![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is the most common secondary malignant neoplasm inside the radiation field for patients with retinoblastoma?
A. Squamous cell carcinoma B. Non-Hodgkin lymphoma C. Fibrosarcoma D. Osteosarcoma |
Correct answer is D. RATIONALE: It is important to know that common secondary malignant neoplasms inside the radiation field for patients with retinoblastoma are osteosarcoma, fibrosarcoma, or spindle cell sarcoma, with osteosarcoma being the most common.
|
|
|
|
Which of the following eye tumors should be diagnosed clinically without a biopsy?
A. Retinoblastoma B. Orbital rhabdomyosarcoma C. Conjunctival lymphoma D. Pseudolymphoma |
Correct answer is A. RATIONALE: A biopsy of retinoblastoma can result in vitreous seeding.
|
|
|
|
Which of the following factors correctly matches the hereditary and sporadic characteristics associated with patients who have retinoblastoma?
Hereditary Sporadic A. Age at occurrence Older Younger B. Risk of secondary malignancies Lower Higher C. Bilateral disease Less common More common D. Incidence Lower Higher |
Correct answer is D.
Reference: Halperin E, Constine L, Tarbell N, Kun L. (eds). Pediatric Radiation Oncology. 4th edition. 2004; Lippincott, Williams & Wilkins. |
|
|
|
Which of the following statements about trilateral retinoblastoma is FALSE?
A. It is associated with an intracranial neuroblastic tumor. B. It has a favorable prognosis with approximately 80% overall survival. C. It has a higher incidence in patients with germline Rb mutations. D. It requires heightened surveillance with MRI until the age of 5 years. |
Correct answer is B.
References: Paulino AC. Trilateral retinoblastoma: is the location of the intracranial tumor important? Cancer. 1999;86(1):135-41. Kivelä T. Trilateral retinoblastoma: a meta-analysis of hereditary retinoblastoma associated with primary ectopic intracranial retinoblastoma. Journal of Clinical Oncology. 1999;1 (6):1829-37. |
|
|
|
What is the cumulative incidence of secondary cancers in patients who receive EBRT for hereditary retinoblastoma?
A. 00% to 5% B. 10% to 15% C. 35% to 40% D. 70% to 75% |
Correct answer is C. RATIONALE: Patients with hereditary retinoblastoma who received external-beam radiation therapy (EBRT) have a 35% cumulative incidence of secondary cancers. A child with unilateral retinoblastoma who presents with advanced intraocular disease and undergoes enucleation has a cure rate of >95%.
REFERENCE: Chintagumpala, et al. The Oncologist. October 2007;12(10):1237-1246. |
|
|
|
Which of the following characteristics is associated with a diagnosis of retinoblastoma?
A. Eighty percent of children are diagnosed in the first year of life. B. Approximately 80% of children with bilateral disease have a family history of the disease. C. Children who present with bilateral disease are usually 2 years older than those who present with unilateral involvement. D. It is rare in children older than 6 years of age. |
Correct answer is D. RATIONALE: Eighty percent of children with retinoblastoma are diagnosed before 3 years of age. There is a family history of the disease in approximately 20% of children diagnosed with bilateral retinoblastoma. Patients with bilateral disease usually present at a younger age (14–16 months) than patients with unilateral disease (29–30 months). The diagnosis of retinoblastoma in children 6 years or older is extremely rare.
REFERENCE: Chintagumpala, et al. The Oncologist. October 2007;12(10):1237-1246. |
|
|
|
Which of the following treatments is most appropriately performed first for a 4-year-old patient who has an International Classification Group D (Reese-Ellsworth Group 5) unilateral retinoblastoma?
