![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
Lesson 1 Objective
|
Describe the pathophysiologic changes that occur in HF. |
|
|
Purpose of the Cardiovascular System
|
Oxygen Delivery: distributes oxygen-rich blood to cells in different parts of the body Waste Removal: transport of by-products of cellular metabolism including carbon dioxide and lactic acid Synthesis and Regulation of Hormones: The heart produces several hormones, including atrial and B-type natriuretic peptide |
|
|
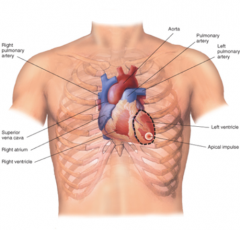
Heart Anatomical Position
|
-The heart is slightly to the left center of the chest -2/3 to the left of the midline and 1/3 to the right of the midline -Size of a mans fist -Lies behind the sternum between the points of attachment of the 2nd and 6th ribs -The apex is the pointed end and is the area of the point maximal impulse -The base is located superiorly and medially. It forms the upper borders of the heart and lies below the second rib |
|
|
Heart Anatomical Position
|
|
|
|
Heart Wall
|
|
|
|
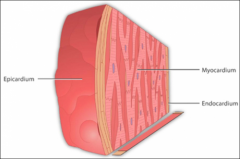
The wall of the heart has three distinct layers of tissue.
|
1. Epicardium: thin, fibrous external surface where the coronary arteries lie 2. Myocardium: thick, middle layer with involuntary cardiac muscle cells that contract to propel blood 3. Endocardium: innermost layer, forms the smooth lining of the heart's chambers and also helps form the heart's valves |
|
|
Cardiac Muscle
|

|
|
|
Cardiac Muscle
|
Green: purkinje fibers
Orange: capillaries Pink: muscle fibers Cardiac muscle: striated, single nucleus branched |
|
|
Pericardium
|
|
|
|
Pericardium
|
Thin membranous, fibroserous sacSurrounds and protects heartConfines and stabilizes position of heart
|
|
|
Pericardial Space
|
Located between pericardium and epicardiumContains pericardial fluid that acts as lubricant
|
|
|
Lymphatic System
|
|
|
|
Lymphatic System
|
|
|
|
Lymphatic System
|
Most fluid is absorbed by tissue cellsExcess drains into lymphatic capillaries and is eventually returned to the cardiovascular circulation
|
|
|
Cardiac Output (CO)
|
|
|
|
Cardiac Output (CO) |
CO is the volume of blood pumped by the ventricle per minute* CO = stroke volume X heart rate
* Cardiac index (CI) represents CO that has been adjusted to a person’s size or body surface area (BSA). Dividing CO by BSA will provide the CI. * Stroke volume (SV): is the volume of blood pumped from the ventricle with each beat.Calculated by subtracting end-systolic volume (ESV) from end-diastolic volume (EDV) * Stroke volume can be measured by echocardiogram |
|
|
Preload
|
|
|
|
Preload
|
The stretching of the cardiac myocytes prior to contraction.Preload is the basis of the Frank-Starling Law* Preload is increased in a failing heart due to volume overload
* Preload is decreased in the presence of hypovolemia |
|
|
Frank-Starling Law
|
Increased end-diastolic fiber (sarcomere) length, volume, and pressure (increased preload) yields increased cardiac outputThis is a physiologic mechanism to allow for the CO to be responsive to increased activityHowever, excessive preload (as found in HF) exhausts the Frank-Starling mechanism, such that further increase in preload no longer increases cardiac output.
