![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
the primary fxn of the kidney is _________
|
the production of urine
or to control the volume and composition of the ECF and in doing so, urine is produced |
|
|
Symptoms of abnormal kidney fxn
|
weakness (due to increased plasma osmolarity)
vomiting coma (due to inability to remove acids) polypnea (resp compensation attempts to raise pH) muscle twitching (neuronal swelling in CNS) cardiac weakness (elevated K+) uremia or azotemia (urea and nitrogenous wate in blood) |
|
|
the kidneys are responsible for the regulation of
|
fluid volume and composition
fluid osmolarity and pH body metabolites urea erythropoietin renin vitamin d elimination of foreign substances |
|
|
4 basic mechanisms involved in the formation of urine
|
filtration
reabsorption secretion excretion |
|
|
filtration
|
the movement of a solution through a membrane from an area of high pressure to an area of low pressure
energy provided by the heart factors determining net movement - solute size - osmotic pressure - membrane pore size - pressure |
|
|
reabsorption
|
refers to direction (not mechanism)
the passive and active diffusion of water and solutes back into the blood stream from the nephron |
|
|
secretion
|
refers to those substances that are added to teh filtrate after filtration has occurred
|
|
|
what process is largely responsible for the ECF concentration of H+, K+, and HCO3-
|
secretion
|
|
|
excretion
|
refers to the production of urine
|
|
|
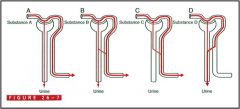
Substance A
- filtered Substance B - filtered & partially reabsorbed Substance C - filtered & totally reabsorbed Substance D - filtered & totally secreted |
|
|
what is the functional unit of the mammalian kidney?
|
the nephron
|
|
|
each nephron consists of
|
renal (malphigian) corpuscle
- glomerulus - bowman's capsule proximal convoluted tubule loop of henle distal convoluted tubule |
|
|
True or false
there are glomeruli in the medulla |
false
|
|
|
mammals that live in an environment where there is an abundance of water have _____ long looped nephrons than those that have little drinking water
(more or less) |
less
|
|
|
what are the major differences b/w glomerular capillaries and extrarenal capillaries
|
the hydrostatic pressure in the glomerulus remains nearly constant
the pressure in the glomerulus is much higher than in systemic capillaries glomerular capillaries are less permeable to protein than extrarenal capillaries so oncotic pressure rises as blood flows through the glomerulat capillaries |
|
|
_______ is the greatest driving force for filtration
|
a net pressure difference between a glomerular capillary and bowman's space
pressure taken into account - hydraulic pressure (from heart) - hydrostatic pressure (from height of column of fluid) - oncotic pressure (water drawing ability of a solution) |
|
|
what is the pressure in the renal pelvis?
how does urine move there? |
pressure is virtually zero
urine moves by peristaltic contractions through ureters into bladder |
|
|
formula for filtration
|
Puf = (Pgc - πgc) - (Pt - πt)
mean ultrafiltration pressure in glomerular capillaries = (glomerular capillary hydraulic pressure - glomerular capillary oncotic pressure) - (bowman's capsule hydraulic pressure - bowman's capsule oncotic pressure) |
|
|
In order for a substance to qualify as a marker for measuring GFR, it must
|
be freely filtered
be neither reabsorbed nor secreted in the nephron be easily measured in plasma and urine neither synthesized or metabolized in the kidney not have a direct effect on GFR |
|
|
The Pectineus muscle is supplied by which nerve?
|
Accessory Obturator nerve L3-4
|
|
|
a reduction in GFR will be signeded by _________ in BUN and Creatinine
|
an increase
|
|
|
an increase in urine flow has what effect on urine concentration?
|
decreases it
|
|
|
an increase in plasma concentration has what effect on urine concentration?
|
increases it.
|
|
|
At the thigh, these two nerves form the Medial Femoral Cutaneous Plexus
|
Great Saphenous nerve and Obterator nerve L2-4
|
|
|
______ is the first and most important step in the formation of urine
|
filtration
|
|
|
if the clearance for a substance is greater than the GFR, what happens to it?
|
it is secreted (net)
|
|
|
if the clearance for a substance is less than the GFR, what happens to it
|
there is a net reabsorption
|
|
|
when reabsorption occurs, fluid moves from where to where?
|
out of the tubular lumen
into the interstitium then into peritubular capillaries |
|
|
______ is the primary activity by which the body conserves what is important (such as glucose, Na+, amino acids, and electrolytes)
|
reabsorption
|
|
|
what do you need to know in order to calculate the amount of glucose reabsorbed
|
urine concentration of inulin
urine flow rate plasma concentration of inulin urine concentration of glucose plasma concentration of glucose amt reabsorbed = (GFR x Pglu) - (Uglu x V) |
|
|
the major feature of a Tm- transported molecule is what?
