![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
166 Cards in this Set
- Front
- Back
|
what are the five vital assessments?
|
temperature, pulse, respiration, pain, nutritional assessment
|
|
|
what are the three parts of The Circle of Nutrition?
|
1. assess the animal
2. assess the diet 3. assess the feeding management |
|
|
what are the two possible outcomes after the first nutritional assessment screening and what actions should be taken for each?
|
1. no risk factors present - no further action required
2. nutritional risk factors present - extended nutritional assessment |
|
|
what are the four basic categories to be examined during a nutritional screening evaluation?
|
1. carnivore vs. omnivore
2. life stage 3. environment 4. breed |
|
|
what are six life stages that can affect a nutritional screening?
|
1. adult in maintenance
2. gestation 3. lactation 4. growth 5. performance 6. geriatric |
|
|
what important nutrient is required to grow hair?
|
sulfur-containing amino acids
|
|
|
what are the six risk factors related to physiology/life stage/environment for a proper nutritional screening evaluation?
|
1. extremely low or high activity level
2. multiple pets in household 3. gestation 4. lactation 5. growth 6. age >7 years |
|
|
what are the six risk factors related to clinical history/diet history for a proper nutritional screening evaluation?
|
1. altered GI function (e.g. vomiting, diarrhea, nausea, flatulence, constipation)
2. previous or ongoing medical conditions/disease 3. medications and/or dietary supplements 4. unconventional diet (raw, homemade, vegetarian, unfamiliar) 5. snacks, treats, table food > 10% calories 6. inadequate or inappropriate housing |
|
|
what are the six risk factors related to body condition/muscle condition for a proper nutritional screening evaluation?
|
1. BCS <4 or >5 out of 9
2. muscle condition: mild, moderate, or marked muscle wasting 3. unexplained weight change 4. dental abnormalities or disease 5. poor skin or hair coat 6. new medical conditions / disease |
|
|
what is measured and reported for evaluating the animal for an extended nutritional evaluation?
|
1. serum chemistry profile
2. urinalysis 3. CBC 4. taurine, B12, iron, T4 - summarize, evaluate, interpret findings - estimate energy needs |
|
|
in estimating the energy needs of a patient, what is calculated for
- hospitalized patients? - outpatients (at home)? |
- hospitalized patients: RER
- outpatients (at home): DER |
|
|
what are the three growth periods of the neonate puppy and how are they influenced by nutrition?
|
1. nursing period - nutrition of the bitch
2. weaning period - stressful; change in food and environment 3. post-weaning period - (2 mos - adult) critical time for skeletal development; nutrition is the most important non-genetic factor for skeletal development |
|
|
what are the two main goals for the first 36 hours of life?
|
1. minimize stress
2. ensure adequate colostrum intake |
|
|
what determines the quantity and quality of colostrum?
|
the health and vaccination status of the dam
|
|
|
in biches and queens, what is the type of placenta and what percentage of their passive immunity is acquired transplacentally?
|
they have an endothelialchorial placenta that confers about 10% of passive immunity to the fetus
|
|
|
how long is the neonate's GI tract able to absorb whole antibodies as a part of passive immunity? Why? How much colostrum do puppies need in this time? Kittens?
|
- 24 hours
- because the pinocytotic endothelium is sloghed off after 24 hours - puppies need 3-10 mL of colostrum - kittens need 3-5 mL of colostrum |
|
|
in addition to nutrition and passive immunity, what other vital function does colostrum play in the day 0 neonate?
|
prevents circulatory failure
|
|
|
if a day 0 neonate cannot receive sufficient passive immunity from colostrum, what alternative route can be used? how is this calculated in the puppy and kitten?
|
- SQ serum
- puppy: 16 mL/day - kitten: 150 mL/kg/day in 3 doses |
|
|
what are five etiologies for fading puppy/kitten syndrome?
|
1. hypothermia
2. deficient colostrum intake 3. immunodeficiency 4. infection 5. cardiopulmonary failure |
|
|
condition when an otherwise healthy neonate starts to die?
