![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Review of normal action potential:
|
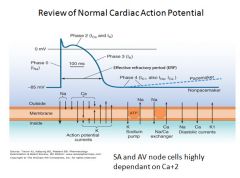
- In phase 0, rapid influx of Na+ causes rapid depolarization.
- In phase 1-2, sodium channels close but the action potential is maintained by slow influx of Ca+2 ions - In phase 3, the Ca+2 channels start to close and K+ channels open, leading to efflux of K+ and a decline of action potential - In phase 4 repolarization is complete and the Na/K and N/Ca pumps are active |
|
|
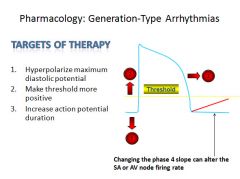
Targets of therapy for generation type arrythmyias:
|
|
|
|
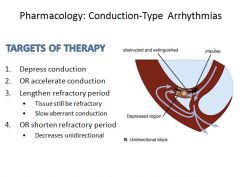
Targets of treatment for conduction type arrhythmias:
|
|
|
|
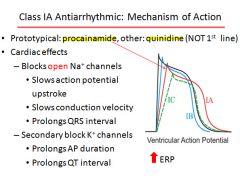
Class I antiarrhythmic agents (sodium channel blocking drugs):
|
IA-procainamide (binds to open state)
IB-lidocaine (binds to closed state) IC-flecainide (binds to open state) |
|
|
Class I antiarrythmic effects on action potential and refractory periods:
|
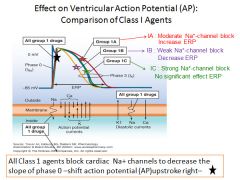
Note: ERP=Effective refractory period
IA would decrease firing rate due to increased refractory period IB would increase firing rate due to decreased refractory period |
|
|
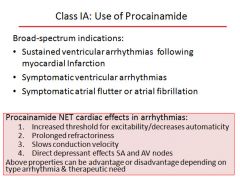
Class IA antiarrythmic Procainamide:
|
|
|
|
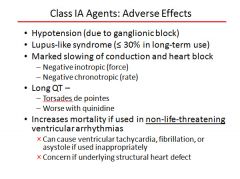
All of the following are properties of procainamide except?
Risk of torsades de points Slows ventricular repolarization Widened QRS wave Decrease Ca+2 influx Prolongs action potential |
Decrease Ca+2 influx
|
|
|
Adverse effects of Procainamide (class IA):
|
|
|
|
Indications for use of Procainamide (class IA):
|
|
|
|
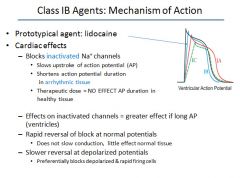
Class IB antiarrythmic Lidocaine:
|
|
|
|
In additional to cardial channels, lidocaine also blocks which of the following with high affinity?
Neuronal Na+ channels Vascular Ca+2 channels B1 SA nodal receptors K+ channels |
Neuronal Na+ channels
|
|
|
Indications for use of Lidocaine (class IB):
|
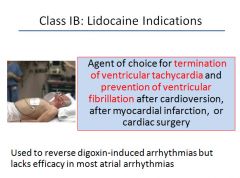
|
|
|
Adverse effects of Lidocaine (class IB):
|
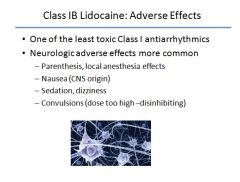
|
|
|
Lidocaine has preferential affinity for which?
Ventricular cells Atrial cells Ca+2 influx SA node Normal cardiac tissue AV node |
Ventricular cells
|
|
|
Class IC antiarrythmic Flecainide:
|
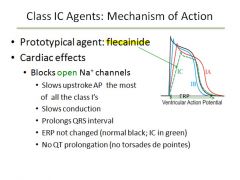
Shortens action potential duration in Purkinje cells
|
|
|
Indications for use of Flecainide (class IC):
|
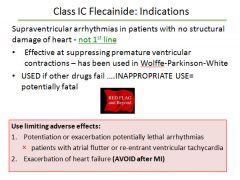
|
|
|
Class II antiarrythmic drugs (Beta blockers):
|
Propranolol
Esmolol Sotalol (also a class III) |
|
|
Class II antiarrythmics Propranolol and Esmolol:
|
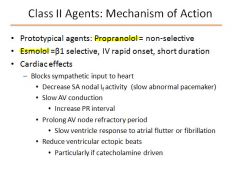
|
|
|
Which of the following regulates sympathetic control of SA and AV nodal conduction?
