![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Pt. with a seizure could have which two types of salt and water disorder?
A. Hypernatremia with hypervolemia B. Hypernatremia w/ hypervolemia C. Hypernatremia with euvolemia D. Hypernatremia with hypovolemia E. Hypertonic hyponatremia F. Isotonic hyponatremia G. Hypotonic hyponatremia |
A. Hypernatremia with hypervolemia
G. Hypotonic hyponatremia |
|
|
What is the equation to find out plasma osmolality?
|
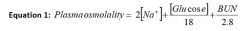
Remember, find plasma osmolality in cases of hyponatremia. This will help you determine what type of tonicity hyponatremia you have- hypertonic hyponatremia, isotonic hyponatremia/pseudohyponatremia, hypotonic hyponatremia (and if hypotonic hyponatremia, then w/ increased, decreased or near normal ECF volume)
|
|
|
1. This form of water-salt disorder is dependent on the method used to measure sodium. There is a problem with how the serum sodium concentration is reported in the presence of large amounts of proteins (Multiple Myeloma) or lipids (familial hyperlipidemias). In these circumstances, the sodium concentration is normal but lab reports it as being low. The true serum osmolality is normal.
A. hypertonic hyponatremia B. isotonic hyponatremia C. hypotonic hyponatremia w/ ECF volume expansion D. hypotonic hyponatremia w/ ECF volume depletion hypotonic hyponatremia w/ ECF normal volume E. hypernatremia with hypervolemia F. hypernatrmia with hypovolemia |
B. isotonic hyponatremia
aka "pseudohyponatremia" |
|
|
In isotonic hyponatremia
(aka "pseudohyponatremia), what are the two common conditions involved? |
*multiple myeloma (large amount of proteins in blood)
*familial hyperlipidemia (large amount of lipids in blood) *this form of hyponatremia is dependent on the method used to measure sodium. There is a problem with how the serum sodium concentration si reported in the presence of large amounts of proteins (Multiple Myeloma) or lipids (familial hyperlipidemias). In these circumstances, teh sodium concnetration is normal but lab reports it as being low. The true serum osmolality is normal so you can rule out "true" hyponatremia. |
|
|
Hyperglycemia is most common cause of this type of hyponatremia.
A. Hypertonic hyponatremia B. Isotonic hyponatremia C. hypotonic hyponatremia w/ volume expansion D. hypertonic hyponatremia w/ volume depletion E. hypertonic hyponatremia w/ normal volume |
A. Hypertonic hyponatremia
|
|
|
In all cases of [ hypernatremia / hyponatremia ] :
*in ALL cases, you must restrict water intake, correct hormonal deficiencies, stop drugs that contribute to hyponatremia (thiazides, for ex.) *if correcting, do not correct Na level at a rate of more than 1 mEq/L/hr! |
hyponatremia
|
|
|
True or False:
True hypotonic hyponatremia is always associated with ingestion or administration of water. |
TRUE!
*hyponatremia does not always equal hypotonicity, but hypotonicity is always associated with hyponatremia! |
|
|
Name possible clinical findings with ECF volume overload. (5)
Name some possible laboratory findings with ECF volume overload. |
CLINICAL:
*edema *pulmonary edema *ascites * +/- HTN (depends on etiol) *can also see JV distension, hepatogugular reflex or hear an S3 gallop LAB: *Prerenal Azotemia might be present(BUN:creatinine ratio > 20:1) * urine electrolytes show low sodium ( <10 mEq/L) and high osmolality (cuz both sodium and water are all being reabsorbed!) But in renal failure, urine sodium will be HIGH. Examples: 1) CHF: decreased EBAV, increased RAAS, increased sympathetic NS, increase ADH secretion => ECF volume overload 2) Nephrotic syndrome- glomerular disease resulting in massive protein leakage into urine. The diseased kidney does not excrete sodium and water normally. 3) Hepatic Chirrosis - three conditions. Primary sodium retention (something produced by liver just causes retention of salt and water by kidney), systemic vasodilation (unknown reason, but think due to nitric oxide. Vasodilation decreases EABV, stimulating RAAS, SNS and ADH thus causing wate and sodium retention in kidney), hypoalbuminemia (failure to synth albumin by diseased liver) 4) Renal failure: too much salt and water and not enough exreted because kidney is not filtering and excreting it. 5) hyperaldosteronism: will learn more about in endocrine. |
|
|
But in renal failure, urine sodium will be [ low / high ].