|
fading puppy/kitten syndrome
|
|
|
in fading syndrome, what are the four aspects of the patent that need to be managed?
|
1. body temperature
2. hydration 3. blood sugar 4. nutrition |
|
|
in fading syndrome, how is hypothermia managed?
|
- slow warming over 1-3 hours
- use equipment such as an incubator with warm circulating air, water pads, and warm water bottles - warm the patient up to 97-98 ºF - ambient temperature after warming: 84-93 ºF; humidity 55-65% |
|
|
in fading syndrome, how is dehydration managed?
|
- warm fluids SQ: 1 mL/30g BW of 50:50 5% Glu:LRS; repeat as needed
- intraosseus fluids: maintenance 60-200 mL/kg/day |
|
|
in fading syndrome, how is hypoglycemia managed?
|
- correct AFTER body temperature is restored
- 1 mL/30g BW of warm 5-10% glucose solution by stomach tube |
|
|
in fading syndrome, how are the patients fed?
|
- don't feed hypothermic neonates
- nursing or hand-rearing |
|
|
why is feeding hypothermic neonates contraindicated?
|
because feeding will cause aspiration, diarrhea, dehyrdration, and further hypothermia due to non-functioning GI tract
|
|
|
why is monitoring the body temperature of neonates so important?
|
becuase puppies and kittens do not have the ability to thermoregulate during the first week of life (no shivering reflex)
|
|
|
what is the body temperature of a healthy neonatal puppy? kitten?
|
First 2 weeks:
- puppy: 94-99 ºF - kitten: 98 ºF Adult temperature by 4-5 weeks |
|
|
how many times per day should a neonate nurse during the first week?
|
4-6
|
|
|
in puppies and kittens, when do the eyes open? ears?
|
- eyes: 10-16 days
- ears: 15-17 days |
|
|
kittens under what birth weight have a low chance for survival?
|
90 g
|
|
|
How should weight gain be monitored in the neonate?
|
- gram scale for accuracy
- daily for the 1st 2 weeks - every 3-4 days until weaned |
|
|
what is the expected weight gain in neonatal puppies?
|
1-2 g/day/lb adult weight during the first 4-5 weeks
|
|
|
what is the expected weight gain for kittens?
|
- 50-100 g/wk until 5-6 wk
- 100 g/wk until 20 wk |
|
|
how long does the dam's milk support growth?
|
4 weeks
|
|
|
when and how often should supplemental food start to be given to neonates?
|
at 3-4 weeks, 3-4 times per day
|
|
|
in the neonate:
- when does gruel become the major nutrient source? - when are they nutritionally weaned? - when are they completely weaned? |
- gruel is major source by 5-6 wk
- nutritional weaning by 6 wk - complete weaning by 8 wk |
|
|
what are four options to feed orphaned neonates?
|
1. colostrum
2. SQ serum 3. foster dam 4. commercial milk replacer |
|
|
how do you bottle feed a puppy/kitten?
|
1. the nipple should have a horizontal slit that allows only 1 drop at a time
2. milk replacer warmed to 100 ºF 3. hold neonate horizontally 4. don't feed if hypothermic (rectal temp < 95 ºF) |
|
|
for feeding a neonate, with a stomach tube:
- what is the appropriate gauge tube? - how is tube length determined? - how much time should it take to administer the food? |
- 5-8 Fr. tube
- tube length is measured from nose to last rib - food is administered over a period of 1-2 minutes |
|
|
what needs to be done after bottle feeding/tube feeding a neonate?
|
stimulate the urogenital reflex because they cannot urinate or defecate on their own
|
|
|
when is the socialization period of the neonate?
|
5-12 weeks
|
|
|
when does the neonate experience the most rapid growth?
|
the first 6 months
|
|
|
when do puppies and kittens reach adult size?
|
- large breed dogs: 12 - 16 m
- small/medium breed dogs: 9 - 12 m - cats: 9 - 12 months (75% of adult BW at 6 m) |
|
|
why is slightly underfeeding the neonate indicated?
