![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
178 Cards in this Set
- Front
- Back
|
which lung would you be more likely to aspirate an object into
|
Right lung
--> because its a straighter path down |
|
|
what is the only part of the lung that is endodermically derived?
|
the airways !!
--> the rest , and the actual lung, are mesenchymal |
|
|
Mediastinum
|
is the anterior thorax – holds the lungs, thymus, heart (separates lungs from each other)
|
|
|
right lung has how many lobes
|
Right lung has 3 lobes: upper, middle, and lower lobes
Left lung usually has 2 lobes: upper and lower lobes |
|
|
left lung has how many lobes
|
Right lung has 3 lobes: upper, middle, and lower lobes
Left lung usually has 2 lobes: upper and lower lobes |
|
|
compare left an right bronchi
|
the right bronchus is a straight shot and the left bronchus is off to the side.
|
|
|
bronchus
|
Bronchus – conducting airway; lined with cartilage; seromucinous glands in its walls
Bronchioles – nothing more than little conducting airways; might also be gas exchange units |
|
|
bronchioles
|
Bronchus – conducting airway; lined with cartilage; seromucinous glands in its walls
Bronchioles – nothing more than little conducting airways; might also be gas exchange units |
|
|
lung have how many blood supplies ?
|
Lungs are really complicated in terms of blood supply: 2 blood supplies
1) Pulmonary circulation: - Pulmonary arteries – right side of heart pumps deoxygenated blood into lungs - Pulmonary veins – transfer oxygenated blood to left side of the heart 2) Bronchiole circulation: lung gets oxygenated - Bronchiole artery (branch of aorta) comes back to lung to feed O2 to lung tissue ---> Ex) if there’s a big blood clot in leg and it travels up through vena cava into right side of heart pumped into lungs and blocks pulmonary artery kills the lung (bcuz lung gets no blood supply) BUT for bronchiole artery, not everytime you get a thromboembolus or blood clot that travels to lung will it kill the lung |
|
|
pulmonary arteries
|
Lungs are really complicated in terms of blood supply: 2 blood supplies
1) Pulmonary circulation: - Pulmonary arteries – right side of heart pumps deoxygenated blood into lungs - Pulmonary veins – transfer oxygenated blood to left side of the heart 2) Bronchiole circulation: lung gets oxygenated - Bronchiole artery (branch of aorta) comes back to lung to feed O2 to lung tissue ---> Ex) if there’s a big blood clot in leg and it travels up through vena cava into right side of heart pumped into lungs and blocks pulmonary artery kills the lung (bcuz lung gets no blood supply) BUT for bronchiole artery, not everytime you get a thromboembolus or blood clot that travels to lung will it kill the lung |
|
|
pulmonary veins
|
Lungs are really complicated in terms of blood supply: 2 blood supplies
1) Pulmonary circulation: - Pulmonary arteries – right side of heart pumps deoxygenated blood into lungs - Pulmonary veins – transfer oxygenated blood to left side of the heart 2) Bronchiole circulation: lung gets oxygenated - Bronchiole artery (branch of aorta) comes back to lung to feed O2 to lung tissue ---> Ex) if there’s a big blood clot in leg and it travels up through vena cava into right side of heart pumped into lungs and blocks pulmonary artery kills the lung (bcuz lung gets no blood supply) BUT for bronchiole artery, not everytime you get a thromboembolus or blood clot that travels to lung will it kill the lung |
|
|
pulmonary circulation
|
Lungs are really complicated in terms of blood supply: 2 blood supplies
1) Pulmonary circulation: - Pulmonary arteries – right side of heart pumps deoxygenated blood into lungs - Pulmonary veins – transfer oxygenated blood to left side of the heart 2) Bronchiole circulation: lung gets oxygenated - Bronchiole artery (branch of aorta) comes back to lung to feed O2 to lung tissue ---> Ex) if there’s a big blood clot in leg and it travels up through vena cava into right side of heart pumped into lungs and blocks pulmonary artery kills the lung (bcuz lung gets no blood supply) BUT for bronchiole artery, not everytime you get a thromboembolus or blood clot that travels to lung will it kill the lung |
|
|
bronchiole circulation
|
Lungs are really complicated in terms of blood supply: 2 blood supplies
1) Pulmonary circulation: - Pulmonary arteries – right side of heart pumps deoxygenated blood into lungs - Pulmonary veins – transfer oxygenated blood to left side of the heart 2) Bronchiole circulation: lung gets oxygenated - Bronchiole artery (branch of aorta) comes back to lung to feed O2 to lung tissue ---> Ex) if there’s a big blood clot in leg and it travels up through vena cava into right side of heart pumped into lungs and blocks pulmonary artery kills the lung (bcuz lung gets no blood supply) BUT for bronchiole artery, not everytime you get a thromboembolus or blood clot that travels to lung will it kill the lung |
|
|
bronchiole artery
|
Lungs are really complicated in terms of blood supply: 2 blood supplies
1) Pulmonary circulation: - Pulmonary arteries – right side of heart pumps deoxygenated blood into lungs - Pulmonary veins – transfer oxygenated blood to left side of the heart 2) Bronchiole circulation: lung gets oxygenated - Bronchiole artery (branch of aorta) comes back to lung to feed O2 to lung tissue ---> Ex) if there’s a big blood clot in leg and it travels up through vena cava into right side of heart pumped into lungs and blocks pulmonary artery kills the lung (bcuz lung gets no blood supply) BUT for bronchiole artery, not everytime you get a thromboembolus or blood clot that travels to lung will it kill the lung |
|
|
describe Respiratory epithelium
|
pseudostratified with cilia and scattered goblet cells
|
|
|
Goblet cells
|
Respiratory epithelium – pseudostratified with cilia and scattered goblet cells
Goblet cells make mucin that is sticky so it catches the bacteria & environmental particles – allows them to be shuttled upward to epiglottis. --> Also produce immunoglobulins – helps keep the lungs sterile |
|
|
Cilia
|
beat in particular motion to carry environmental particles up to epiglottis where they can be swallowed and eaten away by stomach (filled with hydrochloric acid)
|
|
|
describe the transition of intrapulmonary airways
|
go from being bronchi --> to being bronchioles
bronchi get smaller and smaller and branch more and more... and when they lose their cartilage, become bronchioles |
|
|
Terminal bronchiole
|
Terminal bronchiole – last bronchiole that’s a pure conducting airway
Once you get into the respiratory bronchioles – they not only conduct but also have alveolar sacs coming off the walls (for gas exchange). |
|
|
why do larger arteries have collagen
|
Larger airways have cartilage in their walls so they don’t collapse
|
|
|
As you go down into the bronchioles, the epithelium changes as well ....
|
no longer have many goblet cells, and less cilia.
--> Assumption that the “garbage” have already been swept out of the lungs – it would be foolish to have goblet cells in a very small airway (it would just clog the airways). |
|
|
As you go down into the bronchioles, the epithelium changes as well – no longer have many goblet cells, and less cilia.... Why ?
|
Assumption that the “garbage” have already been swept out of the lungs – it would be foolish to have goblet cells in a very small airway (it would just clog the airways).
|
|
|
describe the Outside of the lung
|
Normally it should be white-ish pink.
|
|
|
Pulmonary lobule
|
Practical unit for clinical use
|
|
|
Alveolar wall is how thick
|
Alveolar wall is about 1 cell thick
|
|
|
There are two types of epithelial cells lining the space:
|
The wall is comprised of very thin elastic fibers and endothelial cells (capillaries) – the Type I cells sit in the alveolar spaces – lining the alveolar walls (a lot of cytoplasm stretched out)
|
|
|
can liver cells regenerate ?
