![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
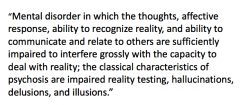
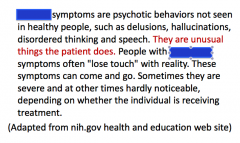
What is defined? |
Psychosis |
|
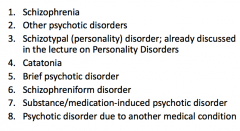
What are these? |
Schizophrenia spectrum disorders |
|
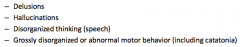
What are these the symptoms of? |
Schizophrenia spectrum disorders POSITIVE symptoms |
|
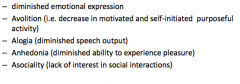
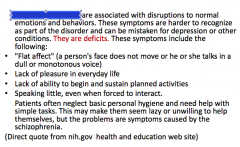
What are these the symptoms of? |
Schizophrenia spectrum disorders NEGATIVE symptoms |
|
What type of symptoms? |
Positive |
|
What type of symptoms? |
Negative symptoms |
|
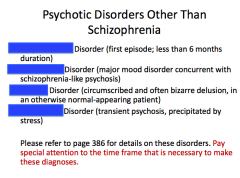
Identify the disorder |
|
|
|
|
|
|
|
|
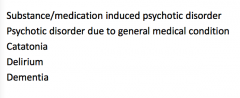
What are all of these? |
Psychotic disorders common in medical settings. |
|
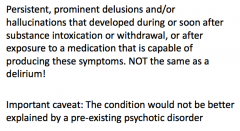
What disorder? |
Substance/medication-induced psychotic disorder |
|
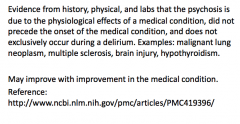
Diagnosis? |
Psychotic disorder due to another medical condition |
|
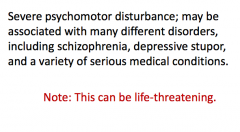
Diagnosis? |
Catatonia |
|
|
Altered mental status lasting hours to days. Potentially life threatening. |
Delirium |
|
|
Natural history Gene-environment interaction Table 48.1 Description of abnormal thought form in schizophrenia Table 48.2 (phases of schizophrenia) Know positive, negative, and cognitive symptoms |
ahsjkdhas |
|
|
For the diagnosis of Schizophrenia, how long must the patient have been sick? What about patients who recover much faster? |
6 months or more for schizophrenia Faster = schizophreniform disorder |
|
|
Loss of meaning due to random connections/loose associations between ideas. |
Derailment |
|
|
Responses to questions are only partially or remotely connected to the topic |
Tangential |
|
|
Excessively detailed or circuitous speech, yet still responsive to the question. |
Circumstantial |
|
|
Creation of words with unique meaning understood only by the individual. |
Neologism |
|
|
Losing track of the goal of speech and not being able to return to the topic |
Blocking |
|
|
Complete disregard for conventions of word usage or grammar, incoherence. |
Word salad |
|
|
The sound of words, instead to the meanings or conventions of speech, determine the flow of speech. |
Clanging |
|
|
Repetition of words or phrases |
Perseveration |
|
|
When does schizophrenia usually appear? |
Adolescence or young adulthood, rarely beyond the fourth decade. |
|
|
What are the three phases of schizophrenia? |
Prodomal, active, residual |
|
|
What two criteria must be met for a schizophrenia diagnosis? |
An active phase with prominent psychotic symptoms > 1 month, unless symptoms are interrupted by effective treatment.
Total duration of symptoms, regardless of phase, or >6 months. |
|
|
Gradual change in behavior that may appear as personality or mood change (aloofness, preoccupation, moodiness, oddities of thought or behavior) lasting weeks to months. |
Prodromal |
|
|
Classic findings of delusions, hallucinations, disorganized thinking and behavior. May include agitation, sleeplessness, and dangerous behaviors. |
Active |
|
|
Continuing oddities of thinning and behavior, often with prominent negative and cognitive symptoms. Delusions or hallucinations are typically absent. |
Residual |
|
|
Movement disorders (purposeless movements repeated over and over and catatonia in which both spontaneous and volitional movement is dysregulated along a continuum of retardation to the point of stupor, and extreme excitement.
Positive, negative, or cognitive symptoms? |
Positive |
|
|
Disturbances or affect or emotional tone, poverty of speech, inability to experience pleasure, lack of motivation, and social withdrawal.
Positive or negative symptoms? |
Negative |
|
|
Impaired focus and attention, deficits in working memory or the inability to use recently learned information.
