![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
what is the primary requirement of the brain and why |
constant o2 rich blood supply. Patientswith damage to their limbic lobe due to alcohol will talk meaningfully andinformatively but things that they say will be false and made-up, but they areunaware what they are saying is false this is called confabulation |
|
|
why does local functioningwithin the brain require constantchanges in local blood flow |
because brainactivity is constantly changing and blood flow needs to match level of activityfor proper local functioning. |
|
|
how is the brain adapted to suit its high activity? |
· High O2 consumption/size ratio · High proportion of cardiac output/size · High resting O2 extraction of 35% (body averageis 25%) |
|
|
how has the brain adapted to achieve this constant high flow of o2 rich blood and o2 extraction? |
developedthe Circle of Willis. An anastomosis – streams of arteries that branch out andthen reconnect with one another. To achieve high O2 delivery/extraction to neurons, capillarydensity is very high (3000-4000 per mm^2) – remember Fick’s law: J = -DA ∆C/x |
|
|
what major arteries make up the circle of willis |
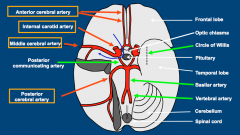
anterior cerebral artery internal carotid artery middle cerebral artery posterior cerebral artery basilar artery |
|
|
where is an embolus passing up the internal carotid artery likely to lodge |
in the middle cerebral artery |
|
|
how does the brain control the CVS to safeguard its own blood supply |
modulate sympathetic-mediated vasoconstriction - has carotidsinus baroreceptors which monitor cerebral perfusion pressure (BP) - Cerebral resistance vessels are spared frombaroreceptor reflex-induced vasoconstriction. - auto-regulation is extremely well developed (myogenic response) - local metabolic vasodilation well developed |
|
|
what is metabolic vasodilation |
So whenmetabolite levels are increasing and activity is high, the vessels willvasodilate to accommodate for this. |
|
|
why is the circle of willis adaptive for the brain |
that if there isa blockage or stenosis somewhere in the circle, then the collateral arteriescan contribute and maintain flow so blood is still flowing around.So the Circle ofWillis is a structural feature that offers a protective function. |
|
|
why are cerebral resistance vessels spared from the baroreceptor reflex |
when BP goesdown, it activates the baroreceptor reflex which vasoconstricts arterioles andincreases Cardiac output to increase BP, the arterioles in the brain are not constrictedduring this process. This allowsblood flow to continue to the brain because other systemic vessels will beconstricted while the cerebral ones are nice and open. |
|
|
Auto-regulation(myogenic response) is extremely well developed in cerebral vessels what does autoregulation mean |
the intrinsicability to maintain blood flow under different blood pressures. |
|
|
what are the carotid sinus baroreceptors |
are stretch sensitivemechanoreceptors that are sensitive to changes in blood pressure. |
|
|
how do carotid sinus baroreceptors mantain bf to the brain |
Changes in bloodpressure will cause them to change firing of their afferent fibres. At lowpressures they will be inactive. so decrease firing in afferent fibres to the NTS. Less excitation of NTS so less excitation CVLM so no turning down of RVLM. RVLMhas neurones that project down and can activate sympathetic neurones at theintermediolateral point. so get inc in sympathetic activity and decrease in parasympathetic activity. |
|
|
how do carotid sinus baroreceptors respond to increased BP |
An increase inblood pressure will cause increased firing in afferent fibres to the NTS. TheNTS will send excitatory info to the CVLM which will send inhibitory signals tothe RVLM (head of sympathetic system). RVLM has neurones that project down and canactivate sympathetic neurones at the intermediolateral point. By turning downthe RVLM neurones there will be less activation of sympathetic nerves. Thismeans there will be decrease in HR, decrease in SV (lower force of contraction)this reduces CO and then there will be reduced tone of arterioles reducing TPR.Together arterial BP will be reduced. |
|
|
between what mean arterial pressures can the myogenic response mantain bf to the brain? |
60mmHG to 160mmHG So when BPincreases/decreases within this range, flow isn’t affected. |
|
|
why does myogenic response mantain bf to the brain at arterial pressures below 60mmHG |
autoregulationrange is surpassed and no longer effective. Despite the vessel being very distended(due to autoregulation) pressure is so low there isn’t enough driving force andnot enough perfusion. At this level of hypotension it is likely to lead tomental confusion and syncope. |
