![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
105 Cards in this Set
- Front
- Back
|
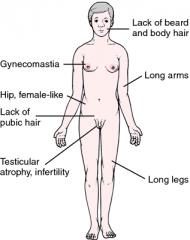
Klinefelter's Syndrome
|
XXY Chromosome Abnormality
Testicular atrophy, eunuchoid body shape, tall, long, extremities, gynecomastia, female hair distribution, developmental delay. Presence of inactivated X chromosome (Barr body). Dysgenesis of seminiferous tubules ---> low inhibin and increased FSH Abnormal Leydig cell function ---> low testosterone and increased LH and estrogen |
|
|
Klinefelter's Syndrome
|
|
|
|
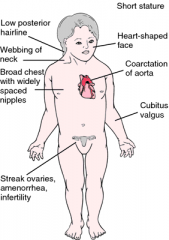
Turner Syndrome
|
XO Chromosome Abnormality
Short stature, ovarian dysgenesis (streak ovary with infertility), shield chest, bicuspid aortic valve, webbing of neck, (cystic hygroma), lymphedema, preductal coarctation of aorta, horseshoe kidney, dysgerminoma ---> primary amennorhea No Barr body. Menopause before menarche; decreased estrogen ---> increased LH And FSH |
|
|
Turner Syndrome
|
|
|
|
Double Y Male
|
XYY Chromosome Abnormality
Phenotypically normal, very tall , acne, antisocial behavior, normal fertility, small percentage dx with autism spectrum disorders. |
|
|
High Testosterone
High LH |
Defective androgen receptor.
|
|
|
High Testosterone
Low LH |
Testosterone-secreting tumor, exogenous steroids.
|
|
|
Low Testosterone
High LH |
Primary hypogonadism.
|
|
|
Low Testosterone
Low LH |
Hypogonadotropic hypogonadism.
|
|
|
Pseudohermaphroditism
|
Disagreement between the phenotypic (external genitalia) and gonadal (testes, ovaries) sex.
|
|
|
Female Pseudohermaphroditism (XX)
|
Ovaries present, but external genitalia are virilized or ambiguous.
Due to excessive and inappropriate exposure to androgenic steroids during early gestation (congenital adrenal hyperplasia or exogenous administration of androgens during pregnancy). |
|
|
Male Pseudohermaphroditism (XY)
|
Testes present, but external genitalia are female or ambiguous.
Most common form is androgen insensitivity syndrome (testicular feminization). |
|
|
True Hermaphroditism
|
Both ovary and testicular tissue are present (ovotestis); ambiguous genitalia; very rare.
|
|
|
Androgen Insensitivity Syndrome
|
Defect in androgen receptor resulting in normal-appearing female; female external genitalia with rudimentary vagina; uterus and uterine tubes generally absent.
Presents with no sexual hair, develops testes (often found in labia majora; surgically removed to prevent malignancy). Increased testosterone, estrogen, LH. |
|
|
5 alpha-reductase Deficiency
|
Autosomal recessive; sex limited to genetic males.
Inability to convert testosterone to DHT. Ambiguous genitalia until puberty when increased testosterone causes masculinization and growth of external genitalia. Normal internal genitalia. Testosterone/estrogen and LH levels are normal. |
|
|
Kallmann Syndrome
|
Defective development of GnRH cells and olfactory placode.
Decreased synthesis of GnRH in the hypothalamus; anosmia; lack of secondary sexual characteristics, autosomal dominant. Decreased GnRH, LH, FSH, testosterone, and sperm count. |
|
|
Hydatidiform Mole
|
Cystic swelling of chorionic villi and proliferation of chorionic trophoblasts that presents with abnormal vaginal bleeding.
Most common precursor of choriocarcinoma. "Honeycombed uterus", "cluster of grapes" appearance, abnormally enlarged uterus. Complete moles usually have "snowstorm" appearance with no fetus during 1st sonogram. Moles can lead to uterine rupture. Increased hCG. Tx is D&C with Methotrexate. |
|
|
Hydatidiform Mole
|

|
|
|
Preeclampsia-eclampsia
|
Preeclampsia: pregnancy-induced hypertension, proteinuria, and edema.