|
|
|
Frank-Starling Law
|
|
|
|
Afterload
|
|
|
|
Afterload
|
The amount of resistance the ventricle has to overcome in order to eject blood * Reflective of aortic pressure for left ventricle and pulmonary artery pressure for the right ventriclePressure in the ventricles must be greater than systemic and pulmonary pressure to open aortic and pulmonic valvesAs arterial pressure increases; afterload increasesAs afterload increases; cardiac output decreases |
|
|
Vascular Resistance
|
|
|
|
Vascular Resistance
|
The resistance to blood flow that must be overcome to push blood from the heart through the circulatory systemSystemic vascular resistance (SVR) is the resistance the left ventricle must overcome to pump blood through the systemic, or peripheral, circulationPulmonary vascular resistance (PVR) is the resistance the right ventricle must overcome to pump blood through the vasculature of the lungs
|
|
|
Heart Failure (HF) Definition
|
* HF is a complex clinical syndrome which can result from any structural or functional cardiac disorder that impairs ability of the ventricle to fill with or eject blood
* Cardinal symptoms are fatigue and dyspnea, and clinical signs are fluid retention and exercise intolerance * HF is a progressive clinical syndrome that involves the interaction of multiple systems in the body Back |
|
|
Causes of HF
|
1. Coronary artery disease/myocardial infarction
2. Hypertension 3. Valvular disease 4. Genetic (e.g. Duchenne muscular dystrophy, certain hypertrophic cardiomyopathies) 5. Congenital abnormalities (e.g tricuspid atresia, septal defects) 6. Peripartum cardiomyopathy 7. Infiltrative cardiomyopathy (e.g amyloidosis, sarcoidosis, hemochromatosis) 8. Infections and inflammatory processes(e.g viral myocarditis, Chagas disease) 9. Metabolic disorders (e.g. hyperthyroidism, diabetes mellitus) 10. Toxins (alcohol, chemotherapy, radiation therapy, illicit drugs) 11. Incessant arrhythmias |
|
|
The Autonomic Nervous System
|
|
|
|
The Autonomic Nervous System
|
Short term control of blood pressure and heart rate The Autonomic Nervous System * Stress Response * ParasympatheticRest and Digest
Antagonistic-most organs receive impulses from both divisions |
|
|
Renin-Angiotensin Aldosterone
|
|
|
|
Renin-Angiotensin Aldosterone
|
Long term control of blood pressure and volume
|
|
|
Sympathetic Stimulation
|
|
|
|
HF Pathophysiology |
|
|
|
Neurohormones in HF
|
Atrial natriuretic peptide (ANP). Synthesized in atrial myocytesB-Type natriuretic peptide (BNP). Synthesized in ventricular myocytes* intrinsic diuretic; promotes natriuresis in fluid volume overload
* BNP secreted by ventricles secondary to wall stress/stretch, indicating high pressures. BNP is therefore a biomarker of cardiac pressure overload:Response to natriuretic peptides is attenuated in HF * Elevated BNP is a significant predictor of mortality; corresponds proportionately with worsened HF/fluid retention * May be higher secondary to renal failure, in women and older individuals; and lower in the presence of obesity |
|
|
Opposition of Neurohormonal Forces in HF
|
|
|
|
Physiology of Endogenous hBNP
|
|
|
|
Neurohormonal Activation
|
|
|
|
Vasopressin (Anti-diuretic Hormone) |
Released in response to arterial underfilling/reduced volume via high pressure baroreceptorsRegulates retention of water by stimulating renal tubular reabsorptionCauses congestion and hyponatremia
|
|
|
Endothelin (ET)
|
Vasoconstrictor peptide expressed in the myocardium stimulated by hypoxia, ischemia, neurohormonesIncreased levels contribute to progression of left ventricular dysfunction and secondary pulmonary hypertension
|
|
|
Dysregulation of the Immune System
|
HF causes immune activation of pro-inflammatory cytokines:* Tumor Necrosis Factor (TNF-α), Interleukin (IL-1, IL-6)
* These are over-expressed in the systemic circulation and myocardium. Sustained over-expression contributes to central and peripheral manifestations * Effects of pro-inflammatory cytokines on left ventricular function:Exert negative inotropic effect * Induce abnormalities in cardiac metabolism * Promote myocardial remodeling * Cardiomyocyte hypertrophy * Necrosis and Apoptosis (programmed cell death) * Endothelial dysfunction |
|
|
Types of HF
|
|
|
|
Diastolic Dysfunction or HF with Preserved Ejection Fraction (HFpEF)
|
HF symptoms with EF > 50%Caused by hypertrophic CM, HTN, Ischemia, AgeImpairment of left ventricular myocardial relaxation and diastolic ventricular filling; increased left ventricular wall stiffness; reduced left ventricular compliance
|
|
|
Systolic Dysfunction or HF with Reduced Ejection Fraction (HFrEF)
|
Decreased contractility EF < 40%CAD, Valve disease, Ischemic and Idiopathic CMPDecreased stroke volumeImpaired contraction with forward or backward failure
|
|
|
Differentiating Between the Definitions of HF
|
Decompensated Advanced Reduced Ejection Fraction Preserved Ejection Fraction |
|
|
Decompensated
|
Decompensated HF exists when the LV is unable to maintain cardiac output to meet the demands of the body and worsening symptoms emerge
|
|
|
Advanced
|
Advanced HF exists when symptoms and NYHA class are refractory to medical management
|
|
|
Reduced Ejection Fraction
|
HF with reduced ejection fraction exists when there is a reduced LVEF with HF symptoms.The LV is commonly dilated
|
|
|
Preserved Ejection Fraction
|
HF with preserved ejection fraction exists when patient present with symptoms of heart failure but the LVEF is normal.
