![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
Basics: Renal blood 1.2L/min. (.2CO)
PCT - Resorbs Na, Cl, H2O, glucose, aa's, HCO3, K, HPO4, Ca, Mg. Loop - resorbs NaCl, regulates Mg DCT - some NaCl, regulates Ca. CT - Na/K exchange, H/K exchange, H2O resorbed (ADH). |
Renal tests - Creatinine CL approx. GFR. (small amount secreted in PCT so overestimates GFR). inaccurate when GFR <30%
BUN - aprox GFR, affected by GI, liver disease, hydration, reabsorbed in tubules (underestimates) BUN/Cr - >20 prerenal, 10-20 normal, <10 post renal. Calculations - (Urine vol * Urine Conc.) / (Plasma conc *1440min) Hint - SrCr x2 --- .5GFR |
|
|
Urinalysis
What can you learn from 1. Color 2. Clarity 3. Odor 4. pH 5. Protein 6. Glucose 7. Specific gravity 8. Billirubin/urobillogen 9. Nitrites 10. Leukocyte esterase 11. Ketones 12. Blood. |
1. nonspecific - drugs, bili, porphyrins, blood etc.
2. Cloudy - phosphates, WBC, dyes, bacteria. Milky - pyuria, lipids, lymph 3. Bacteria, asparagus, aa's. Tyrosine - rancid, Trimethylamine - fish, mayple syrup, methionine - cabbage, hops. 4. kidney function, normal = 6 acid/base status 5. measured by pH shift, + if 10mg/dL Trace - 150mg/day --- >7g/day 6, glucose oxidase reagent, peds pts test for other sugars. DM 7. GFRs osmolarity 285mOsm = sg 1.007 >1.010 concentrated. <1.007 hyposthenuric. 8. primarily conjugated - light sensitive and cannot be left standing. Urobili-readily detected, but light sensitive. 9. Indicates bacterial infection. take first thing in the morning (ammonia producing bac will give neg. result). 10. indicates bac infection of uppoer or lower UT. 11. Diabetic ketoacidosis. can be present normally in children with fever, diarrhea, adults on anesthesia, fasting, or malnourished. Unstable diabetics. 12. abnormal RBC numbers, glomerular damage, tumor, stone, ATN, infection. |
|
|
Azotemia - elevated BUN and Cr. prerenal (hypoperfusion), post renal (obstruction). Normal srcr is .5-1mg/dL
Oliguria - decreased urine production (dehydration, renal failure, hypovolemic shock, urinary obstruction.) Uremia - severe azotemia with clinical signs and sx. Toxic from renal disease and retention of urea in blood. weakness, headache, confusion, N/V, coma. |
Nephrotic syndrome - heavy proteinuria, hypoalbuminemia, edema, hyperlipidemia.
Nephritic syndrome - hematuria, HTN, ARF. Asx hematuria/proteinuria - mild glom. disease ARF - oliguria, anuria, and elevated BUN and Cr. UTI - bacteriuria, pyuria. Nephrolithiasis - rnals stones, pain, hematuria. |
|
|
Anatomy - Arteries - interlobar -- arcuate -- interlobular -- affarent -- glomeruli
Glomerulus - caps wall made up of - fenestrated endothelial cells, GBM, podocytes, mesangial cells, parietal epithelium (on urinary space). |
Pathogenesis of glomerular injury - immune mechanisms - anti GBM ab's. or deposition of immune complexes
|
|
|
Nephrotic syndrome
1. symptoms 2. pathophysiology 3. Causes |
Glomerular disease. Increased glomerular capillary permeability --- proteinurea. (no crescents) Primary - kidney only. Secondary - systemic, SLE, DM, etc.
1. Massive proteinurea >3.5g/day, Hypoalbuinemia ,3g/dL, Edema, Hyperlipidemia (increased production in liver, decreased catabolism. 2. Damage to glomerular capillary wall -- increased permeability -- proteins escape --- decreased albumin --- edema -- loss of OP 3.Causes - primary - membranous nephropathy, minimal change disease, focal segmental glomerulosclerosis, membranoproliferative Glomerulonephritis. Seconday - DM, SLE, Amyloidosis. |
|
|
Minimal Change Disease
1. Causes 2. Morphology 3. Course |
#1 cause of Nephrotic Syndrome in kids! Foot process effacement in glomerulus. Can follow respiratory infection or immunization. Big response to corticosteroids....unlike? (membranous nephropathy, FSGS)
2. Glomeruli look normal by LM, No immune deposits, lesion = visceral epithelial cells (podocytes) -- foot processes. Lipid casts in urine. Diagnostic - normal glomerulai w/ foot process effacement. (reverses with steroids) 3. Prognosis is EXCELLENT. >90% kids ok w/ corticosteroids. (Little Change in Little Kids) |
|
|
Focal Segmental Glomerulosclerosis (FSGS)
1. Types 2. Morphology IF EM 3. Course. |
Nephrotic syndrome. Sclerosis of some glomeruli (focal) only part of glomeruli involved (cap tuft). Capillaries destroyed.
1. Primary idiopathic. Secondary - HIV, obesity, HTN, edema, Hereditary (slit diaphragm genes nephrin, podocin). Common ins Black and Hispanic pop. 2. BM collapsed, hyalinosis. IF - nonspecific IgM, C3 deposits EM - Foot process effacement. W/HIV get collapsing variant where the whole tuft is sclerotic. (poor prognosis). 3. Prognosis is worse than in minimal change. Variable response to corticosteroids. Chronic in 50% of patients, and can progress to RF. Collapsing variant in 5-10% of HIV patients has a poor prognosis. |
|
|
Membranoproliferative Glomerulonephritis. (MPGN)
1. Causes 2. Morphology 3. Pathogenesis 4. Course |
Nephrotic syndrome. Altered BM, proliferation of glomerular cells, leukocyte infiltration. Variable presentation, NS or non-NS range proteinuria/hematuria, or nephrotic/nephritic w/ HTN, renal insufficiency.
