![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
TNF inhibitors SE |

|
|
|
Scleroderma Abs |
Anti scl70 - ILD ACA - pulm HTN RNA polymerase 3 Abs - renal crisis |
|
|
RA Activity Ax |
DAS 28 SCORE ESR Global health rating Total jt count Smalll jt count
Hx: duration morning stiffness, degree of jt and and level of fatigue |
|
|
Gout |
Decide acute/chronic Distribution + deformity Go on to CV exam as is a FR and look for Sx of CKD Ddx: septic arthritis - jt aspirate: neg birefringent crystals, phagocytosis of urate crystals, WCC 20 - 50000. SA > 50 000. Inx: uric acid (1/3 have N level at time of attack), UEC, lipids, bsl, ECG (CV risk factors). XRAY Mx: acute colchicine/NSAIDs/pred. Poor response: feboxustat. 40 then 80mg. Prophylaxis: start 1/12 after attack with prophylaxis for 6/12 Tophi aim ur < 0.3 |
|
|
5 types of psoariatic arthropathy and Inx
|
1. DIP predominant 2. RA pattern 3. Arthritis mutilans 4. oligoarticular (2-4 jts) 5. Axial Infalmmatory arthropathy Findings: nail changes, telescoping/shortening or digits, digit auto amputation |
|
|
Psoriatic arthropathyseronegative spondyloarthritides.
|
erosive change with bone proliferation symmetric polyarthropathy, or asymmetric oligoarthropathy. 30% with rash get arthropathy Inx: HLA B27 (60% +) Dactylitis (sausage fingers), enthesisis, marginal jt erosions, pencil-in-cup, acro-osteolysis (reabsorption of the distal phalanx) and telescoping DdX; RA (no bony proliferations), erosive OA, reactive (usually feet > hands) |
|
|
OA XRAY changes
|
Asymmetrical jt space loss Jt sclerosis Subchondral cyts Osteophytes Bouchards + Heberdens + squaring of base of thumb |
|
|
RA XRAY changes
|
Loss of joint space - symmetrical Marginal jt erosions Periarticular OP (disuse and steroids) Soft tissue swelling - tenosynovitis boutonniere and swan neck deformities, Z deformity, volar subluxation, MCP ulnar deviation Jts: 2-3rd MCP, ulnar styloid, triquetrum |
|
|
Feet RA changes
|
Feetsimilar to the hands, there is a predilection for the PIP and MTP joints (especially 4th and 5th MTP)involvement of subtalar jointposterior calcaneal tubercle erosionhammertoe deformityhallux valgus
|
|
|
TNF i Se |
Infusion reactions: acute and delayed Infection: neutropaenias in 75% - bacterial infections (particularly pneumonia), zoster, tuberculosis, and opportunistic infections. - FBE at 1/12 then 3/12 if stable Malignancy: mixed evidence lymphomas, leukemias, non-melanomatous and solid malignancies. Low risk: pulm fibrosis, hepatotoxicity Demyelinating HF Skin eruptions eg psoroasis Induced autoimminity eg lupus |
|
|
Dermatomyositis - Sx |
Heliotrope rash V Sx Shawl Sx Holster Sx Gottrons papules Ragged cuticles and prominent blood vessels on nail folds Poikiloderma (varying pigmentation) Calcinosis Myopathy Look for cancer! |
|
|
Dermatomyositis Inx |
Myositis: CK, AST, LDH, MRI, EMG, biopsy Skin biopsy: lupus erythematosus ANA + (most), anti-Mi-2, anti-Jo (ILD) Screen for Cancer! Skin checks! |
|
|
Lupus findings: need 4/11 ACR criteria |
Malar rash Discoid rash Photosensitivity skin rash Mouth or nose ulcers: usually painless Arthritis (nonerosive) in two or more joints, along with tenderness, swelling, or effusion. Serositis: pleurisy / pericarditis Neurologic disorder: seizures and/or psychosis Nephritis Hematologic disorder: hemolytic anemia, leukopaenia, thrombocytopaenia Immunologic disorder: dsDNA, anti-Sm, anti-cardiolipin ANA |
|
|
Gout discussion |
Presence of acute flare Chronic tophaeus gout - ? severity Polyarticular gouty arthritis Associations eg IHD, CKD, haematological malignancy Precipitants drugs, infection, dehydration, starvtion, surgery, trauma, fatty foods, Mx: urate lowering Rx, Ur targets |