|
- slows growth and this prevents many diseases
- doesn't influence the adult size |
|
|
why is overfeeding a neonate contraindicated?
|
- increased fat deposition = juvenile obesity
- more rapid growth rate - increased risk of developmental orthopedic diseases (DOD), especially large/giant breed puppies |
|
|
how does a large breed puppy diet generally compare to a normal puppy diet?
|
- larger % protein
- lower Ca and P |
|
|
why is high calcium supplementation contraindicated in puppies?
|
- puppies < 6 mo are unable to protect themselves from excess Ca intake (uncontrolled intestinal diffusion)
- can cause hypercalcitoninism with impaired skeleton remodeling due to decreased osteoclast activity - uroliths - can cause a zinc deficiency |
|
|
what is a major cause for secondary zinc deficiency in puppies? what are 5 clinical signs of zinc deficiency?
|
- excess calcium intake is the main culprit
1. impaired growth 2. anorexia 3. conjunctivitis 4. poor hair coat 5. skin lesions |
|
|
what three major anatomical factors limits the juvenile's daily food intake?
|
1. low digestive capacity
2. smaller mouth 3. smaller, fewer teeth |
|
|
what juvenile disease commonly occurs due to deficient calcium intake?
|
nutritional secondary hyperparathyroidism
|
|
|
demineralization, fracture, and deformation of bone due to vitamin D deficiency
|
rickets
|
|
|
why must dogs and cats obtain vitamin D from the diet?
|
because they do not have the photosensitive enzyme in their skin to synthesize it in sufficient quantities
|
|
|
what are some good dietary sources of vitamin D?
|
- complete and balanced food
- liver - fish liver oil - fish - egg - milk |
|
|
how is DOD managed nutritionally?
|
- commercial diet with adequate energy, Ca, P, and vitamin D
|
|
|
how is nutritional secondary hyperparathyroidism managed nutritionally?
|
- dietary change is sufficient
|
|
|
how is rickets (hypovitaminosis D) treated nutritionally?
|
- feed a food with appropriate vitamin D
- may take several weeks |
|
|
what are four factors in transitioning a pup to a solid food?
|
1. introduce diet gradually
2. start 2-3 days before weaning 3. allow transition period of ~4 days 4. avoid feeding for max growth rate and early maturity |
|
|
when a weanling pup is overfed, what are two major negative health results that may occur?
|
1. hyperplastic obesity
2. DODs |
|
|
what can be said about feeding growing kittens free choice?
|
- they usually self-regulate and do not overeat
- spay/neuter changes this |
|
|
what is the average growth rate of male and female kittens?
|
- male: 20 g/day
- female: 11 g/day |
|
|
what diseases can be caused by feeding growing cats excess vitamin A?
|
- deforming cervical spondylosis
- bony exostoses along the muscular insertions of the cervical vertebrae and long bones of forelimbs - these conditions are very painful - +/- secondary hyperparathyroidsm if Ca:P ratio is reversed |
|
|
why is a high-liver diet bad for growing kittens?
|
- too much Vitamin A (bone deformities)
- Ca:P ratio is reversed, so it can lead to nutritional secondary hyperparathyroidism |
|
|
at what frequency should growing kittens be fed, depending on age?
|
- 3-4 meals/day until 4-6 months of age
- 2 meals/day after 6 months |
|
|
what is the target for optimal kitten feeding?
|
- average growth rate
- want lean BCS (4/9 or 5/9) |
|
|
why do cats require more protein and less CHO than omnivores?
|
- gluconeogenesis of protein is always on
- limited ability of liver to process CHOs because it has no fructokinase |
|
|
what are the two most important essential amino acids in the cat's diet?
|
taurine and arginine
|
|
|
why do cats require high levels of taurine and what is a common syndrome associated with taurine deficiency?
|
- cats can't biosynthesize tauine and it is lost in enterohepatic circulation
- common dz is dilated cardiomyopathy due to taurine deficiency |
|
|
what can happen if a cat meal is devoid of arginine?