1. Primary -idiopathic. Type I, Type II(dense deposit). Secondary - seen with chronic immune disorders - SLE, hepB/C, A1ATD, tumors, complement def. etc. 2. Type I - increased cellularity of glomerulus. Thick tram track BM. EM - subendothelium deposits. IF - granular C3/IgG in glom. BM and mesangium. Type II - dense deposit disease. EM- irregular ribbons of deposits in BM (links of sausage). IF - granular C3 (no IgG) 3. I. immune activates classical/alternative complement. II. alternative complement. 4. Slowly progresses. 50% ESRD in 10 years. no therapy. (MPGN train (on the tram tracks) full of immunocomp. people, and there's no stopping it). |
|
|
Membranous Nephropathy
1. Etiology 2. Morphology 3. Course |
#1 cause of Nephrotic Syndrome in adults. Thick glomerular capillary walls, accum. Ig in subepithelium and BM. Chronic Immune Complex mediated disease.
1. Primary idiopathic. Secondary - drugs, turmors, SLE, infections. 2. thick irregular deposits on subepithelium. *spikes* on BM. IF- granular Ig and complement. LM - uniform glom. cap thickening. 3. 1/3 remission. 1/3 stay proteinuric w/ no RF. 1/3 ESRD Does NOT respond to corticosteroids. |
|
|
Glomerulonephritis
|
Primary site is glomerulus. Inflammation.
Histo - glom. hypercellular -fibrinoid necrosis -glomerular crescents. -IF and EM deposits. Acute nephrotic syndrome - hematuria, azotemia (ARF), HTN, proteinuria and edema less than in nephrotic syndrome. Types - Acute Proliferative Glomerulonephritis (post strep/post infectious) Rapidly Progressive GN IgA nephropathy Chronic GN Also Alports and BFH |
|
|
Chronic Glomerulonephritis\
1. Morph 2. Course |
End stage glomerular disease caused by types of GN. Highest # of pts who progress to chronic GN from RPGN. Most idiopathic.
1. Reduced kidney size. Atrophic, diffuse, granular cortex. Advanced global glomerulosclerosis. >80% of glomerulus - hyaline obliteration. Beomes acellular mass of collagen. Eventual tubule atrophy. Interstitial fibrosis. Vessesls sclerotic - onion like. 2. Develops insidiousy over decades. ESRD, relentless progression if not maintained w/ dialysis or transplant will DIE. (big pink mess in glom.) |
|
|
Thin Basement Membrane Disease
(TBMD, Benign Familial Hematuria) 1. Presents... 2. Morphology 3. Pathogenesis - gene? |
Glomerulonephritis with uniformly thin BM. 1% of population.
1. normal renal function. Persistent microscopic hematuria. Inherited. Non progressive. Excellent prognosis. 2. EM - thin BM 150 - 250 nm (300-400 is normal) 3. COL4A3, COL4A4 mutation. Effecting alpha 3 or 4 chain of Type IV collagen. If Homozygous - autosomal recessive, Alport synrome ---RF |
|
|
IgA nephropathy
1. morphology 2. pathogenesis 3. course 4. predisposing conditions |
Most common glomerulonephritis in the world. frequent cause of hematuria, IgA in mesangium. isolated to kidney, henoch schonlein purpura.
1. mesangial widening, hypercellularity, can have segmental endocapillary proliferation. rarely cresenteric GN. IF - granular mesangial IgA. Some IgG, IgM, C3. EM - big thick mesangium cells next to caps. 2. Aggregates in mucosa, increased IgA trapped in mesangium. activates alternative complement pathway. 3. Presents with micro/gross hematuria, proteinuria, acute neph. syndrome. variable course - many normal renal function for years. 15-40% slow progression to RF. @ risk to progresss w/ age, increased prot., HTN, inc. glomerular sclerosis. May recur even after transplant. 4. Increased chances with sprue, liver disease, crohn's, sjrogens, GI cancer, leprosy. 15-30M, assoc with colds, native americans. |
|
|
Rapidly Progressive Glomerulonephritis (Crescenteric)
1. Types 2. Morphology EM, IF 3. Course |
Glomerulonephritis with severe Glomerular injury. Rapid Progressive loss of renal function -- end stage in wks. Classic - glomerular crescents, can cause kidney or systemic disease.
1. Types a. Anti-glomerular BM - linear IgG deposits (antiGBM abs) from alpha 3 chain IV collagen. can cause Goodpastures - pulm. hemmorhage form anti GBM Abs. in pulmonary alveolar BM. b. Immune complex mediated. RPGN. complication from another immune disease. IF - followe pattern of disease taht caused it (IgA, post. inf. GN, etc). c. Pauci immune GN - no IF deposits. Most have ANCA, can be renal only or systemic vasculitis. 2. Glomerular crescents - parietal cells w/ monos and macros. EM - ruptured GBM, allows prots, cells, etc in. Abs rupture BM, and crescents fill the urinary space 3. Rapid progression to renal failure, w/glomerulonephritis and hematuria, proteinuria, HTN. Treat with steroids, cytotoxic agetns. Goodpastures - hemoptysis, treat w/ plasma exchange and above. If CRF ---dialysis and transplant. |
|
|
Alport Syndrome
1. Types 2. Morphology 3. Course 4. Pathogenesis - gene |
Glomerulonephritis. Hereditary syndrome of isolated hematuria. - glomerular injury/hematuria -- CRF, bilaterally deaf, ocular lesions. X linked - 85% Females don't get RF. rare autosomal recessive/dominant
2. EM - irregular BM thickening and thinning. split lamination of lamina densa, "basket weave." 3. Hematuria, some have prot. MW/Xlinked --- RF. Sx at 5-20 y/o RF by 20-50. no treatment - ACE inhibitors for protein, transplant/dialysis. 4. Defective GBM synthesis from abnormal Type IV collagen (COL4A5 gene) X linked - mutation of alpha5 chain. Autosomal - Alpha 3 and 4. |
|
|
Systemic Lupus Erythematosus
1. Pathogenesis (genes?) 2. Morphology classes of injury 3. Course. systemic sx? renal sx? progression? |
Chronic multisystem autoimmune disease - affects skin, joints, kidney, serosal membranes.
