![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
What are the functions of the kidneys?
|
- Excretion of metabolic waste products and foreign chemicals
- Regulation of water and electrolyte balances - Regulation of body fluid osmolality and electrolyte concentrations - Regulation of arterial pressure - Regulation of acid-base balance - Secretion, metabolism, and excretion of hormones - Gluconeogenesis |
|
|
What is the central physiologic role of the kidneys?
|
Control VOLUME and COMPOSITION of the body fluids
|
|
|
What proportion of the total body water is intracellular fluid (ICF)? What percent of total body weight?
|
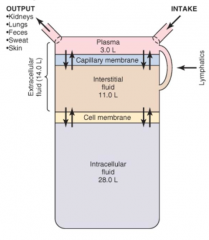
2/3 of total body water
40% of body weight |
|
|
What proportion of the total body water is extracellular fluid (ECF)? What percent of total body weight?
|
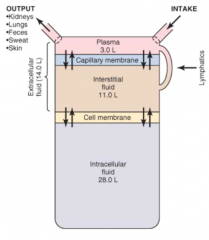
1/3 of total body water
20% of body weight |
|
|
What are the components of extracellular fluid (ECF)? Proportions?
|
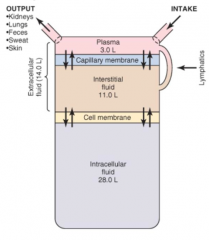
- Interstitial Fluid (3/4 of ECF, 15% total body water)
- Plasma (1/4 of ECF, 5% total body water) |
|
|
How many liters is the ICF? Interstitial fluid component of ECF? Plasma component of ECF?
|
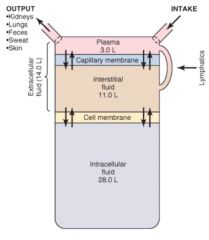
- ICF: 28 L
- Interstitial fluid (ECF): 11 L - Plasma (ECF): 3 L (42 L total) |
|
|
What separates the intracellular fluid (ICF) from the extracellular fluid (ECF) ? What part of the ECF? What determines distribution across this barrier?
|
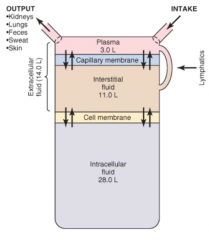
- Cell membrane
- Separates ICF from interstitial fluid - Distribution governed by osmotic forces (not freely permeable to solutes, but is to water) |
|
|
What separates the two components of the ECF?
|
Capillary membrane
|
|
|
What are the major cations in the intracellular fluid (ICF)?
|
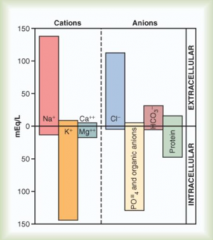
K+
Mg2+ |
|
|
What are the major anions in the intracellular fluid (ICF)?
|
PO4(-3)
Organic anions Protein |
|
|
What are the major cations in the extracellular fluid (ECF)?
|
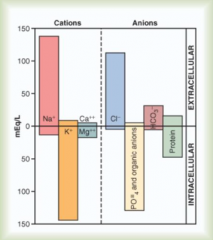
Na+
|
|
|
What are the major anions in the extracellular fluid (ECF)?
|
Cl-
HCO3- (some protein) |
|
|
What is osmolarity? Units?
|
- Concentration of osmotically active particles in total solution
- mOsm / L water |
|
|
What is the normal osmolarity of the ECF and ICF?
|
Averages 280-300 mOsm/L
(nearly identical in all major compartments of body fluids) |
|
|
What is osmolality? Units?
|
Express in terms of mOsm/kg solvent (water)
|
|
|
How does osmolarity compare to osmolality?
|
In relatively dilute solutions, such as those found in body, osmolality ≈ osmolarity
|
|
|
What is the effect on ICF and ECF volume and osmolarity, of adding ISOTONIC NaCl?
|
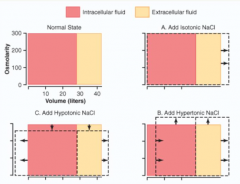
* Increase ECF volume
No change to ICF volume, or ECF/ICF osmolarity |
|
|
What is the effect on ICF and ECF volume and osmolarity, of adding HYPERTONIC NaCl?
|
* Increase ECF volume and decrease ICF volume (water leaves ICF because of increased osmolarity in ECF)
