![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
|
Functions of the Respiratory System (7) |
1. Provides O2 to the blood 2. Removes CO2 from the blood 3. Regulates blood pH 4. Speech (air passes through vocal cords) 5. Microbial defense 6. Influences arterial concentration of chemical messengers 7. Traps and dissolves small blood clots (via enzymes) |
|
|
Diaphragm |
Powerful skeletal muscle - separates thoracic cavity (lungs) from abdominal cavity (digestive organs) - attached below to the abdominal cavity |
|
|
Number of lobes each lung has and why |
Right lung has 3 Left lung has 2 - bottom of the heart leans left, takes up space (cardiac notch) |
|
|
Intrapleural space |
Space between the lung and the chest wall (between visceral and parietal pleura?) - sealed cavity - also contains pleural fluid - pressure here is lower than atmospheric pressure - lung is like fist pushed into a balloon, double membrane |
|
|
Visceral Pleura |
thin membrane that encases the lungs - attached to the lungs |
|
|
Parietal Pleura |
thin membrane that surrounds the visceral pleura - attached to ribs and diaphragm - it expands when you expand your chest and your diaphragm drops |
|
|
Two major divisions of the lungs (basic anatomy) |
The Conducting Zone
The Respiratory Zone |
|
|
Parts of the Conducting zone |
Trachea (C-shaped rings of cartilage to prevent collapse) Left/Right Primary Bronchi Secondary Bronchi Tertiary Bronchi Bronchioles Terminal Bronchioles |
|
|
Parts of the Respiratory Zone |
Respiratory Bronchioles (no cartilage, no cilia) Alveolar Duct (last branch) Alveolar Sac Alveoli |
|
|
Functions of the Conducting Zone |
- conduct air through lungs - microbial defense (bronchial epithelium covered in cilia. Cilia sweeps, germs caught in mucus, swept to trachea where you cough or swallow) (smoking disrupts the coordination of the cilia and leaves you more susceptible to infection) *Air in Conducting Zone is NOT involved in gas exchange |
|
|
Functions of the Respiratory zone |
Gas exchange via the Blood-gas barrier |
|
|
Blood-Gas-Barrier |
Separates the blood in the pulmonary capillaries (that wrap around alveoli) from the air in the alveoli - air brought to one side of the barrier by ventilation - blood brought to other side of the barrier by pulmonary circulation - Type I cells and Capillaries |
|
|
Structures of the Alveolus |
Type I Cells - make up the wall, thin for quick diffusion of O2, CO2 Capillaries - on outside surface Type II Cells - secrete surfactant Macrophages - clean up debris |
|
|
Tidal Volume |
Volume of air in one breath |
|
|
Respiratory Rate |
Number of breaths per minute |
|
|
Pulmonary Ventilation (V sub E) |
The amount of air entering the entire lung (both conducting and respiratory zones) in one minute
Tidal Volume x Respiratory Rate Alveolar Ventilation + Anatomical Dead Space Ventilation |
|
|
Alveolar Ventilation (V sub A) |
Volume of air entering only the Respiratory Zone each minute - important: reps the volume of fresh air available for gas exchange Pulmonary Ventilation (Ve) - Anatomical Dead Space Ventilation (Vd) = Ve - (Conducting zone, approx. 1 mL per pound, X RR) = Total air/min - "non-alveolar" air/min |
|
|
Differences in Alveolar Ventilation with changes in ventilation patterns |
Shallow breathing vs. Deeper breathing - same Pulmonary ventilation - different Tidal Volume (deeper higher) - different Respiratory Rate (shallow higher) - different Alveolar Ventilation (deeper higher) - Deeper breathing gets more air to the alveoli |
|
|
Boyle's Law |
Pressure varies inversely with volume Pressure is proportional to (1/Volume) |
|
|
Atmospheric Pressure |
760 mmHg - this is also the Intrapulmonary pressure when no air is flowing in or out of the lungs |
|
|
Inspiration at Rest |
- active process, requires energy 1. Thoracic Cavity volume increases - external intercostals (b/w ribs) contract, move up and out - diaphragm contracts, moves down and flattens out, does most of the work 2. Pressure in the thoracic cavity drops below 760 mmHg (Boyle's law, volume increased) and air rushes in from the outside) |
|
|
Exhalation at rest |