1. 1 in 2,500. F:M 9:1, 20-30 y/o 2. Failure of self tolerance. Auto Abs. ANA, antidsDNA, antiSm are diagnostic. 3. Lupus nephritis in 50% - immune deposits. Wire loop lesions in LM in Gcaps. IF- IgG in mesangium 6 classes of injury - i. IF deposits. ii. Mesangial prolif. iii. focal glomerular proliferation. iv. diffuse glomerular prolif. v. membranous GN. vi. chronic GN 3. Present in young girl, malar rash, fever, pain in joints, pleuritic CP, photosensitivity. Renal involvement - hematuria, RBC casts, protinuria, NS. waxes and wanes. Treat with immunosuppressants and steroids. progression rare 90% 5 year survival. If die it's from RF or infectious cause. |
|
|
Diabetic glomerulosclerosis
1. Morphology 2. pathogenesis 3. Treatment |
Systemic disease, major cause of renal morbidity. Most common cause of ESRD. 30-40% pts progress to advanced or ESRD. Microalbuminuria (30-300mg/day) predictive of disease later in life.
Massive proteinuria, 10-20 yrs after diagnosis, heralds progressive chronic renal failure. 1. Diffuse mesangial sclerosis, nodular glomerulosclreosis *Kimmelstiel Wilson nodules* = hyaline nodes. Fibrin capsues - hyaline accumulates in capillary loops. IF- Linear IgG EM- GBM thickening, mesangial expansion, foot process effacement. 2. metabolic defect. hemodynamic changes. 3. no specific therapy, long term dialysis, transplant, but disease may reoccur in new kidney. Closely monitor glucose and ACE inhibitors may slow progression. |
|
|
Amyloidosis
1. what is amyloid? Types? 2. Clinical 3. Pathogenesis systemic/renal 4. Course |
Group of systemic diseases with amyloid deposits.
Amyloid is an amorphous eosin, hyaline extracellular substance. Congo red stain, or apple green bifringence to visualise. Non branching, random fibrils. 95% fibril, 5% p compoent/glycoproteins 2 types a. AL (light chain) from plasma cells, Ig light chains. AA - from SAA prot in liver, called secondary amyloidosis -assoc. with chronic inflammatory disorders 2. a.Systemic (primary) assoc with immunocyte dyscrasia. b. Secondary - complication of underlying inflamm process. c. Hemodialysis associated amyloidosis - pts on long term dialysis for RF. d. Familial - rare. 3. abnormal folding of proteins due to failed quality control mechanism. Renal - glomerular vascular and interstitial deposits of amyloid. congo red + and bifringence + 4. most serious/common form of organ involvement. renal --- Proteinuria -- NS Prognosis - systemic immunocyte derived amyloidosis = poor. AL = median survival 2 years. AA =better prognosis, may enter remission. |
|
|
Benign Nephrosclerosis
1. defintion, predisposing? 2. Morphology 3. Clinical features |
sclerosis of renal arterioles and small arteries -- thick walls/small lumens --- ischemia. Causes glomerulosclerosis and chronic tubular injury. HTN and DM increase incidence and severity.
2. normal/reduced size, grain leather cortex, narrow, small arteries. Hyaline arteriosclerosis, fibrointimal thickening, irr. parenchymal damage - patchy tubular atrophy, interstitial fibrosis, glomerular sclerosis. 3. causes minor renal impairment and proteinuria. African Americans, DM, or severe HTN are at risk for RF. |
|
|
Henoch Schonlein purpura
1. What? Who? Sx? 2. Morphology 3. Pathogenesis 4. Course |
purpuric skin lesions on arms, legs, and butt. Common in kids ages 3-8. Also in adults. Abdominal pain, vomit, GI bleed, nonmigratory athralgia. Renal - hematuria, and small %age have RPGN w/ crescents.
2. Identical to IgA nephropathy. *Mesangial* IgA immune deposits by IF. 3. Small vessel vasculiis w/ IgA deposits. Glomerular pathology. 4. Excellent prognosis unles crescents are present then = poor. |
|
|
Simple Cysts
1. Pathogenesis 2. Prognosis |
-found on autopsy. not clinically significant. Gross - simple epithelial lined space. Histo - flat, simple, epithelium.
1. scarring w/ isolation of tubular segments. Secretion into cysts -- cysts expand and pressure atrophy of adjacent parenchyma results. 2. excellent. usually not malignant. Must be differentiated from kidney tumor. |
|
|
Multicystic Renal Dysplasia
1. Pathology 2. Pathogenesis 3. Course |
Cysts. Asymptomatic. Most common abdominal mass in newborns. Not hereditary.
1. unilateral, large, irregular multicystic kidney w/ no normal parenchyma. Histo - cysts lined by flat nonspecific epithelium, weird structures - cartilage, mesenchyme, fat etc. Can have immature glomeruli but ducts are nondescript w/ undiff. mesenchyme "collar" 2. failure of uteric bud to fuse with metanephric blastoma. Similiar to obstruction during organogenesis. 3. Prognosis is excellent if unilateral. Bilateral - Incompatible with life. = potter's syndrome. Facial abnormalities, pulm hypoplasia from low amnio fluid (oligohydraminios) |
|
|
Malignant HTN
1. definition 2. morphology 3. clinical course |
Renal disease assoc with malignant of accelerated HTN. (5% of HTN pts). Characterized by BP >200/120, papilledema, retinal hemorrhages, encephalopathy, CV probs, RF.
