![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
Functions of Respiratory System |
Extensive gas exchange surface area b/w air and circulating blood Filters, warms and humidifies air Moves air to and from exchange surfaces of lungs Protects respiratory surfaces from outside environment Speech Aids in pH regulation |
|
|
CO2 is |
By product of cellular metabolism CO2 + Plasma > Carbonic Acid > H+ & HCO3- ion Tissues also release H+ |
|
|
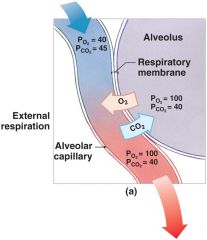
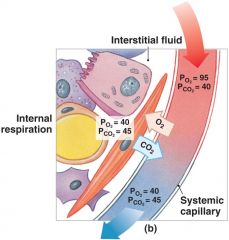
gas exchange |
Occurs across respiratory membranes (alveolar wall + capillary wall) Gases diffuse from high to low concentration
|
|
|
Boyle's Law |
Pressure is inversely related to volume Inspiration: Diaphragm and intercostal muscles contract>Volume increases>Pressure Decreases>Air Moves into lungs Expiration: Muscles relax>Volume decreases>Pressure increases>Air moves out |
|
|
Pulmonary Ventilation relies on |
Gas travelling from high to low pressure |
|
|
Quiet Breathing |
Eupnea-Active inhalation, passive exhalation Diapragmatic Costal |
|
|
Forced breathing |
Hypernea-Active inhalation & exhalation Assisted by accessory muscles (scalenes) Max levels during exhaustion |
|
|
Varying O2 demands lead to changes in |
Respiratory rate: Breaths per minute
Tidal Volume: volume of air per breath |
|
|
Tidal Volume |
Air moved in single breath 500ml |
|
|
Inspiratory Reserve Volume |
Air forcibly taken in above Tidal Volume 3000ml |
|
|
Expiratory Reserve Volume |
Air forcibly pushed out past Tidal Volume 1000ml |
|
|
Residual Volume |
Air that remains in lungs 500ml |
|
|
Vital Capacity |
Maximum amount of air moved through lungs TV+IRV+ERV 4500ml |
|
|
FVC |
Forced Vital Capacity Amount of air moved when forcibly exhale FEV1: Forced Expiratory Volume, air forced out 1 second |
|
|
If FVC is < predicted |
Restricted pulmonary disease (tuberculosis, fibrosis, myasthenia gravis) |
|
|
Obstructive Pulmonary Disease |
FEV1/FVCx100 if less than 80% (Emphysema,chronic obstructive pulmonary disease, asthma, bronchitis, lung cancer,pulmonary edema, decreased left heart output, or lung infections) |
|
|
Alveoli |
Microscopic membranous air sacs Simple squamous epithelial tissue Functional unit of lungs Site of gas exchange b/w respiratory and circulatory systems: diffusion Surfactant reduces surface tension, prevents alveoli collapse |
|
|
|
|
|
As temp increases, what happens to the binding affinity of hemoglobin |
Decreases (skeletal muscle) |
|
|
Bohr Effect |
Effect of pH on hemoglobin-saturation curve due to CO2
Excess CO2 = excess H+ CO2 + H2O > H2CO3 > H+ + HCO3- (with help of carbonic anhydrase) |
|
|
As pH decreases, what happens to binding affinity of hemoglobin |
Decreases (Skeletal Muscle-drop O2, pick up CO2) (pH increases: lungs-drop off CO2, pick up O2) |
|
|
CO2 in bloodstream |
70%is transported as carbonic acid (H2CO3) Which dissociates into H+ and bicarbonate (HCO3-) Chloride ion shift 23%is bound to amino groups of globular proteins in Hb molecule Forming carbaminohemoglobin 7% is transported as CO2 dissolved in plasma |
|
|
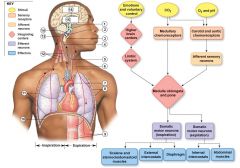
Regulation |
Medulla oblongata: inspiration and expiration Pons: ventilation Rhythmic breathing: network of spontaneous neurons Ventilation subject to modulation by chemoreceptor-linked reflexes and by higher brain centers |
|
|
5 sensory modifiers |
Baroreceptors in aortic or carotid sinuses blood pressure Chemoreceptors are sensitive to PCO2, PO2, or pH of blood or cerebrospinalfluid Stretch receptors respond to changes in lung volume Irritating physical or chemical stimuli in nasal cavity, larynx, or bronchial tree Other sensations including pain, changes in body temperature, abnormal visceral sensations |
|
|
Baroreceptor reflexes |
Baroreceptor stimulation Affects blood pressure and respiratory centers Blood pressure falls=Respiration increases Blood pressure increases=Respiration decreases |
|
|
Chemoreceptors adapt over time |
Excessive stimulation can occur-lead to a higher set point for CO2 Chronic Obstructive Pulmonary Disease Be careful when you giveCOPD patients O2 because CO2 doesn’t accumulate so they don’t breath |
|

|
|

