![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
109 Cards in this Set
- Front
- Back
|
what is the primary, general function of the kidney?
|
to keep the composition and volume of the blood plasma constant
|
|
|
what are the endocrine functions of the kidney?
|
secrete angiotensin and erythropoetin
|
|
|
give the break down of the % body weight that total fluid, intracellular fluid, and extracellualr fluid comprise?
|
60% = total fluid
40% = intracellular fluid 20% = extraceullar fluid |
|
|
what method can be used to directly measure the sizes of fluid compartments?
|
indicator-dilution technique
|
|
|
what is the formula used for indication-dilution technique to determine the volume of different compartments?
|
V = n/C
V=volume n=amount of indicator C=concentration of indicator |
|
|
indicators for measuring total body water include?
|
1. THO
2. D2O 3. Antipyrin |
|
|
indicators for measuring ECF include?
|
Inulin <--- most important
sucrose mannitol sulfate chloride sodium |
|
|
indicators used to measure plasma volume include?
|
1. Evan's blue
2. RISA-(I^131) 3. Cr^51-erythrocytes |
|
|
what type of indicator is optimum for measuring total body water?
|
one that acts the same as water and can enter all fluid compartments just like water
|
|
|
what type of indicator is optimum for measuring ECF?
|
one which is impermeable to cells (enters all areas but the intracellular fluid compartment)
|
|
|
what type of indicator is best for measuring ICF?
|
Trick!!! intracellular fluid cannot be measured directly
|
|
|
what type of indicator is best for measuring plasma volume?
|
one which is impermeable to vessel endothelium or which is bound to plasma proteins
|
|
|
what accounts for most of the ICF anions?
|
fixed negative charges on proteins and nucleic acids
|
|
|
what is the main source of anions in the ECF?
|
chloride
|
|
|
describe the osmolarity between the different fluid compartments?
|
largely the same between all compartments because most cells are very permeable to water
|
|
|
in which compartments would you find an large Na+ concentration?
|
ISF/Plasma
|
|
|
in which compartments would you find a large K+ concentration?
|
ICF
|
|
|
in which compartments would you find a large Cl- component?
|
ISF/Plasma
|
|
|
what is the general osmolarity between the fluid compartments?
|
~283
|
|
|
Pfill = ?
|
Pfill = (Pcap-Pisf) - (∏cap-∏isf)
|
|
|
what is the total body filtration rate, the total body absorption rate, and the lymph flow rate?
|
20, 18, 2 ml/min
|
|
|
how does nephrotic syndrome cause edema?
|
loss of proteins results increased oncotic pressure in the ISF causing filtered water to stay in the ISF.
|
|
|
what is the effect of adding purely water to plasma?
|
it dilutes into all fluid spaces and increases their volume in proportion to their original size (ISF get 1/3 of water added and ICF gets 2/3)
|
|
|
what happens when isotonic saline (9g/L) is added?
|
it Na+ cannot enter the ICF so water is only added to the ECF compartments - dilution of plasma proteins will cause much of the water to stay in the ISD
|
|
|
how can one insure that added volumes of fluid will not enter cells or the ISF, but will instead stay in the plasma fluid space?
|
add colloids which will increase the plasma oncotic pressure along with saline solution
|
|
|
in a 70 kg individual, total body water equals how many liters?
|
42
|
|
|
Name the major portions of the nephron starting from the glomeruli and ending collecting duct?
|
glomerulus -> proximal tubule -> loop of Henle -> distal tubule -> collecting ducts
|
|
|
what are the parts of the proximal tubule?
|
1. proximal convoluted tubule
2. proximal straight tubule |
|
|
what are the parts of the loop of Henle?
|
1. descending thin limb
2. ascending thin limb 3. ascending thick limb |
|
|
what are the parts of the distal tubule?
|
1. distal convoluted tubule
2. connecting tubule 3. initial cortical collecting duct |
|
|
what are the parts of the collecting duct?