|
|
what happens if bp increases above 160mmHG, and myogenic response cannot reduce bf to the brain |
if BP increasestoo much, beyond the upper limit of the myogenic response then the individualis at risk of things like bleeding. Sympatheticstimulation helps increase the range of the autoregulation by enhancing it. |
|
|
why is hypoventilation linked to increased cerebral blood flow |
PCO2 is increased, in response to this increased acidity blood vessels willvasodilate to try blow off the CO2. Soincreased PCO2 is linked to vasodilation and increased flow incerebral vessels |
|
|
why is hyperventilation linked to decreased cerebral blood flow |
PCO2 is decreased. theblood will become more alkaline As you’ll behypocapnic, the cerebral vessels will decide to vasoconstrict to reduce flowand removal of CO2. |
|
|
what effect does hypoxia have on cerebral blood flow and why |
cerebral bloodflow will increase. This is because we want to try maintainoxygen delivery to brain tissue.This is occursas hypoxia leads to release of certain metabolites like adenosine which arevasodilators. |
|
|
what is metabolic hyperaemia |
Localisedchanges of blood flow can be seen when doing different tasks, e.g. whenresting, when doing a test etc. This is because of increased blood for to theareas involved in that task to provide oxygen. |
|
|
why do we get metabolic hyperaemia |
relationship between neuronal firing and blood flow inc neuronal firing = inc bf to that region. K+ in the ECF, increasesas neuronal firing frequency increases because to hyperpolarise the cell andfire again the K+ channels will open and K+ willefflux. During high frequency firing there will be a lot of K+coming out and building up in the ECF. The high K+in the interstitial fluid causes blood vessels to dilate. |
|
|
what is the nervous control of cerebral arteries |
cerebralarterioles within the brain have little innervation and instead are regulatedby intrinsic auto-regulation, myogenic response and metabolic auto-regulation. baroreceptor reflex has little effect on cerebral arterioles |
|
|
what are perivascular nerves and where can they be found |
perivascular(sitting around blood vessels) nerves around the cerebral arteries These nervesconsist of nociceptive fibres, parasympathetic vasodilator fibres andsympathetic vasoconstrictor fibres (little effect). |
|
|
what is the role of the perivascular nociceptor fibres |
Mediate the painof vascular headaches in strokes and the later phase of migrane, They also havemotor function and release dilators (substance P, CGRP) and reduce constrictors(5-HT). |
|
|
what is a migrane |
Amigrane involves a severe headache caused by vasodilation of extracerebralvessels like the middle meningeal artery, as well as inflammation around thevessel. This dilation is thought to be due to release of substance p and CGRP |
|
|
why is Sumatriptan(a 5-HTB agonist) used in migranes |
causesconstriction of blood vessels, this reduces inflammation induced vasodilation. Thishelps reduce the pain |
|
|
what is the blood brain barrier |
The blood brainbarrier is a result of the continuous tight junctions in the cerebralcirculation. This makes it difficult for substances to move across into theinterstitial areas of the brain and keeps them in the lumen of the vessel. |
|
|
what kind of substances can move into the brain (past the BBB) |
Lipophillicsubstances can move across like CO2, O2 and anaesthetics. Things thataren’t lipophilic but are important for the brain e.g. glucose, amino acidsmust have carrier-mediated transport mechanisms to get them across. This isdone by facilitated diffusion |
|
|
what is the function of the Blood Brain Barrier |
The BBB keepssubstances out of the brain -> This is important because in our blood wehave circulating neuro-active chemicals that would interefere with neuronalsignaling e.g. catecholamines like adrenaline. We don’t want these getting intothe brain interstium from the blood as it will alter how the brain is working. The BBB keepssubstances in the brain -> Namely neurotransmitters, otherwise if they couldeasily move out they would be continuously washed out of the brain due to highblood flow |
|
|
The BBBis defective and breaks down at special sites, why is this adaptive. |
this is to allow access of circulating signaling molecules. |
|
|
BBB is broken down in the area postrema of the brainstem. why is this adaptive |
chemosensitivetrigger area) BBB brokendown here, so receives inputs from blood borne drugs (emetic molecules) orhormones and communicates with the vomiting centre ->Angiotensin II can also move into the brain at the area postrema and stimulateAngII receptors to stimulate the sympathetic system. In this way the RAASsystem is communicating with the brain |
|
|