A. Enucleation B. Exenteration C. Radiation therapy D. Chemotherapy |
Correct answer is A. RATIONALE: International Classification Group D and Reese-Ellsworth Group 5 include very large tumors with vitreous seeding. Typically, there is a low probability of vision salvage; therefore, enucleation is recommended.
|
Buatti disagrees with this answer. Although chemoreduction and focal therapy has a low probability of preserving vision in this population, it should be attempted prior to enucleation.
|
|
|
Which of the following factors increases the risk for CNS dissemination in a patient with
retinoblastoma? A. Extension into the orbital fat B. Invasion of >50% of the choroid C. Presence of multiple intraocular tumors D. Involvement of the optic nerve beyond the lamina cribrosa |
Correct answer is D. RATIONALE: Involvement of the optic nerve beyond the lamina cribrosa is a known risk factor for CSF spread because of the access of retinoblastoma cells to the subarachnoid space (the optic nerve is surrounded by meninges).
REFERENCE: Halperin EC, Kirkpatrick JP. Retinoblastoma. Pediatric Radiation Oncology. 4th edition. Chapter 5. Philadelphia: Lippincott Williams & Wilkins Publishers. pp 135-176. |
|
|
|
Approximately what percent of patients with hereditary retinoblastoma develop secondary malignancies within 50 years of follow-up?
A. 15% B. 30% C. 50% D. 65% |
Correct answer is C. RATIONALE: The incidence of secondary malignant neoplasm (SMN) in patients with hereditary retinoblastoma is very high (reported to be 51% in 50 years in one large study).
REFERENCE: Wong FL, et al. Cancer incidence after retinoblastoma. Radiation dose and sarcoma risk. JAMA. Oct 15, 1997;278(15):1262-7. |
|
|
|
What is the most common eye tumor in infants?
|
Metastatic leukemia (1000 cases/yr). Retinoblastoma is the most common primary tumor with 250-300 new cases in the US each year.
|
|
|
|
To what other malignancy are retinoblastoma patients particularly prone?
|
Osteosarcoma (44% of secondary malignancies)
|
|
|
|
From what cell does retinoblastoma originate?
|
Neuroepithelial cells (from the nucleated photoreceptor layer of the inner retina)
|
|
|
|
Which cell cycle checkpoint does Rb1 affect?
|
G1/S
|
|
|
|
What are the 3 most common ocular tumors? (all age groups)
|
Metastatic carcinoma
Melanoma Retinoblastoma |
|
|
|
What percentage of multifocal retinoblastoma is inherited?
|
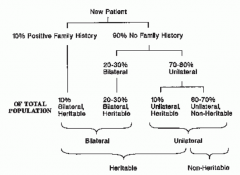
40% are considered heritable with 60% from new germline mutations
|
|
|
|
What percentage of retinoblastomas are bilateral or multifocal?
|
20-30% multifocal/bilateral
70-80% unilateral NB: Bilateral tumors are usually multifocal. |
|
|
|
In what age range is retinoblastoma most commonly found?
|
95% occur before the age of 5
Familial: 1 yo (mean 4.7 mo) Sporadic: 2 yo (mean 22 mo) |
|
|
|
Where is the RB tumor suppressor gene located?
|
Chromosome 13
|
|
|
|
Describe the two hit hypothesis for retinoblastoma
|
1st hit: Germline mutation (hereditary form)
2nd hit: Somatic mutation |
|
|
|
What pathologic features are associated with retinoblastoma?
|
Flexner-Wintersteiner rosettes
Also small round blue cells, calcium and necrosis |
|
|
|
Name five patterns of spread for retinoblastoma
|
Local extension
Invasion of the optic nerve --> brain CSF to the leptomeninges/subarachnoid Hematogenous mets Lymphatic spread via the conjunctiva, ciliary body or iris |
|
|
|
What are the most common sites of hematogenous spread for retinoblastoma?
|
Bone, liver, spleen
|
|
|
|
What percentage of retinoblastoma patients present with distant mets?
|
10-15%
|
|
|
|
What is trilateral retinoblastoma? How common is it?
|
Bilateral retinoblastoma with an intracranial PNET (pineal or suprasellar)
3-9% of hereditary retinoblastomas NB: Prognosis is extremely poor. |
|
|
|
What percentage of retinoblastomas are bilateral at presentation?