|
High
|
|
|
Name some clinical conditions with which you can find ECF volume overload.
|
1) CHF: decreased EBAV, increased RAAS, increased sympathetic NS, increase ADH secretion => ECF volume overload
2) Nephrotic syndrome- glomerular disease resulting in massive protein leakage into urine. The diseased kidney does not excrete sodium and water normally. 3) Hepatic Chirrosis - three conditions. Primary sodium retention (something produced by liver just causes retention of salt and water by kidney), systemic vasodilation (unknown reason, but think due to nitric oxide. Vasodilation decreases EABV, stimulating RAAS, SNS and ADH thus causing wate and sodium retention in kidney), hypoalbuminemia (failure to synth albumin by diseased liver) 4) Renal failure: too much salt and water and not enough exreted because kidney is not filtering and excreting it. 5) hyperaldosteronism: will learn more about in endocrine. Treatment: 1) CHF: dietary sodium restriction, diuretics, Inotropic agent (digoxin), decrease afterload (vasodilators, esp ACEi) 2) Nephrotic syndrome: dietary sodium restriction, diuretics, treat underlying disorder, ACEi 3) Hepatic Chirrosis: dietary sdium restriciton, diuretics 4) Renal Failure: Dietary sodium restriction, diuretics, dualysis 5) Hyperaldosteronism: will learn more about in endocrine |
|
|
Name possible clinical findings with decreased ECF volume. (4)
Name some possible laboratory findings with decreased ECF volume. |
CLINICAL FINDINGS:
* Hypotension *tachycardia *poor skin turgor *dry mucous membranes LABORATORY FINDINGS: *Prerenal Azotemia almost always present *Serum sodium might be low, normal or increased, depending on water homeostasis *urine electrolytes: values depend on source of loss of sodium and water. Renal Losses : urinary sodium > 20 mEq/L ; Extrarenal losses urine sodium < 10 mEq/L . |
|
|
With decreased ECF volume, Renal Losses : urinary sodium _____ mEq/L ; Extrarenal losses urine sodium ____ mEq/L .
|
With decreased ECF volume, Renal Losses : urinary sodium > 20 mEq/L ; Extrarenal losses urine sodium < 10 mEq/L .
|
|
|
With decreased ECF volume, there are renal losses and extrarenal lossess. Detail em.
|
1) Renal losses - three mechs. Primary salt wasting- diseased kidney cannot conserve sodium, aldosterone deficiency, secondary due to admin of drugs like diuretics or osmotic diuresis (glycosuria, contrast agents)
2) Extrarenal losses: GI Losses (diarrhea, vomiting), cutaneous (burns, sweat), sequestration of fluid or blood loss (fluid trapped in "3rd space" like peritoneum or pleural cavities. Ex. is in pancreatitis, intestinal obstruction or crush injuries to limbs) Treatment: 1) Renal losses: Replace volume deficit with normal saline 2) Extrarenal losses: Replace volume deficit with normal saline and replace blood loss. |
|
|
Which water-salt condition is due to ineffective osmoles like alcohol and urea being present?
|
Hyperosmolar states without hypertonicity.
Urea and alcohol are *these are ineffective osmoles, meaning they are substances which cross cell membranes readily and therefore do not exert osmotic pressure effects. |
|
|
Hyperglycemic hyperosmolar non-ketotic coma in Type 2 Diabetes Mellitus is associated with ONE water-salt condition. Name it.
|
Hypertonicity and hyperosmolarity without hypernaturemia.
*basically, there are signs of decreased ECF volume, decreased ICF volume due to shift of water from ICF to ECF b/c of high [glucose], and osmotic diuresis |
|
|
The following are possible clinical findings of [ hypernatremia / hyponatremia ].
