![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Obj.
1. Describe the urinary bladder |
-pelvic organ
-enters abdomen when full (or always in children) |
|
|
Obj.
1. Describe the urinary bladder parts |
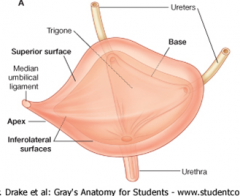
-apex (median umbilical ligament)
-body -fundus (base, related to seminal vesicles or uterus/vagina) -neck (surrounds urethra, attached to prostate) |
|
|
Obj.
1. Describe the urinary bladder surfaces |
superior
inferolateral (2 surfaces) posterior ( base) |
|
|
Obj.
1. Describe the urinary bladder related structures. |
-receives the R & L ureters @ the angles of the smooth-walled trigone
-inferior to peritoneum -separated from the pubic bones by the retropubic space |
|
|
Obj.
2. Describe the blood supply of the urinary bladder. |
arteries:
-superior vesical arteries (branch from umbical artery) supplies anterosuperior bladder gives off artery to ductus deferens (in males) -inferior vesical/vaginal artery supplies neck & fundus veins: -correspond w/ arteries ^ |
|
|
Obj.
2. Describe the innervation (sympathetic & parasympathetic) of the urinary bladder. |
sympathetic: T11-L2
parasympathetic: pelvic splanchnic nerves S2-S4 (via inferior hypogastric plexus) |
|
|
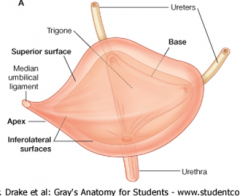
Obj.
3. Identify the parts of the urethra |
-intramural/preprostatic part (surrounded by internal urethral sphincter
-prostatic urethra (traverses prostate gland) -membranous part (in deep perineal pouch, surrounded by external urethral sphincter) -spongy part (penile) |
|
|
Obj.
4. Describe the prostate gland and its gross features and function. |
features: glandular component enclosed by fibrous capsule
functions: produces milky alkaline fluid containing citric acid & acid phosphatase, to neutralize acidity of vagina |
|
|
How does prostatic fluid empty into the prostatic urethra?
|
through individual openings in the prostatic sinuses (on either side of seminal colliculus)
|
|
|
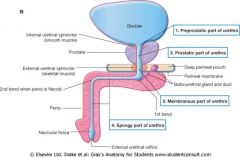
Obj.
5. Describe the testes |
-sperm produced in seminiferous tubules
-sperms stored in body of epididymis -tail of epididymis becomes vas deferens -tunica vaginalis encloses testes, visceral & parietal peritoneal layers, small amount of fluid btwn -tunica albuinea, tough outer surface |
|
|
Obj.
5. Describe the testes artery supply |
testicular artery (from aorta @ L2)
|
|
|
Obj.
5. Describe the veins draining the testes |
pampiniform plexus of veins
^becomes testicular vein @ level of deep inguinal ring ^^R testicular v drains into IVC, L drains into left renal v first |
|
|
Obj.
5. Describe the testes lymphatics |
lateral (paraaortic) nodes
- drains toward abdominal cavity *testicular cancer most common malignancy in young males |
|
|
Obj.
5. Describe the testes innervation. |
-sympathetic fibers run w/ testicular artery from renal or aortic sympathetic plexuses
-afferent sensory nerves accompany efferent sympathetic fibers |
|
|
Obj.
6. Name the lobes of the prostate |
middle lobe = central zone
posterior lobe = peripheral zone |
|
|
Obj.
6. Describe various clinical conditions affecting specific lobes of the prostate. |
benign prostatic hyperplasia (BPH):
typically the middle lobe/central zone,compression of prostatic urethra resulting in nocturia, dysturia, & urgency to urinate Prostate cancer: typically posterior (P) lobe/peripheral zone tends to obstruct urinary flow late in the disease metastasis to vertebrae, brain, & spinal cord |
|
|
Obj.
7. Trace the passage of sperm cells from the testes to outside the body. |
Testes (seminiferous tubules)--> epididymis--> Ductus (vas) deferens--> seminal vesicle--> ejaculatory ducts--> prostates--> urethra-->bulbourethral glands--> spongy (penile) urethra
|
|
|
The ureters cross the pelvic brim near _____________________
|
bifurcation of the common iliac arteries
|
|
|
In males, the ureters are crossed superiorly by the __________ near the entrance to the bladder
In females, crossed anteriorly & superiorly by ____________ at the base of the broad ligament |
ductus deferens
uterine artery |
|
|
What inhibits the reflux of urine into the ureter?
|
pressure from a filling bladder & detrusor muscle contraction
* the ureters traverse the wall of the bladder in an oblique direction |
|
|
Autonomic fibers from __-__ are carried in the renal, aortic, superior & inferior hypogastric plexuses
|
T11-L2
|
|
|
GVA fibers accompany (sympathetic/parasympathetic) nerves
|
sympathetic
|
|
|
Passage of a kidney stone produces ___________________ pain
|
"loin-to-groin"
|
|
|
The urinary bladder is supported by the pelvic diaphram and what ligaments (in male & female)?