2. Fibrinoid necrosis of arterioles (acute, eosino granular change in wall). Onion skinning of arteries and arterioles (intimal thickening from prolif smooth mm and collagen). 3. Emergency - immediate antiHTN therapy. 75% 5ysr, 50% restore RF. |
|
|
Hydronephrosis
1. cause? 2. Pathology |
Not a cystic disease, but in advanced stages, can be mistaken for cysts. Acute - painful but chronic can be Asx.
1. caused by lower GU obstruction. and various with diff. ages/sex 2. gross dilated renal pelvis and calyces w/ atrophy of renal parenchyma. |
|
|
Renal Artery Stenosis
1.Definition 2. Morphology 3. Pathogenesis 4. Clinical course |
1. unilateral, uncommon cause of HTN (2-5%). curable form of HTN with surgical management.
2. 2 types - a. occlusion by atheromatous plaque (70%) in old age, DM. b. fibromuscular dysplasia in 3rd/4th decade, fibrous thickening of vessel wall, can be bilateral. 3. constrict one artry -- HTN proportional to amount of constriction due to stim. of renin by JGA -- angiotensin II 4. arteriography to localize, can sometimes hear bruit, 70-80% cure rate w/ surgery. |
|
|
Thrombotic Microangiopathy (TMA)
1. Definition 2. morphology 3. pathogenesis |
pathological lesion affecting BV's, formation of thrombosis in caps and arterioles in various tissues. Caused by TTP, HUS, drugs, radiation, infections.
2. glomerular caps, small arteries/arterioles occluded by thrombi of platelet/fibrin aggregates. 3. 2 triggers. a. endothelial injury b. platelet activation/aggregation. In TTP, deficient ADAMTS13 allows vWf to accumulate and cause platelet agg. |
|
|
Atheroembolic renal disease
1. definition 2. morphology 3. clinical course |
1. fragments of atherometaus plaque from aorta or renal arteries dislodge and embolize intraparenchymal vessels. Seen in elderly with atherosclerosis, often after surgery or angiography.
2. emboli - rhomboid cholesterol clefts, in lumens and walls of small intraparenchymal renal vessels 3. ARF in elderly/t with dec. RF. |
|
|
Renal Infarcts
|
most due to embolism (thrombosis in LA or LV from MI. limited collateral circulation. Will be wedge shaped, base on the cortical surface and apex pointed at the medulla.
|
|
|
Urinary Tract Obstruction
1. Definition 2., Clinical Course |
Increases susceptibility to infection and stone formation. Unrelieved will lead to hydronephrosis. Can be sudden or insidious, partial or complete, uni or bilateral. Any level of UT from urethra to renal pelvis.
2. acute can cause pain, unilateral - hydronephrosis can be silent for long period, as unaffected kidney is maintaining RF. Bilateral - anuria, incomaptible with life unless relieved. |
|
|
Renal Adenoma
|
Benign tumor. Commonly found on autopsy.
histo - clear cell tumors. Look malignant but are <2.5 cm so rarely metastasize. (but do have some potential to do so) |
|
|
Urolithiasis (renal calculi, stones)
1. Definition 2. Cause and Pathogenesis 3. Morphology 4. Clinical Course |
renal stones, calculi. Stones may form at any level of UT but usually in kidney. 5-10% americans in lifetime, M more than F, peak age 20-30yrs. Hereditary predisposition. favored by low urine volume, and high constituent conc. (exceeds solubility)
2. Four types. a. calcium (70%) b. struvite or triple phosphate stones (15%) magnesium ammonium phosphate, in assoc with UTI especially Proteus. c. uric acid (5-10%). d. Cystine stones (1-2%) 2. Unilateral in 80% of cases. Most likely in renal calyces, pelvises. Staghorn calculi. 3. can obstruct urinary flow. Smaller are more dangerous (into ureters -- colic) Treat with extracorporeal shock wave lithotripsy, surgery, or pass on own with pain relief. |
|
|
Renal Cell Carcinoma
1. Presents 2. Pathology - types? genes? 3. Pathogenesis 3. Prognosis |
Neoplasm. = to clear cell cancer or hypernephroma. 1-3% of malignancies and 85% of renal cancers. 6/7th decade of life. common in smokers, obese, HTN etc.
1. Grows silently. Triad of costovertebral pain, mass, hematuria (10%). Mimics paraneoplastic syndromes - polycythemia, hypercalcemia, HTN, cushings, amyloidosis etc. 2. Clear cell carcinoma (80% loss of VHL). lots of metasteses. Papillary type - MET oncogene. Chromophobe type, collecting duct carcinoma type- very malignant. Gross large solitary, relow w/ hemorrhage, necrosis, and cystic changes. 3. Clear cell - inherited VHL gene (tumor suppressor on 3p.) - ubiuitin ligase complex triggers HIF-1 which senses low O2 and causes ^GF release and vascularity. (w/o this cells would prolif. uncontrollably in low O2 environment). Papillary - MET protooncogene - tyr. kinase receptor for hepatocyte growth factor. 4. Chromophobe type has good prognosis. Papillary and Clear cell types have poor prognoses. CD is highly malignant. Metasteses through veins and lymph go to liver, lung, bone, brain, lymph. 50% die w/in 5 years. Surgical exision. |
|
|
Acute Tubular Necrosis
1. Causes 2. Morphology 3. Clinical course |
Acute loss of renal function (loss of urine) w/ tubular injury. Most common cause of ARF. (50% of hospitalized pts).