*lethargy *increased muscle tone *coma *long-term CNS deficits can occur including subdural hemorrhage and diffuse vascular lesionsin the brain |
hypernatremia
*if pt. is hypotensive or orthostatic, replete with normal saline until blood pressure corrects, then replace water deficit . Beware of overly rapid correction of hypernatremia as it can result in brain swelling, thus should not be corrected faster than 12 mEq/L oer day or 0.5 mEq/L/hr |
|
|
What are some possible clinical findings of hypernatremia?
|
*lethargy
*increased muscle tone *coma *long-term CNS deficits can occur including subdural hemorrhage and diffuse vascular lesionsin the brain *if pt. is hypotensive or orthostatic, replete with normal saline until blood pressure corrects, then replace water deficit . Beware of overly rapid correction of hypernatremia as it can result in brain swelling, thus should not be corrected faster than 12 mEq/L oer day or 0.5 mEq/L/hr |
|
|
True or False:
Hypernatremia is ALWAYS associated with hypertonicity. |
True
only develops if individual is unable to drink adequate amounts of water |
|
|
Hypernatremia with hypervolemia can be caused by...
|
basically, * due to addition of solute to the ECF
so, *salt poisoning in infants *near drowning in sea water *saline abortions treatment: *administer water intravenously with D5W, or po water *+/- diuretics depending on etiology of hypernatremia |
|
|
Hypernatremia with euvolemia is due to:
A. addition of solute to ECF B. "pure" water loss C. hypotonic fluid loss |
B. "pure" water loss
(No fluid lost from body is ever pure water, but in this category, the electrolytes lost are so small as to be clinically insignificant, but the water loss itself IS clinically significant!) Ex. * Renal losses as in diabetes insipidous (central or nephrogenic) *Nonrenal losses as in "insensible losses" like through sweat/small burns, tachypnea |
|
|
Hypernatremia with hypovolemia is due to:
A. addition of solute to ECF B. "pure" water loss C. hypotonic fluid loss |
C. hypotonic fluid loss. In these patients, both solute (NaCl or NaHCO3) and water are lost, with greater loss of water.
Examples: *Renal losses - urine sodium is "high" ( > 20 mEq/L) as in osmotic diuresis like glycosuria, urea, mannitol. With diuretics, postobstructive renal failure. *GI losses - urine sodium is "low" (< 20 mEq/L) as in vomiting and diarrhea *other extrarenal -include sweating, osmotic diarrhea, fistulas or diarrhea associated with laxatives (from Salt and Water problem answer sheet) |
|
|
Match each with the correct salt-water condition.
1. hypernatremia with hypervolemia 2. hypernatremia with euvolemia 3. hypernatremia with hypovolemia A. due to "pure" water loss B. due to hypotonic fluid loss C. due to addition of solute in ECF |
1. C.
2. A. 3. B. |
|
|
[ Hypernatremia / Hyponatremia ] does not always equal [ hypertonicity / hypotonicity ], but [ hypertonicity / hypotonicity ] is always associated with [ Hypernatremia / Hyponatremia ] .
|
Hyponatremia does not always equal hypotonicity, but HYPOTONICITY IS ALWAYS ASSOCIATED WITH HYPONATREMIA!
*true hypotonic hyponatremia is always associated with ingestion or administration of water TREATMENT: in ALL cases, you must restrict water intake, correct hormonal deficiencies, stop drugs that contribute to hyponatremia (thiazides, for ex.) *if correcting, do not correct Na level at a rate of more than 1 mEq/L/hr! |
|
|
If correcting hypernatremia, do not correct at a rate of more than ________ mEq/L/hr ; if correcting hyponatremia, do not correct at a rate of more than _______ mEq/L/hr.
|
Hypernatremia: Beware of overly rapid correction of hypernatremia as it can result in brain swelling, thus should not be corrected faster than 12 mEq/L oer day or 0.5 mEq/L/hr.
Hyponatremia: do not correct Na level at a rate of more than 1 mEq/L/hr! |
|
|
Which salt-water condition does this describe?