|
-pubovesical (female, attach neck of bladder to pubic bones)
-puboprostatic (male, attach to prostate) |
|
|
What is the most common type of tumor in urinary tract?
|
tumor of urinary bladder
*can involve prostate, seminal vesicles, rectum or uterus & vagina |
|
|
If a mass is felt on the anterior aspect of the vagina, where is a tumor likely located?
|
bladder
|
|
|
In males, a vesical venous plexus, is continuous with the ____________ plexus, draining the fundus of bladder, prostates, seminal vesicles, ductus deferens, & penis
|
prostatic venous plexus
|
|
|
The vesical venous plexus mainly drains to internal iliac veins by may also drain into ________ veins into the ___________ plexus
|
sacral veins
vertebral venous plexuses *route for metastasis to vertebral column, pelvic bones, & skull |
|
|
Muscle fibers toward neck of bladder in males forms an involuntary _________________.
|
internal urethral sphincter
|
|
|
Differentiate btwn parasympathetic & sympathetic effects on the internal urethral sphincter
|
parasympathetic-
relaxation of sphincter & contractions of detrusor muscle = bladder emptying sympathetic- contraction of sphincter = inhibition of emptying & prevention of retrograde ejaculation of semen into bladder |
|
|
Most undescended testes descend into the scrotum during the first 3 months. If they do not, what is it referred to as and what does it lead to?
|
-cryptorchidism (undescended testes)
-leads to increased incidence of testicular cancer & sterility *testes 2-7 degrees C lower than body, necessary for spermatogenesis |
|
|
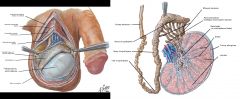
Describe the descent of testes (development)
|
1. primordial testes dvlp in lumbar area, post abdominal wall, ant/inf to dvlping kidneys
2. gubernaculum testes attached to caudal pole guide descent to future scrotum 3. process vaginalis (peritoneal evagination) accompanies testes descent 4. descent creates passageway= inguinal canal w/ inguinal rings 5. testes acquire coverings from external oblique aponeurosis (external spermatic fascia), internal oblique muscles (cremaster muscle & fascia) & transverse fascia (internal spermatic fascia) as they descend 6. Eventually testes become suspended in scrotum by spermatic cords *3rd-7th month, descend retroperitoneally to deep inguinal rings through inguinal canal |
|
|
What do the spermatic cords contain?
|
-ductus (vans) deferens
-blood vessels testicular artery pampiniform plexus of veins (testicular vein) -nerves genital branch of genitofemoral nerve -lymphatics |
|
|
A persistent processus vaginalis leads to what?
|
-accumulation of fluid w/i cavity of tunica vaginalis
-fluid may be: hydrocoele (serous fluid, appears as reddish glow upon transillumination) hematocoele (blood) spermatocoele (sperm-filled cyst, near head of epididymis, usually asymptomatic) |
|
|
What nerve provides the motor component of the "cremaster reflex"?
|
genital branch of genitofemoral nerve
*ilioinguinal nerve = sensory component |
|
|
What causes "bag of worms"?
|
varicocoel of spermatic cord, caused by elongation & dilation of pampiniform plexus of veins, due to defective valves
*usually on left side, adolescents |
|
|
Recognize parts of the epididymis
|
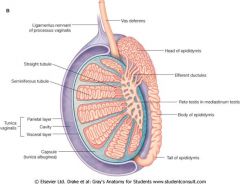
-head
superior, expanded portion, composed of lobules -body sperm stored in convoluted duct while they mature -tail becomes vas deferens |
|
|
Obj.
4. Describe the gross features and function of vas deferens |
features:
cordlike-structure in spermatic cord passes through inguinal canal enters abdominal cavity posterior to urinary bladder supplied by artery to ductus deferens (arising from sup or sometimes in vesical artery) continuation of tail of epididymis terminal part is ampulla of ductus deferens functions: transmits spermatozoa from epididymis to ejaculatory duct |
|
|
what does a vasectomy/deferentectomy accomplish?
|
prevents sperm from passing to urethra by interrupting vas deferens
-sperm degenerates in epididymis/proximal urethra |
|
|
Obj.
4. Describe the gross features and function of the seminal vesicle |
features:
distally joins ductus deferens to form ejaculatory duct functions: contributes alkaline fluid, containing fructose for spermatozoa nutrition, to seminal fluid |
|
|
The ejaculatory duct is formed by the union of what 2 things?
What does it open into? |
seminal vesicle & ductus deferens
opens into prostatic urethra through the seminal colliculus (verumontanum) together w/ prostatic utricle opening |
|
|
The ejaculatory duct traverses the posterior prostate, separating what 2 lobes?
|
middle lobe (central zone)
posterior lobe (peripheral zone |
|
|
The prostate's lymphatic drainage is mainly into the _______________________ nodes
|
internal iliac nodes
|
|
|
Prostatectomy involves removal of the prostate & seminal vesicles, this may damage the _________________________, which form the cavernous nerves.
What would this nerve damage lead to? |
parasympathetic fibers (pelvic splanchnic nerves S2-S4) in the prostatic nerve plexus
leads to impotency |

