![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Describe the epidemiology of STIs
|
- Large increased on almost all STIs from 1998-2007
- Early Syphilis increased from 139 to 2680 cases - Uncomplicated Gonorrhoea increased from 13,212 to 18,710 cases - Genital chlamydia increased from 48,726 to 121,986 cases - Symptomatic HIV diagnoses have increased only from 814 to 833. However, asymptomatic HIV has increased from 1540 to 5949 cases - Total new STI diagnoses have increased from 244,282 to 397,990 |
|
|
Describe the classification of STIs on the basis of presentation
|

Red = not transmitted sexually
|
|
|
What are some of the causes of urethritis in men?
|
- Most common causes:
• Neisseria gonorrhoea • Chlamydia trachomatis - Non-specific urethritis = males present with discharge and dysuria • Ureaplasma urealyticum • Mycoplasma genitalium • ‘True’ NSU • Trichomonas - No cause found in 20-50% - Contact tracting important - Responds well to antibiotics |
|
|
Describe the prevalence of chlamydia infections
|
Prevalence
- The commonest bacterial STI. - 10% sexually active women in the UK, age <25 - Incubation period few days to weeks - 70% of women and 50% of men are asymptomatic - Responds well to treatment Extra genital infection possible but uncommon |
|
|
Describe the complications of chlamydia
|
Complications:
- PID = asccending infection presenting as endometritis or salpingitis - Infertility - Ectopic pregnancy - Chronic pelvic pain - Opthalmia neonatorum (in infants through vaginal births) - Chlamydia pnemonitis (also in infants = more serious) |
|
|
What is the cause of chlamydia?
|
- Chlamydiae are obligate intracellular bacteria
- Chlamydial infection is initiated by attachment of a chlamydial elementary body to the host cell, followed by its entry into the cell. - The chlamydial elementary bodies are internalised in tight, endocyctic vesicles, within which they differentiate into reticulate bodies - The reticulate body replicates eventuallly reverting back to elementary bodies, which leave the cells to infect other cells |
|
|
Describe the symptoms associated with chlamydia in females
|
- Organism replicated and infects within the epithelium of the cervix and urethra
- None - Abdominal pain: Endometritis - Severe abdominal pain & dyspareunia: - Acute PID - Perihepatitis - Vaginal discharge: cervicitis - Post coital or intermenstrual bleeding: mucopurulent cervicitis - Joint pain/swelling: reactive arthritis |
|
|
What are the conditions associated with chlamydia in infants?
|
- Preterm delivery & low birth weight
- Opthalmia neonatorum (neonatal conjunctivitis) - Neonatal pneumonitis if untreated |
|
|
Describe the common symptoms associated with chlamydia in men
|
- None
- urethral discharge: Non-specific urethritis - Penile rash: Circinate balanitis - Testicle pain: orchitis & epididymitis - Joint pain/swelling: reactive arthritis - Reiters syndrome = urethritis. conjunctivitis and arthritis are the classical triad of clinical manisfestations with this syndrome (and predominantly occurs in males) |
|
|
Describe the investigation of chlamydia
|
Specimen collection
- Essential that cells are present in the sample as intra-cellular pathogen - Males = urethral swab or 1st catch urine - Females = endocervical swab, with pus first removed from the cervix - Urine = less sensitive but good for population screening and less painful and easy to carry out (no trained professional) - Neonates = eye swab and FBCs to check WCC Diagnosis 1. Cell culture = obligate intracellular so won't grow on lab media = can used tissue culture but very expensive so now other methods 2. Immunofluorescence = specimen fixed to a slide and stained with a monoclonal Ab tagged with flurescein. Subject to observer error and time-consuming but the cellular quality of the sample can be assessed 3. Enzyme immunoassay (EIA) = uses commercial kits and large numbers of samples processed easily 4. Polymerase chain reaction (PCR) = high sensitivity and specificity. PCR directed against nuclear protein in the plasmid |
|
|
Describe the treatment of chlamydia
|
- Doxycycline
100mg twice a day for seven days OR - Azithromycin 1gram single dose |
|
|
Describe the prevalence of gonorrhoea
|
- N gonorrhoeae is the second most common bacterial STI
