![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Terminology
|

|
|
|
Projection Patterns
|

|
|
|
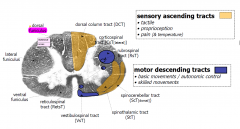
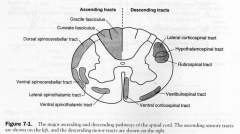
White Matter
|
1. only cells are glial
2. Zones with different tracts |
|
|
The IMPORTANT examinable TRACTS
|
|
|
|
Ascending Tract:
Pain and Temp |
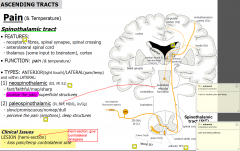
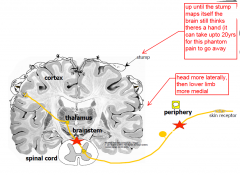
1. PAIN
2. temperature ANTERIOR(light touch)/LATERAL(pain/temp) and within LATERAL (1) neospinothalamic (III, VP, S1) - fast/faithful/map/sharp - localise the pain, superficial structures (2) paleospinothalamic (IV, BRF, MD/IL, In/Cg) - slow/promiscuous/nomap/dull - perceive the pain (emotions), deep structures |
|
|
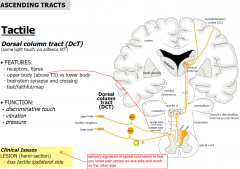
Ascending Tract:
Tactile |
|
|
|
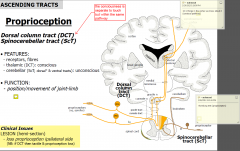
Ascending Tract:
Proprioception |
|
|
|
Descending Tracts:
BASIC |
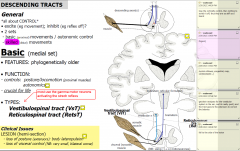
|
|
|
Descending Tracts:
Skilled |
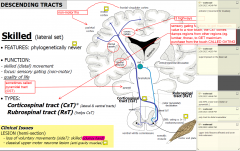
|
|
|
Types of lesions
|
- trauma, tumours, infections,
- ischaemia, demyelination |
|
|
Types of Sx after a sensory lesion?
|
(1) -ve symptoms: nothing
(2) +ve symptoms: abnormal - NERVES BEHAVING BADLY! (eg tingling, pins & needles, burning, phantoms) |
|
|
LMN Sx
|

- much clearer differences than sensory U and L
- Poliomyelitits or Werdnig-Hoffman disease results in damge to motor neurons |
|
|
UMN
|

|
|
|
Spinal Shock
|
- shut doen reflexes below the injury MAY or MAY not affect passing tracts
- return after 2-6wks with the reflexes returning gradually (urogenital then peripheral) MOA: GABAergic interneurone hyperactivity or cell damage? |
|
|
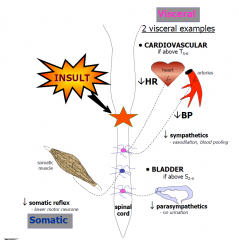
Autonomic Dysreflexia
|
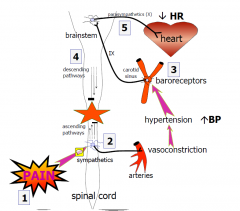
- may occur after spinal shock and can be fatal
• after spinal shock: ~1st year • spinal transection: cervical*, but above T5-6 (heart) • bizarre: causes no ANS unity because of transection • signs/symptoms: headache, sweat, goose-bumps, hypertension (episodic) because there is a complete sever the brain had no idea thus, the barorecptors take care of it, thus PSNS above the lesion |
|
|
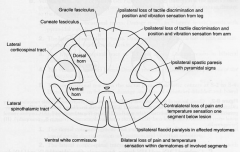
Brown-Séquard syndrome
|

is a loss of sensation and motor function (paralysis and ataxia) that is caused by the lateral hemisection (cutting) of the spinal cord. Other synonyms are crossed hemiplegia, hemiparaplegic syndrome, hemiplegia et hemiparaplegia spinalis, and spinal hemiparaplegia.
|
|
|
Major Tracts
|
|
|
|
Dorsal-Column - medial-lemniscus
|