|
- hyperammonemia
- death in 2-5 hours |
|
|
what are five important essential micronutrients required by the feline?
|
1. arachidonic acid
2. pre-formed vitamin A (cats can process beta-carotene) 3. niacin (B3) - cats can't make it from tryptophan 4. pyridoxine (B6) - high transaminase activity 5. thiamin (B1) |
|
|
what is the life expectancy for dogs, depending on breed size?
|
- small/medium: 13-18 yr
- large: 12-14 yr - giant: 7-10 yr |
|
|
depending on breed size, when should dogs and cats be converted to a senior diet?
|
- small cats, small/medium dogs - 7 years
- large/giant breed dogs - 5 years |
|
|
what are 7 nutritonal factors in aging dogs and cats?
|
1. inactivity and lowered BMR - obesity
2. decreased lean body mass and increased fat mass 3. decreased protein utilization 4. decreased ability to digest 5. increased requirements for vitamins A, E, and B 6. excess P can lead to renal disease 7. excess Na can lead to hypertension |
|
|
what are some factors for maintaining good nutritional status of a healthy senior pet?
|
- minimize stress with a daily routine
- portion controlled multiple meals per day - high quality ingredients - dental care - exercise - therapeutic diet when necessary |
|
|
what nutrients tend to be in higher concentration in a repro diet?
|
protein, fat, CHO, Ca, P
|
|
|
what are three reasons to give dietary CHO during pregnancy?
|
1. energy for fetus
2. prevents hypoglycemia 3. substrate for lactose synthesis |
|
|
what are three consequences of protein deficiency during pregnancy?
|
1. low birth weight
2. increased neonatal morbidity/mortality 3. decreased immunity |
|
|
what are three consequences of CHO deficiency during pregnancy?
|
1. low birth weight
2. increased neonatal morbidity/mortality 3. increased stillbirths |
|
|
what are two consequences of zinc deficiency during pregnancy?
|
1. fetal resorption
2. smaller litters |
|
|
what are two consequences of iron and/or vitamin B deficiency during pregnancy?
|
1. decreased immunity
2. decreased response to vaccination |
|
|
what are two consequences of vitamin A excess during pregnancy?
|
1. congenital abnormalities
2. smaller litters |
|
|
what is associated with vitamin D excess during pregnancy?
|
soft tissue calcification
|
|
|
what and how much should a pregnant bitch be fed during gestation?
|
- maintenance (1.8 - 2 x RER) during first 4 weeks
- growth/lactation (2.2-3.5 x RER) for last 5 weeks |
|
|
what and how much should a pregnant queen be fed during gestation?
|
- G/L diet at mating
- amount linear based on body weight |
|
|
in the periparturient pregnant dam
- when is mammary gland development and milk production at peak? - when does she stop eating? - when does she start eating postpartum? - what diet should she be fed? |
- mammary/milk: 1-5 days prior to parturition
- stop eating 1-2 days prior to whelping/queening - appetite returns within one day - feed a growth/lactation diet |
|
|
lactation:
- what is the target for feeding? - what determines the dam's energy needs? - typically, how much energy versus maintenance do they need? - when is peak milk production? |
- goal: maintain optimal BW and BCS
- energy needs determined by size of litter - require 4-5 x maintenance - milk production peaks at 3-4 weeks |
|
|
how is the DER of lactation calculated differently in the bitch and queen?
|
- bitch: # of puppies determines factor x pre-breeding RER
- queen: weeks of lactation determines an ADDITIONAL amount per kitten + pre-breeding RER |
|
|
what should be done on the day before weaning and the day of weaning?
|
DAY BEFORE
- separate dam from litter during day - withhold food from dam during day - reunite at night, but withhold all food DAY OF WEANING - completely wean - transition dam to maintance over 3-4 days - free choice water - monitor for mastitis |
|
|
what is the best frequency of feeding for gestating bitches and queens and why?
