![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
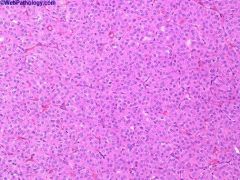
Origin from intercalated cell of collecting duct
4-7% of adult renal epithelial tumors Adults age 50+; 2/3 men; usually an incidental finding 5% are bilateral, 13% are multifocal Benign behavior if follow strict diagnostic criteria; may coexist with renal cell carcinoma;Oncocytoma |
|
|
Birt-Hogg-Dube’ syndrome: autosomal dominant, small dome-shaped papular fibrofolliculomas of face, neck and upper trunk; associated with multiple renal tumors (mean 5.3), usually chromophobe carcinomas or oncocytomas, also oncocytosis
|
|
|
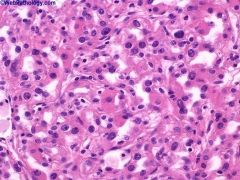
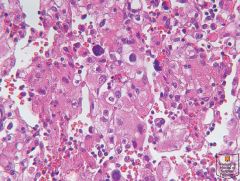
Nuclear grading (Fuhrman) 1
1 - small, round, uniform nuclei (10 microns), inconspicuous nucleoli, look like lymphocytes (may not exist) 2 - slightly irregular nuclei, see nucleoli at 40x only, nuclear diameter 15 microns, open chromatin [40% of tumors] 3 - see nucleoli at 10x, nuclei very irregular, diameter 20 microns, open chromatin [30-40% of tumors] 4 - mitoses, bizarre, multilobated, pleomorphic cells plus grade 3 features, macronucleoli [15% of tumors] |
|
|
Nuclear grading (Fuhrman) 3
1 - small, round, uniform nuclei (10 microns), inconspicuous nucleoli, look like lymphocytes (may not exist) 2 - slightly irregular nuclei, see nucleoli at 40x only, nuclear diameter 15 microns, open chromatin [40% of tumors] 3 - see nucleoli at 10x, nuclei very irregular, diameter 20 microns, open chromatin [30-40% of tumors] 4 - mitoses, bizarre, multilobated, pleomorphic cells plus grade 3 features, macronucleoli [15% of tumors] |
|

|
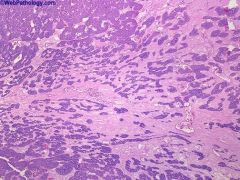
Papillary type, renal cell carcinoma
chromophil; Origin from proximal or distal convoluted tubule 10-20% of adult renal carcinomas; 75% male Tends to present at early stage Associated with adenomatous change in adjacent kidney Molecular/cytogenetics: +7 (75%), +17 (80%), +12, +16, +20, +3q, -Y, -X (p or q for all chromosomes); these changes occur early in tumor neoplasia (Mod Path 2003;16:1053) |
|
|
Mutations in MET protooncogene (#7) are common; MET is a tyrosine kinase receptor for hepatocyte growth factor, and is mutated and activated in papillary renal cell carcinoma via a missense mutation
Also associated with PRCC (papillary RCC gene) on #1; not associated with p53 mutations or 3p- Hereditary papillary carcinoma: t(X;1)(p11.2; p34) - fusion of TFE3 helix-loop-helix transcription factor gene at Xp11.2 with |
|
|
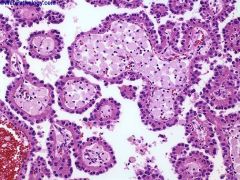
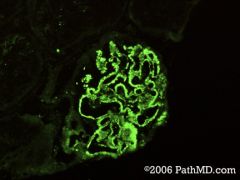
This glomerular disease is associated with low serum complement levels, the presence of granular
immune deposits within the glomeruli, and subepithelial hump-like electron-dense deposits. |
These features are characteristic of acute proliferative glomerulonephritis (a.k.a. poststrep. GN).
|
|
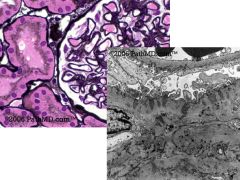
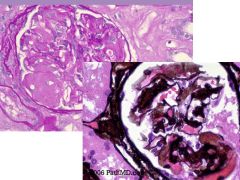
A 35 y/o female with an ovarian mass and possible lupus presents with >3.5grams of protein in a 24
hour urine collection. Histology reveals increased glomerular capillary wall thickening. The Jones (silver) stain reveals irregular spikes that protrude from the glomerular-basement membrane |
membranous glomerulopathy
|
|
patient with an h/o multiple myeloma undergoes a renal biopsy. The histology shows interstitial and glomerular deposition of amorphous material. The PAS stain
shows weak staining of this material present within the glomeruli. The Jones stain shows focally delicate spikes projecting from the outer aspect of the glomerular capillary wall |
AL Amyloidosis is associated with a lambda light chain monoclonal gammopathy. The EM
shows 8-12 nm fibrils. AA Amyloidosis, which is also known as secondary amyloidosis usually, occurs in patients with chronic inflammatory diseases. Fibrillary GN shows 15-30 nm characteristic fibrils on EM, and the immunotactoid GN has microtubules that are 20-50nm on EM. Cryoglobulinemic GN can be associated with an underlying B-cell dyscrasia, but has dense deposits with 25-35 nm tubules. |
|
|
Proteus bacteria are associated with which of the following types of renal stones?