B2 adrenergic B1 adrenergic cAMP levels B3 adrenergic A1 adrenergic |
Both B1 adrenergic and cAMP levels
|
|
|
Indications for the use of Propranolol and Esmolol (class II antiarrythmics):
|
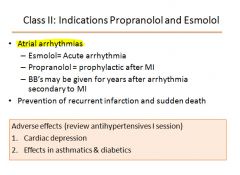
|
|
|
MOA of Class III antiarrythmic drugs:
|
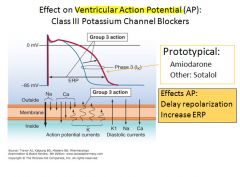
Known for prolongation of QT and increased risk of Torsades
|
|
|
Amiodarone (class III):
|
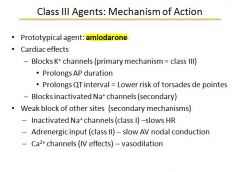
|
|
|
Indications for use of Amiodarone (class III):
|
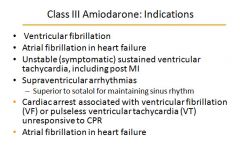
|
|
|
Adverse affects of amiodarone (class III):
|
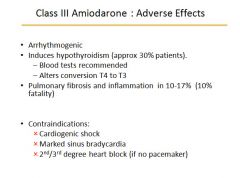
|
|
|
Sotalol (class III):
|
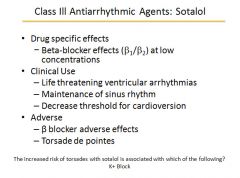
|
|
|
MOA of class IV antiarrythmics Diltiazem and
Verapamil: |
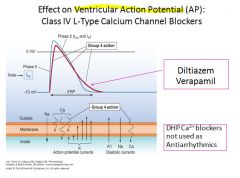
|
|
|
Diltiazem and Verapamil (class IV antiarrythmics):
|
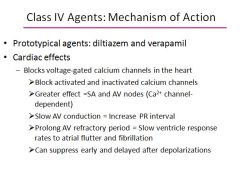
SA & AV nodes are directly dependent on Ca channels for their activation so much more effected when these channels are blocked.
|
|
|
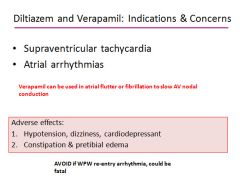
Indications for use of Diltiazem and Verapamil:
|
|
|
|
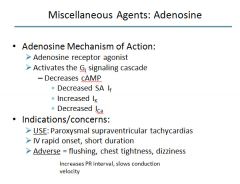
Adenosine:
|
|
|
|
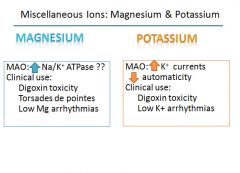
Magnesium and Potassium:
|
|
|
|
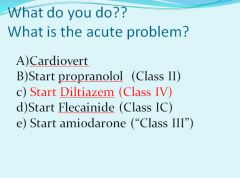
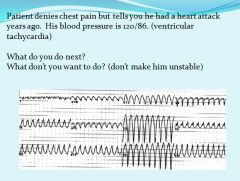
No propranolol; could cause major problems
Flecainide is not available as an IV drug and is not an AV node blocking agent Amiodarone; takes too long to work |
|
|
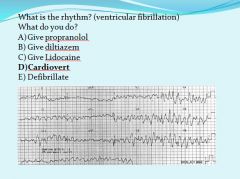
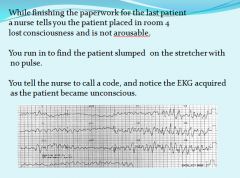
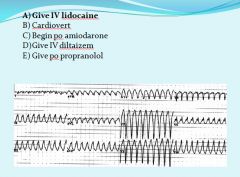
Cardioversion is synchronized to give a shock on the QRS, whereas defibrillation is a random shock
|
|
|
|
|
|
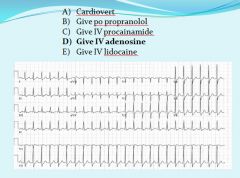
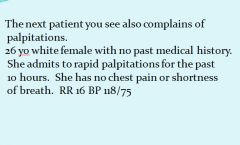
Giving adenosine is like cutting the AV node off for about 6 seconds.