|
cortical, inner medullary, outer medullary tubules
|
|
|
what is the surface area of the body including GI, lung, and genitourinary tract?
|
75 m^2
|
|
|
what percentage of the blood to to the kidney goes to the cortex?
|
93%
|
|
|
what keeps plasma proteins from exiting the the blood flow and entering the nephron?
|
negatively charge basal lamina repels the postively charge plasma proteins
|
|
|
what is allowed past the basal lamina?
|
things smaller than 3.5 nm and positively charged... or anything if it is small enough
|
|
|
of the 120ml per min. filtered into the nephron, how much is returned to the plasma in the tubules?
|
119 ml, meaning only about 1ml per min of urine is produced by the kidney each minute
|
|
|
what is the net filtration pressure in the glomeruli?
|
+9 mm Hg
|
|
|
of the 25% of blood flow entering the kidney how much is actually filtered?
|
20%
|
|
|
what is the equation for filtration fraction?
FF = ? |
FF = GFR / renal plasma flow
|
|
|
why does slowing renal blood flow actually increase filtration?
|
normally the blood is moving through faster than the cappilary hydrostatic pressure (Pc) can eqilibrate with the capillary oncotic (πc) and Bowmans space pressure (Pb) (Net filtration = Pc - (Pb + πc)
With slow flow, net filtration becomes zero because there is time to remove the maximum amount of fluid possible |
|
|
describe the effect of increasing efferent arteriolar resistance on GFR?
|
initially increases GFR then as RPF drops GFR drops off
|
|
|
what is the BP range in which GFR can remain relatively steady?
|
80-180 mmHg
|
|
|
what is the Bayliss relfex?
|
the arterioles in the kidney constrict when stretched (increased BP)
|
|
|
in addition to the stretch reflex in the kidney arterioles, ___ also controls renal perfusion?
|
macula densa
|
|
|
what causes the macula densa to want to reduce GFR?
|
increased Na+ osmolarity
|
|
|
why would the kidney want to produce renin when local control by the macula densa does not reduce distal tubule Na+?
|
renin increases aldosterone production causing increase Na+ reabsorbtion
There of course is the other compenent to renin release which is activation of Angiotensin system which will increase BP systemically |
|
|
what is the equation we need to use for solving the effects that different fixes have on the blood (adding more water, solutes, or saline)?
|
major concern is keeping added fluid out of the cells so to determine volumes in each compartment use the equation
(C fix)(V fix) = (V blood loss)(C blood loss) Then once the volume of a given compartment is found divide the blood loss volume/concentration by the fixed volume/concentration |
|
|
Using hydrolic conductivity (Lp), area (A), change in hydrostatic pressure (Delta P), and change in oncotic pressure (Delta π) how would you calculate GFR?
|
GFR = LP A (delat P – delta π) = Kfil x Pfil
|
|
|
how much filtrate is produced per minute in the kidney?
|
125 ml/min (180L per day)
|
|
|
how can GFR be calculated using Ucreatinine, Pcreatinine, and UFR?
|
GFR = (Ucreatinine/Pcreatinine) (UFR)
|
|
|
what is the formula for determining plasma solute excretion (Cx)?
|
Cx = (Ux/Px) (UFR)
in other words if x is completely filtered and niether secreted or reabsorbed, Cx = GFR |
|
|
how much of the filtrate is absorbed in the proximal tubule?
|
2/3
|
|
|
at the end of the proximal tubule, how much greater should the tubular fluid be than the plasma fluid?
|
1/3 aka 2/3 should have been absorbed
|
|
|
what is the osmotic gradient when comparing the renal tubule to the surrounding lateral space? What pressure difference does this translate into?
|
5-10 mOsM difference --> 100-200 mmHg driving pressure to take water out of tubule and deposit in lateral space
|
|
|
how does the kidney ensure that all the glucose is reabsorbed?
