![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
14 Cards in this Set
- Front
- Back
|
Immune-complex related
|
- Includes lupus, MPGN, post-infectious GN, IgA nephropathy
- Crescents often a poor prognostic indicator - Diagnosis requires demonstration of immune-complex deposits by IF and/or EM |
|
|
Pauci-immune
|
~90% of cases ANCA-positive
Few or no deposits by IF and EM a. P-ANCA (anti-myeloperoxidase) positive - Microscopic polyangiitis (MPA); arteritis seen on only ~ 10% of biopsies - Pauci-immune crescentic GN limited to the kidney - Wegener’s (more often C-ANCA positive, but not always) b. C-ANCA (anti-PR3) positive - Wegener’s - Microscopic polyangiitis (more often P-ANCA positive) - Renal-limited, pauci-immune crescentic GN (more often P-ANCA positive) |
|
|
Anti-GBM nephritis
|
- Autoantibodies to portion of type IV collagen α3 chain (“Goodpasture antigen”)
- Diagnosis requires linear IgG in glomerular capillaries by IF - Confirmed by ELISA using patient serum vs. Goodpasture antigen - No deposits by EM - Antibody can cross-react with pulmonary alveolar BM (“Goodpasture’s disease”) - ~ 20-30% of patients are also ANCA-positive - Least common of the 3 classes of crescentic GN |
|
|
Post-Infectious Glomerulonephritis
Clinical Histology IF EM |
Clinical
- Most often associated with group A, beta-hemolytic streptococcal infection - Typical presentation: nephritic syndrome 1-2 wk after recovery from pharyngitis - Gross hematuria (dark urine) often a presenting symptom. - Serum C3 often low - Prognosis for complete recovery is excellent in children - Small fraction of patients (mainly adults) will progress to ESRD Histology - Diffuse proliferative and exudative GN - Crescents may be present - if numerous a poor prognostic indicator Immunofluorescence - Granular IgG and C3 in glomerular capillary loops and mesangium - C3 persists longer than IgG during recovery phase EM - Subepithelial “humps” are characteristic - Subendothelial and mesangial deposits usually present |
|
|
IgA Nephropathy
Clinical Histology IF EM |
- World’s most common primary GN, but uncommon in African-Americans
- Often discovered as microscopic hematuria ± proteinuria on physical exam - May present as gross hematuria following URI - Up to 40-50% of patients will develop ESRD over 20 years - Proteinuria (>1g/day) and hypertension poor prognostic indicators - Etiology not known - No widely accepted treatment - Probably related to Henoch-Schönlein purpura Histology - Most often focal, mesangial proliferative GN - May be diffuse and/or crescentic; associated with worse prognosis - May look histologically normal; these patients have excellent prognosis Immunofluorescence - Granular IgA, C3 in mesangium ± capillary loops - IgG, IgM may be present, but less intense than IgA - Clq typically absent EM - Mesangial deposits - Subendothelial deposits in ~25% - may correlate with more severe histology |
|
|
Membranoproliferative Glomerulonephritis
|
- Relatively uncommon; forms other than type I extremely rare
- Presentation is typically mixed nephritic/nephrotic - Serum C3 usually low - Progression to ESRD common - High recurrence rate in renal transplants - Subset of patients have mixed cryoglobulinemia (hepatitis C positive) |
|
|
Membranoproliferative Glomerulonephritis (Type I)
Histology IF EM |
Histology
- Diffuse proliferative GN with hyperlobular glomeruli - “Double contours” or “tram-tracks” on PAS and silver stains - Intracapillary pseudothrombi with cryoglobulinemia Immunofluorescence - Granular IgG and C3, ± IgM, Clq in capillary loops and mesangium - Intracapillary pseudothrombi of cryoglobulinemic GN stain for IgG and IgM EM - Subendothelial and mesangial deposits with “duplication” of GBM |
|
|
Clinical Features of Nephrotic Syndrome
|
≥3.5 grams/day
+/- RBCs no RBC casts present often absent, but may be present (especially in FSGS) typically normal, but may be elevated (especially in FSGS) |
|
|
Pathologic finding of Nephrotic Syndrome and the diseases
|
Normal cellularity
Non-inflammatory Glomerulopathies. including: Membranous minimal change FSGS diabetic nephropathy amyloid |
|
|
Clinical Features of Nephritic Syndomes
|
present, but typically <3.5 grams/day
many RBCs often RBC casts often present often present usually elevated |
|
|
Pathologic findings in Nephritic syndromes and the diseases
|
hypercellular
Glomerulonephritis Diseases: post-infectious GN IgA nephropathy membranoproliferative GN lupus nephritis (diffuse/focal proliferative) ANCA-associated (pauci-immune) GN anti-GBM nephritis |
|
|
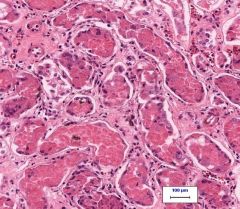
Coagulative tubular necrosis
|
|
|
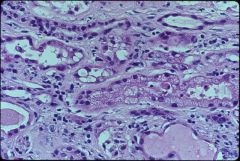
CALCINEURIN INHIBITOR TOXICITY - ISOMETRIC VACUOLIZATION
|
|
|
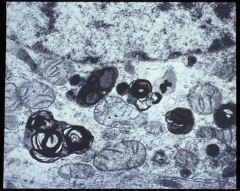
AMINOGLYCOSIDE TOXICITY - MYELOID BODIES
|

