![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
175 Cards in this Set
- Front
- Back
|
What is pulmonary ventilation?
|
Pulmonary ventilation is movement of air in lungs, more plainly breathing.
|
|
|
What happens during external respiration?
|
External respiration is movement of O2 and CO2 between lungs and blood.
|
|
|
What happens during cellular respiration?
|
Cellular respiration is the use of O2 in cellular metabolism.
|
|
|
What is Internal Respiration?
|
Internal respiration is movement of O2 and CO2 between blood and tissues.
|
|
|
Describe the flow of respiratory gasses.
|
O2 from lungs to blood, then to tissues. CO2 from tissues to blood, then to lungs.
|
|
|
What is the respiratory zone and what is it composed of?
|
The respiratory zone is the actual site of gas exchange, it’s composed of repiratory bronchioles, alveolar ducts, and alveoli.
|
|
|
What is the conducting zone and what is it composed of?
|
The conducting zone includes all of the other respiratory passageways and cleans, humidifies, and warms incoming air.
|
|
|
What are the functions of the nose and paranasal sinuses?
|
The clean, warm and moisten air, also provide sense of smell, and act as resonating chamber that amplifies voice.
|
|
|
What is the structure of the nose?
|
The nose is composed of the nasal septum, the olfactory mucosa and the nasal conchae.
|
|
|
What is the nasal septum and what is it composed of?
|
The nasal septum separates the two chambers of the nose, it's composed of septal cartilage, the vomer bone, and part of the ethmoid bone.
|
|
|
What function does the olfactory mucosa serve?
|
The olfactory mucosa contains smell receptors.
|
|
|
Besides the olfactory mucosa, what other kind of mucus lines the nose, and what is its purpose?
|
The respiratory mucosa contains goblet cellsthat secrete the antibacterial enzyme lysozyme.
|
|
|
What is the purpose of the nasal conchae?
|
The nasal conchae assists in cleansing, warming, and humidifying air.
|
|
|
What unique function does the inferior nasal concha serve?
|
The inferior nasal concha sweels with blood and restricts airflow, airflow shifts between right and left nostrils once or twice per hour.
|
|
|
What else is the pharynx known as?
|
The throat.
|
|
|
From superior to inferior, what are the three regions of the pharynx?
|
The nasopharynx, oropharynx, and the laryngopharynx.
|
|
|
What immune system organ is part of the nasopharynx, and what is it made of?
|
The pharyngeal tonsils, also known as the adenoids, which is composed of a cluster of lymph nodes.
|
|
|
What is the larynx commonly known as?
|
The larynx is also known as the voice box.
|
|
|
Describe the path through the pharynx.
|
The nasal cavity and the mouth connect to the esophagus and the larynx via the pharynx.
|
|
|
What are the three functions of the larynx?
|
The larynx provides an patent airway, acts as a switching mechanism to route food and air, and houses vocal chords.
|
|
|
What is the thyroid cartilage, and what type of cartilage is it composed of?
|
The thyroid cartilage is composed of hyaline cargtilage, and it's also known as the Adam's apple.
|
|
|
What is the function of the epiglottis, what type of cartilage is it composed of, and what is the epiglottis' nickname?
|
The epiglottis guards the entrance of the glottis, the opening between the vocal folds, it's composed of elastic cartilage and covered with mucus membrane, and it's nicknamed "guardian of airways".
|
|
|
The larynx is an arrangement of 9 cartilages connected by membranes and ligaments, name three of the cartilages.
|
The thyroid cartilage, epiglottis, and hyoid.
|
|
|
What is the hyoid bone, and what is unique about it?
|
The hyoid bone braces the tounge and laryngeal together so can produce more sounds, and it's the only bone in the body that's not attached to another bone.
|
|
|
What connects to the trachea, and where does it lead?
|
The trachea descends from the larynx, and ends by dividing into the two main bronchi.
|
|
|
What is the trachea commonly known as?