|
multiple small meals throughout the day because her stomach is compressed, but she needs to get enough food in there
|
|
|
in hypometabolic animals, how long does it take to deplete glycogen stores?
|
~28 hours
|
|
|
in the hypometabolic animal, when does somatic protein start to be catabolized?
|
1-2 days
|
|
|
in the hypometabolic animal, when does fat become the main fuel?
|
3 days
|
|
|
in the hypometabolic animal, how are lean muscle mass and fat used as starvation progresses?
|
after glycogen has been depleted after day 1, lean muscle will be burned for 1-2 days. On day 3, fat will take over as the main source, but as fat is depleted, lean tissue will be catabolized.
|
|
|
how does stress cause insulin resistance?
|
- stress stimulates catecholamine, glucocortocoid, glucagon, ADH, and aldosertone release
- this causes a hypermetabolic state - proinflammatory mediators (e.g. TNF, IL-6) are released - the hypermetabolic environment and inflammatory mediators mobilize glucose. this stimulus overcomes the effect of insulin |
|
|
how does change in body condition change with starvation versus starvation + stress?
|
starvation: preservation of lean muscle; body fat burned
stress + starvation: preservation of fat |
|
|
starvation versus starvation + physiological stress how do these precess differ in the change in
- activation of inflammatory mediators? - protein synthesis? - catabolism? - gluconeogenesis? - energy expenditure? - malnutrition level? - change in body fat/muscle? |
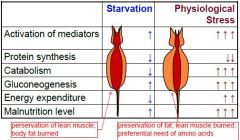
|
|
|
what things in the signalment/clinical history are red flags that the animal may need nutritional support?
|
1. recent weight loss exceeds 10%
2. surgery/trauma 3. food deprivation (or anorexia) > 3 days 4. increased nutrient losses/requirements 5. catabolic drugs |
|
|
for patients needing nutritional support, what is the first thing that should be corrected?
|
hydration and electrolyte abnormalitites
|
|
|
what nutrients should be part of a nutritional support program?
|
- energy: fat > CHO
- high quality protein - highly digestible (blenderizable) - B vitamins - omega 3 FA - Gln, Arg - antioxidants - nucleic acids |
|
|
what are the caloric and therapeutic goals of nutritional support?
|
- meet, not exceed the caloric requirements of the animal
- maintain BW - maintain gut integrity and function - feed to optimize recovery - overfeeding can lead to complications |
|
|
when beginning food dosage in the hospital, how much should you start feeding and how does this change?
|
- start feeding at RER of CURRENT body weight
- increase to DER = RER x appropriate factor by discharge |
|
|
how can impaired neurologic function affect the method by which nutritional support is provided?
|
- no gag reflex poses a risk of aspiration
- if the GIT is functional, use it whenever possible |
|
|
what are four general factors to encourage/enhance oral food intake?
|
1. reduce environmental stressors
2. food texture for palatability and/or ease of force feeding 3. food bowl position (higher for big dogs; wide and shallow for cats) 4. feeding frequency (small meals frequently) |
|
|
what are seven good ways to enhance food palatability to an animal in the hospital?
|
1. freshness - don't leave food in cage all day
2. aroma by warming 3. "cafeteria style" 4. alternate diets 5. feed food that was fed at home 6. homemade balanced diets 7. added flavorings |
|
|
what are the six different types of feeding tubes?
