![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
213 Cards in this Set
- Front
- Back
|
What is hematopoiesis?
|
Refers to the production of all blood cells
|
|
|
What happens during hematopoiesis (general)?
|
Pluripotent stem cell gets signals from the blood to start differentiating and goes to lymphoid cells (T lymphocyte & B lymphocyte) or myeloid (RBCs, neutrophils, platelets)
|
|
|
Explain the embryological development of hematopoietic cells.
|
Hematopoietic cells initially arise in the yolk sac, move into the fetal liver and then go to the bone marrow.
|
|
|
Where do most lymphoid cells develop further after leaving the bone marrow?
|
Cloacal bursa, thymus
|
|
|
What is the general process of RBC maturation?
|
Stem cells--->rubriblast--> prorubricyte--> rubricyte---> metarubricyte--> reticulocyte--> mature RBC
|
|
|
*What is the major growth factor that regulates RBC production (maturation)?
|
Erythropoietin-stimulates RBC maturation
|
|
|
*Where is erythropoietin produced?
|
Peritubular cells of the kidney
|
|
|
What is the general trend of the histologic appearance of RBCs during maturation?
|
Stem cells are big and round then the cell gets small but is still big and round w/ a round nucleus, when get to early erythroblast can pick them out in bone marrow
-Immature cells have delicate, fine nuclear chromatin which gradually becomes coarsely clumped or condensed. -Size of nucleus decreases and nucleoli are lost |
|
|
When is erythropoietin released from the kidneys?
|
In response to hypoxia sensed by the renal cells, erythropoietin goes to the bone marrow
|
|
|
What is a Howell-jolly body?
|
A small fragment of nucleus that remained after the nucleus was extruded from the metarubricyte.
|
|
|
What makes reticulocytes stain with new methylene blue?
|
When vital stains (those that are taken up by living cells) such as new methylene blue is used on reticulocytes, the leftover mRNA of the ER is precipitated and forms a reticular pattern
|
|
|
Where are reticulocytes normally located?
|
Normally stay in bone marrow storage pool for 3 days completing hemoglobin synthesis
|
|
|
How long does it take for a stem cell to become a mature erythrocyte in circulation?
|
About 5 days
-So may take a few days to figure out if anemia is regenerative or not |
|
|
What is the difference b/w a reticulocyte and a polychromatophilic RBC?
|
Essentially the same thing, both are immature RBCs but a reticulocyte uses a new methylene blue stain and a polychromatophilic RBC implies a Wright stain is used.
|
|
|
*What domestic animal does not produce reticulocytes in times of high oxygen demand?
|
Horses
-So can't say if anemia is regenerative or non-regenerative by RBC indices |
|
|
What can cause an increase in the number of nucleated RBCs in circulation?
|
1. Splenic dysfunction
2. Splenic Neoplasia 3. Regenerative anemia 4. Hematopoietic neoplasia 5. Lead poisoning |
|
|
True or false. Nucleated RBCs are cells that are even less mature than polychromatic RBCs.
|
True
|
|
|
Why can splenic dysfunction result in nucleated RBCs in circulation?
|
Nucleated RBCs are seen as foreign to the macrophages in the spleen so remove them
|
|
|
How does lead poisoning cause increased nucleated RBCs in circulation?
|
Paralyzes some enzymes that normally produce hemoglobin; toxic effects on bone marrow
|
|
|
What is the RBC membrane comprised of?
|
Cholesterol and a variety of phospholipids
|
|
|
Why can there be an antibody response to RBCs?
|
The proteins in the RBC membrane can act as antigens
|
|
|
What maintains the membrane integrity of a RBC?
|
Cytoskeleton- can be affected by some disorders
|
|
|
Why is RBC deformability so crucial to survival?
|
Because RBCs are wider than the width of most capillaries
|
|
|
What does the ability of a RBC to deform depend on? (3)
|
1. Cell surface: cell volume
2. Membrane properties 3. Hemoglobin viscosity (internal contents) |
|
|
How do RBCs generate energy?
|
Use metabolic pathways
e.g. glycolysis & pentose phosphate pathway |
|
|
What are the 4 main metabolic pathways of RBCs?
|
1. Glycolysis
2. Pentose phosphate pathway 3. Rapaport-Luebering pathway (AKA DPG shunt) 4. Methemoglobin Reductase pathway |
|
|
What is the energy source of most RBCs?
|
Glucose
|
|
|
What do RBCs produce to protect themselves from oxidative stress?
|
NADPH & NADH
|
|
|
What is the function of the Pentose Phosphate pathway?
|
Metabolizes glucose and produces NADPH.
