![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
What are the 4-zone of the prostate that are clinically important?
|
Peripheral, cnetral, transitional, periurethral
|
|
|
What are the 2 major histologic components of the prostate?
|
Glands and stroma
|
|
|
Describe the two types of cells found in prostate glands
|
Secretory cells: columnar (face the lumen)… (2) Basal cells: low cuboidal(surrounded by basement membrane)
|
|
|
What is the stroma composed of? (hint: muscle)
|
Modified smooth muscle and dense fibrous muscle
|
|
|
Where is testosterone converted into DHT? What is the enzyme needed for the conversion? What is DHT?
|
Where is testosterone converted into DHT? Stromal cells of prostate… (2) What is the enzyme needed for the conversion? 5∂ reductase… (3) What is DHT? Most potent androgen, which promotes stromal and androgen growth
|
|
|
Name the 3-type of prostatitis
|
Acute bacterial, chronic & non-Bacterial, and Granulomatous prostatitis
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/postbiopsy/Allergic) Granulomatous, is associated mycobacteria, fungus and BCG?
|
Infectious Granulomatous Prostatitis is associated with mycobacteria, fungus and BCG
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/postbiopsy/Allergic) Granulomatous, is associated E.coli, other gram netative rods, Enterococci or staphylococci?
|
Acute Bacterial Prostatis and chronic bacterial prostatitis are associated with E.coli, other gram netative rods, Enterococci or staphylococci
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/postbiopsy/Allergic) Granulomatous, is associated wth inflamation, and infiltration of neutrophils, micorabscesses, and necrosis?
|
Acute Bacterial Prostatitis is associated with inflamation, and infiltration of neutrophils, micorabscesses, and necrosis?
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/Postbiopsy/Allergic) Granulomatous, is associated transurethral resection of prostate?
|
Postbiobsy granulomas are seen in pts with a hx of transurethral resection of prostate
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/postbiopsy/Allergic) Granulomatous, is associated recurrent infection due to harboring pathogens in the prostate?
|
Chronic Bacterial prostatitis is associated recurrent infection due to harboring pathogens in the prostate?
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/postbiopsy/Allergic) Granulomatous, is associated eosinophilia?
|
Allergic Granulomatous Prostatitis is associated with Eosinophilia (and granulomatous inflammation of other organs)
|
|
|
Which prostatitis, Acute bacterial, Chronic Bacterial&Non Bacterial, or (Infectious/Non-specific/postbiopsy/Allergic) Granulomatous, is associated urinary tract infections, inflammatory cells in prostate secretions, fever chills, dysuria, and tender boggy prostrate (w/DRE)
|
Actue bacterial prostatitis is associated urinary tract infections, inflammatory cells in prostate secretions, fever chills, dysuria, and tender boggy prostrate (w/DRE)
|
|
|
What is the cause of Non Bacterial prostatitis?
|
unknown
|
|
|
What is the cause of Non-specificGranulomatous?
|
unknown
|
|
|
Which is the most common Granulomatous prostatitis?
|
Non specific granulomatous prostatitis is most common
|
|
|
What ist he disease mechanism of BPH?
|
"Enlargement of the gland Both glandular and stromal involvement --> Leading to formation of nodules --> leading to Large nodules compress urethra → leading to partial/complete obstruction
|
|
|
What is the androgen involvement in BPH? What is the evidence for this?
|
" Androgens → ↑ growth… evidence: ↓ 5∂ reducase → ↓ conversion of T → DHT --> improves symptoms
|
|
|
What is the Estrogen involvement in BPH? (hint: give the mechanism)
|
"Estrogen also plays a role in BPH --> Aging men have ↑ E -->Increases androgen receptors -->↑sensitivity to DHT
|
|
|
What are the zones of involvement of BPH?
|
periurethral and transitional zones are involved in BPH
|
|
|
What is the nodular involvement in BPH?
|
"Nodular involvement: compression of surrounding tissue -->pseudocapsule… Urethral walls encroachment by nodules --> leading to obstruction
|
|
|
What is the general histology BPH? (hint, what is proliferating, glands or stroma?)
|
Proliferation of both the glands and the stroma of the prostate
|
|
|
In the UT obstruction seen with BPH, besides mechanical causes what else causes obstruction with BPH?