|
The windpipe.
|
|
|
What does trachea mean?
|
Trachea means rough.
|
|
|
Describe the structure of the trachea.
|
Trachea wall consists of several layers including: mucosa, submucosa, and adventitia.
|
|
|
What is an adventitia?
|
The adventitia is the outermost connective tissue layer of any organ, vessel, or structure.
|
|
|
What does the mucosa in the trachea do?
|
Contains same goblet cell-containing pseudestratified epithelium as most of respiratory tract, which continually propels mucus toward pharynx.
|
|
|
What does the submucosa do in the trachae?
|
The connective tissue layer beneath the mucosa, contains seromucous glands that produce mucus sheets within trachea.
|
|
|
What does the adventitia do in the trachea, and what is it composed of.
|
Connective tissue reinforced internally by 16-20 C-shaped rings of hyaline cartilage. Cartilage flexible but keeps trachea open for breathing.
|
|
|
Describe the path of air through the conducting zone structures starting at the trachea.
|
Primary bronchi, secondary bronchi, bronchioles, respiratory bronchioles, alveolar ducts.
|
|
|
Which bronchi lodges most aspirated objects and why?
|
The right bronchi is wider and shorter than the left, and is more likely to get objects lodged in it.
|
|
|
What other name do secondary bronchi go by?
|
The secondary bronchi also go by lobar bronchi.
|
|
|
What are bronchioles defined as?
|
Bronchioles are smaller than 1mm in diameter.
|
|
|
What are the smallest of bronchioles, about how many are there and how small are they?
|
The smallest bronchioles are the terminal bronchioles, there are about 65,000 of them, and they're about .5mm in diameter.
|
|
|
What do the terminal bronchioles feed into and what do they contain?
|
The terminal bronchioles feed into the respiratory bronchioles, and the respiratory bronchioles contain alveoli.
|
|
|
Describe the composition of alveolar ducts.
|
Alveolar duct walls are composed of smooth muscled cells and lead to terminal clusters of alveolar sacs.
|
|
|
Describe the support structure changes when passing through the bronchial tree.
|
From cartilage rings, to plates of cartilage, and then no cartilage.
|
|
|
Describe the epithelia of the bronchial tree.
|
From ciliated pseudeostratified columnar, to columnar, then to cuboidal in terminal branches.
|
|
|
By definition, where does the respiratory zone begin?
|
The respiratory zone is defined as having alveoli, and begins as the terminal bronchioles feed into respiratory bronchioles.
|
|
|
What are alveoli?
|
Thin walled air sacs where gas exchange happens.
|
|
|
Describe the difference between alveoli and alveolar sacs.
|
Alveolar sacs are like a bunch of grapes, and alveoli are like individual grapes.
|
|
|
The walls of the respiratory membrane of the alveoli are composed of primarily what?
|
A single layer of squamous epithelial cells called type I cells.
|
|
|
Describe the construction of the respiratory membrane.
|
The alveolar,capillary walls, and their fused basement membranes form the respiratory membrane.
|
|
|
Approximately how thick is the air-blood barrier that has blood flowing on one side and air on the other, and what else is this barrier referred to as?
|
Approximately .5 micrometers.
|
|
|
Scattered amid the type I squamous cells that form the major part of the alveolar walls are what, what do they secrete, and why?
|
Cuboidal type II cells secrete surfacant. Surfacant coats the gas exposed alveolar surfaces.
|
|
|
Describe the changes in smooth muscle when passing through the bronchial tree.
|
The smooth muscle increases as the passageways become smaller.
|
|
|
What is surfacant composed of, and what does it do?
|
Surfacant is composed of a mixture of phospholipids and proteins, and coats alveolar surfaces and decreases surface tension.
|
|
|
What function do the alveolar pores have?
|
The alveolar pores connect adjacent alveoli and allow air pressure to stay equalized throughout the lung if there is damage to a bronchiole.