-NADPH helps to protect hemoglobin from oxidative stress |
|
|
What happens when an animal has an inherited defect in glycolytic enzymes?
|
Can cause hemolytic anemia
-Bc RBCs lack energy from glycolysis? |
|
|
What is the purpose of the Rapaport-Luebering pathway?
|
DPG shunt-produces DPG at the expense of ATP
|
|
|
What is the function of the methemoglobin reductase pathway?
|
Prevents accumulation of methemoglobin (non-functional form of hemoglobin); necessary to keep the heme iron in the functional ferrous (Fe++) state
|
|
|
What happens to an animal when methemoglobin is increased?
|
Animal may become cyanotic with muddy brown looking mucous membranes and blood
|
|
|
What is the primary function of RBCs?
|
Uses hemoglobin for oxygen transport
|
|
|
True or false. Hemoglobin only transports oxygen.
|
False, also transports some CO2
|
|
|
Where is hemoglobin synthesized?
|
Within developing RBCs
|
|
|
What happens to the affinity of hemoglobin for oxygen once it binds the first oxygen molecule?
|
Binding of oxygen to hemoglobin is cooperative i.e. the binding of oxygen at one heme facilitates the binding of oxygen to the other hemes
|
|
|
What is the P50?
|
The partial pressure of oxygen at which hemoglobin is half saturated with oxygen
|
|
|
What happens to the p50 and the dissociation curve when there's increased oxygen affinity?
|
P50 falls and the dissociation curve shifts to the left
|
|
|
What does it mean if the oxygen dissociation curve shifts to the left?
|
Oxygen remains bound to hemoglobin at a lower partial pressure of oxygen
|
|
|
What is the structure of hemoglobin?
|
4 amino acid chains each with a central heme group
|
|
|
What happens to hemoglobin when oxygen leaves?
|
When heme groups unload oxygen, the beta chains are pulled apart, and this allows the entrance of 2,3-DPG, which cross-links the beta chains and stabilizes the deoxy form of hemoglobin
-Also causes decreased affinity for O2 |
|
|
What happens to the structure of hemoglobin when oxygen is uptaken?
|
Bonds are broken and 2,3-DPG is expelled and the affinity for oxygen is increased
|
|
|
What does it mean for hemoglobin when the DPG levels are high?
|
More DPG makes it easier for Hb to release O2
|
|
|
What happens to the oxygen dissociation curve if there's decreased oxygen affinity?
|
Shifts to the right, so easier for O2 to unload
|
|
|
What 4 factors can cause the oxygen dissociation curve to shift to the right?
|
1. Increased 2,3-DPG
2. Increased CO2 3. Increased temp 4. Decreased pH |
|
|
What 4 factors can cause the oxygen dissociation curve to shift to the left?
|
1. Decreased 2,3-DPG
2. Decreased CO2 3. Decreased Temp 4. Increased pH |
|
|
What is the heme molecule comprised of?
|
Iron & protoporphyrin iX
|
|
|
What is hemoglobin comprised of?
|
Globin chains + heme molecule
|
|
|
*What regulates the iron content of the body?
|
Rate of absorption from GI tract (not excretion!)
|
|
|
What is the rare situation where an animal may lack dietary iron?
|
Clostrum in milk isn't very high in iron so in neonates such as piglets that don't eat off the ground
|
|
|
How is iron transferred in plasma?
|
The protein transferrin
|
|
|
What regulates the rate of iron absorption from the GI tract?
|
Iron stores
Erythropoiesis rate |
|
|
What's the main site of iron storage?