|
YES
|
|
|
type 1 cells
|
There are two types of epithelial cells lining the space: Type 1 and Type 2
Type 1 cells – cells where gas exchange occurs across. RBC comes through the capillary – courses through – when it gets close to the type 1 cell, there’s enough of a gradient that O2 can from the RBC across the cytoplasm of the Type 1 cell. And the CO2 can be exchanged. Difficult to see Type 1 pneumocytes but much more common than type 2 – because they line much of the alveolus Exquisitely O2 dependent and sensitive Type 2 cells – they make surfactant and are also phagocytic (eat garbage if in the alveolar spaces). They can differentiate into Type 1 cells. |
|
|
type 2 cells
|
There are two types of epithelial cells lining the space: Type 1 and Type 2
Type 1 cells – cells where gas exchange occurs across. RBC comes through the capillary – courses through – when it gets close to the type 1 cell, there’s enough of a gradient that O2 can from the RBC across the cytoplasm of the Type 1 cell. And the CO2 can be exchanged. Difficult to see Type 1 pneumocytes but much more common than type 2 – because they line much of the alveolus Exquisitely O2 dependent and sensitive Type 2 cells – they make surfactant and are also phagocytic (eat garbage if in the alveolar spaces). They can differentiate into Type 1 cells. |
|
|
type 1 vs type 2 cells
|
There are two types of epithelial cells lining the space: Type 1 and Type 2
Type 1 cells – cells where gas exchange occurs across. RBC comes through the capillary – courses through – when it gets close to the type 1 cell, there’s enough of a gradient that O2 can from the RBC across the cytoplasm of the Type 1 cell. And the CO2 can be exchanged. Difficult to see Type 1 pneumocytes but much more common than type 2 – because they line much of the alveolus Exquisitely O2 dependent and sensitive Type 2 cells – they make surfactant and are also phagocytic (eat garbage if in the alveolar spaces). They can differentiate into Type 1 cells. |
|
|
which type of cell makes surfactant
|
There are two types of epithelial cells lining the space: Type 1 and Type 2
Type 1 cells – cells where gas exchange occurs across. RBC comes through the capillary – courses through – when it gets close to the type 1 cell, there’s enough of a gradient that O2 can from the RBC across the cytoplasm of the Type 1 cell. And the CO2 can be exchanged. Difficult to see Type 1 pneumocytes but much more common than type 2 – because they line much of the alveolus Exquisitely O2 dependent and sensitive Type 2 cells – they make surfactant and are also phagocytic (eat garbage if in the alveolar spaces). They can differentiate into Type 1 cells. |
|
|
why do you need surfactant?
|
type II produces surfactant
Reason you need surfactant – first alveolar is filled with fluid. A big breath at birth will expand the airway and it’ll open up the lungs (like a balloon) – the surfactant lowers the pressure (the tension in the wall). The second breath has far less pressure due to the surfactant. If you do not have surfactant, your lungs will collapse right back down – which makes it difficult for newborns to breathe (not mature enough diaphragms to expand lungs fully again – difficult). |
|
|
what lowers the pressure of newborns lungs during development?
|
surfactant... which is producted by Type II pneumocytes
|
|
|
which are more comon... type I or type II pneumocytes?
|
type I
there are technically more type II... but type I covers more surface area |
|
|
what is special about type I pneumocytes
|
- they create surfactant
- they can convert into type I |
|
|
lymphatics of the lung
|
Macrophages carry the debris into the lymphatics which are located along the pleural surfaces (along outside of the lobules). They carry them back to the chest where there are lymph nodes. And then from the lymph nodes, they go into the thoracic duct and dumped into the right side of the heart.
Lymph nodes are hugely important for a lot of process, but especially for cancer. Say there is a big lung cancer that spreads along the lymphatics to the lymph nodes (gets bigger). And it then spreads to the brain, liver, kidney, wherever else. So it’s important to recognize that lungs have lymphatics that drain to chest lymph nodes (mediastinal lymph nodes) goes wherever they want from there. |
|
|
the alveolar parenchyma derives from?
|
splanchnic mesenchyme
|
|
|
The cells that line the pleura are called
|
mesothelial cells
- The mesothelial cells are the primitive cells that give rise to alveolar sacs and ducts, pneumocytes, and fibroblasts. - They make a little bit of fluid (lubricant) so that when you take a breath, the lung expands and rubs against the chest wall (friction). |
|
|
Mesothelial cells in contact with asbestos fibers lead to _____________
|
malignant mesothelioma.
Cells lining the pleura –> go bad ---> can encase the lung. Invade chest wall causing tremendous pain --> restrict lungs (very hard to breathe) |
|
|
pleuritic chest pain
|
If you get bacterial pneumonia in underlying lung, the bacteria and neutrophils releasing all the enzymes are going to spread to the pleura as well – some of the mesothelial cells will be killed. So everytime you take a breath, you have pleuritic chest pain (everytime you breath, it hurts) – no longer lubricated due to lack of mesothelial cells (major friction).
|
|
|
pulmonary function tests
|
Total lung capacity (TLC)
How much air lungs will hold (men’s lungs a bit larger than that of women’s) Even though the capacity is 5-7 L, you don’t use 7L – you always have a reserve (you can never fully empty your lungs of air or else they would shrivel up like raisins) – what you’re really using is 3-5 L. Vital Capacity (VC) You use 3 L when you’re comfortably talking, 5 L when you’re running the marathon Tidal Volume (TV) Normal breath in; normal breath out With every breath it’s about 1-2 L Forced Vital Capacity (FVC) When you have no choice but to breathe out everything out you can: you can breathe out 3-4 L Forced Expiratory Volume in 1 sec (FEV1) Breathing out all you can in 1 sec: 2-3 L FEV1/FVC ratio which in a normal person should be 60-70%. You should be able to exhale 60-70% the amt of air you can exhale in one sec. So you exhale most of it in 1 sec. |
|
|
how would someone with severe lung disease behave ?
|
Someone with severe lung disease – can’t talk in long stretches, they have to talk in clipped sentences. See how fast they are breathing – how many times chest moves up in a minute. It doesn’t matter when you’re asleep or awake – false notion that you breathe more slowly when you sleep – it’s the same amt. Many of your bodily fxns don’t change when you sleep including your breathing.
|
|
|
TLC
|
Total lung capacity (TLC)
How much air lungs will hold (men’s lungs a bit larger than that of women’s) Even though the capacity is 5-7 L, you don’t use 7L – you always have a reserve (you can never fully empty your lungs of air or else they would shrivel up like raisins) – what you’re really using is 3-5 L. Vital Capacity (VC) You use 3 L when you’re comfortably talking, 5 L when you’re running the marathon Tidal Volume (TV) Normal breath in; normal breath out With every breath it’s about 1-2 L Forced Vital Capacity (FVC) When you have no choice but to breathe out everything out you can: you can breathe out 3-4 L Forced Expiratory Volume in 1 sec (FEV1) Breathing out all you can in 1 sec: 2-3 L FEV1/FVC ratio which in a normal person should be 60-70%. You should be able to exhale 60-70% the amt of air you can exhale in one sec. So you exhale most of it in 1 sec. |
|
|
VC
|
Total lung capacity (TLC)
How much air lungs will hold (men’s lungs a bit larger than that of women’s) Even though the capacity is 5-7 L, you don’t use 7L – you always have a reserve (you can never fully empty your lungs of air or else they would shrivel up like raisins) – what you’re really using is 3-5 L. Vital Capacity (VC) You use 3 L when you’re comfortably talking, 5 L when you’re running the marathon Tidal Volume (TV) Normal breath in; normal breath out With every breath it’s about 1-2 L Forced Vital Capacity (FVC) When you have no choice but to breathe out everything out you can: you can breathe out 3-4 L Forced Expiratory Volume in 1 sec (FEV1) Breathing out all you can in 1 sec: 2-3 L FEV1/FVC ratio which in a normal person should be 60-70%. You should be able to exhale 60-70% the amt of air you can exhale in one sec. So you exhale most of it in 1 sec. |
|
|
TV
|
Total lung capacity (TLC)