|
|
|
What purpose do dust cells serve, what are they also known as, and how are they removed fro the body.
|
Alveolar macrophages crawl freely across the internal alveolar surfaces, about 100 million die per day, they're carried up mucocilary escalator to be swallowed or digested.
|
|
|
Describe the approximate alveolar capillary pressure.
|
MAP: 10mmHg & osmotic (oncotic) pressure = 25mmHg.
|
|
|
What is oncotic pressure?
|
Oncotic pressure in the circulatory system is a form of osmotic pressure exerted by proteins in blood plasma that normally tends to pull water into the circulatory system.
|
|
|
Which way does H2O go, in or out of alveoli?
|
Good question.
|
|
|
Describe the gross anatomy of the lungs.
|
The left side has two lobes, and the right side has three lobes.
|
|
|
Systemic venous blood that's to be oxygenated in the lungs is delivered by what, and describe the pressure and volume of this blood?
|
Delivered by the pulmonary arteries, and it has low-pressure and large volume.
|
|
|
Freshly oxygenated blood travels through what to get back to the heart?
|
Travels via the pulmonary veins.
|
|
|
What provides systemic blood to the lung tissue, and describe the route, volume and pressure of this blood?
|
Systemic blood is brought to the lung tissue by the bronchial arteries from the aorta, and this blood is small volume and high-pressure.
|
|
|
What enzyme is present in the wall of the alveoli, and what does it do?
|
Angiotensin converting enzyme (ACE) activates important blood pressure hormone.
|
|
|
What does ACE do?
|
ACE works in blood pressure regulation.
|
|
|
Describe the sympathetic and parasympathetic control of the lungs.
|
The sympathetic control dilates the air tubes, and the parasympathetic constricts the air tubes.
|
|
|
Describe the purpose of the pleural cavity and the fluid, and its composition.
|
The pleura cavity is between the pleura and is filled with pleural fluid. The pleural fluid is secreted into the pleural cavity by the pleura, and lubricates so the lungs can easily glide over the thorax wall during breathing.
|
|
|
Describe the composition of the pleurae.
|
The pleura is a doubled layer serosa, with the parietal layer covering the thoracic wall and the visceral layer covering the external lung.
|
|
|
What is pleurisy, and what usually causes it?
|
Pleurisy is inflammation of the pleura, and is often caused by pneumonia.
|
|
|
What two functions does the pleura serve?
|
The pleura compartmentalizes the organs in the thorax to prevent the spread of infection, and crates a pressure gradient.
|
|
|
What is the thorax.
|
The thorax lies between the head and the abdomen on an animals body.
|
|
|
What are respiratory pressures always described relative to?
|
Atmospheric pressure (Patm)
|
|
|
What is atmospheric pressure?
|
Patm is the pressure exerted by the air (gases) surrounding the body.
|
|
|
At sea level, what is atmospheric pressure?
|
(P atm) is 760mmHg
|
|
|
What is intrapulmonary pressure, and how does it act?
|
(P pul) Pressure in the alveoli. Pressure rises and falls but always eventually equalizes with the atmospheric pressure (P atm).
|
|
|
What is intrapleural pressure, and how does it act?
|
(P ip) is pressure in the pleural cavity. It changes but is always about 4mm Hg less than (P pul).
|
|
|
What are the three pressures acting thoracic cavity?
|
(P atm), (P ip), and (P pul)
|
|
|
How does (P ip) compare to (P atm) and (P pul), and why?
|
(P ip) is negative relative to both (P atm) & (P pul). Lungs have natural tendency to recoil due to elasticity, and the surface tension of the alveolar fluid working to draw the alveoli to their smallest possible size vs the natural elasticity of the chest wall (tends to pull thorax outward and expand lungs).
|
|
|
What is atelectasis?
|
Lung collapse happens when a bronchiole becomes plugged.
|
|
|
What is the term for the presence of air in the intrapleural space?
|
Pneumothorax.