|
Liver
|
|
|
What does the serum iron levels measure?
|
Transferrin + iron
|
|
|
What does serum transferrin measure?
|
Total iron binding capacity (TIBC)
|
|
|
What is the percent saturation of transferrin? What's normal?
|
How much transferrin is bound to iron, usually 1/3
|
|
|
What does the serum ferritin measure?
|
Circulating storage pool of iron
|
|
|
What does it mean if the percent saturation of transferrin is less than 1/3?
|
There's not enough iron present to be bound by transferrin
|
|
|
What is hemosiderin?
|
A storage form of iron that is less available compared to ferritin stores
-typically iron stuck in spleen and bone marrow |
|
|
True or false. Hemosiderin is not tested clinically.
|
True
|
|
|
What is the medical term for black stool?
|
Melena
|
|
|
What is anisocytosis?
|
Variation in cell size, usually from younger cells leaving the bone marrow
|
|
|
What is the medical term for low serum iron?
|
Hypoferremia
|
|
|
How can you identify iron deficiency (loss or decreased uptake) using laboratory tests?
|
Decreased serum iron
Increased or normal TIBC Decreased serum ferritin Microcytosis develops as RBCs keep dividing due to lack of a full hemoglobin content |
|
|
What can cause a shift of iron to storage sites?
|
Chronic Inflammation
|
|
|
What 2 things can cause hypoferremia?
|
Iron deficiency
Shift of iron to storage sites |
|
|
How can you identify a shift of iron to storage sites using laboratory testing?
|
Decreased serum iron
Decreased TIBC Increased serum ferritin |
|
|
What type of anemia is typical with acute bleeding? Chronic?
|
Acute- Regenerative anemia bc there's no problem with the bone marrow
Chronic-can result in non-regenerative because run out of iron storage to make RBCs |
|
|
What is a fecal occult blood test?
|
Tests for blood in the feces
|
|
|
What is the rough life span of a RBC?
|
2-5 months
Dogs-110 days Cats-68 days Humans-128 days Horses-140 days Cattle-160 days |
|
|
What triggers erythrocyte breakdown?
|
Changes in cell membrane (less deformable) and cell enzymes
|
|
|
How are most RBCs removed from circulation?
|
Extravascular destruction-splenic macrophages
|
|
|
During extravascular destruction, what components are RBCs broken down to?
|
Globin, heme & free iron
|
|
|
What happens to the freed iron that results from extravascular destruction of RBCs?
|
Either returned to plasma transferrin or stored within the macrophage as ferritin or hemosiderin
|
|
|
What happens to the heme group produced by extravascular destruction of RBCs?
|
Broken down to bilirubin and is carried by albumin to the liver, where it is conjugated to form the glucuronide and excreted into bile
|
|
|
True or false. About 15% of RBCs are broken down by intravascular destruction.
|
False, <10%
|
|
|
What happens to the hemoglobin released into circulation after intravascular destruction?
|
Hemoglobin released directly into circulation is unstable and dissociates into dimers that bind to haptoglobin-this can be removed by macrophages in circulation.
|
|
|
What causes hemoglobinuria?
|
The binding capacity of the haptoglobin is exceeded so unbound hemoglobin dimers are filtered out through the renal glomerulus. This hemoglobin can be resorbed or when tubular uptake capacity is exceeded it can be excreted as free hemoglobin in the urine=hemoglobinuria
|
|
|
How can you identify intravascular hemolysis from a urinalysis?
|
Look for hemoglobinuria and hemoglobinemia (pink or red plasma)
|
|
|
What happens to the bilirubin produced by intravascular hemolysis?
|
Same as extravascular hemolysis, goes to the liver and is conjugated then excreted as fecal urobilinogen
|
|
|
What tests can be used to evaluate the erythron?
|
-PCV or hematocrit
-Hemoglobin -RBC count -Indices -Morphology -Reticulocyte count -Coombs' test |
|
|
What is the difference b/w a hematocrit and a PCV?
