![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
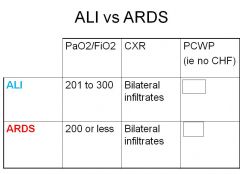
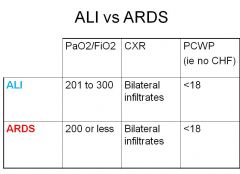
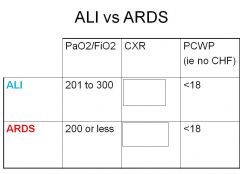
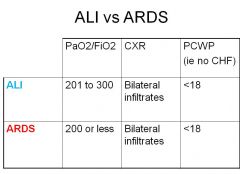
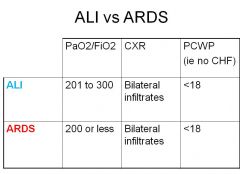
what are the 3 clinical features of acute lung injury?
*** |
Bilateral radiographic infiltrates.
(PaO2/FiO2) between 201 and 300 mmHg - The PaO2 is measured in mmHg and the FiO2 is expressed as a decimal between 0.21 and 1.00 No clinical evidence for an elevated left atrial pressure. If measured, the pulmonary capillary wedge pressure is 18 mmHg or less. (aka no evidence of HF) |
|
|
what is the definition of Acute Respiratory Distress Syndrome (ARDS)
*** |
The definition of ARDS is the same as acute lung injury except that the hypoxia is worse, requiring a PaO2/FiO2 ratio of 200 mmHg or less.
|
|
|
does the severity of the hypoxia with ARDS impact predictability on clinical course or survival?
|
nope...
|
|
|
typically develops over 4 to 48 hours and persists for days to weeks
Progressive hypoxemia despite increasing supplemental oxygen many times requiring mechanical ventilation.. this describes? |
Acute Respiratory Distress Syndrome (ARDS)
|
|
|
how do you calculate FiO2
what is it normally? |
FiO2 = ((Liters of O2) x 3) + 21
33% |
|
|
|
|
|
|
|
|
|
|
|
what are 3 derangements in ARDS?
|
Impaired gas exchange — Ventilation-perfusion mismatching and physiologic shunting are the major causes of hypoxemia
Decreased lung compliance — Decreased pulmonary compliance is one of the hallmarks of ARDS . The low compliance is due to the stiffness of poorly or non-aerated lung Pulmonary hypertension — Pulmonary hypertension occurs in up to 25 percent of patients with ARDS subjected to mechanical ventilation. Contributing factors include hypoxic vasoconstriction and vascular compression by positive pressure ventilation |
|
|
why do you have impaired gas exchange with ARDS?
|
Alveoli have a tendency to collapse – complete collapse can contribute to barotrauma via repeated re-inflation & collapse
Diffuse alveolar damage leads to destruction of type II pneumocytes Loss of surfactant to atelectasis -> increased A-a gradient ->hypoxemia -> increased work of breathing and can result in muscle fatigue and failure |
|
|
how do you have decreased lung compliance in ARDS?
|
Loss of surfactant makes opening and closing of airways more difficult by the increase in airway pressure due to loss of surfactant
Causes a more ‘stiff’ appearance of lung function Not a hemogenous effect – alveoli have different levels of involvment |
|
|
how do you have pulmonary HT in ARDS?
|
Pulmonary vasculature vasoconstricts with hypoxemia leading to increased pulmonary artery pressures and subsequent right ventricluar systolic pressure elevation
If severe enough, forward flow is reduced and cardiac output drops Cardiac output is also affected by intrathoracic pressure of ventilator |
|
|
what is the A-a gradient?
what does a wider gap show? |
Difference between alveolar (A) oxygen content and arterial (a) oxygen content
Wider gap suggests poor diffusion of oxygen from the alveoli to the pulmonary arterial capillaries |
|
|
what should your difference in A-a be?
|
Should not be any more than
Patient age/4 + 2.5 |
|
|
what are the 3 stages in progression of ARDS?
|
“exudative" stage, characterized by diffuse alveolar damage over the first week
"proliferative" stage, characterized by resolution of pulmonary edema and by proliferation of type II alveolar cells, squamous metaplasia, interstitial infiltration by myofibroblasts, and early deposition of collagen. Some patients progress to a third "fibrotic" stage, characterized by obliteration of normal lung architecture, diffuse fibrosis, and cyst formation. |
|
|
what is treatment for Acute respiratory distress syndrome (ARDS)?
|
mostly supportive
can give prolonged ventilation with high O2 Goal is to oxygenate while reducing barotrauma caused by increased pressure from tidal volume/lung expansion |
|
|
if ventillation continues for longer than 10-14 days of ARDS what should you do? "rule of thumb"
|
tracheostomy
|
|
|
diagnosis of ARDS is based on 3 things... what are they
*** |
CXR, PaO2/FiO2 and no clinical findings of CHF
|
|
|
main treatment for ARDS
*** |
supportive
|
|
|
what is the general mechanism of disease with ARDS?
**** |
Cytokine activation with damage to alveolar walls and type II pneumocytes with resultant loss of surfactant and further atelectasis and barotrauma.
|