|
|
Gout risk factors and Ddx |
RF: Hyperuricemia, Obesity, HTN, lipids, CVD, diabetes, CKD, high meat and seafood diet (dairy is protective), ETOH Meds: aspirin, allopurinol, thazides/loop diuretics. Ddx: septic arthritis, trauma, acute calcium pyrophosphate crystal arthritis (pseudogout), cellulitis, rheumatoid arthritis, spondyloarthritis |
|
|
What other systems to exam if have gout? |
CVS - BP and cardiac exam - ? CCF and diuresis as a ppt Renal - fluid balance, fistula, transplant Old - ? haematological malignancy eg LNs, hepatosplenomegarly, Sx BM failure |
|
|
Pregnancy and dmards |
Stop prior to conceiving: MTX - 3 months prior and breast feeding Leflonamide - do levels SSZ - reversible oligospermia, men stop 3 months prior Aspirin and nsaids - can use in 2nd trimester Steroids - cleft lip and gDM Biologics probs ok
|
|
|
Drug induced lupus |
Methyl dopa TNFi Procainamide Hydralazine Minocycline Isoniazid Phenytoin Anti histone +/- ANCA Abs |
|
|
Lupus nephritis classes and Tx |
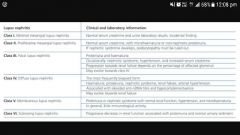
Tx Steroids and CYC or MMP AutoSCT |
|
|
Systemic sclerosis Ddx |
Gadolinum nephrogenic sclerosis GVHD Exposure PVC Drugs: bleomycin Eosinophilic fasciitis Diabetic induced skin thickening. |
|
|
Sx of Tx on exam |
MTX |
|
|
Nutritional ax on exam |
Bedside: grip strength and gait speed BMI and wait circumference Pallor > anaemia Stomatitis, SCDC, peripheral neuropathy > B12 def Glossitis, koilonys=chia >Fe def Gums > scurvy Skin integrity/wounds > micronutrients: zinc, selenium, copper Fat solube: K > eccymoses, A- night vision D - osteomalacia, scolosis, myopathy. |
|
|
Sx of synovitis |
Swelling Warmth Effusion Tenderness |
|
|
When to use Bactrim prophyaxis |
If > 20mg prednisolone/d for > 1 month with a second reason for immunosuppression eg TNFi (MTX is ok) Higher risk of PJP in DM/PM and wegners |
|
|
HCQ monitering and SE |
Test visual fields and acuity at baseline then at 5yrs then annually. Cummulative effect. Bulls eye maculopathy. RARE |
|
|
Pyoderma gangrenosum - grows by 1cm/d or doubles in size over 1/12 |
Painful, rapidly pregressive, purulent ulcer Underminded edges, post pathergy. Dx: biopsy, exclude Ddx Mx: moist dressings, minimise trauma TOP steroids/tacrolimus, dapsone (anti-neutrophilic effect), severe > po pred/cyclosporine/infliximab |
|
|
Pyoderma gangrenosum associations and Ddx
|
IBD Arthropathies Haematological malignancy Ddx: infection (fungal, mycobacterium), skin ca, lymphoma, vasculitis (ANA, RF, ANCA), venous HTN, arterial insufficiency, hypercoagulable states. |
|
|
Rheum |
http://www.rheumtutor.com/sjogrens-syndrome/ |
|
|
SLE
|
Serositis Oral ulcers Arthralgia Photosensitivity Bone dysfunction: anaemia, leukopaenia, thrombocytopaenia, haemolytics anaemia Renal ANA Immunological: dsDNA, anti Sm, low C3/C4 Nephritis Malar Discoid rash |
|
|
SLE Mx - 90% 10yr survival |
Photosensitivity: sun protection Rash: HCQ (less nephritis, improves mortality) Arthralgia: rest, NASIDs, HCQ, MTX Raynauds: warm, CCB CNS, pericarditis, pleurisy, severe haemolytic anaemia or low plts > steroids Clots and APLS: warfarin INR 2.5-3 (no clots, aspirin) Proliferation GN: steroids + MMP (or CYC) OP: ca + vit D and bisphosphonates Others: rituximab, auto SCT Pregnancy: LMWH and aspirin + HCQ Contraception: progesterone only High CVD and malignancy |
|
|
Gout meds and CI
|
Colchicine: CI in renal or hepatic impairment if used with strong inhibitors of CYP3A4 or P‐gp inhibitors. eg clarithromycin eg eGRF - 250mcg/d Moniter FBE at 1 and 6/12 and CK 300 mg allopurinol and 40 mg febuxostat appear similarly effective. Moniter Ur monthly then 6/12 once at target. nb feboxustat/allopurinol increase 6MP/AZA levels. |