|
Really the same thing- % of whole blood made up of RBCs, but considered a PCV when manually done and a hematocrit when use an automatic hematology analyzer
|
|
|
True or false. Differences b/w a PCV and a hematocrit reflect the patient.
|
False, they don't reflect the patient-why you should use the same test each time to monitor patient
|
|
|
How are hemoglobin levels generally measured?
|
Using an automated analyzer or spectrophotometer
|
|
|
What is a normal hemoglobin concentration for a dog?
|
1/3 of the hematocrit
|
|
|
True or false. Lipemia and Heinz bodies do not affect a hemoglobin measurement.
|
False, they will artifactualy affect the assay bc affect the light used to measure Hb
|
|
|
How are RBC counts most often performed?
|
Automated hematology analyzer
-Manual counts w/ a hemocytometer and microscope can be performed |
|
|
What are the RBC indices?
|
MCV: mean RBC size
MCHC: mean corpuscular hemoglobin concentration MCH: mean corpuscular hemoglobin RDW: red cell distribution width |
|
|
What does the mean corpuscular hemoglobin reflect?
|
The weight of hemoglobin in an average RBC
|
|
|
What does the red cell distribution width tell you?
|
A way to quantitatively express the degree of anisocytosis or variation in RBC size
|
|
|
True or false. Central pallor is a normal feature of dog RBCs.
|
True
|
|
|
How large is a normal canine RBC?
|
7 microns
|
|
|
What animal normally has rouleaux of their RBCs?
|
Horses
-Can be seen in healthy cats |
|
|
What are spherocytes?
|
RBCs that are small, dense and round
|
|
|
What are spherocytes associated with?
|
Immune mediated hemolytic anemia
|
|
|
What are schistocytes?
|
RBC fragments
|
|
|
What are schistocytes associated with?
|
DIC, hemangiosarcoma, vasculitis
|
|
|
What is poikilocytosis?
|
Variation in cell shape
|
|
|
True or false. Goat RBCs are normally very small and can have marked poikilocytosis.
|
True
|
|
|
What animals have RBCs that are smaller than a dog's and have slight pallor?
|
Feline, equine, bovine
|
|
|
What are schistocytes?
|
RBC fragments
|
|
|
What are schistocytes associated with?
|
DIC, hemangiosarcoma, vasculitis
|
|
|
What is poikilocytosis?
|
Variation in cell shape
|
|
|
True or false. Goat RBCs are normally very small and can have marked poikilocytosis.
|
True
|
|
|
What is an echinocyte?
|
RBC which contains multiple evenly spaced, regular spicules.
|
|
|
What can cause echinocyte production?
|
Electrolyte abnormalities
Uremia Dehydration in vitro changes (artifact) |
|
|
What are acanthocytes?
|
RBC which contains 2 or more unevenly spaced blunt projections.
|
|
|
What is acanthocyte production associated with?
|
Splenic and hepatic disorders
e.g. hemangiosarcoma and liver disease |
|
|
What test should be done in an animal with high numbers of acanthocytes?
|
Biochem profile (bc related to splenic & hepatic disorders)
|
|
|
What are keratocytes?
|
RBCs with horn-like pointed projections.
|
|
|
What are blister and helmet cells?
|
The blister cell is a stage of keratocytes that preceeds the helmet cell-after the blister cell ruptures
|
|
|
What causes keratocyte formation?
|
Trauma to RBCs
e.g. Associatedw/ DIC, microangiopathic hemolytic anemia, portosystemic shunts, young cats |
|
|
What are codocytes (target cells)?
|
RBC containing dense, central area of hemoglobin
|
|
|
What causes target cell formation?
|
Metabolic disorders that affect the membrane-have an extra fold in membrane giving appearance
|
|
|
What are dacryocytes?
|
Tear shaped RBCs
|
|
|
What is dacryocytes formation associated with?
|
May be artifact or seen in bone marrow disease
|
|
|
What are stomatocytes?
|
RBCs with a mouth-like clear opening near the center-looks like the RBC is smiling or frowning.
|
|
|
What causes stomatocyte production?