|
Magnesium, Amonium, Phosphate stones (struvite) are formed after infections with urea
splitting organisms. Proteus is the most common urease organism associated with UTIs. These lead to the “staghorn calculi” that often form stones that are in the shape of the collecting ducts. A simple way to remember this is that Magnesium, Amonium, Phosphate stones make a “MAP” of the collecting system (struvite stones). |
|
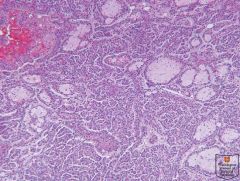
mean 41 years but range is 5-83 years; 40-50% are incidental; 2/3 female; associated with polycythemia as a paraneoplastic syndrome in 12%
|
Metanephric adenoma
stains - CD57+; WT1+; AMACR- ( but positive in papillary); CK7- |
|
Mean 52 years, wide age range; no gender preference
Criteria for urachal origin: centered in anterior wall or dome of bladder, invasion from outside in, bladder mucosa intact or ulcerated, no carcinoma in situ or glandular metaplasia other than cystitis glandularis, presence of urachal remnants is helpful but not always identifiable |
Urachal adenocarcinoma
critical to include the entire urachal tract and umbilicus when performing partial or radical cystectomy for urachal adenocarcinoma. This bladder tumor extended along the urachal tract to produce ulceration around umbilicus (umbilical skin is seen at upper left). |
|
2/3 male, mean age 55 years, but often found in young adults; associated with analgesic nephropathy
|
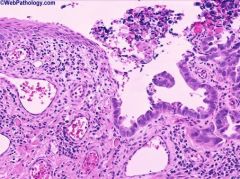
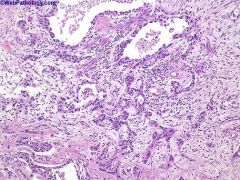
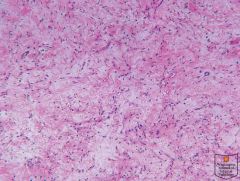
Collecting duct or Bellini duct carcinoma
This rare renal tumor shows differentiation towards medullary collecting tubules. It is usually centered on the medulla with extension towards the cortex. It has a tubulo-papillary architecture accompanied by substantial desmoplastic response. Major criteria: involvement of medullary pyramid (small tumors), irregular tubular architecture, marked desmoplasia, high grade hobnail cells, positive for high molecular weight cytokeratin and Ulex europaeus, no urothelial carcinoma elsewhere Minor criteria: central location (large tumors), papillary architecture with wide fibrous stalks and desmoplastic stroma, inflammatory stroma with neutrophils; extensive renal, extrarenal and vascular infiltration, mucin positive |
|
Origin: proximal or distal convoluted tubule
Epidemiology: 75% male Clinical: tends to present at early stage |
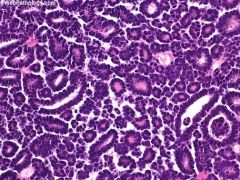
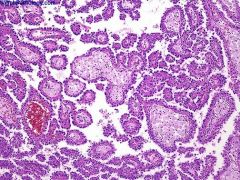
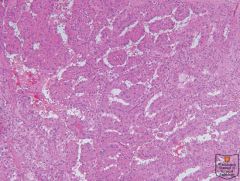
Papillary type, renal cell carcinoma
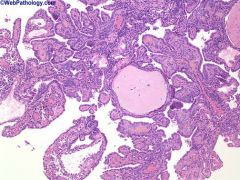
Papillary renal cell carcinoma comprises 15% to 18% of renal cell carcinoma. Note the prominent papillary structures many of which enclose clusters of foamy macrophages. |
|

most common renal tumor of infancy, 5% of pediatric renal tumors; age at presentation varies by type (classic: 16 days, cellular: 5 months, mixed: 2 months); may present in utero causing nonimmune fetal hydrops and polyhydramnios
Unlikely to occur in patients over 2 years old |
