![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
Normal lung function |
Gas exchange |
|
|
Copd features |
Bronchiectasis |
|
|
Causes of copd
|
Main cause is smoking |
|
|
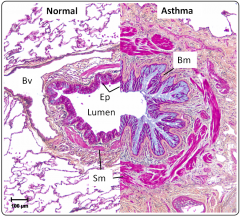
Acute asthma features
|
Charcot Leyden crystals |
|
|
Histology of acute asthma |
|
|
|
Bronchiectasis |
Permanent dilation of bronchioles and bronchi because of chronic and necrotising infections |
|

|
Bronchiectasis |
|
|
Clinical symptoms of bronchiectasis
|
Cough |
|
|
Causes of bronchiectasis
|
Congenital eg CF primary ciliary dyskinesia |
|
|
Chronic bronchitis definition
|
Cough productive of sputum for at least 3/12 of the year for the past 2/1
|
|
|
Features of chronic bronchitis |
Hypersecretion of mucous
Associated with smoking and infections Reversible airway obstruction |
|
|
Bronchiolitis
|
Acute inflam destruction of the smaller bronchioles
Virus, babies young children usually GVH disease |
|
|
Path changes in chronic bronchitis
|
Goblet cell hyperlplasia causing increased mucous |
|
|
Emphysema definition |
Abnormal permanent dilation of the airspace distal to the terminal bronchiole with destruction of their walls but not fibrosis |
|
|
Emphysema effects |
Enlargement of the acinus |
|
|
Classifications of emphysema |
Pan acinar |
|
|
Alpha 1 antitrypsin deficiency
|
Normally synthesised in the liver AD |
|
|
What causes chronic pulmonary fibrosis (honeycomb lung) |
Idiopathic Allergic alveolitis Pneumoconiosis (CWP Asbestosis Silicosis) Radiation Drugs (bleomycin) Connective tissue disorders (RA Sclerodema SLE) Diffuse malignancy Wegners Grannulomatosis Berylliosis Sarcoid |
|
|
Restrictive lung disease
|
Reduced movement
Chronic cough Shortness of breath Progresses to respiratory failure |
|
|
Pathogenesis of restrictive lung disease |
Acute and chronic interstitial diseases |
|
|
Fibrosing (intetstitial) lung diseases
|
Diffuse involvement of connective tissue and bronchiole / alveolar element |
|
|
Usual intetstitial pneumonia (idiopathic pulmonary fibrosis) |
Ie cryptogenic fibrosing alveolitis |
|
|
Acute intetstitial pneumonia
|
ARDS is clinical syndrome |
|
|
Coal miners pneumoconiosis |
Nodular fibrosis aggregates of dust laden macrophages and surrounding collagen
Progressive massive fibrosis widespread coalescent fibrous nodules causing scarring with contraction of the lung ?emphasema |
|
|
Silicosis |
Fibrogenic chronic interstitial |
|
|
Diseases caused by asbestosis
|
Recurrent pleural effusions |
|
|
Patholophysiology of asbestosis |
Fibres inhaled macrophages can't phagocytose macrophage death follows Macrophage cytokines and death cause fibrosis haemosiderin remains |
|
|
Cor pulmonale
|
Pul arteriolar vasoconstriction and medial hypertrophy |
|
|
Resp failure
|
Normal drive to breathe is hypercapnia and hypoxia |
|
|
Blue bloater
|
Mismatched vq |
|
|
Pink puffer
|
High vq |
|
|
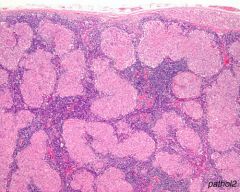
Sarcoidosis - Almost confluent non-caseating granulomas in a lymph node. But TB must be considered |
|
|
Types of lower resp tract infection
|
Lobar pneumonia
Bronchopneumonia Bronchiectasis Lung abcess Emphysema Tb lon |
|
|
Lobar pneumonia
|
Classically strep pneumoniae
Congestion to red hepatisation to grey hepatisation to resolution or death |
|
|
Complications of lobar pneumonia three
|
Abscess emphysema sepsis
|
|
|
Bronchopneumonia
|
Patchy inflam in lung around airways
Worse at bases because of gravity Common in immobile patients who can't cough well with other diseases |
|
|
Organisms that can cause bronchopneumonia
|
Staph strep haemophilus pseudomonas
|
|
|
Complications of bronchopneumonia
|
Abscess emphysema sepsis
|
|
|
Bronchiectasis
|
Focal destruction of bronchi and bronchioles because of infection leading to dilation
|
|
|
Mechanism of bronchiectasis
|
Obstruction to mucous flow due to Timor or foreign body
Viscid mucoid preventing drainage eg cf Ciliary abnormalities eg kartageners syndrome Commonly pseudomonas |
|
|
Bronchiectasis outcome
|
Cannot resolve
Chronic reinfect ion Scarring If focal may need to be excised |
|
|
Complications of bronchiectasis
|
Abcess |
|
|
Lung abscess
|
Focal destructive infection of lung are chums surrounded by fibrous capsule
|
|
|
Mechanisms of lung abscess
