelia, communicating type
cystic cavity in spinal cord ass'd c/ mild cerebellar herniation in Chiari I malformation +/ - Brown-Sequard syndrome Tx: shunts, cyst aspiration |
|
|
|
cystic cavity in spinal cord
ass'd c/ trauma +/ - Brown-Sequard syndrome Disease Tx |
Syringomyelia, non-communicating type
cystic cavity in spinal cord ass'd c/ trauma +/ - Brown-Sequard syndrome Tx: shunts, cyst aspiration |
|
|
|
Diplopia
Dysarthria = unclear speech articulation Homonymous (same halves of the visual field) hemianopsia |
Vertebral artery embolism:
Diplopia Dysarthria Homonymous hemianopsia |
|
|
|
Major head trauma ->
pt briefly loses consiousness lucid for several hours loses consiousness again typically 2/2 to _ Dx Tx |
Epidural hematoma:
Lateral skull fracture -> tears middle meningeal A. -> brief LOC -> lucidity -> LOC, hemiparesis, blown pupil Dx: CT => lens-shape density, may cross the midline Tx: surgery to avoid uncal or cerebellar herniation |
|
|
|
Injury 2/2 violent head motion
CT: crescent-shaped densities adjacent to skull that do NOT cross the midline Dz Tx |
Acute subdural hematoma
2/2 violent head motion CT: crescent-shaped densities adjacent to skull that do NOT cross the midline Tx: surgical decompression if pt is neurologically unstable or hematoma > 1 cm |
|
|
|
Head trauma ->
"worst headache of my life" +/ - altered mental status, photophobia, stiff neck Dz Dx Tx |
Subarachnoid hemorrhage
Head trauma -> "worst headache of my life" +/ - altered mental status, photophobia, stiff neck Confirm dx c/ CT or LP Tx: surgical clip ligation of any operable aneurysms |
|
|
|
Elderly pt c/ :
Dementia Ataxia Urinary incontinence |
Normal P hydrocephalus: Elderly pt c/ :
Dementia Ataxia Urinary incontinence Tx = CSF shunt |
|
|
|
CSF:
high PMNs Low glucose High protein Very high P |
Bacterial meningitis (e.g. Neisseria) => CSF:
high PMNs Low glucose High protein Very high P |
|
|
|
CSF:
high lymphocytes Low glucose High protein High P |
TB/ Fungal meningitis => CSF:
high lymphocytes Low glucose High protein High P |
|
|
|
CSF:
high lymphocytes Normal glucose High protein Normal -high P 3 organisms |
Viral meningitis
enterovirus: 6 mo - 6 y/o Coxsackie Echovirus CSF: high lymphocytes , Normal glucose, High protein, Normal -high P |
|
|
|
Female 20-40 y/o c/:
bilat lateral gaze deficit => diplopia nystagmus scanning speech spastic paraparesis incontinence CSF: high gamma globulin +/- high WBC Disease Dx Tx |
Multiple sclerosis:
internuclear opthalmoplegia => diplopia decreased visual acuity spastic paraparesis incontinence +/ - optic neuritis 2 MRI's: diffuse plaques 2/2 white matter demyelination + /- increased CSF Ig, oligoclonal bands Tx: ABC = Avonex/Rebif = interferon-alpha 1a Betaseron = interferon alpha 1b Copaxone = copolymer-1 (shifts Th1 -> Th2) |
|
|
|
Pt > 40 y/o c/:
Atrophy Fasiculations Spasticity Sparing voluntary muscles of eye, sphincter Mental status intact |
ALS = upper and lower motor neuron degeneration:
Pt > 40 y/o c/: Atrophy Fasiculations Spasticity Sparing voluntary muscles of eye, sphincter Mental status intact |
|
|
|
HIV+ pt c/:
foot paresthesias decrased vibratory and light touch sensation |
HIV+ pt c/:
foot paresthesias decreased vibratory and light touch sensation 2/2 to HIV or anti-virals e.g. zidovudine (AZT), didanosine (ddI) |
|