(TM = transport maximum) |
it is actively transported against a concentration gradient
|
|
|
give some examples of Tm-transported molecules
|
glucose
phosphate sulfate sugars amino acids uric acid albumin |
|
|
the reabsorption of urea is dependent on
|
the flow rate of fluid in the tubular system
as flow increases, urea reabsorption decreases |
|
|
secreted substances are transported from where to where?
|
from interstitium or peritubular capillaries
into the tubular system |
|
|
3 categories of secreted substances
|
active secretory mechanisms that exhibit a Tm limited transport capacity
active secretory mechanism that exhibit a gradient-time-limited capacity passive transport down electrical and/or chemical gradients |
|
|
What 5 things must be known in order to calculate the quantity of PAH secreted
|
urine concentration of inulin
urine flow rate plasma concentration of inulin urine concentration of PAH plasma concentration of PAH quantity secreted = (Upah x V) - (Ppah x GFR) |
|
|
renal blood flow does what
|
delivers oxygen, nutrients, and hormones to the cells of the nephron
returns CO2 and reabsorbed H2O and solutes to the general circulation determines GFR modifies the rate of solute and H2O reabsorption by the PCT plays a role in the concentration and dilution of urine |
|
|
What happens to GFR and RBF if you dilate/ constrict the afferent arteriole?
efferent? |
Afferent Constriction
- decrease GFR - decrease RBF Afferent dilation - increase GFR - increase RBF Efferent Constriction - increase GFR - decrease RBF Efferent dilation - decrease GFR - increase RBF |
|
|
renal blood flow is equal to
|
the difference b/w renal arterial and venous pressure divided by the combined resistances of renal vessels
|
|
|
the juxtaglomerular apparatus is composed of
|
the macula densa of the thick ascending limb of the loop of henle
the extraglomerular mesanglial cells the renin-producing granular cells of the afferent & efferent arterioles |
|
|
sympathetic activity dose what
|
promotes the release norepi and dopamine
stimulates the release of renin enhances the reabsorption of sodium |
|
|
what is autoregulation
why is it impt where is it seen |
the phenomenon by which RBF and GFR maintain relatively constant
if it weren't for this, a 50% increase in pressure might cause a 50% increase in blood flow, but it really only shows a 6-8% increase in flow it is a feature of the cortex only |
|
|
afferent arteriolar vasodilator feedback mechanism
|
low GFR
decreased concentration of Na+ & Cl- in the DCT afferent arteriolar dilation increased RBF & GFR Increased flow rate in the tubules increased Na+ & Cl- concentration in the DCT |
|
|
efferent arteriolar vasoconstrictor feedback mechanism
|
low GFR
decreased concentration of Na+ & Cl- in the DCT J-G cells induced to secrete renin & formation of angiotensin II angiotensin II flows through the glomerulus and constricts efferent arteriole efferent constriction increases GFR & flow rate in tubular fluid |
|
|
extrarenal activities for the control of blood flow
|
sympathetic nerves supplying kidney decrease RBF by powerful constriction of renal arterioles (esp afferent)
angiotensin II causes vasoconstriction in intra and extrarenal arterioles which further decreases blood flow to kidney & reduces GFR atrial natiuretic peptide (promotes excretion of NaCl & H2O) - causes vasodilation of afferent & constriction of efferent arterioles - inhibits renin release - inhibits secretion of aldosterone by the adrenal cortex - inhibits reabsorption of NaCl from collecting duct - inhibits ADH secretion by the posterior pituitary |
|
|
the RAS
|
BP falls
prorenin -> renin angiotensinogen -> angiotensinogen I angiotensin-converting enzyme (ACE) cleaves 2 amino acids from angiotensinogen I to form angiotensinogen II angiotensin II - increases BP by general vasoconstriction - promotes the reabsorption of Na+ & H2O from the kidneys (this increases BP due to expansion of extracellular space) - acts on adrenal glands to promote the secretion of aldosterone which increases NaCl and H2O retention through the kidneys - NaCl retention is due to effects on the PCT to increase Na+ reabsorption |
|
|
the most basic and impt fxn of the RAS is to
|
maintain a relatively constant electrolyte composition and volume of extracellular fluid
|
|
|
an increase in arterial pressure would increase or decrease renin release
|
decrease (provides an inhibitory signal)
|
|
|
increased renal nerve activity has what effect on renin release
|
it increases renin release
|
|
|
the effects of prostaglandins are impt b/c
|
they prevent potentially harmful vasoconstriction and renal ischemia
they are stimulated by decreased ECV adn stress, angiotensin II, and sympathetic nerves |
|
|
nitric oxide
|
impt vasodilatory role in basal conditions
counteracts vasoconstriction produced by angiotensin II & catecholamines decreases total peripheral resistance as well as dilating afferent and efferent arterioles |