1st ORDER: gracille, cuneate fasciculus, collaterals from spinal reflexes travel and terminate in the gracile and cuneate nuclei in caudal medulla
2nd ORDER: become axons and internal arcuate fibres that decussate & form the ML that terminates in the VPL (thalamus) 3rd ORDER: VPL projects through posterior limb of internal capsule to the postcentral gyrus |
|
|
lateral Spinothalamic Tract
|

- pain and temp
- receptors free nerve endings 1st ORDER: inputs from A-delta and C fibres to DRG, to the dorsolateral tract of Lissauer 2nd ORDER: dorsal horn, decussate in the ventral white commissure and ascend contralaterally to the VPS thalamus 3rd ORDER: VPL through posterior limb of IC to primary somatosensory cortex |
|
|
Lateral Corticospinal Tract
|

- skilled motor mainly upper limb
- not fully myelinated until end of 2nd year of life ORIGIN: layer V of cerebral cortex @ 1. premotor cortex 2. 1o cortex 3. Primary sensory cortex TERMINATION: contralaterally through interneurons on ventral horn motor neurons |
|
|
Course of Lateral Corticospinal tract
|
1. Telencephalon; in posterior limb of IC
2. Midbrain: middle 3/5th of crus cerebri 3. Pons: base 4. Medulla; pyramids. 85-90% decussate. the remaining 10-15% form the anterior corticospinal tract 5. Spinal cord: in dorsal quadrant of the lateral funiculus |
|
|
Hypothalamospinal tract
|
- from hypothalamus to ciliospinal center in the intermediolateral cell column at T1-T2
Clincal Features: horners syndrome ipsilateral |
|
|
Spinal Cord Lesions
|
|
|
|
Spinal Cord Pathologies
|