How much air lungs will hold (men’s lungs a bit larger than that of women’s) Even though the capacity is 5-7 L, you don’t use 7L – you always have a reserve (you can never fully empty your lungs of air or else they would shrivel up like raisins) – what you’re really using is 3-5 L. Vital Capacity (VC) You use 3 L when you’re comfortably talking, 5 L when you’re running the marathon Tidal Volume (TV) Normal breath in; normal breath out With every breath it’s about 1-2 L Forced Vital Capacity (FVC) When you have no choice but to breathe out everything out you can: you can breathe out 3-4 L Forced Expiratory Volume in 1 sec (FEV1) Breathing out all you can in 1 sec: 2-3 L FEV1/FVC ratio which in a normal person should be 60-70%. You should be able to exhale 60-70% the amt of air you can exhale in one sec. So you exhale most of it in 1 sec. |
|
|
FVC
|
`Total lung capacity (TLC)
How much air lungs will hold (men’s lungs a bit larger than that of women’s) Even though the capacity is 5-7 L, you don’t use 7L – you always have a reserve (you can never fully empty your lungs of air or else they would shrivel up like raisins) – what you’re really using is 3-5 L. Vital Capacity (VC) You use 3 L when you’re comfortably talking, 5 L when you’re running the marathon Tidal Volume (TV) Normal breath in; normal breath out With every breath it’s about 1-2 L Forced Vital Capacity (FVC) When you have no choice but to breathe out everything out you can: you can breathe out 3-4 L Forced Expiratory Volume in 1 sec (FEV1) Breathing out all you can in 1 sec: 2-3 L FEV1/FVC ratio which in a normal person should be 60-70%. You should be able to exhale 60-70% the amt of air you can exhale in one sec. So you exhale most of it in 1 sec. |
|
|
FEV1
|
Total lung capacity (TLC)
How much air lungs will hold (men’s lungs a bit larger than that of women’s) Even though the capacity is 5-7 L, you don’t use 7L – you always have a reserve (you can never fully empty your lungs of air or else they would shrivel up like raisins) – what you’re really using is 3-5 L. Vital Capacity (VC) You use 3 L when you’re comfortably talking, 5 L when you’re running the marathon Tidal Volume (TV) Normal breath in; normal breath out With every breath it’s about 1-2 L Forced Vital Capacity (FVC) When you have no choice but to breathe out everything out you can: you can breathe out 3-4 L Forced Expiratory Volume in 1 sec (FEV1) Breathing out all you can in 1 sec: 2-3 L FEV1/FVC ratio which in a normal person should be 60-70%. You should be able to exhale 60-70% the amt of air you can exhale in one sec. So you exhale most of it in 1 sec. |
|
|
Residual volume
|
– the air in the lungs you can’t touch (reserve)
|
|
|
volumes of breaths
|
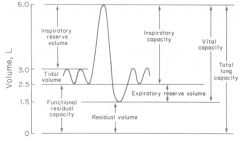
|
|
|
Non-neoplastic lung diseases
|
|
|
|
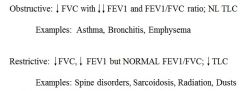
obstructive lung diseases
|
Restrictive lung disease is something that prevents you from taking a breath. It could be Scoliolis, malignant mesothelioma incasing the lung, fluid in pleural cavity – TLC is much less than it should be because lungs are being compressed. Ex) spine disorders, sarcoidosis, radiation, dusts
Obstructive lung disease is like when you have something obstructing your bronchi or airways get scarred – obstructing airflow. Like a big mucous ball obstructs air flow – you wouldn’t have a problem with TLC – you could expand your lungs but you won’t be able to get the air back out. Ex) Asthma, Bronchitis, Emphysema |
|
|
restrictive lung disorder
|
Restrictive lung disease is something that prevents you from taking a breath. It could be Scoliolis, malignant mesothelioma incasing the lung, fluid in pleural cavity – TLC is much less than it should be because lungs are being compressed. Ex) spine disorders, sarcoidosis, radiation, dusts
Obstructive lung disease is like when you have something obstructing your bronchi or airways get scarred – obstructing airflow. Like a big mucous ball obstructs air flow – you wouldn’t have a problem with TLC – you could expand your lungs but you won’t be able to get the air back out. Ex) Asthma, Bronchitis, Emphysema |
|
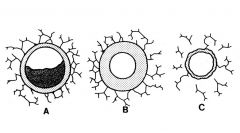
What is A?
|
A – Chronic bronchitis - something is in the air way
- Harder to get air in b/c the lumen is decreased. - Example of chronic bronchitis B – Asthma - thickening of the wall of the airway - Airways have muscle in their walls - The muscle increases in size with function – the wall in this case will decrease the diameter of the lumen If you decrease diameter of lumen, the same thing occurs as in A – less can go through C – Emphysema - Small airways do not have cartilage to hold them open - The pressures are not so great so they are not as likely to collapse - The small airway is held open in part by the alveolar walls - The alveolar walls help keep the lumen open |
|
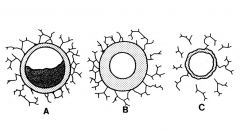
What is B?
|
A – Chronic bronchitis - something is in the air way
- Harder to get air in b/c the lumen is decreased. - Example of chronic bronchitis B – Asthma - thickening of the wall of the airway - Airways have muscle in their walls - The muscle increases in size with function – the wall in this case will decrease the diameter of the lumen If you decrease diameter of lumen, the same thing occurs as in A – less can go through C – Emphysema - Small airways do not have cartilage to hold them open - The pressures are not so great so they are not as likely to collapse - The small airway is held open in part by the alveolar walls - The alveolar walls help keep the lumen open |
|
What is C?
|
A – Chronic bronchitis - something is in the air way
- Harder to get air in b/c the lumen is decreased. - Example of chronic bronchitis B – Asthma - thickening of the wall of the airway - Airways have muscle in their walls - The muscle increases in size with function – the wall in this case will decrease the diameter of the lumen If you decrease diameter of lumen, the same thing occurs as in A – less can go through C – Emphysema - Small airways do not have cartilage to hold them open - The pressures are not so great so they are not as likely to collapse - The small airway is held open in part by the alveolar walls - The alveolar walls help keep the lumen open |
|
|
Obstructive lung diseases
|
- Expiratory airway obstruction and lung tissue destruction
- By 2030…COPD will be the 3rd leading cause of death worldwide - Smoking is the major risk factor, BUT only 10-15% of smokers develop symptoms Emphysema: abnormal permanent enlargement of airspaces without obvious fibrosis Chronic bronchitis: persistent cough with sputum for at least 3 months in at least 2 consecutive years Asthma: hyperreactive airways leading to episodic reversible bronchoconstriction |
|
|
emphysema
|
Emphysema: abnormal permanent enlargement of airspaces
without obvious fibrosis ---> alveolar walls dissolve Chronic bronchitis: persistent cough with sputum for at least 3 months in at least 2 consecutive years ---> a clinical diagnosis (not a morphologic dx) Asthma: hyperreactive airways leading to episodic reversible bronchoconstriction --> could be due to cold, chlorine, dander, bad air, etc. |
|
|
chronic bronchitis
|
Emphysema: abnormal permanent enlargement of airspaces
without obvious fibrosis ---> alveolar walls dissolve Chronic bronchitis: persistent cough with sputum for at least 3 months in at least 2 consecutive years ---> a clinical diagnosis (not a morphologic dx) Asthma: hyperreactive airways leading to episodic reversible bronchoconstriction --> could be due to cold, chlorine, dander, bad air, etc. |
|
|
asthma
|
Emphysema: abnormal permanent enlargement of airspaces
without obvious fibrosis ---> alveolar walls dissolve Chronic bronchitis: persistent cough with sputum for at least 3 months in at least 2 consecutive years ---> a clinical diagnosis (not a morphologic dx) Asthma: hyperreactive airways leading to episodic reversible bronchoconstriction --> could be due to cold, chlorine, dander, bad air, etc. |
|
|
would you see hypoxia during emphysema?
|
- You erase some of the spaces and blow out the alveolar sacs and get bigger.
---Less gas exchange - Since we have 2 lung and are efficient in exchange CO2 for O2 we do not see hypoxia. --- Our blood oxygen levels do not change b/c the drive to breath in brings in the oxygen --- In these patients, when the lung compresses, it doesn’t compress well b/c you have lost the alveolar walls with elastic tissue in them - People with empyhsema have blood oxygen levels that are normal but their blood carbon dioxide levels rise. Midbrain: --- Has breathing centers that are CO2 sensitive – not oxygen sensitive b/c CO2 is a poison. --- These patient’s CO2 levels rise and rise and they get accustomed to it but eventually you build up so much CO2 that it overwhelms their drive to breath --- If you give a lot of O2 to someone with emphysema, you will see them fall asleep and not wake up. |
|
|
Do blood oxygen levels change in emphysema?
|
- You erase some of the spaces and blow out the alveolar sacs and get bigger.