congenital tumor resembling infantile fibromatosis or leiomyoma, with fascicles and whorls of bland myofibroblasts and thin collagen fibers; cellular variant resembles infantile fibrosarcoma
Also called fetal, mesenchymal or leiomyomatous hamartoma |
|
|
Deletions or mutations involving 11p13, 11p15, or Xq11.1 WT1, WT2, WT3, WTX
Zinc-finger DNA-binding protein; tumor suppressor genes IPOX for WT1 |
Nephroblastoma
|
|
|
t(12;15)(p13;q25)
ETV6-NTRK3 Receptor tyrosine kinase RT-PCR, FISH |
Cellular mesoblastic nephroma
|
|
|
Translocations of 22q11, usually t(11;22)(q24;q12)
EWS-FLI1 Transcriptional activator RT-PCR, FISH; IPOX for CD99 or FLI-1 |
Ewing sarcoma / PNET
|
|
|
t(X;18)(p11;q11)
SYT and SSX1, 2, or 4 Chromatin remodeling, transcriptional regulation, β-catenin signaling pathways RT-PCR, FISH |
Synovial sarcoma
|
|
|
t(10;17), del 14q
Undetermined Undetermined Karyotyping |
clear cell sarcoma of kidney
|
|

|
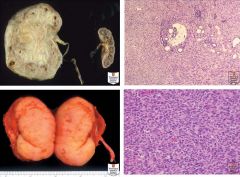
Nephroblastoma and nephrogenic rests. A: This solitary, large, friable tumor bulges beyond the normal renal contour. Residual kidney is to the right. B: Multicentric tumors and hyperplastic nephrogenic rests are present in this post-treatment specimen. C: Diffuse perilobar hyperplastic nephrogenic rests, characterized by diffuse expansion of the kidney and absence of pseudocapsule. A small amount of uninvolved kidney is at bottom center of field. D: Partially differentiated cystic nephroblastoma. Microscopically, immature elements of nephroblastoma were present in the cyst walls.
|
|
|
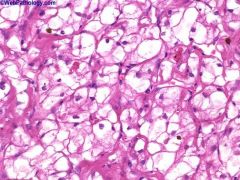
9q34, 16p13.3, 5q mutations
TSC1, TSC2 Tumor suppressor genes Constitutional karyotype |
Angiomyoplipoma
|
|
|
Constitutional 11p15.5 mutation; possible 22q11.2 involvement HBB hSNF5/INI1
Hemoglobin S Chromatin remodeling and transcriptional regulation IPOX for INI1 |
Renal medullary carcinoma
|
|
|
t(X;1)(p11.2;q25) t(6;11)(p21;q12) ASPL-TFE
Transcriptional activators Karyotyping, IPOX for TFE |
Translocation carcinomas
|
|
|
Deletions or mutations involving 22q11.2
hSNF5/INI1 Chromatin remodeling and transcriptional regulation IPOX for INI1 and cytokeratin |
Malignant rhabdoid tumor
|
|
|
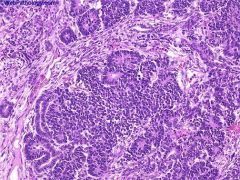
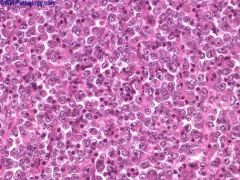
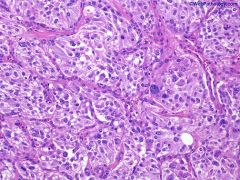
The triphasic nature of Wilms Tumor is obvious here. The epithelial elements surround nodules of blastema and are attempting for form rosettes. The nodules of blastem are separated by myxoid stroma.
Definition: triphasic tumor, usually children, with undifferentiated blastema, fibroblast-like stroma and epithelium triphasic with undifferentiated blastema (cellular with small blue primitive cells with scanty cytoplasm), fibroblast-like stroma and epithelium (abortive tubules, glomeruli with elongate/ovoid nuclei having molded/wedged shapes); may have smooth muscle, cartilage, adipose tissue, squamous or mucinous epithelium, bone, neural tissue; prominent skeletal muscle is associated with bilateral tumors in young children |
|

|
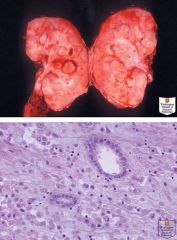
Metanephric stromal tumor.
