![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Definitions
|
Urolithiasis (from Greek oûron, "urine" and lithos, "stone") is the condition where urinary stones are formed or located anywhere in the urinary system.[1] The term nephrolithiasis (or "renal calculus") refers to stones that are in the kidney, while ureterolithiasis refers to stones that are in the ureter
|
|
|
Epidemiology
1:10 males & 1:20 females have stone episodes 50% recurrence |
Epidemiology
Annual incidence 0.2% (US); 0.13% (Aust) Prevalence 7% males, 3% females Risk of stone formation M : F = 3-4 : 1 (higher [Ucit] in women) Peak age 20 - 40 yo Recurrence rate 10% at 1 yr (without Rx) 35% in 5 yrs 50% in 10 yrs Significant impact on QoL |
|
|
Evolution of stone management in Australia: increasing rate of intervention
|
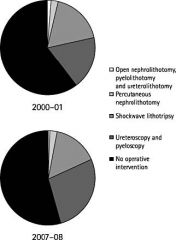
greatest INC in endoscopy
|
|
|
Why has treatment rate outstripped incidence of stone presentations?
|
1. Increased rate of detection of asymptomatic stones: greater prevalence
better imaging 2. Lower intervention threshold: opportunistic treatment during intervention for symptomatic stones 3. Loss of efficiency with less invasive Rx |
|
|
Worldwide evidence
|
Worldwide evidence
Increasing incidence and prevalence, more pronounced in industrialized countries ? Lifestyle & dietary factors ? Better medical access – detection Renal stone formation & predominant stone composition are age & gender dependent Correlation b/w body wt & Uca excretion DM independent risk factor for stone development (Taylor & Curhan, AmJKid 2006) Male preponderance for all stone types except struvite Lower incidence struvite, uric acid incidence stable or same |
|
|
Dietary factors
|
High protein and salt intake risk of Ca stones
High purine diets lower UpH and cause hyperuricosuria Vit B6 deficiency results in ^ formation and excretion of oxalate Low dietary calcium increases oxalate absorption Dehydration - excessive fluid loss, inadequate fluid intake Drugs - Ca supplements, indinavir |
|
|
Dietary Calcium and Oxalate
|
thus need to maintain normal dietary ca (because the oxlate normally binds the ca in the gut and to the faseces..)
|
|
|
Geographical factors
|
Higher incidence during summer months & in tropical countries – effect of global warming on US “stone belt” shifting north (est cost $1 bn US by 2050)
? Mechanism - urinary concentration & acidity or Vit D production and Ca absorption. |
|
|
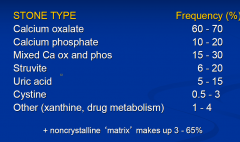
Composition of renal stones
|
|
|
|
“Doctor, how / why did my stone form?”
|
1. Structural / anatomical problems
2. Stone formation varies with stone type a. Exceeding supersaturation: uric acid & cystine b. Infection: triple phopshate (“struvite”) stones c. Calcium stones: most common but least understood |
|
|
Structural / anatomical problems
|
1. divitculum in the kidney
2. medullary sponge kidney |
|