1. ischemic - malig. HTN, HUS, TTP, DIC etc. Toxic injury, acute tubulointerstitial nephritis (hypersens. to drugs), obstruction 2. Tubule epithelial necrosis, loss of PCT brush border, thin epith., slough tubular cells into luman. can be w/ regeneration, interstitial edema, inflam cells, BM maintained. 3. reversible. supportive care and electrolyte balance. good prognosis. can be given temporary dialysis to increase urine output. |
|
|
Pyelonephritis
1. Pathogenesis @ risk? 2. Morphology - Acute 3. Clinical features 4. Chronic |
Follows UTI. Bacterial infection of kidney and pelvis causing suppurative inflammation. cause of interstitial nephritis. local inflamm. systemic - fever, leukocytosis, shock. Medullary pyramids show infectious processes.
1. E.coli most common, 2 routes. a. ascending infection w/own coliform bac. Colonize urethra and bladder, stasis and obstruciton allow to multiply ascend to pelvis and invade medulla by vesicouretal reflux. @risk w/ urethral obstruction, BPH, preggers. b. through bloodstream (hematogenous) from sepsis or endocarditis. 2. Neutros in lumens, bac, pus casts, abscesses. Acute - self limited - treat w/ antibiotics renal surface- gray white inflamm and abcess. neutrophil exudate in tubules and interstitium. 3. sudden onset, pain at costovert. angle. fever, malaise. dysuria, frequency, urgency, leukocytes/bac in urine. Course is usually benign. Treat with antibiotics. More serious w/DM, immunodef. --- sepsis/death 4. repeated renal inflamm and scarring ---scarred deformed kidneys. affects poles more. |
|
|
Acute drug induced interstitial nephritis
1. definition 2. morphology 3. clinical features |
adverse reaction to a large variety of drugs (most frequently antibiotics.diuretics, and NSAIDs.) 2 weeks after exposure and is characterized by fever, eosinophilia (vs. pyloneph with neutros), rash, and renal problems. Hematuria, mild proteinuria, ARF.
2. interstitial infiltration by mononuclear inflammatory cells. (lymphos and plasma cells.) clusters of eosinophils. 3. withdraw offending agent and recover with excellent prognosis. Slight interstitial fibrosis/tubular atrophy. Irr. damage, lose brush border, and progression to chronic disease can occur if agent is not removed. can cause ARF with ATN, trigger interstitial immune rxn, or subtle but cummulative injury to tules that will in years cause CRF. Tubulo Interstitial Disease Thyroidization Toxins TB |
|
|
Analgesic Nephropathy
|
Chronic renal disease form excessive intake of painkillers. Renal papillary necrosis. Pt. have ingested large quantities of atleast 2 antipyretic analgesics (ASA, acetaminophen, codeine).
2. renal papillae show gray/white/yellow necrosis of tips or 2/3 of the pyramids. Papillary necrosis also seen in DM, UTobstruction, and sickle cell |
|
|
Polyomavirus Nephropathy
|
Viral pathogen -- TIN in kidney transplants. Immunosuppression can cause reactivation of latent infection and development of nephropathy. Causes transplant to fail. Intranuclear viral particles in tubular epithelial cells.
|
|
|
Congenital Cystic Disease
Autosomal Dominant Polycystic Kidney Disease (ADPKD) 1. Pathogenesis (gene?) 2. Morphology 3. Course rule of 1/3rds 4. extrarenal anomalies |
Genetic disorder char. by multiple expanding cysts. Bilateral! Destroy parenchyma and cause failure. 5-10% transplants/dialysis. AD with high penetrance. 5th decade.
1. PKD-1 or polycystin 1 (85% cases), more likely to get cysts. RF 20 years earlier. Mechanoreceptor in tubular epith. cells. PKD2/polycystin 2 - put calcium channels into membrane to get Ca from ER. 2. Bilaterally big kidneys. external mass of cysts with no intervening parenchyma. filled with fluid. 3. Cysts at birth, Sx in 4th/5th decade of life. (later if PKD2). HTN and infection most common complication. Rule of 1/3rds - 1/3 die RF, 1/3 die CV disease and HTN complications, 1/3 die of unrelated causes. 4.1/2 polycystic liver disease. Some get berry aneurysms and subarachnoid hemorrhage. some cardiac valvular anomalies. MVP. - can cause liver, spleen, panc, lung cysts. Or aneurysms at the circle of willis -- subarachnoid hem, and death. "Bilateral, Big kidney, Berry aneurysms." *Differentiate from multilocular Renal cysts. |
|
|
Congenital Cystic Disease. Autosomal recessive polycystic kidney disease.
(ARPKD) 1. Pathogenesis gene? 2. Morphology 3.Course 3. Pathology |
most common inheritable cytic renal disease in childhood. Present at birth w/ big kidneys. (abdominal mass dystocia). Non functioning kidneys = Potters syndrome. If survive, develop congenital hepatic failure - die in adolescence. little cysts run parallell to cortex.
1. PKHD1 -chrom 6 protein fibrocystin associated with cilia of CD. 2. enlarged and have smooth external surface. numerous small cysts within give spongelike appearance. Liver usually also cystic. dilated channels perpendicular to cortex. retain reniform shape. 3. highly variable. perinatal death - mild progressive in adolesence. 4 groups - perinatal,neonatal, infantile, juvenile. |
|
|
Benign tumors of the kidney
1. Renal Papillary Adenoma 2. Angiomyolipoma 3. Oncocytoma |
1. small discrete tumor found on autopsy. In cortex, less than .5cm. Composed of comlex branched papillary structures.
2. benign growth of vessels, smooth mm. and fat. Associated with multi system genetic disease tuberous sclerosis. 3. Benign epith. tumor, can grow huge and need surgery. Composted of big eosino cells, with small nuclei, and lots of mitochondria. |
|
|
Renal Cell Carcinoma
1. Clinically 2. Pathology - types? genes? 3. Mophology 4. Prognosis |
Neoplasm. = to clear cell cancer or hypernephroma. 1-3% of malignancies and 85% of renal cancers. 6/7th decade of life. common in smokers, obese, HTN etc.VHL syndrome.