|
In BPH, besides mechanical obstruction due to the size of the prostate, there is a DYNAMIC INCREASE IN MUSCLE TONE
|
|
|
When are decreased bladder compliance, frequency, nocturia, and urgency seen in BPH
|
Decreased bladder compliance, frequency, nocturia, and urgency are seen in later progression of BPH
|
|
|
What are the 5 symptoms associated with BPH?
|
"↓caliber, ↓ force, Hesitancy, Dribbling, Incomplete emptying
|
|
|
Why are UTIs seen in BPH?
|
BPH --> urine retention --> UTI
|
|
|
What urinary tract sequelae arise from chronic obstruction due to BPH?
|
"In BPH with chronic obstruction: Hydroureter (enlargement)
|
|
|
What are the 3 medical Rx of BPH? And what effect do each have?
|
"Rx for BPH: (1) 5 –alpha-reductase inhibitor (finasteride) --> DHT inhibition → ↓ prostate growth… (2) LHRH analogs (leuprolide), transient LH release w/ long term effect... (3) ∂ adrenergic blocker (which relax smooth muscle)
|
|
|
Give 4 risk factors for adenocarcinoma of the prostate
|
Family history, Race, increased exposure to androgens, high fat diet
|
|
|
How much does having a first degree relative increase the risk to prostate cancer?
|
1° increases a persons risk of developing prostate cancer by 1.5-2.4
|
|
|
What effect does blocking androgens have on BPH and carcinoma of the prostrate?
|
Blocking androgens cause involution of BPH and carcinoma of the prostrate?
|
|
|
What diet lower one's risk, or raises one's risk, to prostate cancer?
|
What diet lower one's risk: Cereals..., raises one's risk, to prostate cancer? Animal fat
|
|
|
Which vitamin/minerals lower one's risk to prostate cancer?
|
Which vitamin/minerals lower one's risk to prostate cancer? Vitamin D, beta-carotene, and Vit-A
|
|
|
What is the sensitivity of a combination of DRE + TRUS in detecting prostate cancer?
|
A combination of DRE + TRUS detects prostate cancer in only 1/3 of all cases.
|
|
|
Which of the following is incorrect about BPH? Common > 50 y/o… risk increases w/ age… Not always clinical symptoms... increased risk of cancer
|
BPH causes no increased risk of cancer
|
|
|
"Which does the following description describe better, the BPH prostate glands or stroma: Fibroblastic/smooth muscle, Small blood vessels, and Myxoid (mucus-like) matrix… or Epithelial tufting & papillary projections into lumen
" |
With BPH, the composition of the stroma during BPH is composed of Fibroblastic/smooth muscle, Small blood vessels, and Myxoid (mucus-like) matrix… AND: the glands: have epithelial tufting & papillary projections into lumen
|
|
|
What are the 3 medical Rx of BPH? And what effect do each have?
|
"Rx for BPH: (1) 5 –alpha-reductase inhibitor (finasteride) --> DHT inhibition → ↓ prostate growth… (2) LHRH analogs:
--> Cause transient release of LH → exerts long-term effects (3) ∂ adrenergic blockers --> relaxes sm muscle " |
|
|
Left Grade 1:
➢ Well-circumscribed ➢ Glands: compact regular & medium sized Right: Grade 2: ➢ slightly infiltrated border and ➢ Glands: less regular & less compact, various sizes) |
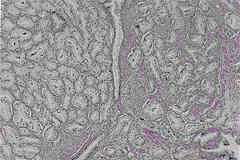
Name the Gleason Pattern Grade (1-5) for the left side and right sides of this image (note, they are different grades)
|
|
|
Gleason Grade 3:
➢ Infiltrating the stroma & between benign glands ➢ Glands: various shapes & sizes, w/ lumen & they are discrete (not fused) |
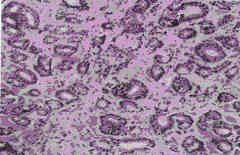
Name the Gleason Pattern Grade (1-5) for this image.
|
|
|
Gleason Pattern Grade 5
➢ Solid nests OR individual turmor cells ➢ No glandular formation |
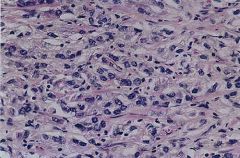
Name the Gleason Pattern Grade (1-5) for this image.