|
divticulium in kidney (thus stagnaented urine)
|
|
|
Uric Acid Stones
|
UA: end-product of purine metabolism of endogenous or exogenous sources.
Weak acid (pK 5.4 at physiologic pH) At urine pH < 5.5 majority exists in its insoluble undissociated form, the major component of UA stone. With more alkaline urine, more soluble Na urate crystals form (but favours Ca phosphate precipitation) Round, smooth, yellow-orange; radiolucent Risk factors: high [urate] - due to high urate excretion (hyperuricosuria) or low Uvol; or low UpH (eg. Idiopathic UA nephrolithiasis - acid urine due to low ammonium excretion, AD disorder, usually male) |
|
|
Cystine stones
|
AR disorder due to mutation of SLC3A1 aa transporter gene on chr 2.
Causes impaired transtubular reabsorption of filtered dibasic aa’s (cystine, ornithine, lysine, arginine), resulting in their excessive urinary excretion Cystine has low solubility - precipitates in hexagonal plates to form major constituent of cystine stones. |
|
|
Struvite stones
aka Triple Phosphate |
aka Triple phosphate, infected stone, matrix
Combination of magnesium ammonium phosphate and carbonic apatite 50% contain nidus of another stone composition Form when urease producing organisms (Proteus, Haemophilus, Klebsiella etc) split urea into ammonia, bicarbonate and carbonate, producing alkaline microenvironment which favours crystallisation of ammonia Risk factors: those which predispose to UTI ie congenital or acquired anatomic abnormalities, neurologic disorders, foreign bodies |
|
|
Aetiological factors for Calcium stones
|
Ca oxalate develops in acidic urine (pH < 6)
Ca phosphate develops in alkaline urine (pH > 7.5) Ca phosphate stones - risk factors: UTI, hyper PTH, RTA Promoters of Ca oxalate stones include: Hypercalciuria Absorptive (intestinal) Renal leak Resorptive Hypercalcaemic Hypocitraturia Hyperuricosuria Hyperoxaluria |
|
|
Stone formation: latest evidence
Human stones arise by one of these pathways: |
Overgrowth of stones on plaque – idiopathic ca ox
Primary interstitial apatite crystal formation - Randall plaques (Lingeman, 2003) Plugging of collecting duct, with growth on plugs or growth of expelled plugs in free solution – Hyperoxaluria, RTA, cystinuria Formation in free solution – Crystal accumulation in lumen of tubules (cap) & erosion Binding of ca ox & growth – mixed ca ox / phosphate stones Calcification & atherosclerotic-type lesions in vasa recta |
|
|
Randall Plaques
|
CaPh crystals and organic matrix initially deposited along BM of thin loop of Henle, and extend further into the interstitial space to the urothelium, constituting the so-called “Randall plaque”.
These CaPh crystals seem to be the origin for development of future CaOx stones, which form by attachment of further matrix molecules and urinary CaOx to the plaque. Cause of idiopathic Ca Ox stone formation. Described by Randall 70 yrs ago on autopsy studies; more recently demonstrated in all idiopathic CaOx stone formers (vs zero in healthy controls; Evan, Lingeman et al, 2003) – demonstrated to connect stones to papilla on microscopic CT. Urothelium is lost at attachment site. No intratubular cystallization in tubules / CD’s in these patients. Positive correlation between frequency of stone recurrences and total papillary surface area covered by plaques (Matlaga, 2006) Currently unknown in this model – initial trigger for crystallization, driving forces, exact pathogenetic mechanisms, involved matrix molecules |
|
|
Clinical manifestations
|
Asymptomatic - incidental discovery during unrelated Ix.
Pain - mild ache Renal colic occurs when stones produce obstruction severe, sudden onset, intensifies over 15 - 30 min Assoc nausea & vomiting Can’t sit still or get comfortable (DDx to lower back pain) |
|
|
Sites of Obstruction
|
Calyx / infundibulum (dull pain- due the low pressure)
PUJ Pelvic brim, arching over iliac vessels Posterior pelvis (females) under broad lig / pelvic vv Above intramural ureter / VUJ - most common |
|
|
Assessment
|
History: ? underlying cause for stones
Gout, FHx, IBD, hypercalcaemia Examination: fever, sepsis, tenderness MSU: pH - low: Urate, Ca ox high: Ca phos infection Bloods: WCC often raised, >15 ? Infection UEC, Ca, Urate |
|
|
Investigation
|
1.Radiology
2.FBC UEC 3.Urinalysis / microscopy / culture 4.Delayed - stone analysis serum Ca / UA / PTH 24 hr urine |
|
|
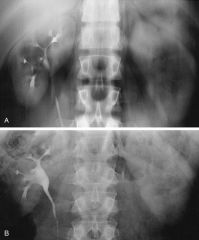
KUB
|
In medicine, KUB refers to a diagnostic medical imaging technique of the abdomen[1] and stands for Kidneys, Ureters, and Bladder.
Quick, inexpensive and easily obtainable Variable sensitivity - 60 - 90% Useful adjunct to CT as a method of predicting stone composition – radiolucency = uric acid ? Dissolution Rx Useful for follow up KUB unless concerns about obstruction or stone lucency; then US or low dose NCCT 1-2% of cancers in US may be attributed to CT radiation |
|
|
Radiological investigation
|
KUB
IVU Renal U/S Non-contrast helical CT |
|
|
Intravenous pyelogram (IVU)
|
Variable quality
Functional study Radiation dose less than CT Good anatomical detail for planning appropriate treatment |
|
|
Renal Ultrasound
|

Procedure of choice for pregnant females
Assess for other causes of acute pain Not a functional study Hydronephrosis Obstruction |
|
|
Non-contrast helical CT Abd/Pelvis
|