---Less gas exchange - Since we have 2 lung and are efficient in exchange CO2 for O2 we do not see hypoxia. --- Our blood oxygen levels do not change b/c the drive to breath in brings in the oxygen --- In these patients, when the lung compresses, it doesn’t compress well b/c you have lost the alveolar walls with elastic tissue in them - People with empyhsema have blood oxygen levels that are normal but their blood carbon dioxide levels rise. Midbrain: --- Has breathing centers that are CO2 sensitive – not oxygen sensitive b/c CO2 is a poison. --- These patient’s CO2 levels rise and rise and they get accustomed to it but eventually you build up so much CO2 that it overwhelms their drive to breath --- If you give a lot of O2 to someone with emphysema, you will see them fall asleep and not wake up. |
|
|
People with empyhsema have blood oxygen levels that are ______, and their blood carbon dioxide levels _____.
|
- You erase some of the spaces and blow out the alveolar sacs and get bigger.
---Less gas exchange - Since we have 2 lung and are efficient in exchange CO2 for O2 we do not see hypoxia. --- Our blood oxygen levels do not change b/c the drive to breath in brings in the oxygen --- In these patients, when the lung compresses, it doesn’t compress well b/c you have lost the alveolar walls with elastic tissue in them - People with empyhsema have blood oxygen levels that are normal but their blood carbon dioxide levels rise. Midbrain: --- Has breathing centers that are CO2 sensitive – not oxygen sensitive b/c CO2 is a poison. --- These patient’s CO2 levels rise and rise and they get accustomed to it but eventually you build up so much CO2 that it overwhelms their drive to breath --- If you give a lot of O2 to someone with emphysema, you will see them fall asleep and not wake up. |
|
|
Midbrain has breathing centers that are sensitive to what?
|
- You erase some of the spaces and blow out the alveolar sacs and get bigger.
---Less gas exchange - Since we have 2 lung and are efficient in exchange CO2 for O2 we do not see hypoxia. --- Our blood oxygen levels do not change b/c the drive to breath in brings in the oxygen --- In these patients, when the lung compresses, it doesn’t compress well b/c you have lost the alveolar walls with elastic tissue in them - People with empyhsema have blood oxygen levels that are normal but their blood carbon dioxide levels rise. Midbrain: --- Has breathing centers that are CO2 sensitive – not oxygen sensitive b/c CO2 is a poison. --- These patient’s CO2 levels rise and rise and they get accustomed to it but eventually you build up so much CO2 that it overwhelms their drive to breath --- If you give a lot of O2 to someone with emphysema, you will see them fall asleep and not wake up. |
|
|
alpha1-antitrypsin deficiency
|
- 1-2% of patients with COPD
- Autosomal recessive disorder (you need two bad copies of this) - alpha1AT is a serine protease inhibitor---elastase Made in the liver - Defective alpha1AT does not neutralize elastase---emphysema - Defective alpha1AT accumulates in the liver---cirrhosis Mutated SERPINA1 gene |
|
|
alpha-1-antitrypsin deficiency is an autosomal _____ disorder
|
- 1-2% of patients with COPD
- Autosomal recessive disorder (you need two bad copies of this) - alpha1AT is a serine protease inhibitor---elastase Made in the liver - Defective alpha1AT does not neutralize elastase---emphysema - Defective alpha1AT accumulates in the liver---cirrhosis Mutated SERPINA1 gene |
|
|
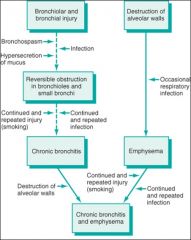
Chronic bronchitis can be from __________
|
Chronic bronchitis can be from tobacco or chronic infections.
- Anything that leads to obstruction in small airways (bronchioles and small bronchi) and continued - injury leads to a type of metaplasia (you get a lot of goblet cells) - The goblet cells are trying to cover the EP and protect everything from the tobacco smoke or the bacteria - You end up making more mucus than you should - Tobacco smoke kills of ciliated cells you get a lot of goblet cells get a lot of mucus end up dehydrated and blocking the airways chronic bronchitis |
|
|
pathway to chronic bronchitis and emphysema
|
|
|
|
describe in laymen terms chronic bronchitis, emphysema & asthma patients
|
Emphysema patients can get air in fine but can't get it out at all.
Chronic bronchitis patients get air in pretty well... but can't get it out at all Asthma patient has a hard time getting the air in and out. |
|
|
describe the bronchial histology with asthma
|
Eosinophils, goblet cells, inflammatory cells, thickened smooth muscle (muscular hypertrophy), and the seromucinous glands can also by hypertrophied
|
|
|
Two clinical stages of asthma:
|
- When someone comes into emergency room and you give them steroid and inhaler and they fell better you do not send them home get 8 to 10 hrs.
- You keep them b/c the goblet cells will make mucus and this appears 8-10 hrs later. |
|
|
Pathogenesis of asthma
|
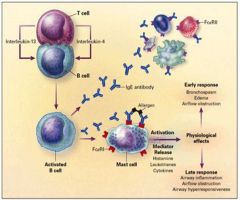
- B cells make IgE antibodies, which crosslink on mast cells and activate eosinophils.
- You get histamine release, leukotriene, cytokines - Anti-histamines are good for people with allergies. |
|
|
Early Physiological Responses of Asthma
|
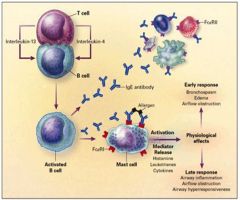
- B cells make IgE antibodies, which crosslink on mast cells and activate eosinophils.
- You get histamine release, leukotriene, cytokines - Anti-histamines are good for people with allergies. |
|
|
Late Physiological Responses of Asthma
|
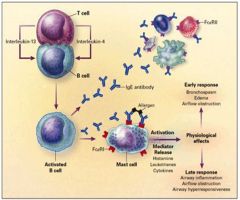
- B cells make IgE antibodies, which crosslink on mast cells and activate eosinophils.
- You get histamine release, leukotriene, cytokines - Anti-histamines are good for people with allergies. |
|
|
asthma: new focus on t-cells
|

CD4 T cells produce interleukin that stimulate other T cells that go on to stimulate other B cells.
Drug companies are trying to make drugs that specifically block IL-12 secretion from the CD4 T helper cell. |
|
|
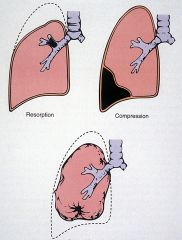
Atelectasis
|
- restrictive lung disorder
- Incomplete expansion or collapse of lung airless lung - REVERSIBLE !!!!! 3 types 1Resorption atelectasis: due to airway obstruction 2) Compression atelectasis: due to pleural cavity expansion; hemothorax, pneumothorax 3) Contraction atelectasis: due to lung or pleural fibrosis |
|
|
is atelectasis reversible?
|
- restrictive lung disorder
- Incomplete expansion or collapse of lung airless lung - REVERSIBLE !!!!! 3 types 1Resorption atelectasis: due to airway obstruction 2) Compression atelectasis: due to pleural cavity expansion; hemothorax, pneumothorax 3) Contraction atelectasis: due to lung or pleural fibrosis |
|
|
resorptive atelectasis
|
- restrictive lung disorder
- Incomplete expansion or collapse of lung airless lung - REVERSIBLE !!!!! 3 types 1Resorption atelectasis: due to airway obstruction 2) Compression atelectasis: due to pleural cavity expansion; hemothorax, pneumothorax 3) Contraction atelectasis: due to lung or pleural fibrosis |
|
|
compressive atelectasis
|
- restrictive lung disorder
- Incomplete expansion or collapse of lung airless lung - REVERSIBLE !!!!! 3 types 1Resorption atelectasis: due to airway obstruction 2) Compression atelectasis: due to pleural cavity expansion; hemothorax, pneumothorax 3) Contraction atelectasis: due to lung or pleural fibrosis |
|
|
contraction atelectasis
|
- restrictive lung disorder
- Incomplete expansion or collapse of lung airless lung - REVERSIBLE !!!!! 3 types 1Resorption atelectasis: due to airway obstruction 2) Compression atelectasis: due to pleural cavity expansion; hemothorax, pneumothorax 3) Contraction atelectasis: due to lung or pleural fibrosis |
|
|
Resorption Atelectasis – like a marble in the airway, or a mucus plug.
- Portion that is normally expanded does not expand b/c there is no air to expand. - Dotted lines are the atelectasis – the collapsed lung Compression Atelectasis – if you get blood in your pleural cavity or fluid pushes and compresses the lung - If there is a lot of fluid they will stick a needle in and drain the fluid. Contraction (restrictive) Atelectasis – caused by scarring of the lung - Dotted line shows how big the lung should be - The total lung capacity is lessened. - But the airways are totally normal – there is no obstruction This type of atelectasis isnt really reversible. |
|
|
resorptive atelectasis
|
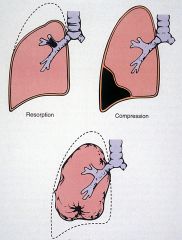
Resorption Atelectasis – like a marble in the airway, or a mucus plug.