|
there are many Na+/Glucose and 2Na+/Glucose cotransporters
|
|
|
Draw the mechanism by which bicarb (HCO3-) is reabsorbed
|
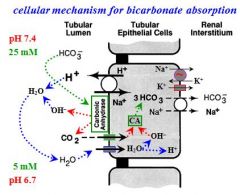
.
|
|
|
what percentage of HCO3- is reabsorbed?
|
93%
|
|
|
where does HCO3- reabsorbtion occur?
|
proximal tubule
|
|
|
what is the effect of renal diabetes mellitus?
|
reduces the maximum reabsorption capacity of the proximal tubule
|
|
|
what effect does parathyroid hormone have in phosphate absorption?
|
when it is present it results in the removal of Na+:PO4- cotransporter from the apical membrane increasing PO4- excreted in the urine
|
|
|
what is used to measure the maximum excretion possible for any solute?
|
PAH (maximally filtered and secreted, but none is absorbed)
|
|
|
is the amount of PAH excreted the same as that of the renal blood supply of PAH?
|
no, even though it is rapidly filtered and secreted, the total PAH availible for excretion is not totally excreted
|
|
|
what are the two types of nephrons and what distinguishes them from each other?
|
1. superficial nephrons - short loop of Henle, located upper/middle in cortex
2. juxtamedullary nephrons - long loop of Henle, located in lower cortex and loop extends deep into medulla |
|
|
what are the two types of cells located in the loop of Henle?
|
1. macula densa cells
2. intercalated cells |
|
|
where does furosemide work?
|
at the Na+:2Cl-:K+ in the intercalated cells of the thick ascending limb of the loop of Henle
|
|
|
how much of the tubular fluid is absorbed through the intercalated cells in the loop of Henle?
|
very little, there are no aquaporins
|
|
|
Describe solute absorption in the thick ascending limb?
|
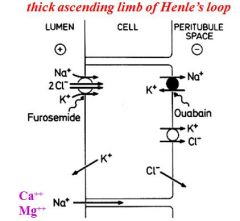
.
|
|
|
Draw solute exchange which occurs in cells of the early distal tubule
|
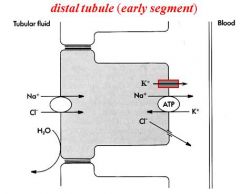
.
|
|
|
Draw solute exchange as it happens in the principle cells of the late distal tubule.
|
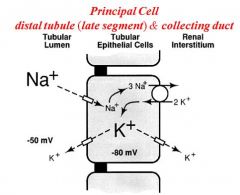
.
|
|
|
Draw the solute exchange which occurs in the Type A Intercalated cells of the late distal tubule?
|
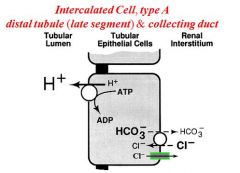
,
|
|
|
Draw the solute exchange which occurs in the Type B intercalated cells located in the late distal tubule?
|
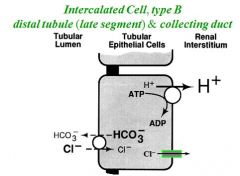
.
|
|
|
what stimulates water reabsorption in the principle cells of the late distal tubule?
|
Vasopressin causes aquaporins to be inserted into apical membrane
|
|
|
what is the normal water input?
|
2L
|
|
|
how does water leave the body? (3)
|
1. .1 L stool
2. .5 L insensible loss 3. 1.4 L in urine |
|
|
During maximum diuresis how much urine is produced per day?
|
17L
|
|
|
During maximum antidiuresis how much urine is produced per day?
|
.7L
|
|
|
what is the max diuresis per min? what is the min?
|
12 ml/min, .5ml/min
|
|
|
what is the osmolarity of urine during max diuresis? what about max antidiuresis?
|
50-60 mOsM, ~1200 mOsM
|
|
|
what causes the insertion of aquaporins in the principle cells of the late distal tubule and collecting ducts in response to water deprivation?