Positive, negative, or cognitive symptoms? |
Cognitive |
|
|
Birth injury Intrauterine malnutrition Exposure to cytokines Infections in 2nd trimester
What are all of these? |
Environmental factors associated with Schizophrenia |
|
|
What portions of the brain are affected in schizophrenia? |
Decreased blood flow to frontal lobes Thinning of medial temporal lobe cortex Frontal cortex Small anterior portions of hippocampus Enlarged lateral and third cerebral ventricles |
|
|
Drugs that relieve symptoms of Schizophrenia all block what? |
Dopamine DA-2 receptors (possible increased activity of dopamine in subcortical mesolimbic brain regions produce positive symptoms)
Hypofunction of DA in prefrontal cortex => cognitive and negative symptoms |
|
|
Identify the clinical feature of delirium:
Symptoms develop over hours to days and represent a clear change from baseline functioning. The time between the onset of the cause of the delirium and the appearance of symptoms varies widely, depending on the specific cause and the presence of other risk factors. |
Acute onset |
|
|
Identify the clinical feature of delirium:
The quality and intensity of disturbances can vary within a 24-hour period and between consecutive days. Periods of transient improvement may be mistaken for resolution. Patients suspected to have delirium should be examined multiple times a day. |
Fluctuating course |
|
|
Identify the clinical feature of delirium:
Difficulty in focusing, sustaining, and shifting attention is typically present. Marked distractibility is a cardinal feature. The absence of attentional impairment makes the diagnosis of delirium unlikely. |
Impaired attention |
|
|
Identify the clinical feature of delirium:
Often described as a change in consciousness, a more accurate description is “abnormal level of arousal” that varies from somnolence to hypervigilance disproportionate to environmental stimulation. |
Altered level of consciousness |
|
|
Identify the clinical feature of delirium:
Impairment in the registration, consolidation, retention, and retrieval of information appear as poor performance on tasks that assess immediate, shortterm, and remote memory. Verbal and nonverbal memory is affected; severe cases may impair procedural memory. Autobiographical memory is usually preserved, but retrieval may vary, leading patients to provide misleading or inaccurate information. |
Memory deficits |
|
|
Identify the clinical feature of delirium:
Delirious patients are usually disoriented to time, place, and situation but rarely to self. Marked impairment in tracking the passage of time may be one of the earliest signs. Disorientation to time typically fluctuates within a day and may respond to environmental cues such as verbal reorientation, clocks, and calendars. |
Disorientation |
|
|
Identify the clinical feature of delirium:
Thoughts may be tangential or circumstantial and demonstrate an illogical flow of ideas. Severe cases include significant paucity of content and lack of spontaneous speech. Thought disorder may make patients’ communication incoherent or hard to follow. |
Disorganized thought |
|
|
Identify the clinical feature of delirium:
Initially, delirious patients may perceive sizes, shapes, and colors abnormally. They can develop illusions or gross misinterpretations of external stimuli in any sensory modality, most often vision and hearing. Misperception of internal stimuli is expressed as hallucinations. These are typically auditory or visual, although tactile and olfactory hallucinations may occur. The presence of vivid and bizarre visual hallucinations is more common in delirium and other secondary syndromes than in primary psychiatric disorders. |
Perceptual disturbances |
|
|
Identify the clinical feature of delirium:
Common and often lead to misdiagnosis of a primary psychotic disorder such as schizophrenia. Delusions in delirium are usually paranoid and bizarre but are not typically fixed or well developed. Delusions may be a form of confabulation, as the patient tries to make sense of internal and external stimuli in the face of distractibility, disorganization of thought, and perceptual disturbances. |
Delusions |
|
|
Identify the clinical feature of delirium:
Slow, slurred speech, paraphasias, dysgraphia, word-finding difficulty, and reduced comprehension may be present. Full-blown expressive or receptive aphasia may develop in severe or prolonged delirium. |
Language disturbances |
|
|
Identify the clinical feature of delirium:
Behavior may vary from absence of voluntary movement to restlessness with purposeless or inappropriate motor activity. Patients may injure themselves or others as a result of clumsiness, agitation, or purposeless aggression. |
Psychomotor disturbances |
|
|
Identify the clinical feature of delirium:
These include daytime drowsiness with frequent napping, followed by nighttime insomnia and fragmented sleep. Symptoms of delirium typically worsen at night (“sundowning”). Dreamlike experiences may occur when awake. |
Sleep disturbances |
|
|
Identify the clinical feature of delirium:
Affect may be constricted or flat. Labile expressions of anxiety, depression, euphoria, and irritability are common, reflecting underlying unstable mood. These emotional states may also be responses to the cognitive and perceptual disturbances that impair the patient’s appreciation of reality. |
Disturbances in affect |
|
|
Extremes of age Preexisting cognitive impairment Preexisting medical conditions Baseline poor health or disability Environmental conditions
What are these all risk factors for? |
Risk factors for delirium |
|
|
Identify the part of the brain associated with clinical features of delirium:
Inattention, thought disorganization, delusions, perceptual disturbances, disorientation/memory deficits, language impairments, psychomotor disturbances |
Frontal lobe/prefrontal cortex |
