![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
What three things influence ventilatory control?
|
Cerebral input, mechanical receptors, and chemoreceptors
|
|
|
Cerebral input, mechanical receptors, and chemoreceptors all channel ventilation control to what part of the brain?
|
Brain Stem Respiratory Centers
|
|
|
What are the two carotid body chemoreceptors?
|
PO2 and PCO2
|
|
|
Changes in the PO2 and PCO2 are sent to what part of the brain?
|
Medullary centers
|
|
|
PAO2 below 60mm/Hg does what? Below 30-40mm/Hg?
|
increases ventilation.
may supress respiratory drive |
|
|
Increased CO2 does what?
|
Stimulates respiratory center and increases ventilation
|
|
|
Hypoxemia
|
Low blood oxygen
|
|
|
Hypercapnia
|
High CO2 levels (end tidal increase of 15mm/Hg or more)
|
|
|
Basal metabolic rate does what during sleep? What does it affect?
|
Decreases.
It decreases minute ventilation. |
|
|
Where are respiratory centers located?
|
pons and medulla
|
|
|
What controls inspiratory volume and respiratory rate?
|
pneumotaxic center
|
|
|
What controls voluntary control of ventilation?
|
Cerebral cortex
|
|
|
Cheyne stokes is most prevalent in what two conditions?
|
CHF and central nervous disease
|
|
|
What three ways can UAR be measured?
|
1.Pressure transducers
2.Respiratory muscle activity 3.esophageal balloon manometry |
|
|
Obesity hypoventilation syndrome would show:
|
An increased respiratory rate and profound desaturations in REM, abd/thor in sync
|
|
|
Negative deflections in Pes monitoring indicates?
|
Obstruction (increased intrathoracic pressure)
|
|
|
What device provides a direct measure of airflow?
|
Pneumotach
|
|
|
When do most arousals occur during an obstructive event?
|
Just before breathing resumes
|
|
|
Ventilation invloves three different pressures:
|
atmospheric, intraalveolar, and intrapleural.
|
|
|
Forced vital capacity
|
maximum forced air out of lungs
|
|
|
Tidal volume
|
air in or out during normal respiration
|
|
|
Residual volume
|
air left in lungs after maximum exhale
|
|
|
Expiratory reserve volume
|
Additional air that can be breathed out after a normal exhale.
|
|
|
Inspiratory reserve volume
|
Additional air that can be breathed in after a normal inhale.
|
|
|
Functional residual capacity
|
air left in the lungs after a tidal breath out
|
|
|
Inspiratory capacity
|
volume that can be inhaled after a tidal breath out
|
|
|
Anatomical dead space of lungs
|
Volume of the conducting airways
|
|
|
Physiologic dead volume
|
anatomic dead space plus alveolar dead space
|
|
|
A person at sea level has a _____lung capacity compared to one from a high altitude
|
smaller
|
|
|
What is air like in high altitude
|
Less dense so it takes more too fully oxygenate.
|
|
|
Total lung capapcity
|
IRV + TV + ERV + RV
|
|
|
Vital capacity
|
IRV + TV + ERV
|
|
|
Restrictive diseases spirometry presentation
|
decreased volumes, FEV1/FVC in normal range (.08-1)
|
|
|
Obstructive diseases spirometry presentation
|
Volumes are normal but flow rates are impeded. FEV1/FVC low
|
|
|
What do obstructive diseases do?
|
Cause a narrowing or bloackage or the airways, decreasing exhaled airflow.
|
|
|
What do restrictive airway diseases do?
|
loss of lung tissue, decrease the lungs ability to expand, decrease lungs ability to transfer oxygen.
|
|
|
Obtructive lung disease examples:(3)
|
COPD, emphysema, asthma
|
|
|
Restrictivelung disease examples:(4)
|
pulmonary fibrosis, sarcoidosis, cancer, pneumonia
|
|
|
What is the phrenic nerve?
|
Carries signals from C3-5 to the diaphram, part of the pituary gland.
|
|
|
A right shift in the oxygen dissociation curve indicates:
|
decrease in the affinity of hemoglobin for oxygen (requiring a higher pressure to maintain same oxygen saturation)
|
|
|
A left shift in the oxygen dissociation curve indicates:
|
increase in the affinity of hemoglobin for oxygen (making oxygen easier to pick up but harder to release)
|
|
|
Typical norm of the oxygen dissociation curve
|
P50= A SaO2 takes 26.6mm/Hg
|
|
|
How is the oxygen dissociation curve shifted to the right?