|
Artifact or hereditary stomatocytosis in malamutes
|
|
|
How can you differentiate b/w dacryocytes that are artifact and those that are actually present in the blood?
|
Artifact: looks like tails all go the same direction
|
|
|
*What are punctate reticulocytes?
|
In cats only
Older-have been in circulation for up to 3 weeks so don't reflect current bone marrow response. |
|
|
True or false. The presence of punctate reticulocytes means that anemia is regenerative.
|
False, if only punctate retics are present then not regenerative because they are old and can be in circulation for as long as 3 weeks.
|
|
|
How can you tell the difference b/w basophilic stippling and punctate reticulocytes?
|
Punctate reticulocytes are seen with new methylene blue stain
Basophilic stippling is seen with Wright's stain. |
|
|
True or false. Basophilic stippling may be seen in markedly regenerative anemia.
|
True
|
|
|
What is basophilic stippling?
|
Aggregates of RNA seen on Wright's stained blood smears
|
|
|
What is a normal reticulocyte % in dogs? Cats?
|
up to 1% in healthy dogs
up to 0.4% in healthy cats |
|
|
What is the corrected reticulocyte percentage?
|
Adjusts for the degree of anemia
-reticulocyte % x (Obs PCV/Norm PCV) -Anything >1% in dogs & >.4% in cats shows some signs of regeneration |
|
|
What is the absolute reticulocyte count?
|
Multiply reticulocyte percentage times the RBC count
|
|
|
Is the absolute reticulocyte count or reticulocyte percentage more accurate?
|
Absolute reticulocyte count
|
|
|
What is a normal absolute reticulocyte number for dogs that implies regenerative anemia? Cats?
|
Dogs:< 60,000/ul
Cats: < 15,000/ul |
|
|
What are Heinz bodies?
|
Aggregates of denatured hemoglobin caused by oxidative stress, which appear as small, round, basophilic blobs on the margin of the RBC
-Stain good w/ new methylene blue |
|
|
What kinds of reticulocytes do cats have?
|
Both aggregate and punctate reticulocytes
|
|
|
What does an increased reticulocyte count mean?
|
Indicates regeneration
|
|
|
Are reticulocyte counts more greatly increased with hemolytic anemia or blood loss?
|
Hemolytic anemia- because there are more raw materials available
|
|
|
What's the earliest you can expect to see reticulocytes to appear following an acute cause of anemia? The peak?
|
48-72 hours
Peak-7 days |
|
|
What does it mean if the reticulocyte count isn't increased when a dog is suffering from anemia?
|
Either isn't regenerative or hasn't had enough time to respond
|
|
|
What does the Coomb's test detect?
|
Immune-mediated hemolytic anemia
-Tests for excess complement or immunoglobulins on RBC surface |
|
|
How do you run a Coomb's test, what's negative and what's positive?
|
Wash patient RBCs and mix with Coomb's reagent
-If positive they agglutinate |
|
|
True or false. If a Coomb's test is negative than the animal doesn't have immune mediated hemolytic anemia.
|
False, false negatives occur, probably false positives too
|
|
|
What is regenerative anemia?
|
Anemia in which the accelerated bone marrow response is evident as an increase in the absolute number of reticulocytes, the MCV and the RDW.
|
|
|
When is the bone marrow examined in an anemic animal?
|
When anemia is non-regenerative
|
|
|
How is anemia defined?
|
Decreased in hematocrit, hemoglobin concentration, and RBC count.
|
|
|
What are 2 causes of regenerative anemia?
|
Blood loss
Hemolysis |
|
|
What are 2 general causes of non-regenerative anemia?
|
Lack of effective bone marrow production
Extra-marrow causes |
|
|
What are some of the clinical findings during a physical exam of an animal with anemia?
|
Pale mucous membranes, weakness, tachycardia & tachypnea
Icterus, hemorrhage, or hemoglobinuria may also be present |
|
|
What are 3 different methods for classifying anemia?
|
1. Classification by RBC indices
2. Classification according to bone marrow response 3. Classification according to the pathophysiologic mechanism |
|
|
How do you classify anemia based on indices (MCV & MCHC)?