|
|
endothelin
|
powerful vasoconstrictor
constriction of afferen & efferent arterioles and decreases GFR & RBF |
|
|
adenosine
|
causes vasoconstriction of afferent & efferent arterioles thus reducing GFR & RBF
|
|
|
dopamine
|
vasodilator that increases RBF and inhibits renin secretion
|
|
|
ADH (vasopressin)
|
controls water conservation or secretion without affecting total amt of solute excreted
when ADH present in lg amts, kidneys produce a sm amt of urine When ADH levels are low, more urine is produced (diuresis) increase in osmolality -> ADH synthesis & release low BP also stimulates baroreceptors which signal ADH release |
|
|
diabetes insipidus
vs. nephrogenic diabetes |
diabetes insipidus
- interference with the hypothalamo-neurohypophyseal system - excretion of lg amts of urine nephrogenic diabetes - ADH is produced and released but receptors are unable to respond to the hormone |
|
|
the actions of ADH in the kidney
|
stimulate the reabsorption of NaCl from the thick ascending limb of the loop of henle
increase the permeability of the collecting duct to water and urea |
|
|
what is the 1st place in the nephron where water and solute move independently of each other
|
the thick ascending LH
|
|
|
diluting segment of the nephron
|
ascending limb of LH
NaCl pumped out but water can't follow so fluid is hypoosmotic to plasma |
|
|
why are the vasa rectae called exchangers
|
b/c both solute and water take a short cut (exchange) through the medullary interstitium
H2O leaves descending capillaries and enters ascending capillaries Solute leaves the ascending limb and enters the descending capillaries |
|
|
approximately 67% of the filtered Na+ is reabsorbed in the _______
|
PCT
|
|
|
Na+ is reabsorbed with what in the proximal PCT?
the distal PCT? |
proximal PCT
- glucose - amino acids - phosphate - lactate - HCO3- distal PCT - Cl- |
|
|
How does increasing CO2 tension affect HCO3- reabsorption?
increasing K+? increasing adrenal corticosteroids? |
CO2 -> increased reabsorption
K+ -> decreased reabsorption steroids -> increased reabsorption of HCO3- and Na+ -decreased K+ in ECF -> decreased K+ intracellular -> increased H+ intracellular |
|
|
severe hyperkalemia
vs. hypokalemia |
hyper
- high K+ - increased excitability of neurons - cardiac arrest & death hypo - low K+ - decreased excitability of neurons - paralysis, cardiac arrhythmias, metabolic alkalosis, death |
|
|
where is K+ reabsorbed?
secreted? |
reabsorbed
- PCT (67%) - loop of Henle secretion - DCT either -collecting duct |
|
|
how does acute acidosis affect K+ secretion
alkalosis? |
reduces it by inhibiting the Na/K pum and decreasing the permability of the apical membranes to K+
Alkalosis increases permeability of apical membranss to K+ & stimulates the Na/K pum. increases intracellular stores of K+ & passive diffusion of K+ |
|
|
does an increased flow rate encourage or inhibit K+ secretion
|
encourages
|
|
|
define acid
base |
a substance that liberates H+ when dissociated in fluid
a substance that readily binds or accepts H+ |
|
|
a change in 1 pH unit indicates a _____ fold change in H+ ion concentration
|
10 fold
|
|
|
what are the 3 impt buffers in the body
|
bicarbonate
phosphate protein |
|
|
what is the 1st line of defense against alteratinos of pH
|
chemical buffers
|
|
|
_____ constitute the greatest buffer system in the body
|
proteins
|
|
|
________ is the most important intracellular buffer
_______ is the most impt extracellular buffer |
hemoglobin
serum albumins & globins |
|
|
if body pH increases, the kidneys respond by
if body pH decreases |
excreting HCO3-
excreting H+ & conserving HCO3- |
|
|
1. what happens to bicarb reabsorption when PCO2 increases above normal?
2. when plasma K+ falls below normal 3. when plama chloride levels fall below nomral |
1. reabsorption increases
2. decreases 3. decreases |
|
|
what is total urinary accid excretion
|
the sum of titratable acid plus the amt of ammonion ion excreted
reflects the amt of base the kidneys have conserved by acidifying the urine |
|
|
in resp acidosis, the shift in pH is minimized initially by
|
chemical buffers
increased RR (if possible) renal excretion of H+ & retention of HCO3- |
|
|
resp alkalosis
|
during hyperventilation plasma H+ will increase and arterial PCO2 will decrease
the kidneys secrete fewer H+ ions and so reabsorb fewer HCO3- ions urine becomes alkaline rich in HCO3- |
|
|
normal anion gap
increased anion gap acidosis normal anion gap acidosis |
15-20
28 - cations normal, anions decreased - addition of acid 15 - decreased bicarb - hyperchloremia |
|
|
what happens to the anion gap if new acid is added to the body
|
it increases
|
|
|
hyperkalemia generally occurs with _______
(resp/ metabolic acidosis or resp/ metabolic alkalosis) |
metabolic acidosis
|
|
|
why do we use inulin for GFR?
|
freely filtered
neither secreted or reabsorbed doesn't react with anything doesn't change chemical composition |