Eclampsia: preeclampsia and seizures. Occurs in 7% of women from 20 wks to 6 wks postpartum. Increased incidence in women with preexisting HTN, diabetes, chronic renal disease, and autoimmune disorders. Caused by placental ischemia due to impaired vasodilation of spiral arteries, resulting in increased vascular tone. Can be associated with HELLP Syndrome: Hemolysis Elevated LFTs Low Platelets Mortality due to cerebral hemorrhage and ARDS. |
|
|
Clinical Features of Preeclampsia
|
Headache, blurred vision, abdominal pain, edema of face and extremities, altered mentation, hyperreflexia; lab findings may include thrombocytopenia, hyperuricemia.
|
|
|
Treatment of Preeclampsia
|
Delivery of fetus as soon as viable. Otherwise, bedrest, salt-restriction, and monitoring and treatment of HTN.
IV magnesium sulfate and diazepam to prevent and treat seizures of eclampsia. |
|
|
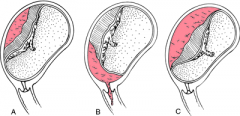
Abruptio Placentae
|
Premature detachment of placenta from implantation site, fetal death.
May be associated with DIC, smoking, HTN, cocaine use. |
|
|
Types of Placental Abruption
|
|
|
|
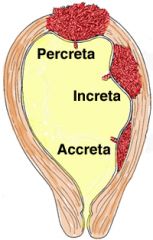
Placenta Accreta
|
Accreta - "encased in" - encased in myometrium.
Defective decidual layer allows placenta to attach to myometrium; no separatin of placenta at birth. Increase risk with prior c-section, inflammation, and placenta previa. Massive bleeding after delivery. |
|
|
Types of Placenta Accreta
|
|
|
|
Placenta Previa
|
Attachment of placenta to lower uterine segment; may occlude internal os.
Increased risk with multiparity and prior c-section. Painless bleeding in any trimester. |
|
|
Types of Placenta Previa
|
|
|
|
Ectopic Pregnancy
|
Most often in fallopian tubes; suspect with history of amenorrhea, increased hCG, and sudden lower abdominal pain; confirm with ultrasound.
Endometrial biopsy shows decidualized endometrium but no chorionic villi (develops only in intrauterine pregnancy). Presents as pain with out without bleeding. Risk factors are history of infertility, salpingitis, PID, ruptured appendix, prior tubal surgery. |
|
|
Retained Placental Tissue
|
May cause postpartum hemorrhage.
|
|
|
Polyhydramnios
|
> 1.5-2 L of amniotic fluid; associated with esophageal/duodenal atresia, causing inability to swallow amniotic fluid, and with anencephaly.
|
|
|
Oligohydramnios
|
< 0.5 L of amniotic fluid; associated with placental insufficiency, bilateral renal agenesis, or posterior urethral valves (in males) and resultant inability to excrete urine.
Can give rise to Potter's syndrome. |
|
|
Cervical Dysplasia and Carcinoma In Situ
|
Disordered epithelial growth; begins at basal layer of squamo-columnar junction and extends outward. Classified as CIN 1, CIN 2, or CIN 3 depending on extent of dysplasia. May progress to invasive carcinoma if left untreated.
Associated with HPV 16 and 18. Risk factors: multiple sex partners, smoking, early sexual intercourse, HIV infection. |
|
|
Cervical Invasive Carcinoma
|
Often squamous cell carcinoma.
Pap smear can catch cervical dysplasia (koilocytes) before it progresses to invasive carcinoma. Lateral invasion can block ureters, causing renal failure. |
|
|
Endometritis
|
Inflammation of the endometrium associated with retained products of conception following delivery (vaginal, C-section), miscarriage, abortion, foreign body, IUD.
Retained material in uterus promotes infection by bacterial flora from vagina or intestinal tract. Presents as abdominal pain, fever, uterine tenderness, menstrual abnormalities, infertility. Treatment: Cefoxitin, ticarcillin-clavulanate, ampicillin-sulbactam. |
|
|
Endometriosis
|
Non-neoplastic endometrial glands/stroma in abnormal locations outside the uterus.