BBB is broken down in the Sub-fornicular of the hypothalamus why is this adaptive |
Inthe hypothalamus, angiotensin II can diffuse into the brain substance and causethirst sensation |
|
|
BBB is broken down in the periventricular osmoreceptors of the hypothalamus why is this adaptive |
Here plasmaosmolarity can be measured by osmoreceptors as the BBB is leaky, this can leadto ADH secretion if required These areasallow the brain to sense what is going on in the circulation |
|
|
what is postural hypotension |
When a personstands up, gravity is going to pull down on the venous blood and as veins arecompliant, blood will pool in the lower limb veins. This is called venouspooling and the veins will distend and pressure will increase as the bloodpushes against the walls. Thisresults in much less blood going back to the heart, there is reduced CVP and soreduced filling and lower SV. This leads to a drop in blood pressure |
|
|
what is the effect of postural hypotension on teh brain |
Drop in CVP-> Will decrease right stroke volume -> Will decrease left ventricularfilling pressure (as less flowing back into heart)-> Decreased left strokevolume -> Decreased arterial pressure (due to decrease CO) -> Decreased cerebral blood flow. The decreasedcerebral blood flow will lead to a decreased O2 supply to the brain,the individual may get dizziness, visual fade and may syncope. |
|
|
what is Vasospasm |
a condition in which an arterial spasm leads to vasoconstriction itcan have the same effect as a blockage and cause ischaemia. |
|
|
what is cerebral artery vasospasm and why is it dangerous |
arterial spasm of cerebral artery leading to vasoconstriction. Vasospasmwill reduce blood flow significantly and this can cause a stroke (cerebralinfarct) |
|
|
what causes Vasospasmof extracerebral arteries |
Vasospasm ofextracerebral arteries is triggered by subarachnoid haemorrhage (a type ofextracerebral haemorrhage), due to the body trying to prevent blood loss. |
|
|
what local vasoconstrictor agents are involved in vasospasm |
-> 5-HT fromperivascular nerves ->Neuropeptide Y from perivascular nerves ->Endothelin-1 released from the vascular endothelium -> K+ions may be released from damaged cells, if they go up extremely high,=vasoconstriction as it depolarises VSMCs,this will activate vgCa2+. |
|
|
what can be used to reduce vasospasm |
-> vgCa2+blockers (e.g. amlodipine, acting on VSM) -> ETAreceptor blockers e.g. bosentan. |
|
|
what are the two types of strokes |
ischaemic (80%) haemorrhagic (20%0 |
|
|
what can cause ischaemic stroke |
-> Caused bya cerebral artery thrombosis or embolism -> Due toatheroma (often) -> Transientischaemic attacks may be caused by small arterial emboli being shed from anatheromatous carotid/vertebral artery. TIAs resolve in hours between episodes. |
|
|
what can cause haemorrhagic stroke. what causes neurological damage in this case |
Common cause isrupture of a microaneurysm ->Neurological damage is due in part to the triggered vasospasm, not just loss ofblood |
|
|
what is the effect of a space occupying lesion |
space occupying lesion = increased intracranial pressure. brainwill move and expand to try and relieve pressure on its structures. Potentially itcan move downwards through the foramen magnum, the increased pressure can pushdown and compress the RVLM in the medulla. |
|
|
how does brain try to maintain bf to it even when under increased intracranial pressure (eg in space occupying lesion) |
space occupying lesion = increased intracranial pressure. brain will move and expand to try and relieve pressure on its structures. Potentially, can move downwards through the foramen magnum. the increased pressure can pushdown and compress the RVLM in the medulla. In response tothis compression there will be increased activity of the RVLM, so this meansthere will be increased sympathetic vasoconstrictor activity, which willincrease TPR (arterioles) and HR + SV (heart). This willincrease BP! |
|
|
why may a person with a space occupying lesion present with high blood pressure (acute hypertension) but reduced heart rate. |
space occupying lesion = increased intracranial pressure.brain will move and expand to try and relieve pressure on its structures. potentially move through foramen magnum -> press on RVLM -> lead to increased activity of RVLM -> increased vasocontricor activity and inc HR/SV -> get inc blood pressure. higher BP will activate baroreflex will increasevagal activity to the heart causing the HR to decrease. This is reflexbradycardia. |
|
|
what drugs may cause postural hyptension |
medications can cause orthostatic hypotension, particularly drugs used to treat high blood pressure — diuretics, beta blockers, calcium channel blockers and angiotensin-converting enzyme (ACE) inhibitors |