- Over 18,000 infections diagnosed in 2007. - Peak age: Males aged 20-24 years and females aged 16-19 years. - Found predominantly in urban areas. - Incubation period 2-5 to days - Much more prevalent in males - Associated with social deprivation, being unmarried, early onset of sexual activity and urban residency - Highly infectious: single exposure affects 60-90% of females and 20-50% of males |
|
|
Describe the presentation of gonorrhoea in men and its complications
|

Presentation:
- May cause urethral discharge, dysuria and tender inguinal lymph nodes - Pus, mucopus, or clear mucus discharges spontaneously from the urethra - Most noticeable after holding urine overnight - Often accompanied by burning sensation during urination - Suggests a sexually acquired urethral infection - Infections may cause urethral discomfort and dysuria without discharge Complications - Less commonly - epididymo-orchitis, abscess of paraurethral glands, urethral stricture - Extragenital problems - rectal pain and discharge, pharyngitis, conjunctivitis - Disseminated gonococcal infection infection - skin, joints, heart valves |
|
|
Describe the presentation of gonorrhoea in females and its complications
|
Presentation:
- Primarily infects the cervix and urethra (note: only infects columnar cells) - May lead to an acute cervicitis with vaginal discharge and 'urethral syndrome' where the urethra is infected Complications: - Pelvic inflammatory disease (occassionally with tubo-ovaruan abscess) - Bartholins abscess - Disseminated gonococcal infection (pain on the joints, tenosynovitis and rash) |
|
|
Describe the microbiology of gonorrhoea
|
- Gram negative intracellular diplococcus
- Fastidious growth requirements = requires culture on chocolate agar - Humans = only natural host - Primarily infect columnar epithelium → Lower genital tract, rectum, pharynx, conjunctiva, - Transluminal spread to prostate, epididymis/ endometrium/ pelvic organs - Rare: haematogenous spread |
|
|
Describe the diagnosis of gonorrhoea
|
- Neisseria gonorrhoea is a fragile gram negative diplococci that does not survive transportation well
- Specimens • In females - endocervial swab, urathral swab and pharyngeal swab • In males - urethral (first thing in the morning), rectal and pharyngeal swabs - Diagnosis 1. Gram Stain - Gm negative diplococcie 2. Culture / sensitivities = more sensitive than microscopy and antibiotic senstivities found. Only grows on chocolate plates |
|
|
Describe the treatment of gonorrhoea
|
- May vary in sensitivitis
- Initial therapy is usually guided by severity of symptoms and local knowledge of sensitivity patterns - Penicillin resistance common - Should eradicate 95% of GC in that community • Ceftriaxone 250mg IM stat • Cefixime 400mg po stat • Ciprofloxacin 500mg po stat • Amoxycillin 3g +Probenecid 1g po stat |
|
|
What questions should be asked if the patient has persistant urethral discharge?
|
1. Was the treatment completed?
2. Has the patient re-exposed himself to an STI? 3, Is he ‘milking’ the discharge? (may cause inflammatory discharge rather than due to infection) |
|
|
Describe the epidemiology of Herpes Simplex virus
|
- Herpes simplex virus
• Type 1 • Type 2 - Most common cause of genital ulcer in the World. - HSV infection worldwide is increasing - Coventry:- • GUM – HSV2 antibody – 22% - HSV 1 antibody – 60% • In HIV positive, African → HSV 1 causes coldsores → HSV 2 more common cause of genital herpes • Caucasians:- → HSV 1 causes coldsores and more common cause of genital herpes → HSV 2 causes genital herpes less often |
|
|
Describe the clinical features of primary genital herpes
|
- Primary infection
→ First attack of G.H → Recurrent herpes - Primary infection: • Usually Severe • Erythematous papules → vesicles → ulceration • Ulcer – superficial ◘ erythematous edge ◘ greyish base ◘ intensely painful ◘ Severe external dysuria ◘ Bilateral ◘ Tender inguinal lymphadenopathy • Symptoms more severe in women and MSM • Systemic Symptoms ◘ Headache ◘ Myalgia |
|
|
Describe some of the complications associated with primary genital herpes
|
• Local
- super infection - urinary retention - Labial adhesive • Systemic - Signs of meningeal irritation - autonomic nervous system dysfunction is rare - transverse myelitis |
|
|
Describe the clinical features of recurruent genital herpes
|
- Usually milder and shorter duration (8-12 days)
- Women > men - Unilateral - Few Vesicles - Inguinal lymphadenopathy occurs in 25% of patients - Dysuria is uncommon |
|
|
How are genital herpes treated?