|
|
|
What is the mantra of pulmonary ventilation?
|
Volume changes lead to pressure changes (gradients) that lead to airflow.
|
|
|
What is Boyle's law?
|
Pressure of a given quantity of gas is inversely proportional to its volume (at constant temperature).
|
|
|
What pressure differences are needed for airflow?
|
Pressure in the lungs and atmospheric pressure.
|
|
|
Describe how the diaphragm acts to change the volume of the lungs.
|
The dome shaped diaphragm contracts, moving inferiorly and flattening out, and the thoracic cavity increases.
|
|
|
Approximately how much of pulmonary airflow is due to the diaphragm?
|
2/3
|
|
|
Describe how the internal and the external intercostals act to change the volume of the lungs.
|
Contraction of the external intercostal muscles lifts the rib cage and pulls the sternum superiorly. The external intercostals aide in quiet and forced inhalation, and the internal aid in forced inhalation.
|
|
|
Approximately how much airflow is attributed to the internal and external intercostals, what do they do by stiffening, and what are they also known as?
|
1/3, stiffen thoracic cage and prevent from caving inward when diaphragm descends.
|
|
|
What accessory muscles work during deep breathing?
|
Erector spinae, sternocleidomastoids, and"pecs"
|
|
|
What other factor expands the lungs?
|
Warming of the air.
|
|
|
What is Charles' Law, and how does it affect inspiration?
|
The volume of a given quantity of gas is directly proportional to its absolute temperature. As inhaling warmed air, expands and helps inflate lungs.
|
|
|
What is the cause of normal expiration, and what kind of action is this, and what happens to muscles at this point?
|
Quiet expiration is passive and relies more on lung elasticity then muscle contraction, muscles stop contracting.
|
|
|
What nerves stimulates the diaphragm at a reduced level, and what effect does it have.
|
The phrenic nerves stimulate the diaphragm and produces a slight braking action that keeps the lungs from recoiling too suddenly
|
|
|
Forced expiration (singing, shouting, coughing, sneezing, etc.) is aided by what muscles?
|
Abdominis, internal intercostals, latissimus dorsi, transverse and oblique abdominis, pelvic muscles, rectus (abs)
|
|
|
In biology, what does rectus mean?
|
Rectus means straight muscle
|
|
|
What is the Valsalva maneuver?
|
The depression of the diaphragm raises the abdominal pressure and assists to expel pee, poop, and babies. Maneuver consists of taking a deep breathe, holding it and contracting the abdominal muscles.
|
|
|
What physical factors influence pulmonary ventilation?
|
Airway resistance, and alveolar surface tension.
|
|
|
What is the formula for airway resistance?
|
force = change in pressure/resistance
|
|
|
What is the primary way of controlling resistance of the airways.
|
The diameter of the bronchioles, just like arteries.
|
|
|
How are bronchodialation and bronchoconstriction affected?
|
Bronchodialation is affected by E and sympathetic nerves, Bronchconstriction is affected by histamine, parasympathetic nerves, cold air, and irritants.
|
|
|
How does surfacant affect the alveoli, and what cell produces it?
|
Alveoli are relatively dry but have thin film of water over epithelium, H bonding creates surface tension, surfacant disrupts H bonding (like soaps and detergents)
|
|
|
What is IRDS, and what are possible treatment options?
|
Infant Respiratory Distress Syndrome is usually seen in premature babies whose lungs don't produce enough surfacant. Positive-pressure respirators that keep alveoli open while breathing and sprayed surfacant can be used.
|
|
|
Describe pulmonary, or lung compliance.
|
Distensibility, or stretchiness of lungs vs stiff lungs. The lower the lung compliance the harder it is to breath
|
|
|
What are the four respiratory volumes?
|
Tidal volume (TV), Inspiratory reserve volume (IRV), Expiratory reserve volume (ERV), Residual volume.
|
|
|
Describe tidal volume
|
TV is the amount of inhaled or exhaled in one breath during quiet breathing.