- passive process 1. Decrease volume of thoracic cavity - external intercostals relax down and in - diaphragm relaxes up *Lungs never deflate completely 2. Pressure in thoracic cavity increases, above 760 mmHg |
|
|
Inhalation during Exercise |
Same as inhalation at rest, but deeper and faster - more contractions of diaphragm and external intercostals, larger movement |
|
|
Exhalation during exercise |
Muscles that relax: (like at rest) - diaphragm - external intercostals Muscles that contract: - internal intercostals (under externals, helps rib cage move down and in) - obliques - rectus abdominus (try to force diaphragm upwards a bit) - this exhalation is active |
|
|
Intrapleural Pressure - what it is and its function |
Pressure in the intrapleural space, 755 mmHg - subatmospheric pressure - in vacuum seal Function - makes sure lung doesn't collapse at the end of expiration - Allows for easy expansion of the lung (no resistance against inflation) |
|
|
Transpulmonary Pressure |
Intrapulmonary pressure - Intrapleural Pressure = about +5 mmHg usually - generated because of elastic recoil forces of lungs and chest wall - normally lungs slide against chest wall. After exhaation, tendency of lung to pull inwardly away from chest wall is balanced by the tendency of the chest wall to recoil in the opposite direction |
|
|
Pneumothorax |
- hole spontaneously develops in visceral pleura (blebs pop and rupture pleura) - air floods intrapleural space, intrapleural pressure becomes atmospheric, transpulmonary pressure goes to 0 - Collapsing (lung) force and Expanding (rib cage) force no longer balanced - Lung collapses and chest wall springs out - hole could also develop in parietal pleura if open to the external environment (i.e. trauma) |
|
|
Lung Compliance |
The change in lung volume as a result of a change in lung pressure Change in lung volume / Change in lung pressure - measures the "stretchability" of the lungs - high compliance = easier for lungs to stretch and increase in volume during inhalation |
|
|
Factors that influence the compliance of the lung |
Elastic Tissue components of the lung itself (1/3) - lung wants to collapse and go back to resting shape Surface tension inside the alveoli (2/3) - increase in either factor will decrease compliance and increase likelihood that lungs will collapse |
|
|
Compliance Factors: Elastic Tissue Components of the Lung
|
Elastin and collagen fibers are present in alveolar walls and throughout the lung - walls of alveoli (Type I cells?) have elastin - elastin wants to recoil - collapse force, helps us exhale - more elastin in lungs = lower compliance |
|
|
Compliance Factors: Surface Tension |
A force developed at the surface of a liquid due to H-bonding between polar water molecules - collapsing force, makes lungs less compliant - thin film of liquid lining the inside of the alveoli, it has surface tension, accounts for 2/3 of elastic behaviour of the lungs, promotes collapse |
|
|
Pulmonary Surfactant |
- Type II cells make Pulmonary Surfactant that sits on the air-liquid interface - it's mostly made up of phospholipids, also some proteins Function - reduces surface tension and increase compliance, prevents alveolar collapse - microbial defense - tags foreign material for macrophages (2/4 proteins involved) |
|
|
Neonatal Respiratory Distress Syndrome (nRDS) - occurs in... - description and reason why - treatment |
- occurs in premature infants - lungs not developed enough, immature surfactant system - lots of surface tension in lungs, poor function, alveolar collapse, hypoxemia (low blood O2) Treatment - administer surfactant like a drug - purify cow surfactant and put into babies' lungs - works until lungs mature and start making their own surfactant |
|
|
Spirometer |
Machine that measures lung volumes, can also help diagnose respiratory diseases - inhaling - bell lowers - exhaling - bell raises - recordings depending on bell movement in and out of the water |
|
|
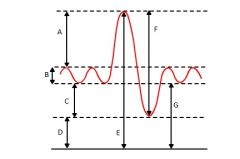