|
Macrocytic, hypochromic
Microcytic, hypochromic etc. |
|
|
How do you classify anemia according to bone marrow response?
|
-Regenerative-significant reticulocytosis (takes at least 3 days)
-Non-regenerative-inadequate reticulocyte response |
|
|
True or false. An increase in nucleated RBCs without reticulocytosis does not constitute a regenerative response.
|
True
|
|
|
How can you classify anemia by the pathophysiologic mechanism?
|
Blood loss-Regenerative
Increased RBC destruction-regenerative Reduced/defective erythropoiesis-non-regenerative |
|
|
True or false. Proteins will not be lost with hemorrhagic anemia.
|
False, protein and RBCs are lost
|
|
|
What are some causes of blood loss (hemorrhagic) anemia?
|
Trauma, parasites, coagulation disorders, ulcers, neoplasia
|
|
|
How does acute blood loss affect protein levels?
|
-If internal hemorrhage protein is resorbed so normal or mildly decreased as it is resorbed
-Otherwise typically hypoproteinemic |
|
|
How long does RBC regeneration take?
|
At least 48-72 hours
|
|
|
What type of anemia do we see with chronic blood loss?
|
Hemorrhagic anemia is regenerative at first
-May become iron-deficient: microcytic, hypochromic non-regenerative anemia |
|
|
What will the PCV and protein look like with hemolytic anemia?
|
PCV decreased
Protein normal |
|
|
Is hemolytic anemia regenerative?
|
Yes, highly regenerative
|
|
|
What are some clinical signs that may be associated with hemolytic anemia?
|
May have icterus, bilirubinuria or both
-w/ intravascular, may also have hemoglobinemia and hemoglobinuria |
|
|
Is RBC morphology helpful with hemolytic anemia?
|
Yes, spherocytes, Heinz bodies, parasites, acanthocytes
|
|
|
What is immune-mediated hemolytic anemia?
|
Accelerated destruction of RBCs due to presence of antibody or complement
|
|
|
Hemolytic anemia is common in what animals?
|
Relatively common in dogs-rare in other species
|
|
|
True or false. Immune-mediated hemolytic anemia has a high mortality.
|
True
|
|
|
What are the 4 criteria to diagnose immune-mediated hemolytic anemia?
|
1. Marked regenerative anemia
2. Autoagglutination (+/-) 3. Spherocytes 4. Positive Coombs' test |
|
|
What are 6 causes of hemolytic anemia other than immune-mediated?
|
1. Toxins
2. Mechanical injury-fragmentation 3. Inherited defects 4. RBC parasites 5. Oxidative injury 6. Hypophosphatemia |
|
|
What are some toxins that cause hemolytic anemia?
|
Zinc, copper, bacterial, snake, spider bite
|
|
|
What types of inherited defects cause hemolytic anemia?
|
Enzyme deficiencies
Membrane defects |
|
|
What are 4 parasites that can cause hemolytic anemia?
|
1. Mycoplasma hemofelis & haemominutum
2. Mycoplasma haemolamae 3. Babesia canis 4. Anaplasma marginale |
|
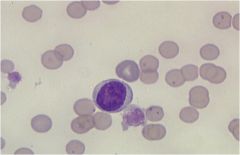
What blood parasite is this?
|
Mycoplasma haemofelis, can see the parasite on the surface of the RBC-tells macrophages cell is abnormal and get phagocytosis
|
|
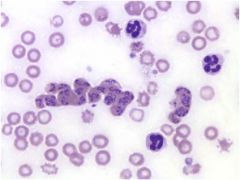
What blood parasite is this?
|
Babesia canis-can see little dots on surface of cells and get inside the RBCs-also causes destruction by macrophages
|
|
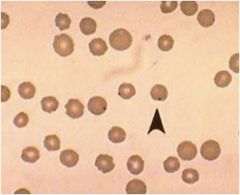
What blood parasite is this? How do you know?
|
Anaplasma marginale-can see little dot that looks like on the surface of the cell but also inside the cell
|
|
|
How can you tell the difference b/w Anaplasma marginale and a Howell-Jolly body?