|
|
|
Gleason Pattern Grade 4:
➢ Infiltrating like pattern 3 ➢ Glands: less formed, fused and anastamosed |
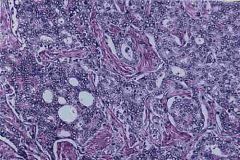
Name the Gleason Pattern Grade (1-5) for this image.
|
|
|
What is TRUS?
|
TRUS is transrectal ultrasonography used to detect prostate cancer
|
|
|
Give the ranges of PSA and what the ramification for these levels:
|
Give the ranges of PSA and what the ramification for these levels: Normal <4 ng/mL… 4-10 ng/mL = 25-35% probablility of prostate carcinoma… >10 ng/mL = 42-64% probability of prostate carcinoma
|
|
|
What percentage of PSA survey (where measurement are <4 ng/mL) is a false negative?
|
What percentage of PSA survey (where measurement are <4 ng/mL) is a false negative? 30% are false negative === not great sensitivity
|
|
|
What does PSA bind to ?
|
PSA binds ∂-antichymotrypsin in the plasma
|
|
|
Which gives greater specificity to prostate cancer, ↑bound PSA w/ ↓ free form → ↑ specificity or ↓bound PSA w/ ↑ free form → ↑ specificity
|
↑bound PSA w/ ↓ free form → ↑ specificity to prostate cancer… which really just means that ↓ free form = improved specificity (greater likelihood of prostate cancer and not a false positive)
|
|
|
If DRE, TRUS and PSA all test positive for prostate cancer, how do you confirm it?
|
After (+) DRE, TRUS, and PSA --> Confirmation: transrectal needle biopsy
|
|
|
Describe the glands in adenocarcinoma of the prostate: size, general description of gland it self, luminal cells, basal cells, nuclei, nucleoli.
|
Describe the glands in adenocarcinoma of the prostate: size=SMALL-MEDIUM, general description of gland it self=COMPACT, luminal cells: SINGLE LAYER OF CUBOIDAL/LOW COLUMNAR, basal cells=NO BASAL CELLS, nuclei=LARGE+CLUMPY, nucleoli=PROMINENT.
|
|
|
What does perineural invasion indicate?
|
In the prostate, perineural infiltration is common in adenocarcinoma and helpful in dagnosis
|
|
|
In diagnosis of prostate cancer, what pathology is seen at low and high magnification?
|
Low: small - intermediate sized tumor, decreased stroma, infiltration… HIGH: loss of basal cells, large/clumpy nuclei, prominent nuclei
|
|
|
What happens to the basal cells in adenocarcinoma of the prostate?
|
the end up looking like luminal cells, thus it appears like the basal cells are absent.
|
|
|
what is meant by infiltration in adenomacarcinoma of the prostrate?
|
Infiltration = large sheets of tumor cells near benign glands of the prostate
|
|
|
Match the Gleason pattern with the following description: slighly infiltrated, glands less regular & less compact with various sizes
|
Gleason Pattern 2: slighly infiltrated, glands less regular & less compact with various sizes
|
|
|
"Match the Gleason pattern with the following description: Infiltrating like pattern 3, with Glands: less formed, fused and anastamosed
|
Gleason Pattern 4: infiltrating like pattern 3, but with Glands less formed, fused and anastamosed
|
|
|
"Match the Gleason pattern with the following description: Solid nests OR individual turmor cells… No glandular formation
|
Gleason Pattern 5: Solid nests OR individual turmor cells… No glandular formation
|
|
|
"Match the Gleason pattern with the following description: Well-circumscribed… w/ Glands: compact regular & medium sized
|
Gleason Pattern 1: Well-circumscribed… w/ Glands: compact regular & medium sized
|
|
|
"Match the Gleason pattern with the following description: Infiltrating the stroma & between benign glands, w/ Glands: arious shape & size, w/ lumen & are discrete
|
Gleason Pattern 3: Infiltration of the stroma & between benign glands, w/ Glands: arious shape & size, w/ lumen & are discrete
|
|
|
Give an example of Gleason Scoring using two scores of 3 and 4
|
Gleason score: 3+4=7/10
|
|
|
Which Gleason score has a better prognosis? High or low?