- Portion that is normally expanded does not expand b/c there is no air to expand. - Dotted lines are the atelectasis – the collapsed lung Compression Atelectasis – if you get blood in your pleural cavity or fluid pushes and compresses the lung - If there is a lot of fluid they will stick a needle in and drain the fluid. Contraction (restrictive) Atelectasis – caused by scarring of the lung - Dotted line shows how big the lung should be - The total lung capacity is lessened. - But the airways are totally normal – there is no obstruction This type of atelectasis isnt really reversible. |
|
|
Compression Atelectasis
|
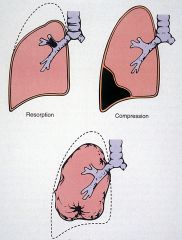
Resorption Atelectasis – like a marble in the airway, or a mucus plug.
- Portion that is normally expanded does not expand b/c there is no air to expand. - Dotted lines are the atelectasis – the collapsed lung Compression Atelectasis – if you get blood in your pleural cavity or fluid pushes and compresses the lung - If there is a lot of fluid they will stick a needle in and drain the fluid. Contraction (restrictive) Atelectasis – caused by scarring of the lung - Dotted line shows how big the lung should be - The total lung capacity is lessened. - But the airways are totally normal – there is no obstruction This type of atelectasis isnt really reversible. |
|
|
Contraction (restrictive) Atelectasis
|
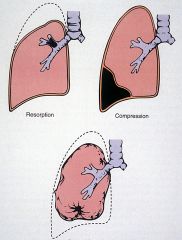
Resorption Atelectasis – like a marble in the airway, or a mucus plug.
- Portion that is normally expanded does not expand b/c there is no air to expand. - Dotted lines are the atelectasis – the collapsed lung Compression Atelectasis – if you get blood in your pleural cavity or fluid pushes and compresses the lung - If there is a lot of fluid they will stick a needle in and drain the fluid. Contraction (restrictive) Atelectasis – caused by scarring of the lung - Dotted line shows how big the lung should be - The total lung capacity is lessened. - But the airways are totally normal – there is no obstruction This type of atelectasis isnt really reversible. |
|
|
Restrictive lung diseases
|
- Spinal disorders
- Neurologic disorders - Sarcoidosis - Hypersensitivity pneumonitis - Pneumoconiosis - occuplational - Idiopathic |
|
|
Sarcoidosis
|
systemic idiopathic entity where you get granulomas and scarring of the lungs
Presents in the head and neck – salivary glands, oral cavity, conjunctiva, etc. restrictive lung disease |
|
|
Hypersensitivity pneumonitis
|
- Synonym: Extrinsic allergic alveolitis
- Immunologic reaction to inhaled antigens - Antigens not identified in up to 66% of cases - Acute and chronic presentations HP type I Anaphylactic type--asthma HP type II Cytotoxic type--antiGBM disease HP type III Immune Complex type--acute HP HP type IV Cell-mediated (delayed) hypersensitivity--sarcoidosis |
|
|
hypersensitivity reaction type I
|
HP type I Anaphylactic type--asthma
HP type II Cytotoxic type--antiGBM disease HP type III Immune Complex type--acute HP HP type IV Cell-mediated (delayed) hypersensitivity--sarcoidosis |
|
|
type II hypersensitivity reaction
|
HP type I Anaphylactic type--asthma
HP type II Cytotoxic type--antiGBM disease HP type III Immune Complex type--acute HP HP type IV Cell-mediated (delayed) hypersensitivity--sarcoidosis |
|
|
type III sensitivity reaction
|
HP type I Anaphylactic type--asthma
HP type II Cytotoxic type--antiGBM disease HP type III Immune Complex type--acute HP HP type IV Cell-mediated (delayed) hypersensitivity--sarcoidosis |
|
|
type IV sensitivity reaction
|
HP type I Anaphylactic type--asthma
HP type II Cytotoxic type--antiGBM disease HP type III Immune Complex type--acute HP HP type IV Cell-mediated (delayed) hypersensitivity--sarcoidosis |
|
|
Extrinsic allergic alveolitis
|
- Synonym: Hypersensitivity pneumonitis
- Immunologic reaction to inhaled antigens - Antigens not identified in up to 66% of cases - Acute and chronic presentations HP type I Anaphylactic type--asthma HP type II Cytotoxic type--antiGBM disease HP type III Immune Complex type--acute HP HP type IV Cell-mediated (delayed) hypersensitivity--sarcoidosis |
|
|
Etiologic agents in hypersensitivity pneumonitis
|
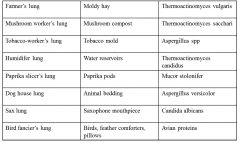
|
|
|
acute presentation of hypersensitivity pneumonitis
|
- Single large bolus exposure to antigen
- Insidious Dyspnea, cough, fever, chills 4-6 hours later - CXR: diffuse granular infiltrates - Pathology: Pulmonary edema - Pathogenesis: Type III hypersensitivity reaction (immune complex disease) - Prognosis: Improvement in a day or so - Reexposure: Recrudescence ***Diagnosis made on clinical grounds |
|
|
what pathology/ pathogenesis would you see in the acute presentation of hypersensitivity pneumonitis
|
- Single large bolus exposure to antigen
- Insidious Dyspnea, cough, fever, chills 4-6 hours later - CXR: diffuse granular infiltrates - Pathology: Pulmonary edema - Pathogenesis: Type III hypersensitivity reaction (immune complex disease) - Prognosis: Improvement in a day or so - Reexposure: Recrudescence ***Diagnosis made on clinical grounds |
|
|
what would you see on the chest x-ray for the acute presentation of hypersensitivity pneumonitis
|
- Single large bolus exposure to antigen
- Insidious Dyspnea, cough, fever, chills 4-6 hours later - CXR: diffuse granular infiltrates - Pathology: Pulmonary edema - Pathogenesis: Type III hypersensitivity reaction (immune complex disease) - Prognosis: Improvement in a day or so - Reexposure: Recrudescence ***Diagnosis made on clinical grounds |
|
|
chronic presentation of hypersensitivity pneumonitis
|
- Prolonged exposure to small amounts of antigen
- Insidious dyspnea, dry cough, fatigue - CXR: Mostly upper lobe interstitial reticulonodular infiltrates - Lab: serum antibodies, skin tests? - BAL: Increased CD8+ lymphocytes - Pathology: Chronic bronchiolitis, interstitial pneumonia, and granulomas - Pathogenesis: Type III and IV hypersensitivity reactions - Prognosis: Improvement in 33%, stable in 33%, worsening in 33% if antigen not removed ****Diagnosis made on clinicopathologic grounds |
|
|
what would you expect to find in a Bronchoalveolar lavage (BAL) in a patient with the chronic presentation of hypersensitivity pneumonitis?
|
- Prolonged exposure to small amounts of antigen
- Insidious dyspnea, dry cough, fatigue - CXR: Mostly upper lobe interstitial reticulonodular infiltrates - Lab: serum antibodies, skin tests? - BAL: Increased CD8+ lymphocytes - Pathology: Chronic bronchiolitis, interstitial pneumonia, and granulomas - Pathogenesis: Type III and IV hypersensitivity reactions - Prognosis: Improvement in 33%, stable in 33%, worsening in 33% if antigen not removed ****Diagnosis made on clinicopathologic grounds |
|
|
what would you find on a chest x-ray in the chronic presentation of hypersensitivity pneumonitis ?
|
- Prolonged exposure to small amounts of antigen
- Insidious dyspnea, dry cough, fatigue - CXR: Mostly upper lobe interstitial reticulonodular infiltrates - Lab: serum antibodies, skin tests? - BAL: Increased CD8+ lymphocytes - Pathology: Chronic bronchiolitis, interstitial pneumonia, and granulomas - Pathogenesis: Type III and IV hypersensitivity reactions - Prognosis: Improvement in 33%, stable in 33%, worsening in 33% if antigen not removed ****Diagnosis made on clinicopathologic grounds |
|
|
how is the diagnosis for chronic presentation of hypersensitivity pneumonitis made ?