|
|
Identify the part of the brain associated with clinical features of delirium:
Inattention, thought disorganization, delusions, perceptual disturbances, disorientation/memory deficits, disturbances in affect, psychomotor disturbances, sleep disturbances |
Basal ganglia, thalamus, hippocampus |
|
|
Identify the part of the brain associated with clinical features of delirium:
Psychomotor disturbances, language impairments |
Cingulate gyrus |
|
|
Identify the part of the brain associated with clinical features of delirium:
Delusions, perceptual disturbances, memory deficits |
Temporal lobe |
|
|
Identify the part of the brain associated with clinical features of delirium:
Perceptual disturbances |
Occipital lobe |
|
|
Identify the part of the brain associated with clinical features of delirium:
Inattention, delusions, perceptual disturbances, disorientation |
Parietal lobe |
|
|
Identify the part of the brain associated with clinical features of delirium:
Inattention, altered level of consciousness, sleep disturbances |
Brainstem |
|
|
What is the only test with SPECIFIC findings in delirium and correlates well with the degree of cognitive impairment? |
EEG Hypoactivity (hyper polarization) appears as diffuse slowing of the dominant rhythms, generalized delta waves, and loss of reactivity of the EEG to eye opening and closing. |
|
|
What are typical psychiatric syndromes (psychosis, major depression, mania, anxiety, catatonia, personality changes) or specific patterns of cognitive behavior that occur in the course of various medical conditions? |
Secondary syndromes |
|
|
– Neurodegenerative conditions (Alzheimer disease, Parkinson disease, Pick disease, Huntington disease) – Multiple sclerosis – AIDS insufficiency/hypercortisolemia)
What are these all etiologies of? |
Secondary syndromes |
|
|
True or false: Secondary syndromes typically spare vital functions and lack signs of diffuse cortical impairment, making recognition less urgent. |
True |
|
|
How do you distinguish delirium from secondary symptoms? |
Secondary syndromes => usually no alteration in consciousness or significant fluctuations in symptoms. Usually due to chronic processes that cause permanent brain damage and PERSISTING symptoms. |
|
|
Review Table 44.1 (should know most of this already). |
Review Table 44.1 |
|
|
Identify the disease:
Characteristic scattered lesions throughout the brain Symptoms worsen during flares May be partially reversed or arrested by treatment |
Multiple sclerosis |
|
|
Effects of vasculitis Rapidly progressive in uncontrolled disease (seizures) |
Autoimmune disorders (SLE) |
|
|
Damage may be focal or diffuse Typically prominent frontal symptoms: personality change, movement disorders May remit with treatment of underlying infection |
Primary HIV infection or CNS or AIDS-related infections |
|
|
Diffuse toxic damage, sometimes prominent cerebellar damage Permanent but may not progress if drinking stopped |
Alcohol related |
|
|
Selective deterioration of mamillary bodies Early acute stage, "Wernicke's encephalopathy," reversible with treatment Later Korsakoff psychosis irreversible, severe loss of short-term memory
|
Thiamine deficiency (related to alcoholism or malnutrition) |
|
|
Diffuse axonal injury, cerebral contusions, and scarring Acceleration of DAT type changes Often frontal damage, personality change, and diminished executive functions Younger people may recover considerable function Depression, mania, or psychosis may occur, depending on site of injury |
Following closed head injury |
|
|
Sluggishness, loss of motivation, slowed thought May be reversible with thyroid replacement |
Hypothyroidism |
|
|
Often associated with anemia or peripheral neuropathy May be improved with vitamin replacement |
B12/Folate deficiency (intrinsic or secondary to alcoholism) |
|
|
Compression of cortical tissue surrounding cerebral ventricles Prominent gait disturbances and incontinence, personality changes May remit with early diagnosis, shunting |
Normal pressure hydrocephalus |
|
|
True or false: You should give antipsychotics to patients with catatonia. |
FALSE! This could turn the catatonia into malignant catatonia => death
TRY BENZODIAZEPINES FIRST! (Ativan = Lorazepam) |
|
|
How many symptoms does it take to be classified as catatonia? |
Just two
Waxy flexibility and mutism are common symptoms tested |
|
|
What to do if psych patient comes to ER? |
History Urine/drug screen Check vitals, look at pupils VERY FIRST VISIT OF SCHIZOPHRENIC-LIKE PATIENT = Diagnose as brief psychotic disorder first! |
|
|
Condition worsens "white crackerjack zombie mother father..." |
Check all vitals, do history, etc., again. FAMILY HISTORY Schizophrenia |
|
|
What are the merits of the atypical psychotics vs. older drugs?
What are drawbacks of atypical antipsychotics? |
Atypicals usually very expensive If schizophrenia, can use 1st or 2nd generation (doesn't matter). If cost is an issue, use first generation. |
|
|
What distinguished clozapine from typical antipsychotics? |
Monitor blood for agranulocytosis |
|
|
Hyperthermia High BP Tachycardia Slurring speech and unsteadiness of gait WBC elevation, elevated serum CK levels Schizophenic who just changed medicine from ziprasidone to perphernazine.
What is going on? |
Neuroleptic malignant syndrome
Discontinue drug, possibly give dantrolene, amantadine, bromocriptine |
|
|
20 year old Giggling to himself when nothing funny Raises hand in class and makes irrelevant comments that are clearly off the wall
What is going on? |
Seems to be schizophrenia Would also see delusions, hallucinations, always need to check about drug abuse, disorganized speech |
|
|
17 year old. Spends days in basement playing violent video games and neglecting hygiene. Makes no eye contact and when asked questions has very little to say. |
Schizophenia-like symptoms |