|
1. orogastric
2. nasoesophageal 3. esophagostomy 4. gastrostomy (PEG, G-tube) 5. enterostomy (J-tube) 6. gastrojejunal tube (G-J tube) |
|
|
orogastric tube:
- how long is it used? - how often is it replaced? - what species is best? |
- 1-2 days of nutritional support
- placed for each feeding - cats |
|
|
nasoesophageal tube
- how long is it used? - in what circumstances is it used? - species (tube size) |
- several days
- used in patients with high risk of anesthesia - dogs (~8 Fr); cats (5-6 Fr) |
|
|
esophagostomy tube (E-tube):
- how long is it used? - how is it placed? - species (tube size) |
- weeks to months
- surgical placement - cats (12-14 Fr); dogs (12-24 Fr) |
|
|
gastrostomy tube (PEG, G-tube)
- how long is it used? - why is it used? - how is it placed? - tube size |
- weeks to months
- it is used to bypass the pharynx and esophagus - placed surgically (G-tube), endoscopically (PEG tube), or blindly - 16-24 Fr |
|
|
enterostomy tube (J-tube)
- why is it placed? - how is it placed? - how is it used? - tube size |
- bypasses pancreas
- placed surgically in the jejunum - requires continuous feeding (via enteral pump) of liquid diet - 5-8 Fr |
|
|
G-J tube
- how is it placed? - how is it used? |
- surgically through the pylorous, duodenum, and into the jejunum
- it requires a liquid diet drip |
|
|
what determines the type of food you will use for tube feeding?
|
- tube size and location
- amount of functioning GIT - presence of metabolic dz - availability - cost |
|
|
for bolus tube feeding
- how much food (calories and frequency) do you feed when you start the tube feeding regimen? - how does amount and frequency change with time? |
- start at 1/3 to 1/2 of RER; feed every 2 hours
- increase to 100% RER by day 2 or 3; gradually increase to Q 6-8 hr/day |
|
|
when tube feeding, when is constant rate infusion indicated?
|
- volume intolerant
- intermittent vomiting - delayed gastric emptying |
|
|
how do you wean a patient off of tube feeding?
|
- offer fresh diet orally before each feeding
- wean when patient is consuming 75% RER orally - remove tube when 100% RER orally and BW gain/maintenance trend established |
|
|
what is
- total parenteral nutrition? - partial parenteral nutrition? - peripheral parenteral nutrition? - central parentral nutrition? |
- total: (human medicine) all nutrients fed parenterally
- partial: (vet med) because of cost, some things have to be left out - peripheral: in a vein (cephalic/saphenous) with a short catheter - central: external jugular or CVC (via the saphenous vein) with a long catheter |
|
|
what substances are typically in parenteral solutions?
|
- dextrose
- amino acids - lipid emulsion - B vitamins - other minerals/additives - fluids, if required |
|
|
what should be monitored during parenteral feeding?
|
- TPR
- BW and BCS - blood and urine glucose - PCV / TP/ albumin - serum lipids (gross evaluation) - others depending on dz (BUN, ammonia, electrolytes) |
|
|
what are requirements for a food to be "certified organic"?
|
95% or more of the ingredients must be organic and manufactured in a certified organic facility
|
|
|
what nutrients can be missing from a vegan diet?
|
- taurine, vitamin A, arachidonic acid (cats!)
- essential amino acids - B12 |
|
|
what is the major problem with meat-based diets?
|
inverse Ca:P --> NSHP
|
|
|
what are common problems associated with homemade diets?
|
- excess/deficiency of key nutrients
- unbalanced Ca:P - unpalatable - mineral/vitamin deficiencies (e.g. choline, iodine, zinc) |
|
|
what disorder can be caused by feeding
- garlic/onion? - cod liver oil? - tuna? - raw meat? - raw eggs? - liver? - raw fish? |
- garlic/onion: Heinz body anemia
- cod liver oil: hypervitaminosis D, A - tuna: mercury poisoning - raw meat: food poisoning - raw eggs: avidin in raw egg binds to biotin (B7) - liver: hypervitaminosis A - raw fish: thiaminase in fish destroys thiamin (B1) |
|
|
what is evaluated using the "5 ingredients rule" of homemade diets?
|
1. protein source (at least one of animal origin)
2. CHO source (cooked cereal grain; CHO:protein ratio) 3. fat source (animal fat and essential fatty acids) 4. Ca/P (bone meal, Ca carbonate, Dicalcium Phosphate) 5. Other minerals and vitamins (supplements are usually insufficient; use iodized salt) |
|
|
what is an "elemental" diet?
|
monomers
|
|
|
why are human baby foods not appropriate for animals?