|
10-15%
|
|
|
|
Describe an ophthalmic exam for retinoblastoma
|
Awake: Visual acuity, pupillary examination, extraocular movements, slit lamp exam, indirect ophthalmoscopy,
EUA: Portable slit-lap exam, fundal photography and indirect ophthalmoscopy |
|
|
|
Describe the work-up for retinoblastoma
|
Complete H&P
Ophthalmic exam Ocular ultrasound MRI Consider systemic staging with CSF cytology, bone marrow cytology, and spinal axis MRI if extraocular Consider genetic counseling/testing NB: Try to minimize ionizing scans due to increased risk of secondary malignancy. Do NOT biopsy due to fear of seeding. |
|
|
|
What should your ophthalmologist note on exam?
|
Unilateral or bilateral nature of the lesions
Number of tumors Location in the retina (posterior pole, anterior retina), and anatomica relations with optic disc and macula Tumor size (diameter, thickness) Subretinal fluid and tumor seeds Vitreous seeding (localized vs diffuse) |
|
|
|
What is the Reese-Ellsworth system (in general)?
|
Used to the most commonly used staging system for intraocular retinoblastoma. It predicts vision preservation after EBRT; it is NOT a good predictor of survival.
|
|
|
|
What is the International Classification System for Intraocular Retinoblastoma (in general)?
|
Currently supported staging system for retinoblastoma.
Developed for use in COG protocols Predicts rate of response to chemoreduction therapy |
|
|
|
What are the general treatment options for retinoblastoma?
|
Surgery: Enucleation, exenteration
Radiation: EBRT, eye plaque brachytherapy Local Therapies: cryotherapy, photocoagulation, hyperthermia Systemic: Chemotherapy |
|
|
|
ICIR Group A
|
"Small intraretinal tumors away from the foveola and disc"
All tumors <=3 mm in height, confined to retina, and >= 3 mm (2DD) from fovea and >= 1.5 mm (1DD) from optic nerve |
|
|
|
ICIR Group B
|
"All remaining discrete tumors confined to the retina"
All other tumors confined to the retina that are not in Group A Tumor-associated subretinal fluid less than 3 mm from the tumor with no subretinal seeding |
|
|
|
ICIR Group C
|
"Discrete local disease with minimal subretinal or vitreous seeding"
Localized vitreous seeding (C1) Subretinal seeding <= 3 mm from tumor margin (C2) Both (C3) |
|
|
|
ICIR Group D
|
"Diffuse disease with significant vitreous or subretinal seeding"
Diffuse vitreous seeding (D1) Diffuse subretinal seeding >3 mm from tumor (D2) Both (D3) Subretinal fluid (no seeding) >3mm from tumor margin |
|
|
|
ICIR Group E
|
Any of the below factors:
Tumor touching the lens Tumor involving the ciliary body or anterior segment Diffuse infiltrating retinoblastoma Neovascular glaucoma Vitreous hemorrhage Orbital cellulitis-like presentation Phthisis bulbi Extraocular disease on imaging Involvement of optic nerve |
|
|
|
How does retinoblastoma present?
|
Leukocoria, strabismus, painful glaucoma (US)
Proptosis, orbital mass, mets (developing countries) |
|
|
|
What is the vision preservation rate for ICIR Group B patients?
|
Up to 93%, using chemoreduction and local therapy
|
|
|
|
What is sub-tenon chemotherapy?
|
Injection of chemotherapeutic agents (usually carboplatin) into the eye through the capsule of Tenon
Performed under anesthesia |
|
|
|
What is the cumulative risk of secondary malignancy in Rb patients who had radiation? No radiation?