Characterized by cyclic bleeding from ectopic endometrial tissue resulting in blood-filled "chocolate cysts" in ovary or peritoneum. Manifests clinically as severe menstrual-related pain. Menorrhagia, dysmenorrhea, dyspareunia. Often results in pain intercourse and infertility. Can be due to retrograde menstrual flow. Uterus is normal-sized. |
|
|
Adenomyosis
|
Endometrium within the myometrium.
Menorrhagia, dysmenorrhea, pelvic pain, uterus is enlarged. Treatment is hysterectomy. |
|
|
Endometrial Hyperplasia
|
Abnormal endometrial gland proliferation usually caused by excess estrogen stimulation.
Increase risk for endometrial carcinoma. Manifests as postmenopausal vaginal bleeding. Risk factors include anovulatory cycles, HRT, PCOS, and granulosa cell tumor. |
|
|
Endometrial Carcinoma
|
Most common gynecologic malignancy typically preceded by endometrial hyperplasia. Presents with vaginal bleeding.
Peak occurence at 55-65 years old. Risk factors include prolonged use of estrogen without progestins, obesity, diabetes, HTN, nulliparity, and late menopause. Increased myometrial invasion ---> decreased prognosis |
|
|
Leiomyoma
|
Whorled pattern of smooth muscle bundles - myometrial fibroid tumor; most common female tumor.
Often presents with multiple tumors with well-demarcated borders. Benign smooth muscle tumor; malignant transformation is RARE. Estrogen-sensitive; tumor size increases in pregnancy and decreases in menopause. Peak occurrence at 20-40 years of age; increased incidence in black. May be asymptomatic, causes abnormal uterine bleeding, or results in miscarriage. Severe bleeding may lead to iron deficiency anemia. |
|
|
Leiomyosarcoma
|
Bulky, irregularly shaped tumor with areas of necrosis and hemorrhage; typically arising de novo (not from Leiomyoma).
Highly aggressive tumor with tendency to recur. May protrude into cervix and bleed. Most commonly seen in middle-aged women and increased incidence in blacks. |
|
|
Gynecologic Tumor Epidemiology
|
Incidence: endometrial > ovarian > cervical (US); cervical cancer is most common worldwide.
Worst prognosis: ovarian > cervical > endometrial. |
|
|
Premature Ovarian Failure
|
Premature atresia of ovarian follicles in women of reproductive age.
Patient presents with signs of menopause after puberty but before age 40. Decreased estrogen, increased LH and FSH. |
|
|
Most Common Causes of Anovulation
|
PCOS
Obesity Asherman's Syndrome (adhesions) HPO Axis abnormalities Eating disorders Cushing's Syndrome Adrenal Insufficiency |
|
|
PCOS
|
Increased LH, decreased FSH, increased testosterone and estrogen.
Increased LH leads to anovulation, hyperandrogenism due to deranged steroid synthesis by Theca cells. Enlarged, bilateral cystic ovaries. Manifests as amenorrhea, infertility, obesity, hirsutism, acne. Associated with insulin resistance. Increase risk of endometrial cancer. |
|
|
Treatment for PCOS
|
Weight reduction, low-dose OCPS, medroxyprogesterone (decreases LH and androgenesis), spironolactone (acne and hirsutism), clomiphene for women who want to get pregnant.
|
|
|
US of PCOS
|
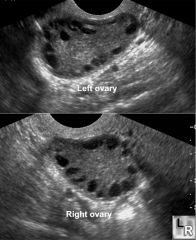
|
|
|
Follicular Ovarian Cyst
|
Distention of unruptured graafian follicle.
May be associated with hyperestrinism and endometrial hyperplasia. Most common ovarian mass in young women. |
|
|
Corpus Luteum Cyst
|
Hemorrhage into persistent corpus luteum.
Commonly regresses spontaneously. |
|
|
Theca-Lutein Cyst
|
Often bilateral/multiple.
Due to gonadotropin stimulation. Associated with choriocarcinoma and moles. |
|
|
Hemorrhagic Cyst
|
Blood vessel rupture in cyst wall. Cyst grows with increased blood retention; usually self-resolves.
|
|
|
Dermoid Cyst
|
Mature teratoma.