1. Grows silently. Triad of costovertebral pain, mass, hematuria (10%). Mimics paraneoplastic syndromes - polycythemia (erythro) or hyper calcemia, cushings etc. Metastasize widely before sx. Treat with nephrectomy. 2. a. Clear cell carcinoma (80%) loss of VHL. lots of metasteses. clear sheets of cells. b. Papillary type (10%), trisomy 7, 16, 17. loss of Y c. Chromophobe type -5%, pale eosino cells wth perinuclear halo. d. collecting duct carcinoma type- very malignant. rare. 3. Gross large solitary, at poles. yellow w/ hemorrhage. invades renal vein and can extend to R heart. 4. Chromophobe type has good prognosis. Papillary and Clear cell types have poor prognoses. CD is highly malignant. |
|
|
Urothelial carcinoma of renal pelvis
1. Presents 2. Pathogenesis 3. Prognosis |
5-10% renal tumors from urothelium or renal pelvis.
1. Old people. Smokers -- hematuria, obstruction, pain, mass, fever, malignant cells in urine. 2. "field effect" cuz all urothelium is exposed to the same pathogenic factors (seeding from single source?) Can have multiple primary tumors. (multifocal) and have tumors in ureter, pelvis, or bladder at once. 3. renal pelvis tumors tend to invade into sinus and have a poor prognosis. |
|
|
Wilm's Tumor (nephroblastoma)
1. Presents: 2. Pathogenesis, gene? 3. Pathology 4. Course/prognosis |
Neoplasm. Most common renal malignant tumor of children. Renal mass w/in 2 years of age (looks like developmental embryonic tumor.
1. Presents w/ mass(90%), HTN (69%), Anorhexia (10-15%) Constipation (5-10%) Hematuria (5-10%) Pulmonary Metasteses (25%) 2. WTI gene - transcription factor in developing kidney and tumor suppresssor. Assoc with renal genital syndromes - Denys Drash, WAGR (wilms, aniridia, genital anomalies, retardation) , Beckwith Wiedemann syndrome 3. Pathology - resembles early developing kidney, very well differentiated. large solitary mass. 10% bilateral or multicentric. 4. treated with chemo, rad, surgery combo has good response. 85% cure rate. Poor prognosis with age of onset >2 ,advanced stage, size, or anaplasia. |
|
|
Acquired (Dialysis Associated) Cystic Disease
|
kidney from pat with ESRD undergoing dialysis can get multiple cortical/medullary cysts. .5-2cm luid filled. Asx or hematuria. Complication - RCC in walls of cysts (5-10% dialyzed pts).
|
|
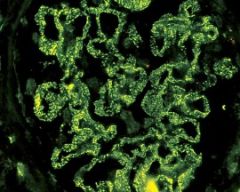
What type of immunofluorescence is this? What diseases is it characteristic of?
|
granular looks like specks of sand grains on glomerulus. Probably means mesangial/BM damage of some sort, or disruption of BM. – Found in all Nephrotic syndromes except minimal change (None)
1. Membranoproliferative Glomerulonephritis - IgG/C3 if type I. Just C3 if Type II. 2. Membranous Nephropathy – IgG/Complement. 3. Acute proliferative Glomerulonephritis – IgG/C3 found in post strep type. 4. Focal Segmental Glomerulosclerosis – IgM and sometimes C3 only in affected areas |
|
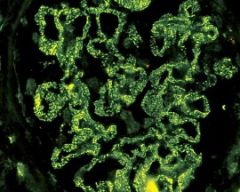
What type of Immunofluorescence, and what disease is it char. of?
|
Linear, characteristic of classic anti-GBM disease (E).
follows ribbon like path along capillary loops– means diseased BM and thickening/proliferation of cells. 1.. DM – IgG 2. Rapidly Progressive Crescenteric GN – AntiBM ab type, and goodpastures – IgG |
|
|
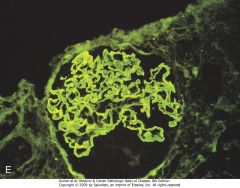
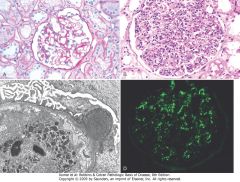
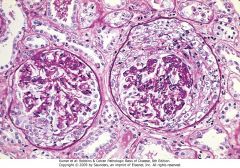
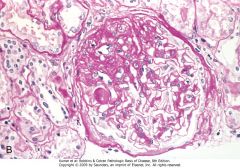
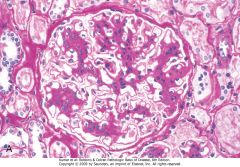
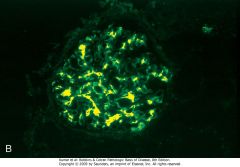
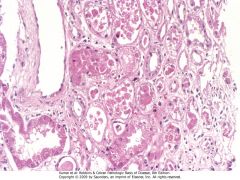
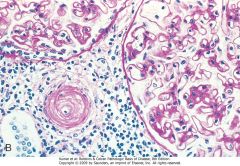
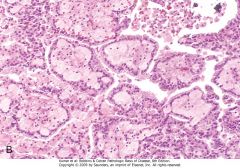
Acute proliferative glomerulonephritis. A, Normal glomerulus. B, Glomerular hypercellularity is due to intracapillary leukocytes and proliferation of intrinsic glomerular cells. C, Typical electron-dense subepithelial "hump" and a neutrophil in the lumen. D, Immunofluorescent stain demonstrates discrete, coarsly granular deposits of complement protein C3, corresponding to "humps" illustrated in part C
|
|
|
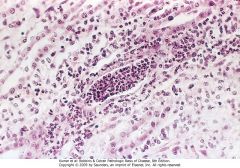
Crescentic glomerulonephritis (PAS stain). Note the collapsed glomerular tufts and the crescent-shaped mass of proliferating parietal epithelial cells and leukocytes internal to Bowman capsule.