|
- Prolonged exposure to small amounts of antigen
- Insidious dyspnea, dry cough, fatigue - CXR: Mostly upper lobe interstitial reticulonodular infiltrates - Lab: serum antibodies, skin tests? - BAL: Increased CD8+ lymphocytes - Pathology: Chronic bronchiolitis, interstitial pneumonia, and granulomas - Pathogenesis: Type III and IV hypersensitivity reactions - Prognosis: Improvement in 33%, stable in 33%, worsening in 33% if antigen not removed ****Diagnosis made on clinicopathologic grounds |
|
|
what is the pathology & pathogenesis for the chronic presentation of hypersensitivity pneumonitis ?
|
- Prolonged exposure to small amounts of antigen
- Insidious dyspnea, dry cough, fatigue - CXR: Mostly upper lobe interstitial reticulonodular infiltrates - Lab: serum antibodies, skin tests? - BAL: Increased CD8+ lymphocytes - Pathology: Chronic bronchiolitis, interstitial pneumonia, and granulomas - Pathogenesis: Type III and IV hypersensitivity reactions - Prognosis: Improvement in 33%, stable in 33%, worsening in 33% if antigen not removed ****Diagnosis made on clinicopathologic grounds |
|
|
what happens if one and a half lungs are scarred?
|
person will be able to function normally (NOT HYPOXIC) .. but if they try to exercise or exert themselves... they cannot do it
gas exchange is okay.. but TLC is much less --> as disease progresses, you are always able to exchange gas across the gradients... but you haev fewer units for gas exchange |
|
|
what happens in fibrous lung damage?
|
gas exchange is okay.. but TLC is much less
--> as disease progresses, you are always able to exchange gas across the gradients... but you haev fewer units for gas exchange |
|
|
Pneumoconiosis
|
- Most significant form of work-related illness in the world
- Over 17,000 respiratory ailments a year in US alone Pathologic response related to: - intensity of exposure - duration of exposure - quantity of exposure - size of particle - physiochemical properties of particle - route of clearance - efficiency of clearance - host response - interactions with other environmental pollutants |
|
|
Malignant mesothelioma:
- The lung is compressed here by the tumor that involves LNs. - The lung drains into chest LNs. - You also have a big space – pleural blood (hemothorax) pressing the lung further - This lung will not expand b/c of the tumor. |
|
|
With restrictive lung disease gas exchange is ________
|
normally good at the beginning but progressively decreases
|
|
|
_______ liters of air with ______ microorganisms inhaled each day
|
10,000 liters of air with 10,000 microorganisms inhaled each day!
|
|
|
pathogenesis of interstitial pneumonia
|
virus --> infection of Type i pneumocytes --> alveolar injury --> interstitial pneumonia
|
|
|
pathogenesis of intra-alveolar pneumonia
|
pyogenic bacteria --. acute inflammatory response to bacterium --> intra-alveolar pneumonia
|
|
|
symptoms of Bacterial pneumonias
|
Symptoms: Fever, malaise, productive cough and +/- chest pain
Signs: Tachypnea, decreased breath sounds, dullness to percussion Radiology: Infiltrate(s) Treatment: Afebrile within 48 to 72 hours after antibiotics < 10% of pneumonia admissions die!! |
|
|
signs of bacterial pneumonia
|
Symptoms: Fever, malaise, productive cough and +/- chest pain
Signs: Tachypnea, decreased breath sounds, dullness to percussion Radiology: Infiltrate(s) Treatment: Afebrile within 48 to 72 hours after antibiotics < 10% of pneumonia admissions die!! |
|
|
treatment of bacterial pneumonia
|
Symptoms: Fever, malaise, productive cough and +/- chest pain
Signs: Tachypnea, decreased breath sounds, dullness to percussion Radiology: Infiltrate(s) Treatment: Afebrile within 48 to 72 hours after antibiotics < 10% of pneumonia admissions die!! |
|
|
4 stages of bacterial pneumonia morphology
|
Congestion: bacteria with edema and vascular engorgement
Red hepatization: red cells, neutrophils and fibrin White hepatization: fibrin, fibroblasts with few neutrophils Resolution: return to normal |
|
|
complications of bacterial pneumonia
|
1) Abscess
2) Empyema - inflammatory response spreads into the pleural cavity - pus in the pleural space 3) Organization - consolidation; bacteria are killed, but the lung does not clean itself up - when TB consolidates the lung, it is not subtle. It is NOT interstitial. It fills the air spaces and the whole lung. 4) Bacteremic dissemination 5) Bronchiectasis - airway leading into the air spaces is - inflamed/distorted/fibrotic - permanent enlargement and distortion of air aways |
|
|
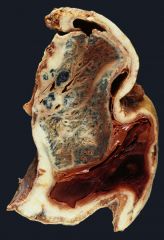
Pulmonary abscess
|
--> prone to alcoholics
Abscess formation: local necrosis of the lung Following pneumonia S. aureus, K. pneumoniae, pneumococcus type 3 fungi Aspiration of infective material Mixed organisms including oral anaerobic flora Bacteroides, Fusobacterium, Peptococcus Septic emboli deep leg veins or right heart valves Neoplasia--10 to 15% of cases post-obstructive pneumonias |
|
|
who are prone o get pulmonary abscesses ?
|
--> prone to alcoholics
Abscess formation: local necrosis of the lung Following pneumonia S. aureus, K. pneumoniae, pneumococcus type 3 fungi Aspiration of infective material Mixed organisms including oral anaerobic flora Bacteroides, Fusobacterium, Peptococcus Septic emboli deep leg veins or right heart valves Neoplasia--10 to 15% of cases post-obstructive pneumonias |
|
|
Bronchiectasis
|
Chronic necrotizing infection with dilation of airways
1) Bronchial obstruction Tumor, foreign body, mucus impaction (COPD) 2) Congenital or hereditary conditions Cystic fibrosis, Kartagener’s syndrome 3) Necrotizing pneumonia M. Tuberculosis and Staphlococcus infections |
|
|
what can cause bronchiectasis?