|
|
|
Describe inspiratory reserve volume.
|
IRV is the maximum effort in excess of TV
|
|
|
Descrive expiratory reserve volume
|
ERV is the maximum effort in excess of TV
|
|
|
Describe residual volume.
|
Air that can never be exhaled.
|
|
|
Describe respiratory capacities?
|
Include inspiratory capacity, functional residual capacity, vital capacity, and total lung capacity, ALWAYS CONSIST OF 2 OR MORE LUNG VOLUMES
|
|
|
Describe dead space, and what is it usually?
|
Air inhaled that never reaches alveoli and fills the conducting zone. Usually 150ml (1ml/pound of body weight)
|
|
|
What kind of equipment is used for pulmonary function tests, and what is this test able to find?
|
Spirometer uses a hollow bell inverted over water, or an electric spirometer. Able to distinguish between obstructive pulmonary diasease (involving increased airway resistance), and restrictive disorders (involving a reduction in total lung capacity.
|
|
|
Describe alveolar ventilation, give the formula, and approx figures.
|
Takes into account the volume of air wasted in the dead space and measures the flow of fresh gases in and out of the alveoli during a particular time interval. AVR (alveolar ventricular rate) = frequency (breaths/minute) X (TV - dead space). 500ml of air, 150ml = dead air, 350ml ventilates the alveoli X respiratory rate (12breaths/minute) = 4200 ml/min = alveolar ventilation rate.
|
|
|
What are some common non-respiratory air movements
|
cough, sneeze, crying, laughing, hiccups, yawn
|
|
|
What is Dalton's law?
|
Dalton's law states that the total pressure of a gas mixture is = to the sum of partial pressure of individual gases.
|
|
|
Break down the contents of air that we inhale, not the composition of air in the alveoli.
|
Air: N2=79%, O2=21%, CO2=.04%, H2O=.46%
|
|
|
How is partial pressure formulated?
|
% of substance in atmosphere X atmospheric pressure (760mm Hg @ sea level)
|
|
|
What is the formula that describes (P B), and what are the levels @ sea level (P atm 760mm Hg).
|
(P B)= (P N2) + (P O2) + (P CO2) + (P H20)
{760 = 597 + 159 + 0.3 + 3.7} |
|
|
What is the most important partial pressure, and what is it at sea level, Camp Muir, and in the Titanic?
|
P O2 (21% x mmHg).
|
|
|
What is the mantra for partial pressure?
|
Pressure differences move gas molecules.
|
|
|
What is Henry's law?
|
Diffusion of gases into liquids at the gas-water interface, the amount of gas that dissolves in water is determined by its solubility in water and its partial pressure in the air.
|
|
|
What is the affect of Henry's law in the respiratory process?
|
The greater concentration of a gas in the gas phase, the more and faster it will go into a solution.
|
|
|
Describe the solubility of O2, CO2, and N2, in order of most to least soluble.
|
CO2, O2, N2
|
|
|
Describe the gaseous makeup found in the alveoli compared to those found in the atmosphere, and why is this so.
|
The atmosphere contains almost entirely O2 and N2, and the alveoli contains much more CO2 and water vapor, and much less O2. This reflects gas exchanges, humidification of air by conducting passages, and mixing of alveolar gas with every breath.
|
|
|
What happens to AVR when breathing depth increased?
|
A high alveolar ventilation rate brings more O2 into the alveoli, increasing alveolar P O2, and rapidly eliminates CO2 from the lungs.
|
|
|
What way do gases flow in terms of a pressure gradient?
|
Gases flow down their pressure gradients, and the rate of loading depends on the steepness of the gradient.
|
|
|
Compare CO2, O2, and N2 in terms of solubility?
|
CO2 is about 20 times as soluble as O2, and N2 is about half as soluble as O2.
|
|
|
How does the rate of solubility, and the pressure gradient of O2 and CO2 affect how the 2 gases are exchanged at the alveolar-blood barrier?