|
- meat high in protein and fat
- not nutritionally balanced (e.g. low Ca) - harmful ingredients such as garlic/onion - high sodium |
|
|
what is AAFCO's definition of an additive and what are some examples?
|
an ingredient added to basic feed mix to fulfill a specific need
- flavorings - colorings - binders - emulsifiers - preservatives |
|
|
what is AAFCO's definition of a supplement?
|
a feed used with another to improve the nutritive balance or performance of the total
|
|
|
what are four common diseases commonly responsive to increased fiber intake?
|
1. obesity
2. diabetes mellitus 3. diarrhea 4. constipation |
|
|
how does solubility of fiber determine:
- fermentability - clinical signs when fed in excess |
- soluble is more fermentable than insoluble
- soluble fiber excess: watery stools, slowed GI transit time - insoluble fiber excess: large stool volume, stimulates GI motility (no effect on transit time) |
|
|
what are 3 general ways to manage constipation? What are two specific diets to manage constipation?
|
GENERAL
1. increase water intake 2. walk after feeding (gastrocolic reflex) 3. multiple small meals SPECIFIC 1. increased fiber approach 2. decreased fiber approach |
|
|
what is the most common type of diabetes mellitus in dogs? cats?
|
- dogs: Type I (50%)
- cats: Type II (80%) |
|
|
what are four risk factors for diabetes mellitus?
|
1. obesity (cats have 4X risk)
2. age (dogs 4-14 yr; cats > 6 mo) 3. gender (dogs: females 2X males; cats: neutered males) 4. breed (Keeshound, puli, Carin terrier, minpin, poodle) |
|
|
what are two easy to recognize clinical signs that may clue you into diabetes mellitus?
|
1. PU/PD
2. polyphagia with concurrent weight loss |
|
|
what are three common laboratory results indicative of diabetes mellitus?
|
1. hyperglycemia
2. hyperlipemia 3. glucosuria |
|
|
how does high dietary fat lead to diabetes mellitus in dogs?
|
high fat can cause pancreatitis, which can destroy endocrine pancreatic tissue
|
|
|
what should be ruled-out before putting a diabetic onto a high protein diet?
|
kidney disease
|
|
|
what are two important factors that the owner must comply with when treating canine diabetes mellitus?
|
1. be consistent - same diet, same amount of food, same time each day
2. insulin must be coordinated with intake |
|
|
what is the best diet for cats with diabetes mellitus?
|
high protein diet low in carbs
|
|
|
what are the two types of diet plans for cats with diabetes mellitus?
|
1. fiber-enhanced (F-E)
2. low starch (L-C) |
|
|
for a cat newly diagnosed with diabetes mellitus, which type of diet should be used?
|
- start with a low carb diet
- if obese, start with a fiber enhanced diet |
|
|
what are the six major risk factors for obesity?
|
1. neutering
2. age 3. diet 4. environment 5. activity level 6. owner factors |
|
|
what are 8 complications associated with rapid weight loss diets?
|
1. decreased activity/performance
2. rebound (yo-yo) effect 3. behavioral problems 4. skeletal disorders 5. loss of lean muscle mass 6. skin/hair disorders 7. immunocompromise 8. hepatic lipidosis (cats) |
|
|
what are characteristics of a good weight loss diet?
|
- low fat
- +/- high fiber - high protein - other nutrients (e.g. vitamins.minerals) meet daily requirements |
|
|
what is the safe range of weight loss for an animal on a weight loss diet?
|
0.5 - 2% BW/wk
|
|
|
how can fat maldigestion/malabsorption contribute to vomiting?
|
excess CCK release inhibits gastric emptying
|
|
|
how can fat maldigestion/malabsorption cause diarrhea/steatorrhea?
|
- impairs colonic water and electrolyte reabsorption
- accelerates colonic transport - loss of bile salts |
|
|
how does maldigestion/malabsorption contribute to bone loss?
|
- loss of fat-soluble vitamins
- loss of minerals (FFAs form indigestible soaps with Ca and Mg) - accelerated GI transport causes loss of minerals |
|
|
fat in the feces
|
steatorrhea
|
|
|
what are four causes of steatorrhea?