|
Pick your paper:
Lin review (30 year risk): 35% with radiation vs 6% without radiation JAMA 1997 (50 year risk): 51% overall for hereditary Rb, 5% overall for non-hereditary Green book: With RT (familial cases) - 4% at 10 yrs, 18% at 35 years, 50% at 50 yrs No RT (familial cases)- 15-35% at 50 yrs |
|
|
|
Describe the mechanism of normal Rb protein
|
Binds the transcription factor E2F, which stops transcription of E2F target genes, which are responsible for cell cycle progression
Also binds to histone deacetylase (HDAC), which silences transcription In short: Rb is a tumor suppressor and stops cell cycle progression |
|
|
|
What other genetic aberrations can be found in retinoblastoma?
|
n-Myc amplification (10%)
Upregulation of MDMX (65% Upregulation of MDM2 (10%) |
|
|
|
Treatment for ICIR Group A
|
Local therapy only (cryotherapy, hyperthermia, photocoagulation or brachytherapy)
|
|
|
|
Describe the general treatment paradigm for unilateral, intraocular retinoblastoma
|
Goal of vision preservation and cure
Local therapy alone vs. Chemoreduction --> Local therapy |
|
|
|
Treatment for ICIR Group B
|
Chemoreduction with vincristine and carboplatin (2 agent chemo) x 6 cycles --> focal therapy with 2-6 cycles
Repeat EUA after cycles 2, 4 and 6 |
|
|
|
What is photocoagulation?
|
A laser is used to obliterate the retinal blood vessels feeding a tumor
Can be used for focal therapy in Group A/B tumors or for recurrence. Tumors should be posteriorly located away from the optic disc and macula. |
|
|
|
What is the typical dose for eye plaque brachytherapy to a retinoblastoma?
|
40 Gy to the tumor apex
A dose reduction to 20-30 Gy may be considered after chemotherapy. |
|
|
|
Treatment for ICIR Group C
|
Chemoreduction with vincristine, high dose carboplatin, and etoposide (three agent chemo) --> focal therapy
Reassess after every cycle |
|
|
|
When is cryotherapy appropriate for retinoblastoma?
|
Small, intraocular tumors located anterior to the equator
|
|
|
|
Treatment for ICIR Group D
|
Chemoreduction with vincristine, high dose carboplatin, and etoposide (three agent chemo) --> focal therapy
OR EBRT |
|
|
|
Treatment for ICIR Group E
|
Enucleation followed by prophylactic three agent chemotherapy
|
|
|
|
Treatment for bilateral retinoblastoma
|
Individualize treatment for each eye
|
|
|
|
When is EBRT used in retinoblastoma?
|
- Persistent or progressive disease with chemo
- Extraocular disease - Involvement of the macula - Diffuse vitreous seeding - Diffuse subretinal implants NB: EBRT is only used upfront if vision can be preserved. |
|
|
|
What are common doses for retinoblastoma EBRT?
|
Buatti: 36-45 Gy. Don't treat lower unless on trial.
36-40 Gy (Green book) 42-45 Gy (Blue book) 40-45 Gy with lower doses if chemotherapy is given first. Ex: 26 Gy in a consolidation setting following chemo and focal therapy. (Halperin) NB: All delivered using 4-6 MV photons |
|
|
|
Treatment for extraocular retinoblastoma
|
Look for a protocol
Options: Orbital EBRT with chemo, high dose chemo with stem cell rescue, intrathecal chemotherapy for CNS or meningeal disease, |
|
|
|
What is the disease-free survival for intraocular and extraocular retinoblastoma?
|
5 yr DFS: >90% intraocular, <10% extraocular
|
|
|
|
What is the eye preservation rate in most retinoblastoma series?
|
60-90% overall
65-100% for Reese Ellsworth groups 1-3 |
|
|
|
Describe different beam arrangement options for retinoblastoma: unilateral vs bilateral
|
Unilateral: 4 anterior oblique fields (noncoplanar)
Bilateral: Opposed laterals with anterior obliques (80:20 weighting) or 3DCT/IMRT Other options: protons |
|
|
|
Describe the retinoblastoma treatment volume
|
Either the entire globe or the entire retina/vitreous with sparing of the lens
Also include 5-8 mm of the proximal optic nerve NB: Studies suggest that anterior-sparing techniques may result in slightly more failures. |
|
|
|
What is the benefit to using protons in retinoblastoma?