|
ADH
|
|
|
what are the 4 effects of ADH (vasopressin) on the production of urine?
|
1. increases apical membrane H2O permeability in late distal tubule and collecting duct
2. increases urea permeability for inner medullary collecting duct 3. stimulates NaCl absorption in TALH 4. increases blood flow to juxtamedullary glomeruli |
|
|
whats the thirst threshold in regards to plasma osmolarity?
|
294 (normal = 280-296)
|
|
|
if a person presents with high plasma osmolarity with low plasma ADH what is the underlying cause?
|
Lack of ADH release cause by diabetes insipidus
|
|
|
if a person presents with high plasma osmolarity with high plasma ADH what is the underlying cause?
|
Lack of V2 receptor or AQP2 in distal tubule and collecting ducts
|
|
|
how is osmolar clearence (Cosm) determined? (equation)
|
Cosm = (Uosm/Posm)(UFR)
|
|
|
how is the free water clearence (Cw^free) determined? (equation)
|
Cw^free = UFR-Cosm
|
|
|
what is the difference between Cosm during diuresis as compared to antidiuresis?
|
it is exactly the same because as UFR increases, the osmolarity of the urine drops and as UFR drops, the osmolarity increases
|
|
|
what percentage of the filtered load do the proximal tubule and the TALH reabsorb?
|
92%
|
|
|
what is a normal range for Cosm?
|
1.7-7.0 ml/min
|
|
|
what causes the production of ADH?
|
1. decrease ECF volume
2. increased plasma K+ concentration |
|
|
describe the two actions of angiotensin II?
|
1. immediate vasoconstriction
2. later increases in ADH production |
|
|
if Na+ levels are increased and there is volume expansion, what is released and what is the result?
|
ANP is released causing decreased Na+ absorption in the distal tubule = increases Na+ excretion and reduces volume
|
|
|
if the macula densa senses long term NaCl what happens?
|
it increases renin excretion
|
|
|
hyperkalemia stimulates the release of this hormone which in turn causes what effects?
|
Aldosterone causes increased K+ secretion from distal tubules
|
|
|
what is the normal percentage of filtered K+ excreted every day?
|
40% (300 mmol/day
|
|
|
under the effects of aldosterone, how much K+ can be secreted every day?
|
up to 200% of the filtered load
|
|
|
in hyokalemic states, how much K+ will be absorbed?
|
all but 1%
|
|
|
draw an intercalated cell in regards to K+ absorption?
|
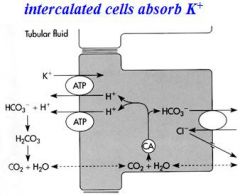
.
|
|
|
what are the 3 types of diuresis?
|
1. water
2. osmotic 3. natriuretic |
|
|
what causes water diuresis?
|
lack of ADH
|
|
|
what causes osmotic diuresis?
|
diabete mellitus
|
|
|
what causes natriuresis?
|
inhibition of Na+ reabsorption
|
|
|
Where does this diuretic work?
Acetazolamide |
proximal tubule
|
|
|
Where does this diuretic work?
Furosemide |
TALH
|
|
|
Where does this diuretic work?
Thiazide |
distal tubule
|
|
|
Where does this diuretic work?
amiloride |
distal tubule and collecting duct
|
|
|
What is the mechanism of action for this diuretic?
Acetazolamide |
inhibits carbonic anhydrase thereby increasing the osmolarity and H2O excreted
|
|
|
What is the mechanism of action for this diuretic?
Furosemide |
inhibits Na+:K+:2Cl– : cotransporter reduces medullary gradient suppresses tubuloglomerular feedback
|
|
|
What is the mechanism of action for this diuretic?
Thiazide |
inhibits Na+:Cl– cotransporter
|
|
|
What is the mechanism of action for this diuretic?
amiloride |
inhibits Na+ channel (ENaC)
|