*occurs when there is additional solute in blood which can exert an osmotic pressure (ex. Glucose, mannitol, glycerol). *hyperglycemia is most commmon cause of this type of salt-water condition |
hypertonic hypnatremia
*plasma osmolality is high though sodium is low due to dilution by "extra water" in ECF. *hyperglycemia is most commmon cause of this type of hyponatremia treatment: *treat underlying disorder (if hyperglycemic, give fluids, insulin. If toxicity do dialysis) |
|
|
What is pseudohyponatremia?
|
Also called isotonic hyponatremia, this form of hyponatremia is dependent on the method used to measure sodium. There is a problem with how the serum sodium concentration si reported in the presence of large amounts of proteins (Multiple Myeloma) or lipids (familial hyperlipidemias). In these circumstances, teh sodium concnetration is normal but lab reports it as being low. The true serum osmolality is normal so you can rule out "true" hyponatremia.
|
|
|
True or False:
Hypernatremia with increased ECF volume symptoms are primarily caused by swelling of brain cells in an encloesd space. Manifestations can be: HA, nausea/vomiting, abdominal cramping, muscle twitching. Confusion , seizures, coma and death possible if not treated. |
FALSE.
Though hypernatremia with increased ECF volume symptoms can also have seizures, these symptoms are more related to hypotonic hyponatremia. *plasma osmolality is low. (This category is ALWAYS associated with increased water intake.) |
|
|
Which salt-water condition does this describe?
*plasma osmolality is low. (This category is ALWAYS associated with increased water intake.) |
Hypotonic hyponatremia
*plasma osmolality is low. (This category is ALWAYS associated with increased water intake.) |
|
|
Etiology of this hypotonic hyponatremia condition include CHF, cirrhosis, nephrosis.
|
Hypotonic hyponatremia with increased ECF volume.
*there is increased total body sodium and water with greater increase in water *associated with decreased EABV, which thus stimulated salt and water retention in kidney. Must also be accompanied by increased water ingestion. |
|
|
Etiology of this hypotonic hyponatremia condition include Renal losses - urine sodium is "high" ( > 20 mEq/L) because disorder prevents the kidney from conserving sodium even when volume depleted. Extrarenal losses (urine sodium is < 20 because kidney responds to decreased volume by holding onto sodium and water): diarrhea, vomting, "third space" fluids, burns
|
Hypotonic hyponatremia with ECF volume depletion.
|
|
|
Etiology of this hypotonic hyponatremia include: *psychogenic polydipsia
*anterior pituitary insufficiency (cortisol required to turn off ADH secretion) *thiazide diuretics (remember, thiazides inhibit ability of kidney to dilute urine) *syndrome of inappropriate ADH secretion (SIADH) though this is usually a diagnosis of exclusion |
Hypotonic hyponatremia w/near normal total body sodium and near normal ECF volume
|
|
|
How do you approach problem solving with hyponatremia problems?
|
1) When you have a case of hyponatremia, you must first determine if the serum osmolality is reduced.
2) If it is, you must determine the volume status. If not, then you have hypertonic hyponatremia or pseudohyponatremia 3) Based on the status, what is the differential? |
|
|
What is the relative deistribution of fluid into the various body fluid compartments?
|
60% of our total weight is total body water. 40% ICF, 20% ECF. ECF breakdown is 5% plasma, 15% interstitial fluid
|
|
|
True or False:
Normal saline (0.9% NaCl in water) stays in ECF when administered whereas water and 5% dextrose is distributed to/among all TBW compartments. |
TRUE.
|
|
|
What is the difference in the distribution of normal saline, 5% dextrose and water among TBW?
|
Normal saline (0.9% NaCl in water) stays in ECF when administered whereas water and 5% dextrose is distributed to/among all TBW compartments.
|
|
|
What is the equation for plasma osmolality?
|

Alternatively, if glucose and BUN are normal, just multiply 2[Na].
|
|
|
How does both volume overload and volume depletion cause “prerenal azotemia”?