* Increased ECF and ICF osmolarity d/t hypertonic sol'n |
|
|
What is the effect on ICF and ECF volume and osmolarity, of adding HYPOTONIC NaCl?
|
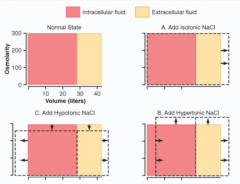
* Increase ECF and ICF volume
* Decrease ECF and ICF osmolarit |
|
|
What are the kidney processes that determine the composition of the urine?
|
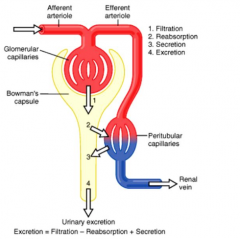
1. Filtration
2. Reabsorption 3. Secretion 4. Excretion |
|
|
What is the relationship between filtration, reabsorption, secretion, and excretion?
|
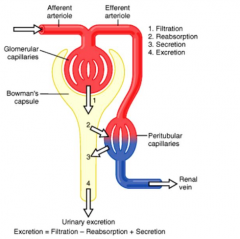
Excretion = Filtration - Reabsorption + Secretion
|
|
|
What is the most likely cause for a chronic decrease in GFR?
|
Decrease in total area of glomerular capillary membrane
|
|
|
What is the glomerular filtrate?
|
Ultra-filtrate of plasma
|
|
|
What causes the formation of the Glomerular Filtrate?
|
Net effect of Starling forces to move (filter) fluid out of glomerular capillaries and into Bowman's space
|
|
|
What is the concentration of most salts and organic substances in glomerular filtrate compared to plasma?
|
Mostly the same concentration
|
|
|
What is the concentration of large proteins, substances bound to protein, and cellular elements in glomerular filtrate compared to plasma?
|
Normally they are excluded from glomerular filtrate and remain in plasma
|
|
|
How often does the entire plasma volume (3L) get filtered through kidneys?
|
Every 30 min
|
|
|
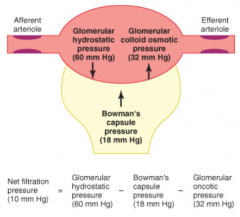
What are the physical forces causing filtration by glomerular capillaries?
|
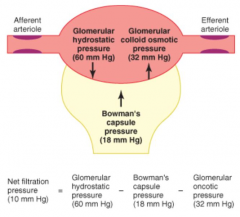
- Glomerular hydrostatic pressure promotes filtration
- Glomerular colloid osmotic pressure opposes filtration - Bowman's capsule pressure opposes filtration |
|
|
What is the net filtration pressure? Contributions?
|
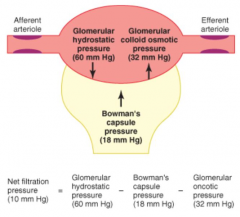
Net filtration pressure (10 mmHg) = Glomerular Hydrostatic Pressure (60 mmHg) - Bowman's Capsule Pressure (18 mmHg) - Glomerular Oncotic Pressure (32 mmHg)
|
|
|
What is the normal Renal Plasma Flow (RPF)?
|
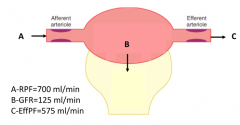
700 mL/min
|
|
|
What is the normal Glomerular Filtration Rate (GFR)?
|
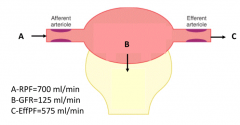
125 mL/min
|
|
|
What is the normal Efferent Plasma Flow (EffPF)?
|
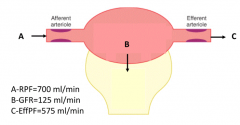
575 mL/min
(RPF (700) - GFR (125) = EffPF) |
|
|
How can you calculate GFR?
|
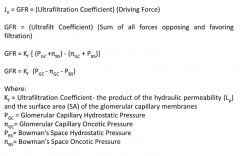
GFR = Kf * (Pgc - πgc - Pbs)
Kf = ultrafiltration coefficient (product of hydraulic permeability and surface area of glomerular capillary membranes) Pgc = glomerular capillary hydrostatic pressure πgc = glomerular capillary oncotic pressure Pbs = Bowman's space hydrostatic pressure |
|
|
Why do you not include πbs in calculating GFR?
|
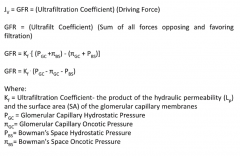
There should not be protein (oncotic pressure) in Bowman's space normally
|
|
|
How are RBF and GFR auto-regulated? What are the implications of this?
|