|
Pressure gradient of O2 is much greater than CO2, but because CO2 is more soluble and diffuses more rapidly, equal amounts or the 2 gases are exchanged.
|
|
|
In terms of gas exchange, what is ventilation?
|
The amount of gas reaching the alveoli
|
|
|
In terms of gas exchange, what is perfusion?
|
The blood flow in pulmonary capillaries.
|
|
|
(autoregulator) Describe ventilation-perfusion coupling when experiencing poor alveolar ventilation.
|
Poor alveolar ventilation results in low O2 and high CO2 levels in the alveoli. Consequently the pulmonary arteries constrict and the airways dilate, bringing air flow and blood flow into closer physiological match.
|
|
|
(autoregulatory) Describe ventilation-perfusion coupling when experiencing high P O2 and low CO2 in the alveoli.
|
These levels in the alveoli will cause respiratory passageways to constrict, and promote flushing of blood into the pulmonary capillaries.
|
|
|
Describe the thickness of respiratory membrane in healthy lungs.
|
Only about .5 to 1 micrometer thick, and gas exchange is usually very efficient.
|
|
|
Describe the surface area of respiratory membranes in healthy lungs.
|
The greater the surface area of the respiratory membrane, the more gas can diffuse across it in a given time period. The surface area in healthy lungs is enormous, about 90 meters squared
|
|
|
In internal respiration, how do the partial pressure and diffusion gradients act.
|
P O2 in the tissues is always lower than in the systemic arterial blood, so O2 moves quickly from the blood into the tissues until equilibrium is reached. CO2 moves quickly along its pressure gradient into the blood.
|
|
|
Compare gas exchanges between the blood and the alveoli, and between tissue cells and blood.
|
Both take place by simple diffusion driven by partial pressure gradients of O2 and CO2.
|
|
|
How much oxygen is carried in the body by plasma and hemoglobin within RBCs, and why?
|
O2 is poorly soluble in water so only about 1.5% of O2 transported is dissolved in plasma, 98.5% of O2 is carried from the lungs to the tissues by hemoglobin.
|
|
|
Describe the structure of Hemoglobin (Hb), and how many molecules of O2 can bind to a hemoglobin.
|
Hb is made of four polypeptide chains, each bound to an iron-containing heme group, and 4 molecules of O2 can bind to a hemoglobin.
|
|
|
What is the hemoglobin-oxygen combination called, and how is it written?
|
Oxyhemoglobin, written HbO2
|
|
|
What is hemoblobin that has released oxygen called, and how is it written?
|
reduced hemoglobin or deoxyhemoglobin, written HHb
|
|
|
What is the reversible equation of loading and unloading of O2?
|
HHb + O2 -->lungs-->
<--tissues<--HbO2 + H+ |
|
|
Describe what happens after the first O2 binds to iron.
|
After first O2 molecule binds to iron, the Hb molecule changes shape, as result it more readily takes up tow more O2 molecules, and uptake of fourth even more facilitated.
|
|
|
What is a hemoglobin molecule called when all four heme groups are bound to O2?
|
Fully saturated.
|
|
|
What is a hemoglobin molecule called with one, two, or three O2 molecules are bound?
|
partially saturated.
|
|
|
Describe what happens to a fully saturated Hb molecule when one O2 is removed.
|
Unloading of one O2 molecule enhances the unloading of the next and so on.
|
|
|
Describe how the affinity of Hb for oxygen and how it changes.
|
It changes with the rate of O2 saturation, so both loading and unloading are very efficient.
|
|
|
For every O2 dissolved in plasma, how many are carried by Hb?
|
70 carried by Hb for every O2 dissolved in plasma
|
|
|
Describe the major changes in the oxygen-hemoglobin the steep slope for P 02 between 10 and 50 mmHg, and plateau between 70 and 100.