|
Recommended regimens (all for five days):
• Aciclovir 200 mg five times daily • Famciclovir 250 mg three times daily • Valaciclovir 500 mg twice daily |
|

Describe syphilis
|
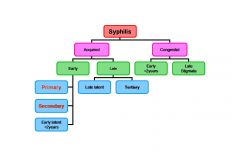
- Primary syphilis presents as ulcer (chancre) formation of usually the genitalia (but can occur anywhere and point of initial exposure)
- It is important to diagnose the ulcers early as they are self-healing and painless = can easily be missed if the patient does not present to the doctor - Secondary syphilis may present as a symmetrical reddish-pink non-itchy rash on the trunk and extremities. The rash can involve the palms of the hands and the soles of the feet. Mucous patches may also appear on the genitals or in the mouth. Most contagious here as all rash and lesions contain the virus - Diagnosis • Direct: demonstration of Treponema pallidum → Dark field microscopy → Direct fluorescent antibody (DFA) test → PCR • Indirect: different serological test → VDRL → TPPA → EIA |
|
|
Describe the Human Papilloma Virus (HPV)
|
- Genital warts caused by HPV are the commonest STI diagnosed at GUM clinics throughout the UK
- Over 100 HPV types have been described - however, the vast majority of individuals infected with HPV fail to develop warts - Warts are unsightly and difficult to treat - The main concern with the virus is the strong association of certain high risk types with cervical carcinoma - although these types don't cause the warts it is possible to be infected with numberous strains at once |
|
|
Describe the trichomonas vaginalis infection
|
- T. vaginalis is a flagellated protozoan.
- Almost exclusively sexually transmitted. - Frothy yellowish vaginal discharge (30%) - Vulval itching, dysuria, offensive odour. - Responds to Metronidazole |
|
|
Describe bacterial vaginosis
|
- Commonest cause of abnormal discharge in women of childbearing age.
- Prevalence from 5% to 50%. - Overgrowth of anaerobic organisms in the vagina - Remit spontaneously in sexually active and non- active women. - Not regarded as a sexually transmitted disease. |
|
|
Describe candidiasis
|
- Candida albicans 80-92%
- Thick white discharge with itching and vulval soreness - Common in women of childbearing age - 10-20% women can be asymptomatic - Treatment: Azole therapy topical or oral - Not transmitted sexually |
|
|
List some other STIs
|
- Chancroid
- LGV - Donovanosis - Molluscum contagiosum - Scabies - Pubic lice |
|
|
Describe the general treatment of STIs
|
- Multiple infecctions are common, so patients presenting with one infection should be screened for a number of other infections (especially important as many infections are asymptomatic or only become symptomatic later)
- Antibiotic therapy is usually initiated on the initial visit and regimes that ensure compliance are utilised - Important part of management is contact tracing of sexual partners - Patients should also receive health education, advice on contraception and instruction in safe sex |
|
|
How can infection spread into the female pelvis?
|
A) Bloodbourne
B) AIrbourne C) Direct ascending from genital tract (most common) D) Direct from GI tract e.g. during gynae surgery if torn E) Lymphatic spread - Particularly susceptible due to direct ascending route |
|
|
What is pelvic inflammatory disease?