|
|
|
Strategies for increasing O2 supply or decreasing demand in ischemia:
|
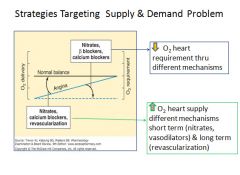
|
|
|
MOA of nitric oxide donors:
|
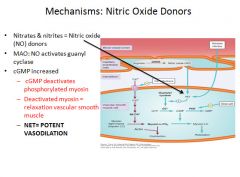
|
|
|
Effect of nitrates on cardiac function:
|
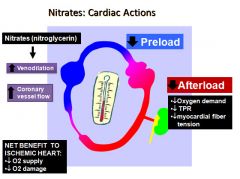
More venodilation with nitrates, so tend to decrease preload most.
Decreases oxygen demand via less wall stress and decreased total peripheral resistance. Reducing afterload will increase the amount of blood flow out of the aorta and improve coronary blood flow. |
|
|
Indications for Nitrate therapy:
|
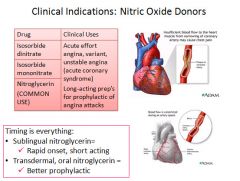
Tolerance to nitrates may develop over time.
Patches are usually worn during the day and taken off at night to prevent this from occuring. |
|
|
Adverse effects of Nitrate therapy:
|
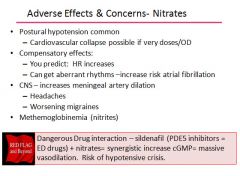
|
|
|
MOA of calcium channel blockers in treatment of angina:
|
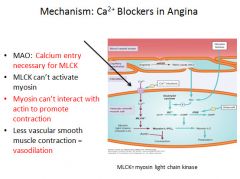
|
|
|
Use of calcium channel blockers in treatment of angina:
|
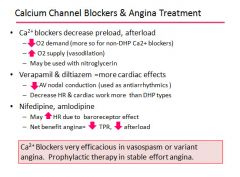
|
|
|
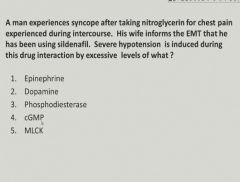
cGMP
|
|
|
Beta blockers used in treatment of angina:
|
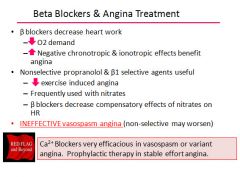
|
|
|
Ranolazine:
|
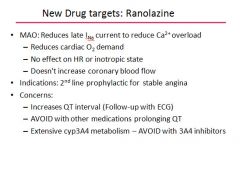
This drug is also a K+ channel blocker; that is why it can cause QT prolongation.
|
|
|
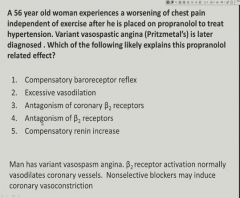
Antagonism of coronary B2 receptors
|
|
|
Therapies used as an adjunct to drugs for angina:
|
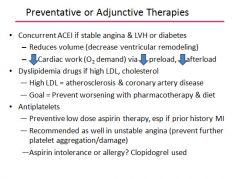
|
|
|
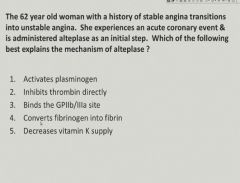
Activates plasminogen
|
|
|
Treatment when stable turns to unstable angina:
|

|
|
|
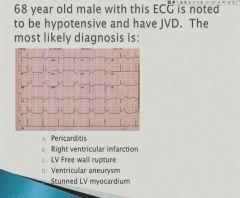
During what time after an MI is a patient at risk for myocardial rupture?
|
Between 3-7 days; dead tissue is being removed and collagen is being laid down - if not enough collagen is in place, you can get a rupture.
|
|
|
Right ventricular infarction
OR it could have been ventricular free wall rupture |
|
|
Predictors of outcomes post MI:
|
1) the most important is the LV ejection fraction. If the EF is under 30% the patient should receive an implanted difibrillator.