|
Chronic necrotizing infection with dilation of airways
1) Bronchial obstruction Tumor, foreign body, mucus impaction (COPD) 2) Congenital or hereditary conditions Cystic fibrosis, Kartagener’s syndrome 3) Necrotizing pneumonia M. Tuberculosis and Staphlococcus infections |
|
|
Atypical pneumonias
|
- as opposed to the bacterial pneumonias, atypical
- pneumonias include the viral pneumonias COUGH IS DIFFERENT – DRY COUGH ---> Bacterial pneumonia cough: a lot of mucus production |
|
|
Fungal respiratory infections
|
Candidiasis--normal oral flora
Candida albicans usually aspiration or hematogenous spread Histoplasmosis--Ohio and Mississippi rivers Histoplasma capsulatum Self-limited, chronic and disseminated forms Coccidiomycosis--Southwest and Far West Coccidioides immitis All inhalers become infected 10% have fever, cough and chest pain + skin lesions San Joaquin Valley fever complex |
|
|
PPD test
|
Induration is what matters
Rash does not mean anything intradermal injection 6-10 mm in diameter after 48-72 hours measure the induration depending on the health status, the size of the induration is positive 5 mm or greater HIV (+) or organ transplantation 10 mm or greater recent immigrant (within 5 years from high prevalence country) 15 mm False (+) is possible such as BCG vaccine |
|
|
Interstitial pneumonias without alveolar exudates
|
Mycoplasma pneumoniae
Legionella pneumophilia (Viruses) Chlamydia pneumoniae (psittacosis) Coxiella burnetti (Q fever) |
|
|
general features of pulmonary TB
|
Mycobacteria grow slowly and drug sensitivities can take 6 weeks
Mycobacteria are aerobic non-spore forming nonmotile bacilli with a waxy coat M. tuberculosis and M. bovis cause tuberculosis M. avium and M. intracellulare afflict immunocompromised folks M. leprae causes leprosy M. tuberculosis infects 33% of the world’s population M. tuberculosis kills 3 million patients yearly --Single most important infectious cause of death |
|
|
pathogenesis of pulmonary TB
|
Pathogenicity: ability to escape initial macrophage and T cell attacks
1) Cord factor: grow in cords 2) Lipoarabinomannan (LAM): g- endotoxin-like substance Inhibits macrophage activation by INF-gamma Induces macrophage TNF-alpha secretion fever, weight loss, tissue damage Induces macrophage IL-10 secretion suppresses T-cell proliferation 3) CR3 uptake receptor faciliates macrophage uptake without respiratory burst 4) Heat-shock protein All leading to granulomatous inflammation and destruction by self! |
|
|
grow in cords
|
Part of the Parthenogenesis of TB
1) Cord factor: grow in cords 2) Lipoarabinomannan (LAM): g- endotoxin-like substance Inhibits macrophage activation by INF-gamma Induces macrophage TNF-alpha secretion fever, weight loss, tissue damage Induces macrophage IL-10 secretion suppresses T-cell proliferation 3) CR3 uptake receptor faciliates macrophage uptake without respiratory burst 4) Heat-shock protein All leading to granulomatous inflammation and destruction by self! |
|
|
Lipoarabinomannan
|
Part of the Parthenogenesis of TB
1) Cord factor: grow in cords 2) Lipoarabinomannan (LAM): g- endotoxin-like substance Inhibits macrophage activation by INF-gamma Induces macrophage TNF-alpha secretion fever, weight loss, tissue damage Induces macrophage IL-10 secretion suppresses T-cell proliferation 3) CR3 uptake receptor faciliates macrophage uptake without respiratory burst 4) Heat-shock protein All leading to granulomatous inflammation and destruction by self! |
|
|
CR3 uptake receptor
|
Part of the Parthenogenesis of TB
1) Cord factor: grow in cords 2) Lipoarabinomannan (LAM): g- endotoxin-like substance Inhibits macrophage activation by INF-gamma Induces macrophage TNF-alpha secretion fever, weight loss, tissue damage Induces macrophage IL-10 secretion suppresses T-cell proliferation 3) CR3 uptake receptor faciliates macrophage uptake without respiratory burst 4) Heat-shock protein All leading to granulomatous inflammation and destruction by self! |
|
|
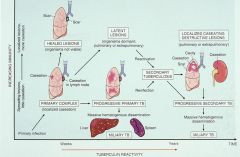
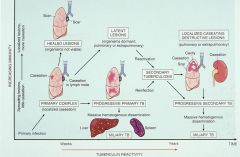
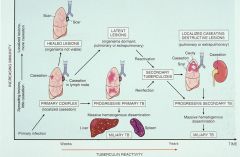
primary complex TB lesion
|
|
|
|
miliary TB
|
|
|
|
healed TB lesions
|
|
|
|
secondary TB
|
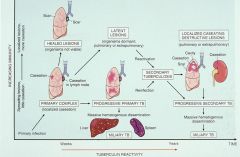
|
|
|
Ghon complex
|
Primary tuberculosis: Ghon complex
1) parenchymal subpleural lesion around upper/lower lobe fissure 2) enlarged caseous lymph nodes draining lung lesion **Ghon lesion --> primary lesion found in areas in the high oxygen content **GHON COMPLEX is more than just Ghon lesion --> macrophage carry the organism to the local lymph node. This is the Ghon complex (primary lesion + the associated lymph node); Caseous (cheese-like) Possible outcomes - Healed lesions: scars without organisms - Latent lesions: dormant organisms - Progressive primary Tb: massive lung spread - Miliary Tb: massive hematogenous spread |
|
|
possible outcomes of gohn complex
|
Primary tuberculosis: Ghon complex
1) parenchymal subpleural lesion around upper/lower lobe fissure 2) enlarged caseous lymph nodes draining lung lesion **Ghon lesion --> primary lesion found in areas in the high oxygen content **GHON COMPLEX is more than just Ghon lesion --> macrophage carry the organism to the local lymph node. This is the Ghon complex (primary lesion + the associated lymph node); Caseous (cheese-like) Possible outcomes - Healed lesions: scars without organisms - Latent lesions: dormant organisms - Progressive primary Tb: massive lung spread - Miliary Tb: massive hematogenous spread |
|
|
latent TB lesions
|
Latent lesions:
- dormant organisms disseminate - host weakens…cancer, infection - reactivation of infection --> Reactivation in 5 to 10% of cases --> Lung apices where there is high O2 tension Possible outcomes - scar with or without therapy - localized cavitation...bronchial..laryngeal…intestinal spread - bronchopneumonia “galloping consumption” - lymphangitic spread to other areas of lung or other organs - vascular spread |
|
|
possible outcomes of latent TB lesions
|
Latent lesions:
- dormant organisms disseminate - host weakens…cancer, infection - reactivation of infection --> Reactivation in 5 to 10% of cases --> Lung apices where there is high O2 tension Possible outcomes - scar with or without therapy - localized cavitation...bronchial..laryngeal…intestinal spread - bronchopneumonia “galloping consumption” - lymphangitic spread to other areas of lung or other organs - vascular spread |
|
|
Miliary TB
|
NECROTIZING GRANULOMATOUS INFLAMMATION
Nodules of necrosis surrounded by histiocytes and giant cells Ziehl-Neelsen (ZN) stain highlights organisms--red snappers Miliary TB: Pattern of hemotagenous spread |
|
|
change in US death rates since 1950
|
Drop in heart disease, pneumonia/influenza, strokes
Cancer death rate stayed the same (bcuz we didn’t come up with preload/afterload reduction, cholesterol lowering drugs) |
|
|
causes of lung cancer
|
Tobacco
Environment Infections Diet Genetic |
|
|
Tobacco smoke
|
Tobacco smoke causes 90% of lung cancer
1.9% of men, 13.0% of women non-smokers!! Duration and intensity of smoking correlate with incidence and mortality Low tar-low nicotine cigarettes--cotinine levels!! Involuntary or passive smoking is a proven cause of lung cancer |
|
|
Non-tobacco procarcinogens
|
Asbestos
Indestructible and fire resistant fibers Amosite, tremolite, chrysotile, crocidolite Incite inflammation, fibrosis, malignancies Synergistic-multiplicative effect with tobacco smoke Nickel compounds Copper compounds Arsenic compounds Chromate compounds Mustard gas Benzene |
|
|
Radioactivity in cigarette smoke
|
Alpha emitters polonium-210 and lead-210
Particles accumulate at bifurcations of segmental bronchi 1.5 packs per day = 300 CXR per year to the skin |
|
|
Radon
|
Radon...gaseous product of radium-226 decay
Half life 3.8 days; decays into 2 alpha emitting daughters Particles deposit on dust inhaled into the bronchial tree Beware of well insulated airtight homes in the Reading Prong Synergism between decay products and tobacco smoke 2nd cause of lung cancer in US according to EPA 20,000 deaths per year |
|
|
Lung cancer Clinical features
|
- Peak age 60-70 years, range 11-whenever
- Slight male predominance - Symptoms asymptomatic cough or change in existing cough weight loss chest pain dyspnea wheezing/stridor/hoarseness sputum production/hemoptysis SVC syndrome Pancoast syndrome Paraneoplastic syndromes metastatic disease |
|
|
Paraneoplastic syndrome
|
Paraneoplastic syndrome is when tumor makes factors that mimic other factors
Ex) Makes PTH or steroids |
|
|
SVC syndrome
|
SVC syndrome is when tumor grows and suppresses the superior vena cava (which collects blood from above the heart) – so neck veins bulge.
|
|
|
Horner’s syndrome
|
When tumor invades ansa cervicalis and brachial plexus, the following can present:
Miosis (smaller pupils), ptosis (drooping of upper eyelids), anhidrosis (dec sweating on affected side of face) |
|
|
Paraneoplastic syndromes
|
DEFINITION: Symptom complexes not explained by tumor
or hormones produced by organ involved by tumor. Occurs in 1-10% of lung cancer patients Hypercalcemia Hypocalcemia Gynecomastia Carcinoid syndrome Cushing syndrome Eaton-Lambert myasthenic syndrome Syndrome of Inappropriate ADH secretion (SIADH) |
|
|
Diagnostic procedures for lung cancer
|
Cytology
sputum bronchial wash/brush fine needle aspiration Transbronchial biopsy Mediastinoscopy or scalene lymph node biopsy Surgical resection wedge biopsy lobectomy pneumonectomy |
|
|
Two major types of lung cancer
|
small cell (SCLC) and non-small cell (NSCLC)
|
|
|
Small cell carcinoma
|
- Smoking-related
- Widespread at the time of diagnosis - Paraneoplastic syndromes I- nitially responsive to chemotherapy - There are almost NO survivors |
|
|
small cell carcinoma
|
Present with systemic complaints...H/A, fatigue...