|
Rapid loading and unloading of O2 to and from Hb occur at P O2 values in the steep portion of the curve (10-50mm Hg),
|
|
|
How saturated is Hb at a P O2 of 70mm Hg in tissues, and why?
|
Almost completely saturated,
|
|
|
Describe how much nearly fully saturated O2 blood reacts at a P O2 in the tissues of about 70 mm Hg.
|
Normal resting conditions: (PO2=100mm Hg) arterial blood Hb is 98% saturated, and 100 ml of systemic arterial blood contains about 20ml of O2 (this content written as 20 volume%), as arterial blood flows through systemic capillaries, about 5ml of O2 per 100ml of blood is released, yielding 75% Hb saturation, and O2 content of 15% venous blood.
|
|
|
About what percentage of Hb bound O2 is unladed to the tissues after one round, and about how much of the venous Hb blood is saturated after one round through the body.
|
Abouth 25% of Hb-bound O2 is unloaded to the tissues, and about 75% saturated Hb saturated with O2 in venous blood after one round through the body.
|
|
|
Reproduce the oxygen-dissociation curve.
|
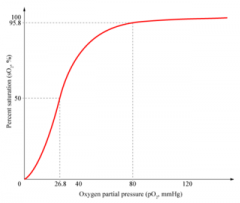
Oxygen-dissociation curve
|
|
|
What is the adaptive significance that Hb is almost completely saturated at a P O2 of 70mm Hg in the tissues, and further increases in P O2 only produce small increases in O2 binding.
|
O2 loading and and delivery to the tissues can still be adequate when P O2 of inspired air is well below its usual levels, like at higher altitudes, because most UNLOADING occurs on the steep portion of the curve, a small drop in P O2 will cause a large increase in unloading.
|
|
|
On the steep portion of the oxygen-dissociation curve, what will a small drop in P O2 do.
|
Cause a large increase in unloading.
|
|
|
What effect does an increase, and a decrease of temp, P CO2, H+ content of blood, or BPG have on the oxygen-hemoglobin dissociation curve, and why?
|
An increase of either causes the curve to move to the right, and a decrease causes the curve to move to the left. A decrease in any factor increases hemoglobin's affinity for oxygen.
|
|
|
What happens when H+ binds to HBO2, and what is the typical concentration gradient of P O2 from arterial blood to the tissue fluid.
|
It reduces the affinity of Hb for O2 and tends to make Hb release it. O2 consumption by respiring tissues keeps the P O2 of tissue relatively low, and so there's a typical concentration gradient of 95 to 40 mm Hg from arterial blood to the tissue fluid.
|
|
|
Where on the oxygen-dissociation curve can the venous reserve be found.
|
The venous reserve can be found on the plateau.
|
|
|
What is the venous reserve, and how long will it last?
|
Only 20-25% of bound O2 is unloaded in one systemic circuit, this reserve is sufficient to sustain life for 4-5minutes even in the event of respiratory arrest.
|
|
|
What other factors act on Hb saturation, and how?
|
Temp rising, P CO2, H+, and BPG will all cause O2 unloading to tissues to increase
|
|
|
What is the Bohr effect?
|
Both declining blood pH (acidosis) and increasing PCOS
|
|
|
How does cell metabolism effect O2, CO2, and H+.
|
As cells metabolize glucose and use O2, they release CO2, which increases the P CO2 and H+ levels in the capillary bed.
|
|
|
Describe the vasodialating and vasoconstricting properties of NO, and Hb, and where is NO produced, and describe how NO reacts with iron?
|
NO is a potent vasodialator produced in vascular endothelial cells, and Hb is a vasoconstrictor. Iron destroys NO.
|
|
|
If iron is destructive to NO, how is no transported by Hb?
|
Hb carries NO binded to its proteins.
|
|
|
Where are the 2 places NO binds to Hb, and describe the circumstances.
|
In the lungs at the same time the heme picks up O2, and dual NO and O2 unloading and CO2 loading at tissues (when O2 unloaded in tissues, so is NO which induces smooth muscles the blood vessels to relax.