2) negative indicators are arrythmias and recurrent ischemia 3) ETT can be used to stratify risk in patients 4) Post MI patients can receive therapy including B-blockers, statins, ACE inhibitors and in patients with LV dysfunction aldosterone antagonist are used. |
|
|
Initial treatment for all ACS syndromes:
|
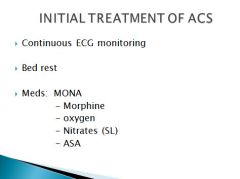
ASA = aspirin
|
|
|
What are the two initial treatments for unstable angina and NSTEMI?
|
Anti- ischemic therapy
Anti-thrombotic therapy (even more important in NSTEMI) |
|
|
Anti-ischemic therapy:
|

|
|
|
Anti-thrombotic therapies:
|
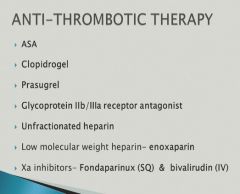
|
|
|
What is the first thing you should give a patient who has signs of ACS?
|
An aspirin!
|
|
|
Clopidrogel (Plavix):
|
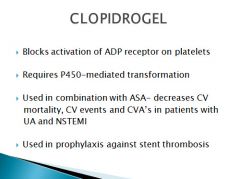
Also called Plavix
P450 system has great variability due to differences in genetics. Prasugel: Same mechanism of action as clopidrogel More potent anti-platelet agent Metabolized more evenly in most patients More risk |
|
|
Abciximab:
|
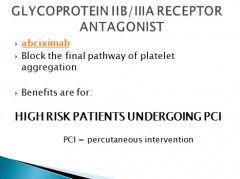
|
|
|
Heparin:
|
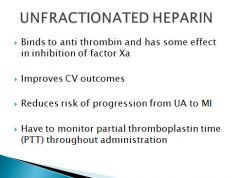
|
|
|
Enoxaparin:
|
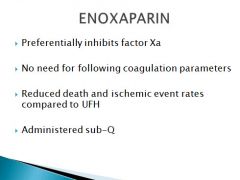
|
|
|
Treatment protocol for patients with US/NSTEMI:
|
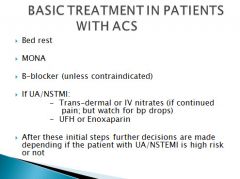
Beta blockers contraindicated in asthmatics and those with bradycardia.
|
|
|
TIMI score for stratifying risk for patients with UA/NSTEMI adverse outcomes:
|
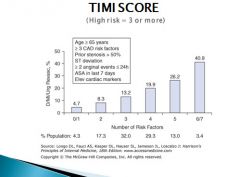
If the patient has a TIMI score higher than 3 the treatment will be different.
|
|
|
Decision tree with TIMI scoring:
|
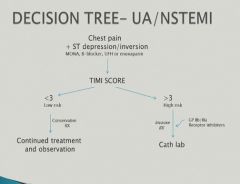
Plavix is used in patients who are expected to undergo only minor surgery.
Plavix should not be given to patients who might need to have more invasive surgery. |
|
|
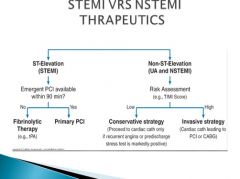
Treatment of STEMI:
|
- Goal is to open completely occluded artery
- Fibrinolytics - Percutaneous coronary revascularization; superior to fibrinolytic therapy if able to be performed in < 90 min from hospital presentation |
|
|
STEMI vs NSTEMI therapeutic decision tree:
|
|
|
|
Risk assessment and treatment combined table:
|
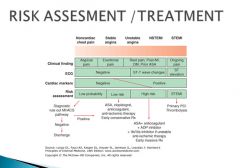
|
|
|
Therapy to start after an MI:
|
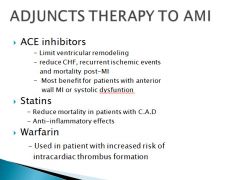
|
|
|
One more time, what does everybody get when they come in with an MI?
|
Morphine, Oxygen, Nitrates, Aspirin, Beta blocker (unless contraindicated) and Heparin (even if the patient ultimately receives fibrinolytics)
|