|
|
|
Normal Cardiac Pressures
|
|
|
|
Central venous pressure (CVP) 0-5 mm Hg
|
Pressure of blood in the vena cava, near the right atriumReflects the amount of blood returning to the heartGood approximation of right atrial pressure
|
|
|
Right ventricular pressurevc
|
Systolic – 15-30 mm HgDiastolic – 0-5 mm Hg
|
|
|
Pulmonary artery pressure
|
Systolic – 15-30 mm HgDiastolic – 5-10 mm Hg
|
|
|
Pulmonary capillary wedge pressure (PCWP) 6-12 mm Hg
|
Indirect pressure of left atrial pressurePulmonary edema reflective of PCWP >25 mm Hg
|
|
|
Left ventricular systemic pressure (systolic)
|
100-140 mm Hg
|
|
|
Pulmonary vascular resistence (PVR)
|
(PAP-PCWP)* 80 } / (CO) =150-250 dynessec/cm^5PAP- PCWP/ CO= PVR in wood unitsAn increase in PVR can result in RV failureAbnormally high PVR can be a contraindication to cardiac transplantation as it could cause RV dysfunction in the transplanted heart
|
|
|
Systemic vascular resistance (SVR)
|
SVR = (MAP - CVP) x 80 / CONormal SVR range is 800 - 1200 dyn·s·cm−5
|
|
|
Intra-cardiac Pressures Guide Diagnosis and Treatment of HF
|
Compensatory mechanisms increase blood flow in addition to cardiac filling pressures to maintain pumping function and supply adequate blood flowDamaged myocardium stretches out of shape causing increased filling pressures
|
|
|
Fluid Imbalance in HF
|
|
|
|
Fluid Imbalance in HF
|
Blood plasma and the interstitial fluid exchange readily through the thin walls of the capillariesThe primary forces that govern this exchange are:* Outward hydrostatic pressure
* Inward oncotic pressure (osmosis) |
|
|
Fluid Imbalance in HF
|
When the heart’s function is compromised, venous hydrostatic pressure rises. The increased venous pressure is transmitted back to the capillaries.* Sodium and water retention result in increased capillary hydrostatic pressure and decreased capillary oncotic pressure
* In the setting of HF, net flow of fluid goes into the interstitial space, resulting in excess fluid accumulation, or edema * Volume overload results from inappropriate renal sodium and water retention (decreased sodium and water excretion) in the setting of already normal or increased extra cellular fluid volume. |
|
|
More on Fluid Imbalance…
|
Baroreceptor sensing of arterial under filling can occur as result of a decrease in cardiac output, even though blood volume is not decreasedNeurohormonal mechanisms are activated and cause renal sodium and water retentionEstimated 15% of total blood volume resides in arterial circulation; total blood volume increased primarily by expansion of blood volume in venous circulation, which then produces peripheral edema and ascites
|
|
|
Perils of Elevated Pulmonary Vascular Resistance (PVR) |
In patients with end stage HF, elevated PVR is a possible contraindication to cardiac transplantationElevated PVR causes RV dysfunction or failure and death in heart transplant recipients especially in the first month after transplant
|
|
|
Myocardial Remodeling
|
Alteration in the structure (dimensions, mass, shape) of the heart muscle in response to the hemodynamic changes and/or cardiac injury in association with neurohormonal activation A remodeled heart is less elliptical and more spherical Left ventricular dilatation Left ventricular hypertrophy LV remodeling may occur with a process that can create volume overload such as: * Aortic stenosis |