|
1. exocrine pancreatic insufficiency (PEI / EPI)
2. intestinal inflammation 3. motility disorders 4. short bowel disease |
|
|
after how long is vomiting considered chronic?
|
3 days
|
|
|
how is vomiting < 3 days treated?
|
- NPO 12-24 hours
- small quantites of water (ice cubes/ice chips) - reintroduce small meals Q 4-6x/day - diet highly digestible and moderate to low fat - gradually increase food amount over 3 days (tube feed if they don't eat) - transition to regular diet after 5-7 days |
|
|
how is vomiting >/= 3 days duration treated?
|
- correct fluid, electrolyte, acid/base imbalances
- blood chemistry - adequate nutritional support - enteral or parenteral - antiemetics - reintroduce water, then food when vomiting is controlled/resolved |
|
|
why is a slow NE drip good for vomiting patients
|
- small volumes may not induce vomiting and the GI tract is still utilized
|
|
|
what are clinical signs/history associated with pancreatitis?
|
- acute vomiting (mild-severe): dehydration, depression, fever
- abdominal pain, anorexia, diarrhea - cats (chronic in nature): PU/PD and weight loss - dietary indiscretion (e.g. dog eats entire ham) or high fat/low protein diet |
|
|
what dog breed is associated with hyperlipidemia and pancreatitis?
|
Miniature Schnauzer
|
|
|
what are six risk factors associated with pancreatitis?
|
- hyperlipidemia (obesity, idiopathic as in Miniature Schnauzers)
- high fat / low protein diet (dogs) - hypercalcemia - drugs - ischemia-reperfusion of the pancreas - manipulation or trauma |
|
|
what is the pathogenesis of pancreatitis?
|
pancreatic lysozomes fuse with zymogen granules. The zymogens become activated by the lysozyme.
|
|
|
what is the basic process of treating pancreatitis with vomiting?
|
- give pancreas a rest
- stop the vomiting - make sure animal has adequate fluids and nutrition (may need parenteral or J-tube) - when vomiting resolves, reintroduce GI-based nutritional management for at least 1 week - transition back onto regular diet |
|
|
what are the key nutritional factors for a pancreatitis diet (enteral)
|
- highly digestible
- water - restricted protein - low to moderate fat |
|
|
what enzyme in the adipose tissue mobilizes fat and how do insulin and glucagon regulate this enzyme
|
hormone sensitive lipase
- insulin inhibits - glucagon stimulates |
|
|
which enzyme in the blood is involved with processing VLDLs exported from the liver and how do insulin and glucagon regulate this enzyme
|
lipoprotein lipase
- insulin stimulates - glucagon inhibits |
|
|
how are hormone sensitive lipase and lipoprotein lipase involved in hepatic lipidosis?
|
- starvation: high glucagon, low insulin
- hormone sensitive lipase will be activated and remove fat from adipocytes --> lipdemia --> body cells and liver - lipoprotein lipase is down-regulated, so the VLDL produced by the liver cannot return the fat to body cells |
|
|
what are clinical signs of hepatic lipidosis in the cat?
|
- +/- obesity
- anorexia, janudice, weight loss, +/- hepatic encephalopathy, hepatomegaly - hyperbilirubinemia, elevated ALP (associated with cholestasis) - hypoalbuminemia, anemia, muscle wasting - fatty liver on histopath |
|
|
how is hepatic lipidosis treated nutritionally in the cat?
|
- prevent catabolism and further peripheral lipolysis
- avoid excess energy consumption, which will lead to more trigs - feeding tube for 2-6 weeks |
|
|
in treating cats with hepatic lipidosis, what are aspects of the food that is administered?
|
- adequate (not excess energy); feed at RER for ideal body weight
- high fat - high protein - high energy density - potassium - L-carnitine - vitamins K1, E, B - S-adenosylmethionine - don't use LRS because there may be lactate intolerant |