- As arterial pressure increases, urine output increases
- This means that RBF and GFR will remain relatively constant from 50 - 150 mmHg - Only at very low arterial pressures (causes drop) or high arterial pressures (causes increase) do you get changes in RBF or GFR |
|
|
Which of these will increase when renal perfusion pressure goes from 100mHg to 130mmHg?
- Renal Blood Flow (RBF) - GFR - Urinary osmolarity - Urine flow rate |

Urine flow rate
(RBF and GFR are auto-regulated and only fluctuate at arterial pressure <50 mmHg or >150 mmHg) |
|
|
What are the mechanisms of GFR and RBF Auto-Regulation?
|
- Myogenic mechanism
- Tubuloglomerular feedback |
|
|
Where is the myogenic mechanism? Function?
|
- Intrinsic property of blood vessels
- Stretch of vascular smooth muscle, as experienced during increased arterial pressure, elicits contraction, which elevates vascular resistance and maintains constant blood flow (and GFR) - GFR and RBF auto-regulation mechanism |
|
|
Where is tubuloglomerular feedback? Function?
|
- Auto-regulatory mechanism unique to kidney
- In response to an elevation of perfusion pressure, increased fluid is filtered leading to increased delivery of NaCl to macula densa - This increased delivery elicits an increase in vascular resistance - GFR and RBF auto-regulation mechanism |
|
|
What is the major determinant of resistance in renal blood flow to kidney?
|
Afferent arterioles
|
|
|
How does a drop in arterial pressure affect the kidney?
|

- ↓ Arterial pressure →
- ↓ Glomerular hydrostatic pressure → - ↓ GFR → - ↓ NaCl sensed at Macula Densa (also d/t ↑PT NaCl reabsorption) → - ↑Renin → ↑AngII → ↑Efferent arteriolar resistance - ↓Afferent arteriolar resistance - ↑Efferent arteriole resistance and ↓Afferent arteriole resistance → ↑ Glomerular Hydrostatic Pressure |
|
|
What factors cause ↓ NaCl sensing at Macula Densa?
|

- ↑ Proximal tubule NaCl reabsorption
- ↓ GFR (d/t ↓ arterial pressure) |
|
|
What are the outcomes of ↓ NaCl sensing at Macula Densa?
|

- ↑Renin → ↑AngII → ↑Efferent arteriolar resistance
- ↓Afferent arteriolar resistance - Both lead to ↑ Glomerular hydrostatic pressure (↑GFR) |
|
|
Which hormones decrease GFR?
|
- NE
- Epi - Endothelin - AngII (or no change) |
|
|
Which hormones increase GFR?
|
- Endothelial derived NO
- Prostaglandins |
|
|
What are the components of the glomerular filtration barrier?
|
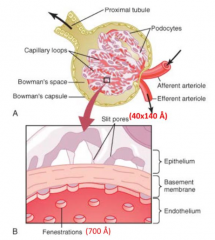
- Capillary wall (w/ 700 Å fenestrations)
- Basement membrane - Podocytes (w/ processes and slit pores - 40x140 Å) |
|
|
How is the filtration barrier selective? Implications?
|
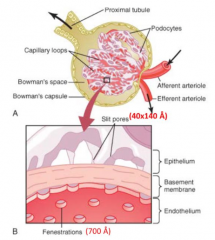
- Size-selective: more permeable to small molecules
- Charge-selective: more permeable to positively charged molecules (proteins are generally negatively charged) |
|
|
What structures are in the slits between podocyte foot processes?
|