Cystic growths filled with various types of tissues such as fat, hair, teeth, bits of bone, cartilage. |
|
|
Endometrioid Cyst
|
Endometriosis within ovary with cyst formation.
Varies with menstrual cycle. When filled with dark, reddish-brown blood it is called a "chocolate cyst". |
|
|
Ovarian Germ Cell Tumors
|
Most common in adolescents.
|
|
|
Ovarian Germ Cell Tumor: Dysgerminoma
|
Tumor markers: hCG, LDH
Malignant, equivalent to male seminoma but rare (1% of germ cell tumors in females vs. 30% in males). Sheets of uniform cells; associated with Turner Syndrome. |
|
|
Ovarian Germ Cell Tumor: Choriocarcinoma
|
Tumor marker: hCG
Rare but malignant, malignancy of trophoblastic tissue and absence of chorionic villi; can develop during pregnancy in mother or baby, increased frequency of theca-lutein cysts. Early hematogenous spread to lungs. |
|
|
Ovarian Germ Cell Tumor: Yolk Sac Tumor (Endodermal Sinus)
|
Tumor marker: AFP
Aggressive malignancy in ovaries (testes in boys) and sacrococcygeal area of young children. Yellow, friable, solid masses. 50% had Schiller-Duval bodies that resemble glomeruli. |
|
|
Ovarian Germ Cell Tumor: Teratoma
|
90% of ovarian germ cell tumors that contain cells from 2 or 3 germ layers.
Mature teratoma (dermoid cyst) is most common frequent benign ovarian tumor. Immature teratoma is aggressively malignant. Struma ovarii contains functional thyroid tissue and can present as hyperthyroidism. |
|
|
Ovarian Non-Germ Cell Tumor: Serous Cystadenoma
|
20% of ovarian tumors; benign, frequently bilateral, lined with fallopian tube-like epithelium.
Increased CA-125 is a general ovarian cancer marker used for progression but not screening. |
|
|
Ovarian Non-Germ Cell Tumor: Serous Cystadenocarcinoma
|
45% of ovarian tumors; malignant and frequently bilateral. Psammoma bodes seen in histology.
Risk factors: BRCA-1,2, HNPCC, family history. |
|
|
Ovarian Non-Germ Cell Tumor: Mucinous Cystadenoma
|
Multilocular cyst lined by mucus-secreting epithelium. Benign, intestine-like tissue.
|
|
|
Ovarian Non-Germ Cell Tumor: Mucinous Cystadenocarcinoma
|
Malignant, Pseudomyxoma peritonei - intraperitoneal accumulation of mucinous materinal from ovarian or appendical tumor.
|
|
|
Ovarian Non-Germ Cell Tumor: Brenner Tumor
|
Benign and unilateral; looks like Bladder.
Solid tumor that is pale yellow-tan color and appears encapsulated. "Coffee bean" nuclei on H&E. |
|
|
Ovarian Non-Germ Cell Tumor: Fibromas
|
Bundles of spindle-shaped fibroblasts.
Meigs' syndrome - triad of ovarian fibroma, ascites, and hyrdothorax. Pulling sensation in groin. |
|
|
Ovarian Non-Germ Cell Tumor: Granulosa Cell Tumor
|
Secretes estrogne ---> precocious puberty (kids). Can cause endometrial hyperplasia or carcinoma in adults.
Call-Exner bodies - small follicles filled with eosinophilic secretions. Abnormal uterine bleeding. |
|
|
Ovarian Non-Germ Cell Tumor: Krukenberg Tumor
|
GI malignancy that metastasizes to ovaries, causing a mucin-secreting signet cell adenocarcinoma.
|
|
|
Vaginal Carcinoma
|
1. Squamous cell carcinoma (SCC) secondary to cervical SCC.
2. Clear cell adenocarcinoma - affects women who had exposure to DES in utero. 3. Sarcoma botryoides (rhabdomyosarcoma variant) - affects girls < 4 years of age; spindle shaped tumor cels that are desmin positive. |
|
|
Benign Breast Tumor: Fibroadenoma
|
Small, mobile, firm mass with sharp edges.
Most common tumor in those < 35 years of age. Increase in size and tenderness with increased estrogen (pregnancy, menstruation). Found in stroma. NOT a precursor to breast cancer. |
|
|
Benign Breast Tumor: Intraductal Papilloma
|
Small tumor that grows in lactiferous ducts, typically beneath areola.