|
It depends on the cause of the volume change! Remember prerenal azotemia occurs whenever you decrease renal perfusion (renal blood flow). In heart failure, decreased cardiac output causes decreased renal blood flow. 25% of the cardiac output usually goes to the kidney. Decrease cardiac output and that really affects blood flow to the kidney. Decreased blood flow is ‘seen’ by the kidney as volume depletion so you see increased reabsorption from the proximal tubule. In cirrhosis, you have systemic vasodilatation –this decreases blood pressure. On top of that the renal arteries constrict (increased resistance) and this markedly decreases blood flow to the kidneys. So, again they think they need to increase volume to compensate
|
|
|
EABV is determined by what three things?
|
Remember EABV (BP is the best way of thinking of EABV) is determined by cardiac output, systemic vascular resistance and the actual volume. (The pump, the pipes and the fluid)
|
|
|
What are the three definitions for orthostatic hypotension?
|
systolic BP decrease by 15 ; diastolic BP decrease of 10;
increase in heart rate by 15 |
|
|
ADH is secreted in response to osmotic and volume stimuli. It is more sensititive to changes in _______, but changes in _______have a much more potent response.
|
ADH is secreted in response to osmotic and volume stimuli. It is more sensititive to changes in osmolality, but changes in volume have a much more potent response.
So that decreases in volume “over-ride” the response to osmotic stimuli. In other words if I am volume depleted and have a serum sodium of 120, I will not turn off ADH secretion until the volume is corrected. |
|
|
The two nonosmotic and nonvolume stimuli of ADH to remember from lecture are....
|
pain and nausea
There are others but Dr.D said just know these for now. |
|
|
Pain and nausea are two nonosmotic and nonvolume stimuli of ______.
|
ADH
|
|
|
True or False:
ADH release is inhibited by alcohol. |
TRUE.
This is why we become dehydrated when we drink alcohol –thus we get the headache, cotton mouth, etc. |
|
|
What are the differential diagnosis of polyuria?
|
1. Water diuresis (due to increased water ingestion or increased water excretion as in Diabetes Insipidus)
2. Solute diuresis (glucose, sodium, mannitol are most common) |
|
|
What are the causes of central diabetic insipidus? (5) And what is the treatment?
|
Causes of Central Diabetes Insipidus are:
Trauma, tumors, granulomas, vascular events, idiopathic, sporadic or hereditary |
|
|
What are some physical findings and lab findings for
A. volume overload B. volume depletion |
OVERLOAD: edema, ascities, increased jugular venous pressure, possible left ventricular failure (S3 gallop and pulmonary edema) ; hemodilution and prerenal azotemia.
DEPLETION: tachycardia, hypotension, low BP, dry axilla; hemoconcentration, prerenal azotemia, decreased urine Na concentration (in response to aldosterone) and increased urine osmolality (in response to ADH). |
|
|
[ Central DI / Nephrogenic DI ] is when you don't make ADH and thus water diuresis occurs whereas [ Central DI / Nephrogenic DI ] is when you just don't respond to ADH, even though it is present.
|
Central DI = don't make it (but can respond to it!)
Nephrogenic DI = don't respond to it |
|
|
What are the causes of Nephrogenic Diabetes Insipidus?
|
Hereditary : X-linked V2 receptor mutation, or autosomal recessive aquaporin defect.
Acquired: via lithium, hypercalcemia and severe hypokalemia. Urinary obstruction (Partial or post resolution). Treatment is very difficult and best we can do is give HCTZ which only helps a little. |
|
|
What test would you do to differentiate whether someone has Central DI or Nephrogenic DI?
|
Hallmark of Diabetes insipidus is dilute urine in the face of dehydration.
Water deprivation test can help differentiate between CDI and NDI. Before doing a water deprivation test, you MUST make sure that patient is euvolemic and has normal serum sodium concentration. Urine is monitored for 16 hours or 5% of lost body weight. Then ADH is administered and urine volume and osmolality are measured for another 2 hours afterwards. If urine osmolality increases and urine output decreases, patient has CDI. If urine output osmolality stays the same and urine volume remains high, patient has NDI. |
|
|
What are the urine electrolytes in someone with volume overload due to CHF, Nephrotic syndrome, Cirrhosis vs Renal Failure?
|
In CHF, Nephrotic syndrome and Cirrhosis, urine electrolytes show low sodium ( <10 mEq/L) and high osmolality (cuz it's all being reabsorbed!)