|
|
|
Combined UMN & LMN disease
|
- amyotrophic lateral sclerosis (ALS or Lou Gehrig's Disease)
- damage to the CsT and also LMNs. No sensory deficit |
|
|
Sensory Pathway Lesions
|
- Dorsal column disease; eg neurosyphilis, loss of tactile discrimination and position & vibration sensation. Irritation of dorsal roots leads to pain and paraesthesias. +ve Rhomberg, sign of dorsal colum ataxia
|
|
|
Combined Motor and Sensory Lesions
|
A. Spinal cord Hemisection (brown sequard)
B. Ventral spinal a. occlusion C. Subacute combined degeneration (B12 neuropathy) D. Syringomyelia E. Friedreich's ataxia F. MS |
|
|
Ventral Spinal Artery Occlusion
|
- infarct the anterior 2/3 of the cord (spares DC and dorsal horns)
- DAMAGES: 1. lateral CsT bilateral (pyramidal signs below the lesion) 2. lateral StT bilateral 3. hypothalamospinal tract above T2 bilateral horners 4. Ventral horns; bilateral flaccid paralysis of innervated muscles 5. CsT to sacral PSNS S2-4. |
|
|
Subacute Combined Degeneration
|
- B12 neuropathy (pernicious anaemia)
DAMAGE to: 1. DC bilateral 2. l CsT bilateral 3. ScT bilateral arm and leg dystaxia |
|
|
Syringomyelia
|
central cavitation of unknown origion
- DAMAGES; 1. Ventral white commissure 2. ventral horns |
|
|
Friedreich's ataxia
|
same as subacute combined degeneration
|
|
|
MS
|
plaques primarily involve white matter of the cervical segments
- random and asymmetric |
|
|
Peripheral Nervous System Lesion
- Guillain Barre Syndrome *acute idiopathic polyneuritis or post infectious polyneuritis) |
G-B Syndrome
1. demyelination and oedema 2. Upper cervical (C4) and resp paralysis are common 3. Caudal CN with facial diplegia in 50% of cases 4. Elevated protein causing papilledema 5. Less degree sensory affected causing paraesthesias 6. elevated proteins in CSF without pleocytosis |
|
|
IV disc herniations
|
L4-S1 90% of cases
C5-7 10% - herniation of nucleus pulposus through the defective anulus fibrosus into the vertebral canal - impinging spinal nerves |
|
|
Cauda Equina Syndrome
|
L3-Co
- usually due to nerve root tumour, ependymoma, dermoid tumour, lipoma of termial cord Sx A. severe radicular unilateral pain B. sensory distribution in unilateral saddle shaped area C. unilateral muscle atrophy and absent L3 and S1 jerks D. Incontinence and sexual functions are not marked E. Onset gradual unilateral |
|
|
Conus Medullaris Syndrome
|
S3-Co (usually intramedullary tumour
A. pain usually bilateral and not severe B. Sensory Dist in bilateral saddle C. Muscle changes not marked and normal reflexes D. Incontinence and sexual functions severly impaired E. Onset sudden and bilateral |
|
|
Nuclei in the spinal cord grey matter
|
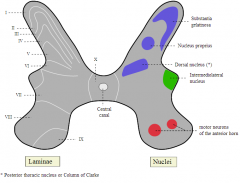
|
|
|
Internal capsule
-anterior - posterior limbs |
Anterior[edit]
The anterior two-thirds of the occipital part of the internal capsule contains fibers of the corticospinal tract, which arise in the motor area of the cerebral cortex and, passing downward through the middle three-fifths of the base of the cerebral peduncle, are continued into the pyramids of the medulla oblongata. Posterior[edit] The posterior third of the occipital part contains: (1) sensory fibers, largely derived from the thalamus, though some may be continued upward from the medial lemniscus; (2) the fibers of optic radiation, from the lower visual centers to the cortex of the occipital lobe; (3) acoustic fibers, from the lateral lemniscus to the temporal lobe; and (4) fibers which pass from the occipital and temporal lobes to the nuclei pontis. |
|
|
Subacute combined degeneration of spinal cord
|
Subacute combined degeneration of spinal cord, also known as Lichtheim's disease,[1][2] refers to degeneration of the posterior and lateral columns of the spinal cord as a result of vitamin B12 deficiency (most common) or vitamin E deficiency. It is usually associated with pernicious anemia.
|
|
|
Syringomyelia
|
Syringomyelia /sɪˌrɪŋɡɵmaɪˈiːliə/ is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in pain, paralysis, weakness,[1] and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. The disorder generally leads to a cape-like loss of pain and temperature sensation along the back and arms
|
|
|
Amyotrophic lateral sclerosis
|
Amyotrophic lateral sclerosis (ALS) – also referred to as motor neurone disease in some Commonwealth of Nations countries and as Lou Gehrig's disease in the United States – is a debilitating disease with varied etiology characterized by rapidly progressive weakness, muscle atrophy and fasciculations, muscle spasticity, difficulty speaking (dysarthria), difficulty swallowing (dysphagia), and difficulty breathing (dyspnea). ALS is the most common of the five motor neuron diseases.
|
|
|
Romberg's test
|
Romberg's test or the Romberg maneuver is a test used by doctors and physical therapists in a neurological examination, and also as a test for drunken driving. The exam is based on the premise that a person requires at least two of the three following senses to maintain balance while standing: proprioception (the ability to know one's body in space); vestibular function (the ability to know one's head position in space); and vision (which can be used to monitor [and adjust for] changes in body position).
|
|
|
All TRACTS
|

|
|
|
DDx Cauda equina and Conus Medullaris Syndromes
|
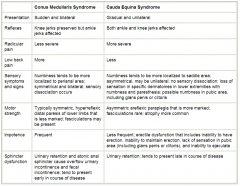
Patients can present with a pure canda equina or conus medalluris syndrome, or a mixture of both. Canda equina syndrome is really a peripheral nerve lesion.
Conus medullaris Syndrome may have some upper motor neurone(UMN) signs and present with increased tone and reflexes (UMN) and bilateral signs |