Fast, highly sensitive and specific > 99%
Strictly speaking is not a functional study, but can infer obstruction by indirect signs ie perinephric stranding, urinoma Can use in patients with contrast allergy Greater ability to detect alternative pathology Good anatomical detail with coronal reconstruction CT for prediction of stone composition CT densitometry: stone > 1000 HU more likely to fail SWL Stone size, position & skin-to-stone distance also assessable on NCCT and determine outcome |
|
|
Management
|
1. Analgesia - oral, PR, parenteral
- NSAIDs, narcotics 2. ?? iv fluids - if dry (otherwise too much water can be painful) 3. Determine if renal unit is - obstructed - infected -> URGENT DRAINAGE 4. Other criteria for admission - ongoing pain, solitary kidney, renal impairment, pregnant 5. Rx: Conservative or Definitive if required -URS, SWL 6. Prevention – investigation of causes of urolithiasis, lifestyle modification, medication |
|
|
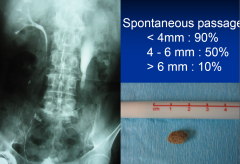
Treatment options
|
Conservative:
Consider chances of spontaneous passage - > 6 mm : 10% 4 - 6 mm : 50% < 4 mm: 90% Role of medical expulsive therapy - tamsulosin Drainage: Nephrostomy Stent Definitive Ureteroscopy SWL PCNL Laparoscopic or open surgery |
|
|
Spontaneous passage
|
|
|
|
Ureteroscopy
|
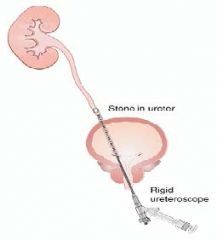
|
|
|
ENERGY SOURCES
|
EHL
EKL, “lithoclast” Laser |
|
|
Laser lithotripsy
|
Ho:YAG – solid-state laser, 2100nm wavelength, pulsed
Photothermal & photodynamic capacity: thermal fragmentation most efficient Pros: short tissue penetration due to water absorption(0.5 –1 mm), diverse applications incl stricture incision & tumour ablation, small fibers (0.2 – 0.6 mm) Cons: long pulse width (= lower pulse energy), ureteric injury Remains the best laser for stone disease in 2012 |
|
|
SWL
|
Requirements:
Shock wave generator Coupling mechanism Localisation Image intensifier US |
|
|
SWL – how does it work?
|
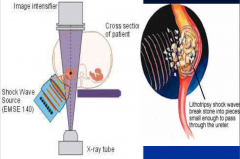
Shock wave -> negative pressure bubble - acoustic cavitation; combined with positive (compression) wave causing shear / tensile stress.
Vascular response: transient but marked reduction in renal perfusion/GFR; structural changes due to rupture of small blood vessels with subsequent haemorrhage Poor understanding until recently considering its broad utilisation Recent evidence from US suggests increased incidence of DM & HT in patients treated with SWL. |
|

|

|
|
|
Percutaneous nephrolithotomy
|
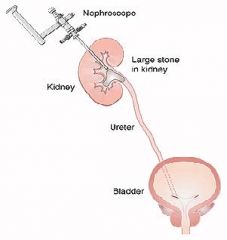
Principles:
Access Removal Drainage Combined Rx |
|
|
Management of recurrent stone formers
|
General
Fluids - how much ?? Lime / orange juice - boosts urinary K cit levels, increases bicarbonate release Specific Dietary advice - reduced protein, oxalate, NOT calcium Hyperuricosuria - Allopurinol, urinary alkalinisation Hypercalciuria - chlorthalidone |
|
|
AVOID…
|

|
|
|
Dietary Factors
|
Fluids: 1996 RCT showed 5yr stone recurrence rate 12%(high uo) vs 27% (low vol uo)
Lemonade / OJ increase urinary citrate Animal protein (meat, chicken, fish) increases urinary ca, UA and phosphate. Salt increases ca & UA excretion. Restrict < 6g/day. - do not restrict Ca - |
|
|
Specific measures
|
Dissolution therapy (uric acid stones)
hydration pH manipulation – potassium citrate / sodibic Allopurinol if hyperuricosuric Hypercalciuria - Thiazides Cystinuria – fluids, low protein, alkaline urine (Uro-cit-K); binders – thiola, penicillamine |
|
|
Renal Colic - Important DDs
|
Abdominal aortic aneurysm
Retro-caecal appendicitis Torsion of testis |
|
|
Dietary Advice for Stone Formers
|
Increased fluid intake (2L urine/day)
Normal calcium intake low oxalate intake (colas, tea, nuts, spinach/rhubarb) Reduce salt intake |
|
|
Medical Treatment of Calcium Stone Formers
|
Hypercalciuria
Exclude and treat hypercalcaemia (hyperparathyroidism, renal tubular acidosis, sarcoidosis) Thiazide diuretics (HCT, Indapamide) enhance Ca reabsorption Hypocitraturia Lemon juice (120mls in 2L water) Potassium citrate Hyperoxaluria Low oxalate diet, correct acidosis,oxalate binders Hyperuricosuria allopurinol |
|
|
Uric Acid Stones Tx
|
Radiolucent
Causes hyperuricaemia gout diuretics high purine diet Effective medical therapy (alkalinise urine to pH >6.5 and allopurinol) – the only stone that can be dissolved |
|
|
Staghorn Stones
|
Infection stones (Urease producing Gm –ve , not E Coli)
Often no loin pain or presents with recurrent UTI Risk of progressive renal damage / sepsis Usually treated by Percutaneous nephrolithotomy +/-ESWL or retrograde pyeloscopy for any residual fragments |