|
|
Cardiorenal Syndrome
|
Cardiorenal syndrome occurs when reduction in cardiac output results in disproportionate reduction in renal perfusion Leads to diminished glomerular filtration rate (GFR) and increased serum creatinine levels Worsening renal function:* Change in serum creatinine >0.3 mg/dL or >25% over baseline (normal range: adult male: 0.8 to 1.4 mg/dL; adult female: 0.6 – 1.4 mg/dL) |
|
|
Cardiorenal Syndrome
|
Cardiorenal Syndrome is a complex interaction between the heart and kidneys resulting in bidirectional injury and dysfunction •There are 5 subcategories ◦ADHF leading to acute renal failure (ARF) ◦Chronic HF leading to chronic kidney disease (CKD) ◦ARF leading to cardiac event ◦CKD leading to worsening CV disease ◦Acute illness (i.e. sepsis) leading to simultaneous heart and kidney failure |
|
|
Pathophysiology of Cardiorenal Syndrome
|
|
|
|
Hyponatremia
|
Hyponatremia defined as serum sodium concentration <136 mmol/L •Mild hyponatremia is seen in approximately 25% of patients with acute HF •Hyponatremia poses significantly greater risk of death after discharge •Reduction in cardiac output triggers hyponatremia |
|
|
Hyponatremia as a Prognostic Tool
|
Hyponatremia is one of the strongest predictors for poor outcomes in HF patients •Hyponatremia may be caused by multiple factors: ◦RAAS: Aldosterone causes sodium and water retention. ◦Antidiuretic Hormone, Vasopressin ◦Impaired renal function leads to a decreased ability of the kidneys to excrete sodium and water. •Efforts should be made to limit nephrotoxic medications and therapies such as: ◦Dye loads ◦Non-steroidal anti-inflammatory drugs (NSAIDs) ◦Antibiotics |
|
|
Diuretic Resistance
|
Diuretic Resistance is the persistence of congestion despite diuretic therapy ◦May result from renal under-perfusion ◦Distal tubules develop hypertrophy ◦There is enhanced sodium reuptake downstream from loop diuretic site of action ◦Oral absorption of loop diuretics is impaired in the setting of gut hypoperfusion and edema •Treatments ◦Restricting sodium intake◦Change timing of diurectic dose ◦Use of combination diuretic therapies. ◦Ultrafiltration and hemodialysis |
|
|
1. This is the resistance against which the ventricle must generate pressure in order to eject blood out of the heart during systole: Choose one: Preload End-diastolic volume Afterload Pulmonary vascular resistance |
Afterload
|
|
|
2. Which of the following BNP concentrations is consistent with a diagnosis of severe or acute decompensated heart failure (ADHF)? Choose one: 5 pg/mL 76 pg/mL 269 pg/mL 4,000 pg/mL |
4,000 pg/mL
|
|
|
3. Which statement is false regarding HFpEF? Choose one: Impairment of left ventricular relaxation Increased left ventricular wall stiffness; reduced compliance Impaired diastolic ventricular filling Not as common as HFrEF |
Not as common as HFrEF
|
|
|
4. Pathologic remodeling occurs with: Choose one: Pressure overload (eg, aortic stenosis, hypertension) Volume overload (eg, valvular regurgitation) Following cardiac injury (eg, MI, myocarditis, or idiopathic dilated cardiomyopathy) All of the above |
All of the above
|