|
|
|
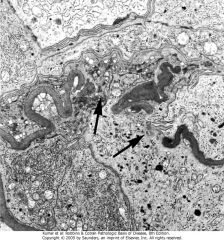
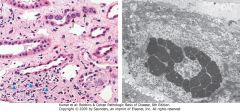
Crescentic glomerulonephritis. Electron micrograph showing characteristic wrinkling of GBM with focal disruptions
|
|
|
Focal segmental glomerulosclerosis, PAS stain. A, Low-power view showing segmental sclerosis in one of three glomeruli (at 3 o'clock).
|
|

|
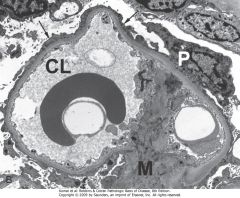
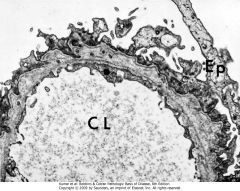
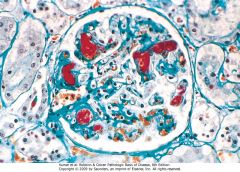
Membranous nephropathy. A, Silver methenamine stain. Note the marked diffuse thickening of the capillary walls without an increase in the number of cells. There are prominent "spikes" of silver-staining matrix (arrow) projecting from the basement membrane lamina densa toward the urinary space, which separate and surround deposited immune complexes that lack affinity for the silver stain. B, Electron micrograph showing electron-dense deposits (arrow) along the epithelial side of the basement membrane (B). Note the effacement of foot processes overlying deposits. CL, capillary lumen; End, endothelium; Ep, epithelium. C, Characteristic granular immunofluorescent deposits of IgG along GBM. D, Diagrammatic representation of membranous nephropathy
|
|
|
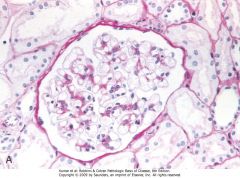
Minimal-change disease. A, Glomerulus stained with PAS. Note normal basement membranes and absence of proliferation.
|
|
|
B, Ultrastructural characteristics of minimal-change disease include effacement of foot processes (arrows) and absence of deposits. CL, capillary lumen; M, mesangium; P, podocyt
|
|
|
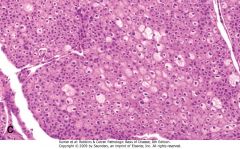
Focal segmental glomerulosclerosis, PAS stain. B, High-power view showing hyaline insudation and lipid (small vacuoles) in sclerotic area.
|
|
|
Collapsing glomerulopathy. Visible are retraction of the glomerular tuft, narrowing of capillary lumens, proliferation and swelling of visceral epithelial cells, and prominent accumulation of intracellular protein absorption droplets in the visceral epithelial cells. The appearance is identical in cases wherein the etiology is idiopathic to cases associated with HIV infection. Silver methenamine stain.
|
|
|
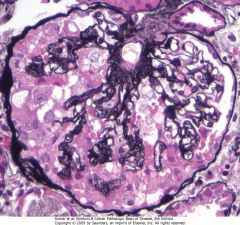
Membranoproliferative glomerulonephritis, showing mesangial cell proliferation, increased mesangial matrix (staining black with silver stain), basement membrane thickening with segmental splitting, accentuation of lobular architecture, swelling of cells lining peripheral capillaries, and influx of leukocytes (endocapillary proliferation).
|
|
|
IgA nephropathy. A, Light microscopy showing mesangial proliferation and matrix increase.
|
|
|
B, Characteristic deposition of IgA, principally in mesangial regions, detected by immunofluorescence.
|
|
|
Hereditary nephritis (Alport syndrome). Electron micrograph of glomerulus with irregular thickening of the basement membrane, lamination of the lamina densa, and foci of rarefaction. Such changes may be present in other diseases but are most pronounced and widespread in hereditary nephritis. CL, capillary lumen; Ep, epithelium.
|
|
|
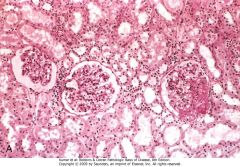
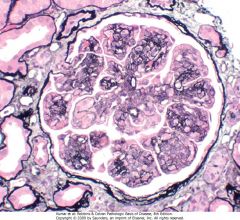
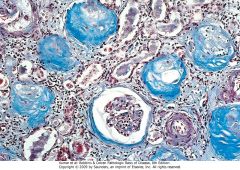
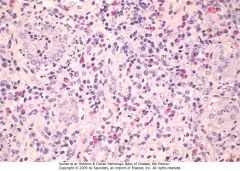
Chronic glomerulonephritis. A Masson trichrome preparation shows complete replacement of virtually all glomeruli by blue-staining collagen.
|
|
|
Acute kidney injury. Some of the tubular epithelial cells in the tubules are necrotic, and many have become detached (from their basement membranes) and been sloughed into the tubular lumens, whereas others are swollen, vacuolated, and regenerating.
|
|

|
Vesicoureteral reflux demonstrated by a voiding cystourethrogram. Dye injected into the bladder refluxes into both dilated ureters, filling the pelvis and calyces.
|
|

|
Acute pyelonephritis. Cortical surface shows grayish white areas of inflammation and abscess formation.
|
|
|
Acute pyelonephritis marked by an acute neutrophilic exudate within tubules and interstitial inflammation.