|
|
|
List the three ways CO2 is transported in the body, and their percentages of being transported.
|
7% dissolved in plasma, 20% bound to Hb as carbinohemoglobin (HbCO2), and 70% as bicarbonate (HCO3-).
|
|
|
How is CO2 carried in plasma?
|
Simply dissolved in plasma.
|
|
|
How is CO2 chemically bound to hemoglobin, what is CO2 bound to hemoglobin called, and list the chemical reaction.
|
CO2 bound to hemoglobin as carbinohemoglobin, reaction is quick and doesn't require a catalyst, <--CO2 + Hb
-->HbCO2 |
|
|
Describe the process of bicarbonate being formed, what happens after its made, and list the chemical reaction.
|
CO2 diffuses into the RBCs, combines with water, forming carbonic acid (H2CO3), H2CO3 is unstable and quickly dissociates into H+ ions and bicarbonate ions. Once HCO3 is produced, quickly moves from RBCs to the plasma and to the lungs. CO2 +H2O <-->H2CO3<-->H+ + HCO3-
|
|
|
Describe the differences of bicarbonate being formed in plasma and in RBCs, and what happens when RBCs release bicarbonate.
|
Once generated in RBCs HCO3- moves quickly into the plasma, to counter balance anions leaving cell Cl- ions move into RBCs, this called cholride shift, bicarbonate able to be made in plasma, but more quickly produced in RBCs because catalyzed by hte enzyme carbonic anhydrase.
|
|
|
Describe cholride shift.
|
To counter bicarbonate anions leaving RBC, RBC accepts CL- via diffusion
|
|
|
How does the Bohr effect affect bicarbonate production?
|
H+ released from reaction bind to Hb, O2 release is enhanced by CO2 loading.
|
|
|
Describe the process of how bicarbonate is released in the lungs.
|
Blood moves through the pulmonary capillaries, its P CO2 declines from 45-40 mm Hg, HCO3- reenters RBCs, and Cl- moves into plasma, HCO3- binds with H+ to form carbonic acid, which is split by carbonic anhydrase to release CO2 and water, then diffuses along partial pressure gradient from blood into alveoli.
|
|
|
Approximately how saturated is Hb when arriving, and when leaving the systemic capillaries?
|
Arriving = 97% saturated, leaving = 75% saturated
|
|
|
How does H+ binding to HbO2 affect its O2 affinity?
|
Reduces affinity of Hb for O2 and tends to make Hb release it.
|
|
|
Describe the Haldane effect.
|
Rate of CO2 loading is also adjusted to varying needs of tissues, lor HbO2 allows blood to transport more CO2 (HBO2 doesn't bind CO2 as well as HHb and HHb binds more H+ than HbO2)
|
|
|
What influence does CO2 have on blood pH?
|
If H+ concentration in blood begins to rise, excess H+ is removed by combining with HCO3- to form carbonic acid, if H+ concentration drops below normal, carbonic acid dissociates, releasing H+ and lowering pH again.
|
|
|
What part of the brain sets the basic respiratory rhythm?
|
The medullary respiratory centers
|
|
|
What part of the brain is responsible for tweaking the basic respiratory pattern?
|
The pons respiratory centers.
|
|
|
What are the two hypothesis's for the genesis of the respiratory rhythm?
|
There are pacemaker neurons in the heart, or result of two sets of pacemaker neurons that inhibit each other to generate rhythm
|
|
|
Briefly list the influencing factors of breathing rate and depth.
|
pulmonary irritant reflexes, inflation reflex (Hering-Breuer), Hypothalamic (crying, laughing, anxiety), cortical (voluntary)
|
|
|
Describe the pulmonary irritant reflexes.
|
Due to smoke, dust, etc.:nerve impulses to respiratory and bronchial muscles to promote bronchioconstriction, apnea, coughing
|