|
Reduced dose to the orbital bone (Lee 2005)
Reduced dose to the lens (Krengli 2005) Possibly better tumor coverage |
|
|
|
Name the OAR when treating a retinoblastoma with EBRT
|
Contralateral eye
Lacrimal gland Optic chiasm Pituitary Brain stem Teeth Upper cervical spine |
|
|
|
How would you simulate a retinoblastoma?
|
Supine
Thermoplastic face mask CT and fuse MRI |
|
|
|
What chemotherapy is used in retinoblastoma?
|
Vincristine, carboplatin +/- etoposide
|
|
|
|
What are the indications for enucleation in retinoblastoma?
|
Don't enucleate unless there's no chance for vision preservation.
Large tumors filling vitreous Tumor in anterior chamber Neovascular glaucoma |
|
|
|
During enucleation for retinoblastoma, how much optic nerve should be removed?
|
10-15 mm
|
|
|
|
Risk factors for extraocular involvement at the time of enucleation for retinoblastoma
|
Optic nerve invasion (potential access to CSF)
Uveal invasion (potential access to scleral and emissary veins) Orbital invasion (potential access to vascular and lymphatic channels outside the eye) Large volume of choroidal involvement??? |
|
|
|
When is chemoradiation indicated after enucleation for retinoblastoma?
|
Positive margin
Positive lymph node |
|
|
|
What are the indications for eye plaque brachytherapy in retinoblastoma?
|
Solitary lesion with:
- 2-16 mm base diameter - <10 mm height - Located at least 3 mm from the fovea/optic *Videtic and Suh books, Halperin |
|
|
|
Side effects of retinoblastoma EBRT
|
Skin reaction
Telangectasias Facial or temporal bone hypoplasia Cataracts Decreased tear production (lacrimal gland toxicity) Direct corneal injury Ectropion/entropion of eyelid Vitreous hemorrhage Retinopathy Hypopituitarism SECONDARY MALIGNANCY!! |
|
|
|
Describe follow-up for retinoblastoma
|
H&P:
Q3 months for 1 year Q4 months for second year Q6 months for years 3-4 Then annually If familial or bilateral: Also need biannual CT/MRI until age 7 and screening of the contralateral eye Q2-4 months for up to 7 years |
|
|
|
Side effects of eye plaque brachytherapy
|
Retinopathy
Cataract Maculopathy Glaucoma Papillopathy Risk of orbital bone hypoplasia is low |
|
|
|
What radioisotopes are used for retinoblastoma eye plaque brachytherapy?
|
Iodine-125 and Ru-106
NB: Ru-106 has a steeper dose falloff so tumors should be <5 mm deep |
|
|
|
DDx for leukocoria
|
Hyperplastic primary vitreous, retrolental fibrodysplasia, Coat disease, congential cataract, toxocariasis, toxoplasmosis
|
|
|
|
Reese Ellsworth Group I
|
Very favorable
A: Solitary tumor, less than 4 DD in size, at or behind the equator B: Multiple tumors, none greater the 4 DD, all at or behind the equator |
|
|
|
Reese Ellsworth Group II
|
Favorable
A: Solitary tumor, 4-10 DD in size, at or behind equator B: Multiple tumors, 4-10 DD, behind the equator |
|
|
|
Reese Ellsworth Group III
|
Doubtful
A: Any lesion anterior to the equator B: Solitary tumor, >10 DD, behind the equator |
|
|
|
Reese Ellsworth Group IV
|
Unfavorable
A: Multiple tumors, some larger than 10 DD B: Any lesion anterior to the ora serrata |
|
|
|
Reese Ellsworth Group V
|
Very unfavorable
A: Massive tumor involving over half the retina B: Vitreous seeding |
|