A. Inspiratory Reserve Volume - amount you can breathe after normal inhalation B. Tidal Volume - 500 mL for normal, healthy man C. Expiratory Reserve Volume - after end of exhalation, extra volume that you can still get out. Usually smaller than IRV D. Residual Volume - what's left behind that you can't expire, cannot measure with spirometer. About 1.5 L in normal 70 kg man. E. Total Lung Capacity - about 6L, ERV + TV + IRV + RV F. Vital Capacity - amount of useable air you can move through your lungs, Max exhalation to Max inhalation. ERV + TV + IRV (not RV) |
|
|
Forced Vital Capacity (FVC) |
Deepest breath in and out in a limited amount of time - amount of air you can move in and out of your lungs as fast as possible |
|
|
Forced Expiratory Volume (FEV-1) |
At the start of exhalation, amount of air you can get out in 1 sec Normal FEV-1/FVC = 80% - you exhale about 80% of your deepest breath in 1 sec |
|
|
Characteristics of obstructive diseases, that is how they affect the results of a pulmonary function test 3 obstructive diseases |
- obstruction to exhalation - total lung capacity is the same (FVC the same) - but it takes much longer to get the air out (FEV1 much smaller) FEV1 / FVC < 80% Asthma Chronic Bronchitis Emphysema |
|
|
Asthma |
Spasms in airways, can be triggered by exercise, air pollution, allergies - airway is hyper-responsive to things it shouldn't be - airways inflamed, narrow, bronchoconstriction -> hard to breathe - problem with smooth muscle contraction |
|
|
Chronic Bronchitis |
Excessive mucus and inflammation in the bronchial tube - enlarged mucus glands - productive cough (fluid behind it) - mucus blocks airways - resistance - smoking is chief cause |
|
|
Emphysema |
Walls between alveoli break down creating large air sacs (SA decreases) - loss of elastin (under Type I and II cells) - reduces elastic recoil, high compliance -> air can't come out - walls between alveoli destroyed, reduced number of alveoli = reduced gas exchange - smoking is major cause |
|
|
Characteristics of Restrictive diseases, how they affect the results of a pulmonary function test |
- lung capacity decreases, can't take in as much air -> decreased FVC and FEV-1 FEV1/FVC > 80% |
|
|
Pulmonary Fibrosis - what it is - causes |
Restrictive disease - fibrous scar tissue forms in lungs, lungs become less compliant, more stiff - scars less elastic than normal tissue, they contain a lot of collagen - alveoli won't expand easily (balloon with tape on it) Causes - chronic inhalation of asbestos, coal dust, pollution, sometimes unknown |
|
|
Partial Pressure of a gas - definition - in atmospheric pressure context - formula - PO2 and PCO2 of air at sea level |
Pressure exerted by a single gas in a mixture of gases or while dissolved in a liquid Atmospheric pressure of 760 mmHg at sea level - 21% O2 - 78% nitrogen - 0.03% CO2 PP = total pressure of all gases x fractional concentration of the one gas PO2 of air at sea level = 159 mmHg PO2 of air at sea level = 0.3 mmHg |
|
|
5 Factors that maximize simiple diffusion across the blood gas barrier Fick's Law |
1. Thin membrane (BGB, Type I cells) 2. High SA (lots of alveoli) 3. High pressure gradient 4. Blood velocity - slow in capillaries, max. time for diffusion 5. Lipid solubility for both CO2 and O2 Fick's Law: Rate of diffusion = (Pressure gradient x SA) / thickness |
|
|
Pressure of O2 and CO2 in: - atmosphere - alveoli - Pulmonary veins - Systemic arteries - body tissues - systemic veins - pulmonary arteries Where gas exchange happens and what's going in/out |
Atmosphere: PO2 = 159 mmHg, PCO2 = 0.3 mmHg Alveoli/Pulmonary veins/Systemic arteries: PO2 = 100 mmHg, PCO2 = 40 mmHg Body tissues/Systemic Veins/Pulmonary arteries: PO2 = 40 mmHg, PCO2 = 46 mmHg Gas exchange (always with capillaries): Alveoli - CO2 enters, O2 leaves Body Tissues - O2 enters, CO2 leaves |
|
|
Effects of holding breath (without changing metabolic activity) on arterial PO2, PCO2, pH |
Decreased PO2 Increased PCO2 Decreased pH (carbonic acid?) |
|
|
Effects of hyperventilating (without changing metabolic activity) on arterial PO2, PCO2, pH |
Increased PO2 Decreased PCO2 Increased pH |
|
|
Effects of increase in metabolic activity (exercise) without changing ventilation on arterial PO2, PCO2, pH |