|
Anaplasma marginale can have multiple organisms in one cell and tend to be on the margin of the cell, whereas howell-jolly bodies do not.
|
|
|
What are some compounds that cause oxidative injury?
|
Acetaminophen (Why toxic to cats), onions, garlic, red maple, copper toxicosis
|
|
|
What can cause hypophosphatemia, which results in hemolytic anemia?
|
Secondary to insulin
Post-parturient in cattle |
|
|
How do you know if a RBC has undergone oxidative injury?
|
The presence of Heinz bodies
|
|
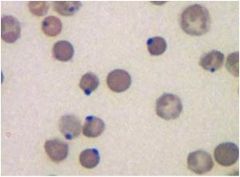
What is the structure on these RBCs?
|
Heinz bodies-mean the cell underwent oxidative injury
|
|
|
When an animal has anemia from reduced or ineffective erythropoiesis (non-regenerative), this implies that one of these four basic categories is lacking.
|
1. Normal stem, progenitor and precursor cells.
2. Normal stimulating/growth factors 3. Normal nutrients (e.g. iron) 4. Normal microenvironment-bone marrow |
|
|
When an animal has anemia from reduced or ineffective erythropoiesis, what should you be looking for in the bone marrow?
|
Decreased erythropoiesis in the marrow w/ abnormal-looking developing cells or abnormal maturation sequence
|
|
|
True or false. Nutritional deficiencies can actually result in increased erythropoiesis.
|
True, but the cells will be abnormal looking
|
|
|
What are the 4 classifications of anemias from reduced or ineffective erythropoiesis based on RBC indices?
|
1. Normocytic, normochromic anemia w/ normal or increased neutrophils and platelets
2. Normocytic, normochromic anemia w/ decreased neutrophils and platelets 3. Microcytic, hypochromic anemias w/ variable neutrophils and platelets 4. Macrocytic, normochromic anemias w/ variable neutrophils and platelets |
|
|
What are 4 causes of normocytic, normochromic anemia with normal or increased neutrophils and platelets?
|
1. Anemia due to lack of erythropoietin (EPO)
2. Anemia of inflammation 3. FelV-associated anemia 4. Immune-mediated anemia e.g. pure red cell aplasia |
|
|
What kind of anemia does renal failure result in?
|
Normocytic, normochromic anemias w/ normal or increased neutrophils and platelets
-Lack of erythropoietin |
|
|
How severe is anemia of inflammation? How common?
|
A common, usually fairly mild non-regenerative anemia
|
|
|
What is the pathogenesis of anemia of inflammation?
|
Related to the production of IL-6 and increased production of hepcidin by liver-this results in decreased transport of iron and inability of bone marrow to respond to EPO --> mild non-regenerative anemia
|
|
|
What does hepcidin do?
|
Stops ferroportin (a transmembrane protein that transports iron from inside to outside of a cell) stops release of iron stores
-Related to pathogenesis of anemia of inflammation IL-6--> hepcidin---> stops ferropotin---> increased iron storage--> anemia of inflammation |
|
|
True or false. FelV-associated anemia only causes normocytic, normochromic anemias with normal or increased neutrophils and platelets.
|
False, can be macrocytic or normocytic
|
|
|
What makes an immune-mediated anemia non-regenerative instead of regenerative?
|
Most immune-mediate anemias are regenerative, but if the antibody is directed against developing cells the anemia will be nonregenerative, normocytic and normochromic
|
|
|
What are 2 types of anemia that have RBC indices of normocytic and normochromic with pancytopenia (decreased neutrophils & platelets)?
|
Aplastic anemia
Myelophthistic anemia |
|
|
What is aplastic and myelopthistic anemia characterized by?
|
Pancytopenia in peripheral blood and marrow hypoplasia or marrow infiltration with abnormal cells.
|
|
|
What are 4 causes of aplastic anemia?
|
1. Infectious agents-Ehrlichia spp, FelV, parvovirus, FIV, chronic EIA
2. Drugs/toxins-estrogen, chemotherapy, bracken fern 3. Irradiation-in preparation for transplant 4. Idiopathic |
|
|
What is myelophthistic anemia?