Up to 85% have extrathoracic disease at diagnosis Present with paraneoplastic syndromes SIADH or Cushing syndrome 5 year survival 4% Gross features often virtually undetectable bronchial wall lesions Microscopic features small cells with little cytoplasm dark nuclei without nucleoli mitotically active |
|
|
what would you see under a microscope for small cell lung cancer?
|
Called “small cell” because they’re small blue cells w/very little cytoplasm but mitotically active.
|
|
|
Small cell lung cancer staging
|
Anatomic extent of limited disease can be included
within an irradiation field. Limited: Tumor confined to ipsilateral chest (30%) Extensive: Tumor beyond ipsilateral chest (70%) |
|
|
Small cell lung cancer treatment
|
NONSURGICAL THERAPY
Limited: Concurrent chemotherapy and radiation Extensive: Chemotherapy Limited 10% 5 year survival Extensive 0-2% 5 year survival |
|
|
Squamous cell carcinoma
|
Had been the most common type for years
Most common type found in men Correlates with smoking Usually central/hilar location ---> 15% 5 year survival Microscopic features squamous metaplasia dysplasia carcinoma keratinization intercellular bridges |
|
|
Adenocarcinoma
|
Most common subtype of lung cancer
Most common type in women and non-smokers Usually peripheral location 5-25% 5 year survival associated with scars Gross features can be very very small, but still very very bad! Microscopic features acinar papillary micropapillary solid lepidic |
|
|
which is the glandular forming lung cancer tumor?
|
adenocarcinoma
|
|
|
how do we stage small cell lung cancer?
|
Limited: ipsilateral field
Extensive: otherwise |
|
|
how do we stage non-small cell lung cancer?
|
we apply the TNM.
|
|
|
"T" category in lung cancer staging
|
T1: 3.0 cm or smaller tumor
not within the main bronchus T2: Larger than 3.0 cm but smaller than 7.0 cm tumor not within 2.0 cm of the carina Any tumor invading visceral pleura Any tumor causing atelectasis or pneumonia to hilum T3: Larger than 7.0 cm Any tumor extending into chest wall, diaphragm, pericardium Any tumor in the main bronchus within 2.0 cm of the carina Separate cancer in the same lobe! T4: Any tumor invading mediastinum, heart, esophagus... Any tumor involving the carina Separate cancer in same side lung but different lobe |
|
|
T1
|
T1: 3.0 cm or smaller tumor
not within the main bronchus T2: Larger than 3.0 cm but smaller than 7.0 cm tumor not within 2.0 cm of the carina Any tumor invading visceral pleura Any tumor causing atelectasis or pneumonia to hilum T3: Larger than 7.0 cm Any tumor extending into chest wall, diaphragm, pericardium Any tumor in the main bronchus within 2.0 cm of the carina Separate cancer in the same lobe! T4: Any tumor invading mediastinum, heart, esophagus... Any tumor involving the carina Separate cancer in same side lung but different lobe |
|
|
T2
|
T1: 3.0 cm or smaller tumor
not within the main bronchus T2: Larger than 3.0 cm but smaller than 7.0 cm tumor not within 2.0 cm of the carina Any tumor invading visceral pleura Any tumor causing atelectasis or pneumonia to hilum T3: Larger than 7.0 cm Any tumor extending into chest wall, diaphragm, pericardium Any tumor in the main bronchus within 2.0 cm of the carina Separate cancer in the same lobe! T4: Any tumor invading mediastinum, heart, esophagus... Any tumor involving the carina Separate cancer in same side lung but different lobe |
|
|
T3
|
T1: 3.0 cm or smaller tumor
not within the main bronchus T2: Larger than 3.0 cm but smaller than 7.0 cm tumor not within 2.0 cm of the carina Any tumor invading visceral pleura Any tumor causing atelectasis or pneumonia to hilum T3: Larger than 7.0 cm Any tumor extending into chest wall, diaphragm, pericardium Any tumor in the main bronchus within 2.0 cm of the carina Separate cancer in the same lobe! T4: Any tumor invading mediastinum, heart, esophagus... Any tumor involving the carina Separate cancer in same side lung but different lobe |
|
|
T4
|
T1: 3.0 cm or smaller tumor
not within the main bronchus T2: Larger than 3.0 cm but smaller than 7.0 cm tumor not within 2.0 cm of the carina Any tumor invading visceral pleura Any tumor causing atelectasis or pneumonia to hilum T3: Larger than 7.0 cm Any tumor extending into chest wall, diaphragm, pericardium Any tumor in the main bronchus within 2.0 cm of the carina Separate cancer in the same lobe! T4: Any tumor invading mediastinum, heart, esophagus... Any tumor involving the carina Separate cancer in same side lung but different lobe |
|
|
"N" category in lung cancer staging
|
N0: No nodes
N1: Peribronchial or ipsilateral hilar nodes N2: Ipsilateral mediastinal nodes or subcarinal nodes N3: Contralateral hilar or mediastinal nodes; any neck nodes |
|
|
N0
|
N0: No nodes
N1: Peribronchial or ipsilateral hilar nodes N2: Ipsilateral mediastinal nodes or subcarinal nodes N3: Contralateral hilar or mediastinal nodes; any neck nodes |
|
|
N1
|
N0: No nodes
N1: Peribronchial or ipsilateral hilar nodes N2: Ipsilateral mediastinal nodes or subcarinal nodes N3: Contralateral hilar or mediastinal nodes; any neck nodes |
|
|
N2
|
N0: No nodes
N1: Peribronchial or ipsilateral hilar nodes N2: Ipsilateral mediastinal nodes or subcarinal nodes N3: Contralateral hilar or mediastinal nodes; any neck nodes |
|
|
N3
|
N0: No nodes
N1: Peribronchial or ipsilateral hilar nodes N2: Ipsilateral mediastinal nodes or subcarinal nodes N3: Contralateral hilar or mediastinal nodes; any neck nodes |
|
|
"M" category in lung cancer staging
|
M0: No known metastases
M1: Separate carcinoma in other lung Pleural nodules Malignant pleural effusion Distant metastasis Regional lymph nodes (>50%) Adrenal gland (>50%) Liver (30-50%) Brain (20%) Bone (20%) |
|
|
M0
|
M0: No known metastases
M1: Separate carcinoma in other lung Pleural nodules Malignant pleural effusion Distant metastasis Regional lymph nodes (>50%) Adrenal gland (>50%) Liver (30-50%) Brain (20%) Bone (20%) |
|
|
M1
|
M0: No known metastases
M1: Separate carcinoma in other lung Pleural nodules Malignant pleural effusion Distant metastasis Regional lymph nodes (>50%) Adrenal gland (>50%) Liver (30-50%) Brain (20%) Bone (20%) |
|
|
Most common sites of metastisis for lung cancer
|
Regional lymph nodes (>50%)
Adrenal gland (>50%) Liver (30-50%) Brain (20%) Bone (20%) |
|
|
**WHat is the most common tumor on the lung?
|
its NOT a lung tumor... its a metastasis
bcuz the blood supply flows through R heart into the lungs on its way to L heart. So if you have a uterine sarcoma/carcinoma, ovarian tumor, liver tumor, renal kidney tumor, bone tumor, soft tissue tumor, it will make its way to the lung. |
|
|
What is the most common primary lung tumor?
|
**The most common primary lung tumor is a NSCLC.
|
|
|
Lung cancer Summary
|
- Most common cause of cancer death in the world
- 90% of lung cancers are smoking-related - # cases in US men and women dropping - Local, systemic symptoms and paraneoplastic syndromes - Hx, PE, CXR, CT scan, cytology and biopsies - There are many different types of malignant lung tumors - All types are bad; however, size and location matter - Non-small cell carcinoma is treated surgically - Small cell carcinoma is treated with chemo and radiation - Overall 5-year survival rate is 15%. - Other tumors love the lungs |
|
|
causes of bronchectasis
|
Obstructive
- tumors - inhaled foreign bodies - mucous plug (i.e. asthma) Non-Obstructive - usually childhood infections (viral or bacterial) |
|
|
pathogenesis of bronchiectasis
|
the inflammation caused by agents will destroy the elasticity of the wall --> the wall dilates
|
|
|
what is empyema
|
pus on the surface of the lung (called pyothorax)
--> body tries to wall it off |