Decreased PO2 Increased PCO2 Decreased pH |
|
|
Blood Composition |
RBCs aka erythrocytes - 45% WBCs ala leukocytes + Platelets - 1% Plasma (incl. proteins, ions, water, hormones, etc.) - 55% |
|
|
Two ways oxygen is transported in the blood
|
1. Dissolved in plasma - 1.5% 2. Bound to hemoglobin HbO2 inside RBCs - 98.5% - reversible reaction: O2 + Hb <--> HbO2 to generate oxyhemoglobin |
|
|
Structure of hemoglobin |
4 protein chains (globins), each with a heme group Each heme group has an iron, where O2 binds 1 hemoglobin binds 4 O2 molecules |
|
|
Functions of hemoglobin |
1. Bind Oxygen at the lungs 2. Dissociate that oxygen at the cells of the body's tissues for use 3. Pick up waste products (CO2) from cells 4. Bring CO2 back to lungs for removal |
|
|
Oxyhemoglobin dissociation curve + Saturation + steep slope - Resting cell - Alveoli |
% O2 saturation of hemoglobin vs. PO2 Resting cell - 75% O2 saturation in blood - tissues receive about 1 O2 from each hemoglobin Alveoli - 98% saturated hemoglobin, PO2 highest - saturated hemoglobin in lungs Steep slope: large saturation changes, lots of unloading O2 in the tissues |
|
|
Carbon Monoxide Poisoning |
- CO from car exhaust and tobacco smoke - CO binds to Hb heme group better than O2 does - treat by administering higher % of O2 |
|
|
How loading and unloading of oxygen is influence by PCO2, pH and temp |
Oxyhemoglobin dissociation curve shifts to left (hemoglobin more likely to hold onto O2 than give it to tissue) when: - CO2 drops - pH increases (blood more basic) - Temperature decreases |
|
|
The Bohr Effect |
In the presence of carbon dioxide or protons, hemoglobin has a decreased affinity for oxygen CO2 + H2O <-(carbonic anhydrase catalyst)-> H2CO3 <--> HCO3- + H+ - more CO2 and H+ will shift the oxyhemoglobin reaction to the left (less HbO2) - oxyhemoglobin dissociation curve shifts to the right, can drop more O2 off into tissues |
|
|
Carbon Dioxide Transport (3 ways) in the blood |
1. Dissolved form - 10% - CO2 20 more soluble than O2 2. Carbamino form - 20% CO2 + Hb <--> HbCO2 - attaches to the globin proteins, not the heme group like O2 3. Bicarbonate (HCO3-) form - 70% CO2 + H2O <-(carbonic anhydrase catalyst)-> H2CO3 <--> HCO3- + H+ - carbonic anhydrase found inside RBCs - carbonic acid quickly dissociates into bicarbonate and H+ - more CO2 = more acidic blood |
|
|
Erythropoiesis |
Helps maintain the proper number of erythrocytes Hormone erythropoietin released from kidneys stimulates erythrocyte synthesis in bone marrow Stimulated by drop of O2 in kidneys caused by: - decrease in number of RBCs - decrease in cardiac output - lung disease (poor gas exchange - emphysema, fibrosis, etc.) - high altitude (lower atmospheric pressure) |
|
|
Negative feedback loop - regulation of ventilation |
Set point: Arterial blood - PO2 = 100 mmHg, PCO2 = 40 mmHg, pH = 7.4 Controlled variables: PO2, PCO2 Sensor: Chemoreceptors (Peripheral, Central) Control Centre: Respiratory Centre in Medulla Effector: Respiratory muscles -> alter pulmonary ventilation |
|
|
Regulation of ventilation - types of chemoreceptors and where they're found |
Peripheral chemoreceptors: in aortic arch, carotid body Central Chemoreceptors: in medulla, bathed in CSF |
|
|
Central Chemoreceptors (medulla) - how they sense |
Central chemoreceptors only sensitive to H+ ions - H+ ions can't cross the BBB (to the medulla from the arteries) - Some CO2 in blood diffuses across BBB into CSF - CO2 + H2O etc etc., although it's slower with out carbonic anhydrase -> makes H+ and turns on chemoreceptor to tell brain that you have too much CO2 -> you breathe faster and deeper |
|
|
Peripheral Chemoreceptors - how they sense |
- sensitive to decreased PO2, decreased pH, and increased PCO2 - stimulates respiratory muscles to breathe deeper and activate exhalation |
|
|
Role of cerebral cortex in ventilation regulation response |
Cerebral cortex can override the medulla, making breathing voluntary But when blood pH drops too much, eventually chemoreceptors will kick in and medulla regains control - you can't die holding your breath! |