|
Apiration of infected material
Following pneumonia etc Septic emboli Direct trauma |
|
|
Lung abscess effects
|
Scarring, may need drainage
|
|
|
Lung abcess complications
|
Sepsis
Clubbing Secondary amyloidosis |
|
|
Empyema
|
Focal pyogenic infection of pleural space
Becomes compartmentalised |
|
|
Tb behaviour
|
Behaves like a cancer |
|
|
Reactivated tb
|
Often affects lung apices |
|
|
Miliary tb
|
Spread through bloodstream
Kidneys meninges bone and any other site In inmunocompromised pattern can be unusual with early dissemination |
|
|
Primary tb
|
Bronchopneumonia
Spreads to Hilar lymph nodes leaving scar and enlarged scarred node (gohn complex) Infection usually controlled |
|
|
Asthma prevalence
|
0.5–3% of UK population
More common in children but more severe in adults |
|
|
Clinical presentation of asthma
|
Rapid onset of difficulty in expiration with wheezing
Reduced peak flow |
|
|
Asthma improved by
|
Steroids
Beta two agonists Anticholinergics Others |
|
|
Types of asthma
|
Defined by trigger |
|
|
Cause of rapid asthma onset
|
Type one sensitivity
Sudden release of histamine from mast cells and other mediators Both can be activated by non specific factors eg cold |
|
|
Pathology of asthma
|
Smooth muscle contraction
Oedema and inflam exudate Excess mucus secretion |
|
|
Long term consequences of asthma
|
Overdistension of lung
Focal lung collapse Bronchiectasis Infection aspergillus etc |
|
|
Causes of pulmonary embolism
|
Usually thrombus
Fat – bone marrow from fracture Amniotic fluid during parturition Injected material eg drugs Risk factors include immobility, surgery, hypercoagulability, contracteptive pill, underlying malignancy, pelvic mass with obstruction of venous return |
|
|
Causes of dvt
|
Trauma, inflam
Innate or acquired increased clotting Reduced flow Commonest cause due to immobility of muscle pump Genetic predisposition to clotting usually also |
|
|
Predisposing conditions to dvt
|
Surgery
Obesity Pro coagulant States eg Oestrogenic drugs Hyperviscosity Malignancy Auto antibodies Inherited |
|
|
Presentation of DVT
|
Acute painful swelling of calf or whole leg
Superficial veins may be distended Skin red and warm as blood gets round obstruction Pitting oedema |
|
|
Swollen painful leg could be
|
Dvt
Cellulitis Ruptured bakers cyst synovial due to arthritis of the knee Obese elderly can be predisposed to all three |
|
|
Pelvic thrombus caused by
|
Tumours
Inflam Surgery |
|
|
Effects of pulmonary thromboembolism depend on |
Size
Large saddle embolus causes death Multiple small causes pulmonary hypertension Medium sized embolus causes wedge shaped infarct |
|
|
Clinical presentation of thromboembolis |
Large – collapse breathlessness death
Intermediate – pleuritic chest pain tachypnea cyanosis haemoptysis Small – may be a symptomatic may be pleuritic pain |
|
|
Paradoxical embolus
|
Misses lungs and enters systemic circulation via shunt eg septal defect
May cause stroke limb or bowel ischaemia etc |
|
|
Amniotic fluid embolus |
Fluid contains everything that falls off foetus
Lodges in small vessels Causes diffuse intravascular coagulation, shock, death |
|
|
Fat embolus
|
Follows major trauma
Lodges in small vessels 90% of major trauma No allergic response Causes symptoms only when massive |
|
|
Pulmonary oedema effects |
Causes dyspnoea
May be severe enough to teach upper airways– frothing |
|
|
Haemodynamic causes of pulmonary oedema
|
Lhs failure
Mitral stenosis Volume overload Pulmonary vein obstruction Lymphatic obstruction Decreased oncotic pressure eg low albumin nephrotic syndrome liver disease protein losing enteropathies |
|
|
Micro vascular injury causes of pulmonary oedema
|
Inhaling noxious gases |
|
|
Shock lung – ARDS
|
Diffuse damage to alveolar wall capillaries and epithelium
Membrane of inflam exudate, dead cells Lungs become firm and lose elasticity Severe impairment of gas transfer, refractory to oxygen therapy |
|
|
Causes of ARDS
|
Same as cause PE but more severe
Hypoxic patient on ventilator May follow shock Often associated with damage to other organs eg renal failure by same cause |
|
|
Primary hypertension
|
Idiopathic |
|
|
Secondary hypertension
|
Chronic |
|
|
Lung transplant consideration
|