|
- Clinical syndrome in females, unrelated to pregnancy or surgery, whereby organisms ascend from the cervix, via the uterus, to the uterine tubes and contiguous pelvic structures to produce inflammatory conditions
|
|
|
List the types and sites of PID
|
- Endometritis = endometrial canal
- Salpingitis = tubes - Oophoritis = ovary - Parametritis = generalised infection of uterine tissue - Pelvic peritonitis = general pelvic peritoneal inflammation - Tubo-ovarian abscess = large pockets of pus around the tubes and ovary (TOAs) |
|
|
What are the effects of inflammation on pelvic structures?
|
- Classic inflammation: rubor,calor,dolor,turgor
- Oedema → obstruction / paralysis of cilia = important in function 1. Hydrosalpinx = full of fluid 2. Pyosalpinx = full of inflammatory exudate (pus) 3. Eventually get Fibrosis = scarring, tethering / adhesion 4. Occlusion of tube 5. This will lead to chronic pain, ectopic pregnancies and infertility |
|
|
What are the risk factors of PID?
|
- Increasing number of sexual partners
- Exposure to STI - No barrier contraception - ? IUCD (but now less common due to aseptic technique) - Common – 1 in 60 visits by women <45 years so important as expensive to government and individual |
|
|
What are the symptoms of PID?
|
On history:
- Mild disease may be fairly symptoms free but its diagnosis and treatment is vital - Lower abdominal pain = often bilateral - Dyspareunia - vaginal discharge - feverish/ unwell - menstrual abnormalities |
|
|
What are the signs of PID?
|
- Elevated Temperature
- Lower abdominal tenderness = may have guarding and rebound tenderness - Bimanual tenderness over uterus and ovaries - Cervical motion tenderness / excitation = acute discomfort when move cervix - PID shuffle = move slowly as don’t want to move organs - But little sensitivity or specifivity on exam so make differentials - Markers of inflammation including raised WCC, CRP and ESR may be noted |
|
|
List some differential diagnoses of PID
|
1. Urinary Tract : Cystitis, pyelonephritis, renal stones
2. GI Tract: Appendicitis, Inflammatory bowel disease, Diverticulitis 3. Reproductive Tract : Ectopic pregnancy, ovarian cysts (rupture, torsion), Septic abortion (miscarriage introducing infection), septic retained placenta |
|
|
Describe the diagnostic threshold of PID
|
- High index of suspicion
- Low threshold to diagnose and treat - Based on history and clinical findings - Sequelae serious so need to seriously consider treatment as early as possible |
|
|
What investigations could be carried out to investigate PID?
|
- Blood tests – hCG, CRP WBC
- Urine tests – urinanalysis, microscopy - Ultrasound - Laparoscopy – look and see - Endocervical swabs – identify organisms that trigger PID e.g. gonococcus and chlamydia |
|
|
Describe the microbiology of PID
|
- Organism depends on where the PID is and the history (e.g. past surgery)
- By the time there is generalised pelvic infection it is always polymicrobial - Organisms include: • Chlamydia trachomatis • Neisseria Gonorrhea • Mycoplasmas • Bacteroides • Other Anaerobes • Polymicrobial • Actinomyces – primarily associated with IUCDs |
|
|
Describe the management of PID
|
- Early and adequate-reduce tubal damage and significant consequences
- Inpatient – if seriously unwell, low WCC and high temperature VS outpatient = usually if think they’ll be compliant and not too unwell and no serious signs - Antibiotics - Analgesia - Abstinence = contraception and sexual practises = education |
|
|
What are some of the consequences of PID?
|
- Due to tubal damage = as inflammation heals get fibrosis and tethering and adhesion
- Chronic pelvic pain= 20% as adhesion → pulled organs - Ectopic pregnancy = if damaged, narrowed tubes - Infertility ( one episode=10%) ( two episodes= 20-30%) ( three episodes=> 50%) - Advise patient of risks on episodes |
|
|
How can PID be prevented?
|
- STD screening / treatment
- Barrier contraception - Avoid promiscuity |