A: This large tumor extends out from renal medulla. B: Entrapped tubule surrounded by a “collarette” of spindled tumor cells. C: Entrapped artery shows angiodysplasia, with epithelioid transformation of mural smooth muscle cells. |
|
benign abdominal mass in infants (mean age 2 years), centered on renal medulla, with bland spindle cells that entrap native kidney
Often misdiagnosed as mesoblastic nephroma May be related to Wilms’ tumor Treatment: excision is curative |
Metanephric stromal tumor
|
|
pure epithelial tumor composed of embryonal-type epithelium with bland features
Rare, 0.2% of adult renal epithelial neoplasms; < 100 cases described |
Metanephric adenoma
|
|
|
Mesoblastic nephroma. A: This tumor with “classic” histology resulted in fetal hydrops and stillbirth. Contralateral kidney (right) included for comparison. B: Classic histology resembling infantile fibromatosis, with infiltration of adjacent renal parenchyma. C: This tumor in an older infant had cellular histology. D: This cellular tumor is histologically identical to congenital fibrosarcoma
|
|
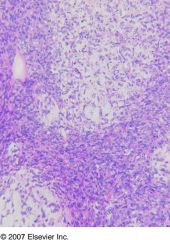
Definition: monotonous proliferation of uniform small round cells with evenly distributed fine chromatin, separately by uniform vascular network
Also called bone metastasizing renal tumor Epidemiology: mean age 36 months, range 2 months-14 years, peaks at ages 2-3 years; 2/3 male, graph 4% of childhood renal tumors; 20 new cases per year in US; rarely in teenagers / adults |
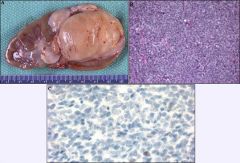
Clear cell sarcoma of kidney.
|
|
1-2% of childhood renal tumors
Epidemiology: 60% are <1 year old, 30% 1-3 years old, rare > 5 years, age distribution 15% are associated with primary embryonal tumors in the midline posterior fossa, often medulloblastoma Clinical: usually stage 2 or higher; 9% are bilateral Very aggressive; 82% present with metastases; 90% die in 2 years |
Rhabdoid tumor - Kidney
Positive stains: keratin (particularly CK8), vimentin, EMA Negative stains: muscle markers, neural markers, WT1, HSNF5/INI1 |
|
Epidemiology: all patients have been black; sickle cell trait or hemoglobin SC disease in almost all cases; average age 21-24 years, 75% male; 75-89% occur in right kidney (Urology 2007;70:878)
Clinical: aggressive; usually advanced disease at presentation with metastases to lymph nodes, adrenal gland, peritoneum, perinodal retroperitoneum, liver, lungs or inferior vena cava; death in 4-6 months |
Medullary carcinoma of kidney
|
|
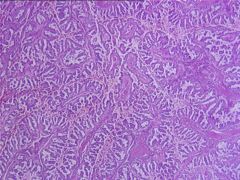
papillary or tubulopapillary tumor with foamy macrophages and intracellular hemosiderin, no clear cells; trisomy 7, 17
Also called chromophil; some cases were formerly called renal cell carcinoma-granular type due to granular cytoplasm |
Papillary type, renal cell carcinoma
|
|
|
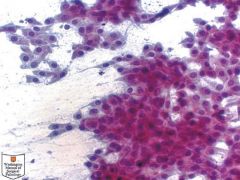
Renal cell carcinoma, Fuhrman nuclear grade 4
|
|
|
Multilocular cystic renal cell carcinoma with clear cell lining and neoplastic cells within septum
|
|
|
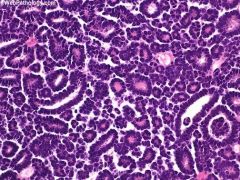
Papillary renal cell carcinoma, Type 1, with small basophilic cells.
|
|
|
Papillary renal cell carcinoma, Type 2, with large eosinophilic cells.
|
|
|
Renomedullary interstitial cell tumor.
|
|
|
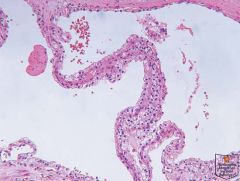
This urothelial carcinoma was involving the renal pelvis. The neoplastic cells show low nuclear pleomorphism, inconspicuous nucleoli, and abundant cytoplasm, consistent with a low grade lesion
|
|
|
|
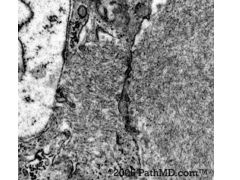
Metanephric adenoma of kidney.
|
|
|
|
Metanephric adenoma of kidney.
|
|
Also called extra-adrenal pheochromocytoma
Uncommon in bladder (< 0.5% of bladder neoplasms) Rarely associated with neurofibromatosis, urothelial carcinoma, renal cell carcinoma ~50% have attacks during urination or full bladder of bursting headache, pounding sensation, anxiety, sweating, syncope, hypertension or hematuria Median age 44 years vs. 70 years for urothelial carcinoma, often young women 50% have positive urinary VMA |
Paraganglioma
|
|
urinary bladder
|
Nephrogenic metaplasia is a metaplastic process seen after surgical manipulation of the urinary tract, or in association with trauma, stones, and inflammation. Papillary, polypoid, or cystic structures lined by cuboidal epithelium are seen here.
|