Hypertensive heart due to hard lung may be too much for new lung, so may need lung and heart transfer
|
|
|
What usually worsens asthma? what usually worsens COPD? |
Allergen
Infection |
|
|
Cause of blackened lymph nodes in the lung
|
Uptake of anthracotic pigment by macrophages (carbon from polluted air)
Seen in older people and smokers |
|
|
Yellowish lung lobe |
Consolidation due to infection eg secondary to tumour
|
|
|
Why small cell carcinoma of the lung so dangerous |
Metastasises early (as do many lung cancers), often widely disseminated before the primary lung tumour is diagnosed. |
|
|
Definition of pneumonia
|
Acute or chronic inflammation of the alveoli
|
|
|
Non infection causes of pneumonia (6)
|
Neoplasia
Sarcoid Amyloid Vascullitis Drugs radiotherapy |
|
|
Chronic pneumonia and six causes
|
Pneumonic illness >1/52
Associated cxr changes Causes Tb Mycobacterium Nocardia Fungi Protozoa Worms |
|
|
Aspiration pneumonia
|
Elderly or altered consciousness at risk
Much of damage immediate and due to acid Infection may follow a few days later |
|
|
Atypical pneumonia
|
Fails to respond to usual antibiotics
Bacteriology fails to provide diagnosis Mycoplasma pneumoniae Chlamydiaophila |
|
|
Ventilator associated pneumonia
|
Ventilated patient >48h/ intubation
|
|
|
Epidemiology of cap
|
50+
1/100 /1 Mid winter or spring 60–90% have underlying disease 20% require hospital 5–10% mortality Rfs for death are age severe inter current illness recent anaesthetic smoker heart failure hiv copd |
|
|
Causes of cap
|
Viral bacterial fungi
Strep pneumoniae is most common cause, is a commensal Certain organisms peak in epidemic years Some from environment eg legionella or animals eg chlamydiophilla psittaci |
|
|
How can bacteria get into lungs
|
From upper airways, exogenous or already colonising
Less commonly via haematogenous spread |
|
|
Commensal s pneumoniae
|
Can invade if we acquire new epithelial serotypes
Flu can cause activation, strep will bind more to receptors |
|
|
Signs of pneumonia
|
Fever
Low bp Increased resporatory rate Tachycardia Cobsolidation / effusion Severe Exhaustion Cyanosis Use of accessory muscles |
|
|
Effusion vs consolidation
|
Effusion compresses lung
Consolidation is an infiltration of the lung |
|
|
Parapneumonic effusion
|
Exudative phase – pleural inflam generates fluid
Fibropurulent stage – fibrin deposition, organisms invade Pleural glucose and ph fall Look up final stage |
|
|
Investigations for pneumonia |
FBC
u&e Crp Lft Abg if unwell Cxr Ct in recurrent, those unresponsive to treatment or sometimes in Inmunocompromised early |
|
|
Microbiological investigations
|
Blood cultures, not often positive but very useful
Serology useful in outbreak situation Antigen testing Pleural fluid sampling Sputum Bal |
|
|
Sputum samples
|
Not a good means of diagnosing pneumonia because bugs come through mouth
Only six percent produce sputum Half of cultures are negative Useful when non–commensal bacteria are being considered Cold agglutinins Lung biopsy rare useful for immunocompromised patients |
|
|
In all severe pneumonia patients check
|
Pneumococcal antigen blood sputum urine
Legionella antigen .. Others |
|
|
Management of pneumonia
|
Early antibiotics
Switch to oral at 48h if doing well Longer for legionella gram negative or staph aureus Guide to drugs in notes 3–5/365 for mild generally oral route 1–2/52 in severe or longer for invasive staph |
|
|
If fail to respond to antibiotics
|
Older may take longer as may multilobe involvement or pre exiting lung disease
Consider resistant organisms |
|
|
Complications
|
Empayema
Sepsis Abcess Ards Metastatic infection Rarely neurological sequelae Bronchiectasis (less common in antibiotic era) |
|
|
Hospital acquired pneumonia
|
>48h after admission
Risk factors age immobility coexisting illness sepsis dysphasia reduced consciousness instrumentation etc |
|
|
Bugs of HAP
|
Staph aureus
Chlamydia trachomatis Pneumocystis jerovecii (commonest opportunistic infection in hiv patients) |
|
|
History of atypical
|
Cxr worse than signs suggest
Usually lower loves Mild urti followed by pneumonia |
|
|
Legionella colonises what
|
Water piping systems |
|
|
Pott's disease |
Collapse of the spine due to TB infection |