- Nephrin (N)
- P-Cadherin (P-C) |
|
|
How does the molecular weight compare to the filterability of a substance by glomerular capillaries?
|
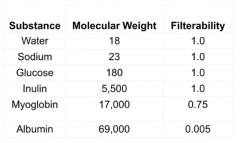
Smaller MW → greater filterability
- H2O, Na+, glucose, inulin = 100% filterable - Myoglobin = 75% filterable - Albumin = .5% filterable |
|
|
What happens in the thin descending loop of Henle?
|
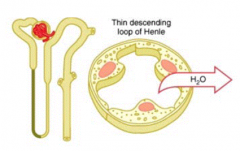
Reabsorption of H2O secondary to cortical-medullary osmotic gradient
|
|
|
What happens in the thin ascending loop of Henle?
|
- Impermeable to H2O
- Passive reabsorption of Na+, dilution of tubular fluid - Permeable to urea, urea is secreted |
|
|
What happens in the thick ascending loop of Henle?
|
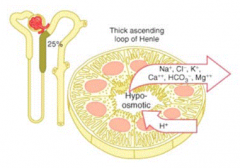
- Reabsorbs 25% of filtered Na+ by Na+/K+/2Cl- transport
- Lumen positive potential drives paracellular reabsorption of Na+, K+, Mg2+, Ca2+ - Impermeable to H2O, dilutes tubular fluid |
|
|
What are the mechanisms of Na+, Cl-, and K+ transport in the thick ascending loop of Henle? What inhibits this?
|
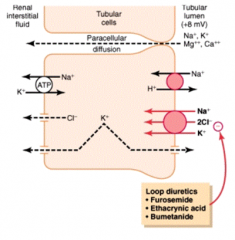
- Na+/K+/2Cl- co-transporter reabsorbs these ions from tubular lumen
- Inhibited by loop diuretics: furosemide, ethacrynic acid, bumetanide - Na+/H+ exchanger also reabsorbs Na+ while secreting H+ - Paracellular diffusion of Na+, K+ into interstitium |
|
|
What happens in the early distal tubule?
|
- Reabsorbs Na+, Cl-, Ca2+, and Mg2+
- Impermeable to H2O |
|
|
Which part of the nephron is sensitive to thiazide diuretics? What transporter does it act on?
|
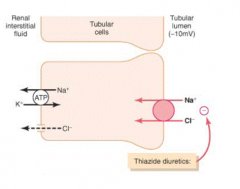
Early Distal Tubule - acts by inhibiting Na+/Cl- co-transporter
|
|
|
What happens in the late distal tubule and cortical collecting duct in principal cells?
|
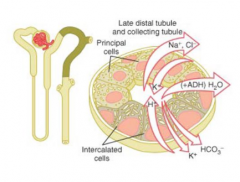
- Reabsorbs Na+, secretes K+
- Regulated by aldosterone - Water permeability regulated by ADH |
|
|
Which part of the nephron is sensitive to K+-sparing diuretics?
|
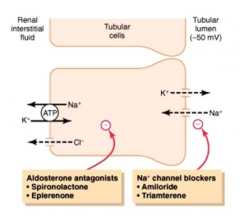
Late distal tubule and cortical collecting duct (principal cells)
|
|
|
What is the Na+ channel on the apical membrane of principal cells? What drugs inhibit this channel?
|
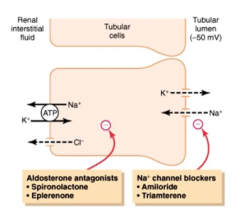
- ENaC - epithelial sodium channel
- Inhibited by Amiloride and Triamterene |
|
|
What happens in the medullary collecting duct?
|
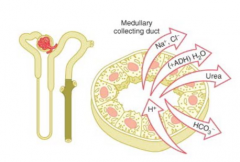
- Reabsorbs Na+ (similar to principal cells)
- ADH-stimulated water reabsorption - Urea reabsorption in medullary collecting duct |
|
|
Where is the action of aldosterone? Effects?
|

- Acts in principal cells of late distal tubule and collecting duct
- Increases NaCl reabsorption - Increases K+ secretion - Increases H2O reabsorption |
|
|
Where is the action of Angiotensin II? Effects?
|

- Proximal tubule, thick ascending loop of Henle / distal tubule, collecting tubule
- Increases NaCl, H2O reabsorption - Increases H+ secretion |
|
|
Where is the action of Anti-Diuretic Hormone? Effects?
|

- Distal tubule / collecting tubule and duct
- Increases H2O reabsorption |
|
|
Where is the action of Atrial Natriuretic Peptide? Effects?
|

- Distal tubule / collecting tubule and duct
- Decreases NaCl reabsorption |
|
|
Where is the action of Parathyroid Hormone? Effects?
|

- Proximal tubule, thick ascending loop of Henle / distal tubule
- Decreases PO4 reabsorption - Increases Ca2+ reabsorption |
|
|
Which hormones increase NaCl reabsorption?
|

- Aldosterone
- Angiotensin II |
|
|
Which hormones decrease NaCl reabsorption?
|

Atrial Natriuretic Hormone
|
|
|
Which hormones increase H2O reabsorption?
|

- Aldosterone
- Angiotensin II - ADH |
|
|
Which hormones increase K+ secretion?
|

Aldosterone
|
|
|
Which hormones increase H+ secretion?
|

Angiotensin II
|
|
|
Which hormones affect PO4 and Ca2+ reabsorption? How?
|

Parathyroid Hormone:
- Decreases PO4 reabsorption - Increases Ca2+ reabsorption |

