![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
|
How successful is splenic intervention ?
|
splenic biopsy is successful in 91% ,
splenic fluid aspiration in 100%, and splenic fluid drainage in 86% |
|
|
pre op
|
(a) a minimum platelet count of at least 50,000/μL; (b) an
acceptable international normalized ratio of less than 1.2; and (c) an acceptable activated partial thromboplastin time of 20–33 seconds. In adult patients, conscious sedation is produced by using midazolam (Versed; Roche Laboratories, Nutley, NJ) and fentanyl citrate (ElkinsSinn, Cherry Hill, NJ). After the procedure, all outpatients are monitored; blood pressure and pulse rate are measured every 15 minutes for the 1st hour, every 30 minutes for the next 2 hours, and then every 3 hours. Typically, patients are kept in the hospital for 3 hours after biopsy and 24 hours after catheter drainage to monitor for |
|
|
reason for doing procedure
|
The primary indication for splenic biopsy is an
indeterminate solid or cystic lesion for which a combination of clinical, radiologic, and blood culture findings has failed to allow diagnosis |
|
|
Hemostasis
|
At the end of the procedure, we
often inject hemostatic gelatin sponge to achieve hemostasis along the needle track |
|
|
technique
|
Pleural puncture can be
avoided during biopsy of splenic lesions located near the dome of the diaphragm by using realtime US guidance (Fig 5) or the gantry tilt CT technique, 22 degree |
|
|
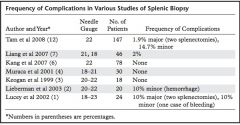
splenic procedural complication
|
|
|
|
pneumothorax complication
|
Although the transpulmonary approach can be used for biopsy of hepatic
or splenic lesions near the dome of the diaphragm, it is associated with an approximately 15% risk of pneumothorax. |
|
|
other complications
|
In cases of progressively expanding
hematomas not responding to fluid resuscitation and transfusion, the treatment options include transcatheter embolization and splenectomy. Other less common complications include pneumothorax, pleural effusion, and colonic injury |
|
|
advantage of drainage over surgery
|
Image-guided treatment is less invasive
than surgical treatment and has the advantage of avoiding long-term immunologic dysfunctions related to splenectomy |
|
|
drainage complication
|
Lucey et al (1)
and Taşar et al (14), one of seven and one of nine patients who underwent catheter drainage, respectively, experienced significant hemorrhage that led to splenectomy. This is why patients should be admitted to the hospital after the procedure and closely monitored for possible complications. |
|
|
alcohol treatment of cyst
|
alcohol ablation has been
most extensively used for treatment of liver and renal cysts, it has also been used for treatment of pancreatic cysts, splenic cysts, thyroid cysts, bronchogenic cysts, lymphoceles, lymphangiomas, and spermatoceles. |
|
|
splenic cyst treatment with ETOH
|
The procedure is typically performed with conscious sedation produced
by means of intravenous midazolam and fentanyl. With US guidance, an 8–10-F pigtail catheter is inserted by using the trocar technique and all fluid is aspirated (Fig 13). The fluid is sent for Gram staining, culture, and cytologic analysis. |
|
|
splenic drainage procedure
|
A small amount of diluted contrast material
can be injected through the catheter to ensure optimal placement of the catheter and rule out leakage of fluid into the peritoneal cavity. Approximately 50% of the aspirated fluid volume is replaced with 95% ethyl alcohol (maximum, 100 mL) and removed after 20 minutes |
|
|
post procedure follow up splenic cyst ETOH treatment
|
Complications of alcohol ablation include hypotension, pain, bleeding, infection, and chemical
damage to adjacent organs. Follow-up CT is performed 3 months later to evaluate for recurrence of the treated cyst and to plan any additional interventions, if needed. |
|
|
splenic pseudoanuerysm treatment with thrombin
|
Another technique for treatment of
pseudoaneurysms is percutaneous occlusion with image-guided thrombin injection. This approach has been most extensively used for management of femoral artery pseudoaneurysms (28). This method has also been used to treat pseudoaneurysms secondary to pancreatitis (29,30). Robinson et al (31) described use of endoscopic US-guided thrombin injection for treatment of a splenic artery pseudoaneurysm. |