|
|
|
Polyomavirus nephropathy. A, The kidney shows enlarged tubular epithelial cells with nuclear inclusions (arrows) and interstitial inflammation (arrowheads). B, Intranuclear viral inclusions visualized by electron microscopy.
|
|

|
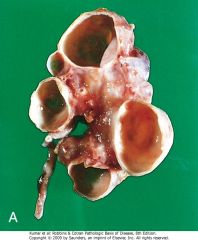
A, Chronic pyelonephritis. The surface (left) is irregularly scarred. The cut section (right) reveals characteristic dilation and blunting of calyces. The ureter is dilated and thickened, a finding that is consistent with chronic vesicoureteral reflux
|
|
|
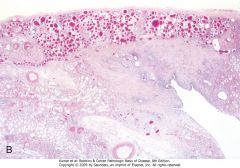
A, Chronic pyelonephritis. The surface (left) is irregularly scarred. The cut section (right) reveals characteristic dilation and blunting of calyces. The ureter is dilated and thickened, a finding that is consistent with chronic vesicoureteral reflux. B, Low-power view showing a corticomedullary renal scar with an underlying dilated deformed calyx. Note the thyroidization of tubules in the cortex.
|
|
|
Drug-induced interstitial nephritis, with prominent eosinophilic and mononuclear cell infiltrate
|
|

|
Analgesic nephropathy. A, The brownish necrotic papilla, transformed to a necrotic, structureless mass, fills the pelvis. B, Microscopic view. Note the fibrosis in the medulla.
|
|
|
Urate crystals in the renal medulla. Note the giant cells and fibrosis around the crystals.
|
|

|
Close-up of the gross appearance of the cortical surface in benign nephrosclerosis illustrating the fine, leathery granularity of the surface.
|
|
|
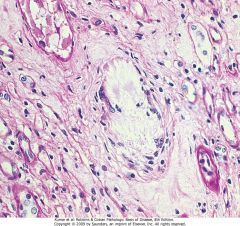
Hyaline arteriolosclerosis. High-power view of two arterioles with hyaline deposition, marked thickening of the walls, and a narrowed lumen.
|
|
|
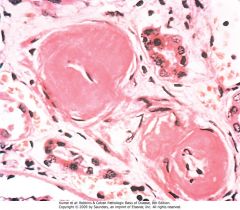
Malignant hypertension. A, Fibrinoid necrosis of afferent arteriole (PAS stain).
|
|
|
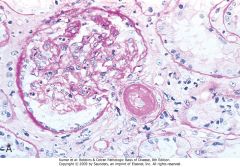
Malignant hypertension. B, Hyperplastic arteriolitis (onion-skin lesion).
|
|
|
Fibromuscular dysplasia of the renal artery, medial type (elastic tissue stain). The media shows marked fibrous thickening, and the lumen is stenotic.
|
|

|
Atheroemboli with typical cholesterol clefts in an interlobar artery.
|
|
|
Fibrin stain showing platelet-fibrin thrombi (red) in the glomerular capillaries, characteristic of thrombotic microangiopathic disorders.
|
|

|
Diffuse cortical necrosis. The pale ischemic necrotic areas are confined to the cortex and columns of Bertin.
|
|
|
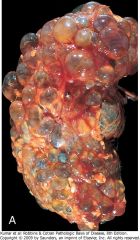
ulticystic renal dysplasia. A, Gross appearance.
|
|
|
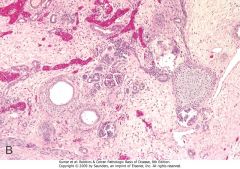
ulticystic renal dysplasia. B, Histologic section showing disorganized architecture, dilated tubules with cuffs of primitive stroma, and an island of cartilage (H&E stain).
|
|
|
A and B, Autosomal-dominant adult polycystic kidney disease (ADPKD) viewed from the external surface and bisected. The kidney is markedly enlarged and contains numerous dilated cysts.
|
|

|
A and B, Autosomal-dominant adult polycystic kidney disease (ADPKD) viewed from the external surface and bisected. The kidney is markedly enlarged and contains numerous dilated cysts.
|
|
|
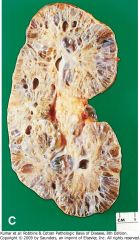
C, Autosomal-recessive childhood PKD, showing smaller cysts and dilated channels at right angles to the cortical surface.
|
|

|
D, Liver cysts in adult PKD.
|
|

|
Medullary cystic disease. Cut section of kidney showing cysts at the corticomedullary junction and in the medulla.
|
|

|
Hydronephrosis of the kidney, with marked dilation of the pelvis and calyces and thinning of the renal parenchyma.
|
|

|
Nephrolithiasis. A large stone impacted in the renal pelvis.
|
|

|
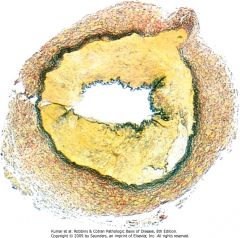
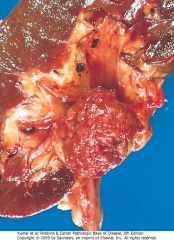
Renal cell carcinoma. Typical cross-section of yellowish, spherical neoplasm in one pole of the kidney. Note the tumor in the dilated thrombosed renal vein.
|
|
|
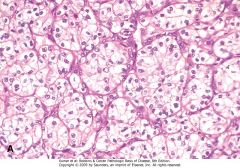
Renal cell carcinoma. A, Clear cell type.
|
|
|
Renal cell carcinoma. B, Papillary type. Note the papillae and foamy macrophages in the stalk.
|
|
|
Renal cell carcinoma.C, Chromophobe type.
|
|
|
Urothelial carcinoma of the renal pelvis. The pelvis has been opened to expose the nodular irregular neoplasm, just proximal to the ureter.
|