But in renal failure, urine sodium will be HIGH. |
|
|
What are some clinical examples of ECF volume overload?
|
1) CHF: decreased EBAV, increased RAAS, increased sympathetic NS, increase ADH secretion => ECF volume overload
2) Nephrotic syndrome- glomerular disease resulting in massive protein leakage into urine. The diseased kidney does not excrete sodium and water normally. 3) Hepatic Chirrosis - three conditions. Primary sodium retention (something produced by liver just causes retention of salt and water by kidney), systemic vasodilation (unknown reason, but think due to nitric oxide. Vasodilation decreases EABV, stimulating RAAS, SNS and ADH thus causing wate and sodium retention in kidney), hypoalbuminemia (failure to synth albumin by diseased liver) 4) Renal failure: too much salt and water and not enough exreted because kidney is not filtering and excreting it. 5) hyperaldosteronism: will learn more about in endocrine. |
|
|
What are the general causes of ECF volume depletion?
|
1) Renal losses - three mechs. Primary salt wasting- diseased kidney cannot conserve sodium, aldosterone deficiency, secondary due to admin of drugs like diuretics or osmotic diuresis (glycosuria, contrast agents)
2) Extrarenal losses: GI Losses (diarrhea, vomiting), cutaneous (burns, sweat), sequestration of fluid or blood loss (fluid trapped in "3rd space" like peritoneum or pleural cavities. Ex. is in pancreatitis, intestinal obstruction or crush injuries to limbs) Renal Losses : urinary sodium > 20 mEq/L ; Extrarenal losses urine sodium < 10 mEq/L . |
|
|
For treatment of hypernatremia, do not correct faster than ______mEq/L/hr ; for hyponatremia do not correct faster than ____ mEq/L/hr.
|
hypernatremia: 0.5 mEq/L/ hr decrease
hyponatremia: 1.0 mEq/L/hr increase |
|
|
What are the symptoms of hypernatremia and how do we treat it?
|
Symptoms of hypernatremia are lethargy, increased muscle tone, then coma. Long term CNS deficits can occur includign subdural hemorrhage and diffuse vascualr lesions in the brain.
Treatment is: If pt. is hypovolemic or orthostatic, replete with normal saline until BP corrects, then replace water deficit. Be sure to correct at max 0.5 mEq/L/hr or else brain swelling can occur. |
|
|
Headaches, nausea/vomiting, abdominal cramping, muscle twitching , confusion , seizures are symptoms of hyponatremia. What is treatment in general?
|
For all cases of hyponatremia- FLUID RESTRICT!
If [Na] <120 mEq/L OR pt symptomatic: correct with 3% saline If [Na] > 120 and volume depleted, just give saline If[Na] > 120 and SIADH, then fluid restrict, may give a vaptan or demeclocycline Never correct faster than 1 mEq/L/hr |
|
|
How do you approach problem solving for hyponatremia problems?
|
1. recognize hyponatremia state
2. calculate plasma osmolality - if normal then you have "pseudohyponatremia" where measuring methods are at fault (occurs in multiple myeloma or familial hyperlipidemia) - if elevated, then have more solutes in blood. Usually hyperglycemia, can be too much mannitol and glycerol too. - if hypotonic then... 3. detemine the volume status 4. figure out differential from there |
|
|
When you have hypertonic hyponatremia, the most common cause is _________ while other possible causes are ___________. How can you check to see if the hyponatremia is solely attributed to the most common cause?
|
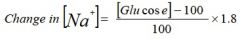
Most common cause: hyperglycemia. Other causes: mannitol and glycerol levels that are high. (Mannitol often given to decrease intracranial pressure; glycerol used during cystoscopic prostate surgery).
|
|
|
What is the equation to use to check if hyperglycemia is the only cause of a patient's hypertonic hyponatremia?
|
|
|
|
If you see a hypokalemic metabolic alkalosis with HTN , think of what disorder?
|
Some form of primary hyperaldosterone or renal artery stenosis!
|