|
increase in temp, increase in PCO2, and a decrease in pH
|
|
|
How is the oxygen dissociation curve shifted to the left?
|
decrease in temp, decrease in PCO2, and a increase in pH
|
|
|
Hyperthermia does what to the oxygen dissociation curve?
|
rightward shift
|
|
|
Carbon monoxide does what to the oxygen dissociation curve?
|
shifts left
|
|
|
Abnormal hemogobin does what to the oxygen dissociation curve?
|
shifts left
|
|
|
Fetal hemoglobin does what to the oxygen dissociation curve?
|
shifts left (enchances placental uptake of oxygen)
|
|
|
Obstructive diseases spirometry presentation
|
Volumes are normal but flow rates are impeded. FEV1/FVC low
|
|
|
What do obstructive diseases do?
|
Cause a narrowing or bloackage or the airways, decreasing exhaled airflow.
|
|
|
What do restrictive airway diseases do?
|
loss of lung tissue, decrease the lungs ability to expand, decrease lungs ability to transfer oxygen.
|
|
|
Obtructive lung disease examples:(3)
|
COPD, emphysema, asthma
|
|
|
Restrictivelung disease examples:(4)
|
pulmonary fibrosis, sarcoidosis, cancer, pneumonia
|
|
|
What is the phrenic nerve?
|
Carries signals from C3-5 to the diaphram, part of the pituary gland.
|
|
|
A right shift in the oxygen dissociation curve indicates:
|
decrease in the affinity of hemoglobin for oxygen (requiring a higher pressure to maintain same oxygen saturation)
|
|
|
A left shift in the oxygen dissociation curve indicates:
|
increase in the affinity of hemoglobin for oxygen (making oxygen easier to pick up but harder to release)
|
|
|
Typical norm of the oxygen dissociation curve
|
P50= A SaO2 takes 26.6mm/Hg
|
|
|
How is the oxygen dissociation curve shifted to the right?
|
increase in temp, increase in PCO2, and a decrease in pH
|
|
|
How is the oxygen dissociation curve shifted to the left?
|
decrease in temp, decrease in PCO2, and a increase in pH
|
|
|
Hyperthermia does what to the oxygen dissociation curve?
|
rightward shift
|
|
|
Carbon monoxide does what to the oxygen dissociation curve?
|
shifts left
|
|
|
Abnormal hemogobin does what to the oxygen dissociation curve?
|
shifts left
|
|
|
Fetal hemoglobin does what to the oxygen dissociation curve?
|
shifts left (enchances placental uptake of oxygen)
|
|
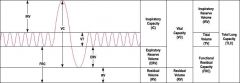
Lung Volume Diagram
|
Lung Volume Diagram
|
|
|
Normal PaO2
|
75-100mm/Hg
|
|
|
Normal PaCO2
|
35-45mm/Hg
|
|
|
Normal Ph
|
7.35-7.45
|
|
|
Normal SaO2
|
94-100%
|
|
|
Bicarbonate (HCO3)
|
22-26mEq/liter
|
|
|
Path of air:
|
mouth--larynx--trachea--bronchi--broncus--bronchi--broncioles---alveoli
|
|
|
Ideal gas law
|
P V = n R T
|
|
|
Inspiration process
|
diaphram down, ribcage elevates, increased inthrathoracic volume, decreased inthrathoracic pressure...high pressure air into low pressure lungs
|
|
|
Expiration process
|
diaphram up, ribcage depresses, decreased inthrathoracic volume, increased inthrathoracic pressure...low pressure air out of high pressure lungs
|
|
|
hemoglobin
|
iron contained oxygen carrier
|
|
|
Upper airways do what to inspired air?
|
cleans, warms, and humidifies
|
|
|
Upper airways do what to exspired air?
|
a quarter of the heat is recaptured and moisture is recaptured
|
|
|
How is air heated?
|
takes heat and moisture from the mucosa lining of the respiratory tract
|
|
|
How is heat and moisture recovered?
|
Cooled mucosa from inspiration causes the exhaled air to evaporate
|
|
|
What happens with excess moisture loss in the airway?
|
Reduced patency and lung compliance, gel layer thicker and cilia less able to move
|
|
|
orthopnea
|
decreased lung compliance and vital capacity when laying down
|
|
|
platypnea
|
flat breathing
|
|
|
dyspnea
|
SOB
|