|
Low Gleason scores have a better prognosis
|
|
|
"Which of the following are true of PIN (prostatic intraepithelial neoplasm): precancerous lesion, most carcinomas develop from PINs, found in 80% of biopsied carcinomas, no nuclear crowding
|
Which of the following are true of PIN (prostatic intraepithelial neoplasm): frecancerous lesion, most carcinomas develop from PINs, found in 80% of biopsied carcinomas, no NUCLEAR CROWDING… FALSE, YES there is nuclear crowding
|
|
|
"Which of the following are true of PIN (prostatic intraepithelial neoplasm): heaped up epithelium lining ducts, doesn't lead to adenocarcinoma of the prostoate, no stromal invasion, no basal cells (no basal cells in invasive carcinoma)
|
Which of the following are true of PIN (prostatic intraepithelial neoplasm): heaped up epithelium lining ducts, doesn't lead to adenocarcinoma of the prostoate-FALSE MOST CARCINOMAS DO DEVELOP FROM PIN, no stromal invasion, no asal cells FALSE - THERE ARE BASAL CELLS with PIN(no basal cells in invasive carcinoma)
|
|
|
T/F PSA is only associate with prostate cancer, but is also seen in BPH.
|
TRUE
|
|
|
What are the 4 factors of staging for prostate cancer?
|
"1. Amount of prostate involvement (1 lobe vs 2 lobe)… 2. Confined to prostate… 3. Lymph node… 4. Metastasis
|
|
|
Match the following with the appropriate stage of prostatic adenocarcinoma (A,B,C,D): microscopic, not palpable, confined to prostate
|
Stage A: microscopic, not palpable, confined to prostate
|
|
|
Match the following with the appropriate stage of prostatic adenocarcinoma (A,B,C,D): palpable tumor, confined to prostate
|
Stage B: palpable tumor, confined to prostate
|
|
|
Match the following with the appropriate stage of prostatic adenocarcinoma (A,B,C,D): Lymph node of distant metastasis
|
Stage D: Lymph node of distant metastasis
|
|
|
Match the following with the appropriate stage of prostatic adenocarcinoma (A,B,C,D): Tumor extending beyond prostatic capsule
|
Stage C: Tumor extending beyond prostatic capsule
|
|
|
T/F: Radical prostatectomy is the gold standard for localized adenocarcinoma confined to prostate. What are the complication of Radical prostatectomy
|
True: Radical prostatectomy is the gold standard for localized adenocarcinoma confined to prostate. (2) What are the complication of Radical prostatectomy: incontinence and impotence
|
|
|
Is Radical prostatectomy with complete removal curative?
|
Radical prostatectomy with complete removal IS curative.
|
|
|
How is Radiation used in prostatic adenocarcinoma?
|
"How is Radiation used in prostatic adenocarcinoma? (1) Alternative to radical prostectomy… (2) Adjunct to radical prostectomy (for residual or aggressive dz)
|
|
|
What are the 5 approaches to Hormonal Rx?
|
Orchietomy (castration), Inhibit GnRH, Inhibit androgen synthesis, Inhibit androgen binding to androgen receptor, Inhibit 5∂-reductase
|
|
|
Name the 3 drugs used to inhibit GnRH.
|
"GnRH inhibitors: ➢ Estrogen, Leuporlide, LHRH analog
|
|
|
Why does hormone induced remission sometimes fail with hormone Rx?
|
Why does hormone induced remission sometimes fail with hormone Rx? Tumor ultimately progresses due to eventual emergence of testosterone insensitive clones.
|
|
|
In the past chemotherapy had been unsuccessful with prostatic adenocarcinoma, when is it used?
|
In the past chemotherapy had been unsuccessful with prostatic adenocarcinoma, when is it used? Chemo is used for hormonal refractile metastatic (hormonal resistant cancer)
|
|
|
In post-op surveilance, (1) does an increase in PSA indicate re-emergence of a tumor? (2) Which is a better prognosis, short or long interval for PSA rise after surgery. (3) which is a better prognosis, short or long doubling time for PSA?
|
In post-op surveilance, (1) does an increase in PSA indicate re-emergence of a tumor? NOT NECESSARILY CLINICALLY SIGNFICIANT... (2) Which is a better prognosis, short or long interval for PSA rise after surgery. LONG... (3) which is a better prognosis, short or long doubling time for PSA? LONG
|