Serious or blood nipple discharge, slight risk for carcinoma. |
|
|
Benign Breast Tumor: Phyllodes Tumor
|
Large bulky mass of connective tissue and cysts, "leaf-like" projectins found in the stroma.
Most common in 60s, some may become malignant. |
|
|
Malignant Breast Tumors
|
Common postmenopause and arise from mammary duct epithelium or lobular glands most often located in upper-outer quadrant of breast.
Overexpression of estrogen/progesterone receptors or erb-B2 is common and affects therapy and prognosis. Axillary lymph node involvement is the most important prognostic factor. |
|
|
Risk Factors for Malignant Breast Tumors
|
Increased estrogen exposure
Increased total number of menstrual cycles Older age at first live birth Obesity |
|
|
Noninvasive Malignant Breast Tumor:
Ductal Carcinoma In Situ (DCIS) |
Fills ductal lumen, arises from ductal hyperplasia.
Early malignancy without basement membrane. |
|
|
Noninvasive Malignant Breast Tumor:
Comedocarcinoma |
Ductal, caseous necrosis, subtype of DCIS.
|
|
|
Invasive Malignant Breast Tumor:
Invasive Ductal |
Firm, fibrous, rock-hard mass with sharp margins and small, glandular, duct-like cells.
Classic "stellate" morphology. Worst and most invasive, most common (76% of all breast cancers). |
|
|
Invasive Malignant Breast Tumor:
Invasive Lobular |
Orderly row of cells.
Often multiple and bilateral. |
|
|
Invasive Malignant Breast Tumor:
Medullary |
Fleshy, cellular, lymphocytic infiltrate.
Good prognosis. |
|
|
Invasive Malignant Breast Tumor:
Inflammatory |
Dermal lymphatic invasion by breast carcinoma.
P'eau d'orange (breast skin resembles orange peel); neoplastic cells block lymphatic drainage. 50% survival at 5 years. |
|
|
Invasive Malignant Breast Tumor:
Paget's Disease |
Eczematous patches on nipple. Paget cells = large cells with epidermis with clear halo.
Suggests underlying carcinoma, also found on vulva. |
|
|
Fibrocystic Disease
|
Most common cause of "breast lumps" from age 25 to menopause.
Presents with premenstrual pain and multiple lesions, often bilateral and fluctuation in size of mass. Usually does not indicate increase risk of carcinoma. |
|
|
Fibrosis Fibrocystic Disease
|
Hyperplasia of breast stroma.
|
|
|
Cystic Fibrocystic Disease
|
Fluid filled, blue dome. Ductal dilation.
|
|
|
Sclerosing Adenosis Fibrocystic Disease
|
Increased acini and intralobular fibrosis associated with calcifications.
|
|
|
Epithelial Hyperplasia Fibrocystic Disease
|
Increase in number of epithelial cell layers in terminal duct lobule.
Increase risk of carcinoma with atypical cells. Occurs in women > 30 years of age. |
|
|
Acute Mastitis
|
Breast abscess during breast-feeding.
Increase risk of bacterial infection through cracks in the nipple; S. aureus is most common pathogen. |
|
|
Fat Necrosis
|
A benign painless lump that forms as a result of breast tissue trauma.
|
|
|
Gynecomastia
|
Results from:
1. Hyperestrogenism - cirrhosis, testicular tumor, puberty, old age. 2. Klinefelter's Syndrome 3. Drugs - estrogen, marijuana, heroin, psychoactive drugs, Spironolactone, Digitalis, Cimetidine, Alcohol, Ketoconazole (Some Drugs Create Awesome Knockers). |
|
|
Prostate Pathology: Prostatitis
|
Dysuria, frequency, urgency, low back pain.
Acute: bacterial (e. coli) Chronic: abacterial |
|
|
Benign Prostatic Hyperplasia (BPH)
|
Common in men > 50. Hyperplasia of the prostate gland that may be due to an age-related increase in estradiol with possible sensitization of the prostate to growth-promoting effects of DHT.