|
Occurs when bone marrow is replaced by neoplastic cells or nonhematopoietic cells (myelofibrosis)
|
|
|
What are the 5 possible etiologies of microcytic, hypochromic or normochromic anemia w/ variable number of neutrophils and platelets?
|
1. Iron deficiency
2. Anemia of inflammation-if long standing see microcytosis 3. Portosystemic shunts 4. Pyridoxine (B6) & copper deficiency 5. Some breeds like akitas have microcytic RBCs normally |
|
|
True or false. Breeds like akitas who have normally microcytic cells are in a constant state of anemia.
|
False, not anemic
|
|
|
What will you see in iron tests for an animal with iron deficiency anemia?
|
Decreased serum iron & ferritin
TIBC normal to increased Sometimes thrombocytopenia |
|
|
What will you see in the iron tests for an animal with anemia of inflammation?
|
Serum iron will be decreased but serum ferritin is increased
|
|
|
What is the definition of polycythemia?
|
An increase in the hematocrit, hemoglobin, and RBC count.
|
|
|
What are 5 possible etiologies of macrocytic, normochromic anemia with variable neutrophils and platelets (non-regenerative)?
|
1. Vitamin B12 and folic acid deficiency (more in humans)
2. FeLV infection 3. Congenital dyserythropoiesis of Herefords 4. Erythroid neoplasia 5. Poodles can have macrocytosis as a breed disorder |
|
|
Does FeLV infection result in regenerative or non-regenerative anemia?
|
Non-regenerative, cats may be severely anemic but lack reticulocytosis
|
|
|
What are the 2 types of polycythemia? Which is most common?
|
Relative-most common
Absolute |
|
|
What is the erythron mass with relative polycythemia? Absolute polycythemia?
|
Relative- Normal
Absolute-Increased |
|
|
What are the 2 causes of relative polycythemia?
|
Splenic contraction
Dehydration |
|
|
What will you see on the blood work of an animal that's dehydrated?
|
Increased hematocrit
Increased hemoglobin Increased RBC count Increased total protein |
|
|
What are the 2 types of absolute polycythemia?
|
Primary absolute (polycythemia vera-neoplasia of RBCs)
Secondary absolute |
|
|
What causes primary absolute polycythemia?
|
This is a myeloproliferative disease with unregulated production of erythrocytes
-Neoplasia of RBCs |
|
|
What are the erythropoietin levels of primary absolute polycythemia?
|
Normal to decreased
|
|
|
What are the 2 types of secondary absolute polycythemia?
|
Appropriate polycythemia
Inappropriate polycythemia |
|
|
What causes appropriate polycythemia?
|
Associated with chronic hypoxia of cardiac and/or pulmonary disease that leads to increased erythropoietin production
|
|
|
How can you diagnose appropriate polycythemia that's not related to blood work?
|
Check PaO2 levels-they will be low
|
|
|
What is inappropriate polycythemia associated with?
|
Paraneoplastic EPO-like production or renal cysts which cause increased EPO production
|
|
|
What type of polycythemia develops when an animal is at a high altitude?
|
Appropriate polycythemia (secondary absolute polycythemia)
|
|
|
How can you distinguish b/w inappropriate polycythemia and appropriate polycythemia?
|
Appropriate polycythemia will have decreased pO2 and inappropriate will have normal pO2
|
|
|
As a general rule regenerative anemias due to hemorrhage or hemolysis will be either ______ & _____ or normocytic & normochromic.
|
Macrocytic and hypochromic
OR Normocytic and normochromic |
|
|
What should you do if you get the blood work back on an animal and it has microcytosis, hypochromasia and iron deficiency anemia?
|
Check for evidence of bleeding into the GI tract (tarry stool/melena) and internal or external parasites
|
|
|
When you see a mild non-regenerative anemia what should be high on your differentials?
|
Anemia of inflammation
-Most common cause of anemia especially normochromic normocytic mild non-regenerative anemia |