Nodular enlargement of periurethral (lateral and middle) lobes which compress the urethra into a vertical slit. Not considered a premalignant lesion. Increased PSA is marker. |
|
|
Clinical Features of BPH
|
Increased frequency of urination, nocturia, difficulty startin and stopping stream of urination, and dysuria.
May lead to distention and hypertrophy of the bladder, hydronephrosis, and UTIs. Tx: alpha 1-antagonists (terazosin, tamsuloin), finasteride. |
|
|
Prostatic Adenocarcinoma
|
Common in men > 50.
Arises most often from the posterior lobe (peripheral zone) of the prostate gland and is most frequently diagnosed by digital rectal exam (hard nodule) and prostate biopsy. PAP and PSA are useful tumor markers. Osteoblastic metastases in bone may develop in late stages. |
|
|
Cryptorchidism
|
Undescended testis (one or both); impaired spermatogenesis (since sperm develop best at temps < 37 C); normal testosterone levels.
Associated with increase risk of germ cell tumors, prematurity increases risk of cryptorchidism. Decreased inhibin, increased FSH, normal LH and testosterone. |
|
|
Variocele
|
Dilated veins in pampiniform plexus due to increased venous pressure; most common cause of scrotal enlargement in adult males. "Bag of worms" appearance, dx by US.
Most often on left side because of increased resistance to flow from left spermatic vein drainage into the left renal vein. Can cause infertility. Tx: variocelectomy, embolization. |
|
|
Testicular Germ Cell Tumors
|
95% of all testicular tumors; most often malignant; can present as mixed germ cell tumor.
DDx for testicular mass that does not transilluminate: cancer. |
|
|
Testicular Germ Cell Tumor:
Seminoma |
Malignant; painless, homogenous testicular enlargement; most common testicular tumor mostly affecting males 15-35.
Large cells in lobules with watery cytoplasm an a "fried egg" appearance. Radiosensitive. Late metastasis, excellent prognosis. |
|
|
Testicular Germ Cell Tumor:
Embryonal Carcinoma |
Malignant; painful; worse prognosis that seminoma.
Often glandular/papillary morphology. "Pure" embryonal carcinoma is rare; most commonly mixed with other tumor types. May be associated with increased hCG and normal AFP when pure (AFP increased when mixed). |
|
|
Testicular Germ Cell Tumor:
Yolk Sac Tumor (Endodermal Sac) |
Yellow, mucinous. Schiller-Duval bodies resemble primitive glomeruli.
Increased AFP. |
|
|
Testicular Germ Cell Tumor:
Choriocarcinoma |
Malignant with increased hCG; disordered syncytiotrophoblastic and cytotrophoblastic elements.
Hematogenous metastases to lungs; may produce gynecomastia because hCG is a LH analog. |
|
|
Testicular Germ Cell Tumor:
Teratoma |
Mature teratoma in males in malignant.
Increased hCG and/or AFP in 50% of cases. |
|
|
Testicular Non-Germ Cell Tumor:
Leydig Cell |
Contains Reinke crystals; usually androgen producing, gynecomastia in men; precocious puberty in boys; golden brown color.
|
|
|
Testicular Non-Germ Cell Tumor:
Sertoli Cell |
Androblastoma from sex cord stroma.
|
|
|
Testicular Non-Germ Cell Tumor:
Testicular Lymphoma |
Most common testicular cancer in older men; not a primary cancer; arises from lymphoma metastases to testes.
|
|
|
Tunica Vaginalis Lesions
|
Lesions in the serous covering of tesis - presents as testicular mass that can be transilluminated.
1. Hydrocele - increased fluid due to incomplete fusion of processus vaginalis. 2. Spermatocele - dilated epididymal tract. |
|
|
Penile Pathology:
SCC |
More common in Asia, Africa, and South America. Commonly associated with HPV, lack of circumcision.
|
|
|
Penile Pathology:
Peyronie's Disease |
Bent penis due to acquired fibrous tissue formation.
|
|
|
Penile Pathology:
Priapism |
Painful sustained erection not associated with sexual stimulation or desire.
Associated with trauma, sickle cell disease (block vascular channels), medications (anticoagulants, PDE5 inhibitors, antidepressants, alpha-blockers, cocaine). |

