![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
145 Cards in this Set
- Front
- Back
- 3rd side (hint)
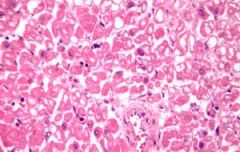
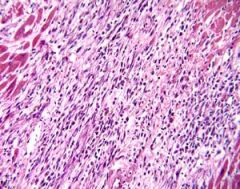
A 56-year-old man experienced chest pain and was admitted to the hospital suffering from an acute myocardial infarction. Five days later, he developed ventricular tachycardia, which progressed to ventricular fibrillation, and could not be resuscitated. The microscopic section shows an area of myocardium between an established infarct and normal myocardium. The myocytes in the figure show
A. cell injury with undetermined ultimate fate B. early coagulation necrosis C. early liquefaction necrosis D. irreversible injury and will die within hours |
Option A (cell injury with undetermined ultimate fate) is correct. The cells show vacuolation due to loss of the ability to synthesize ATP via aerobic respiration. This, in turn, shuts down the Na+-K+ pump of the cell membrane. Sodium is no longer excluded from the cytosol, and water follows it into the cell, causing swelling and vacuolation. This is a reversible process.
|
Option B (early coagulation necrosis), Option C (early liquefaction necrosis), and Option D (irreversible injury and will die within hours) are incorrect. No signs of necrosis are present in the myocytes. Although the cells show injury, there is no change visible on light microscopy that can be used to diagnose irreversible cell damage and impending cell death.
|
|
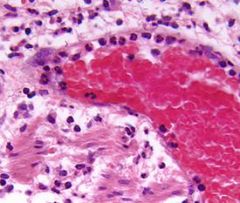
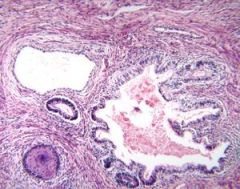
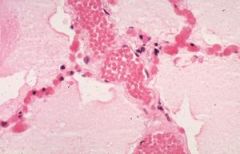
The photomicrograph shows subserosal connective tissue taken from the appendix of a 7-year-old girl suffering from acute appendicitis with a fibrinopurulent exudate coating the serosal surface. The neutrophils within this venule show evidence of
A. apoptosis B. diapedesis C. margination D. pavementing E. rolling |
Option D (pavementing) is correct. At the pavementing stage, the neutrophils are tightly adherent to the endothelium and are preparing to pass through it by diapedesis.
|
Option A (apoptosis) is incorrect. Many of the neutrophils eventually undergo apoptosis, but at this stage none show characteristic morphologic changes, such as nuclear fragmentation.
Option B (diapedesis) is incorrect. None of the cells appear to be passing through the vessel wall, although they will eventually move through the wall. Option C (margination) is incorrect. During margination, the neutrophils move to the periphery of the flowing blood and are not adhering to the endothelium. Option E (rolling) is incorrect. At this stage, the neutrophils are still moving along the vessel, but have begun to adhere to the endothelium. |
|
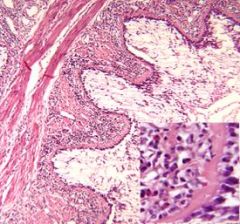
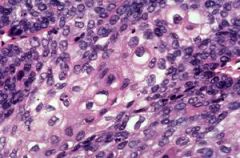
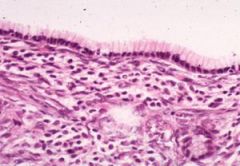
The photomicrograph shows the diseased bronchus of a 42-year-old woman who died of acute respiratory failure. The histologic appearance of this bronchus is a result of which of the following?
A. Acute viral pneumonia B. Bronchiectasis C. Centriacinar emphysema D. Chronic bronchitis E. Extrinsic asthma |
Option E (extrinsic asthma) is correct. The inflammation seen in the diseased bronchus includes numerous eosinophils, thickening of the basement membrane, stellate folding of the mucosa, smooth muscle hypertrophy, and mucous plugging of the lumen, all of which strongly suggest disease caused by extrinsic asthma.
|
Option A (acute viral pneumonia) is incorrect. Viral pneumonia generally leads to a chronic interstitial inflammatory response, with varying degrees of destruction of the mucosal epithelium.
Option B (bronchiectasis) is incorrect. Bronchiectasis is a necrotizing infection that ultimately destroys much of the bronchial wall. Option C (centriacinar emphysema) is incorrect. Centriacinar emphysema is a disease primarily of the respiratory bronchioles in which the walls of the bronchioles have been destroyed, producing large air spaces in the central portion of pulmonary acini. Option D (chronic bronchitis) is incorrect. Chronic bronchitis tends to result in hypersecretion of mucus and in bronchial gland hypertrophy. |
|
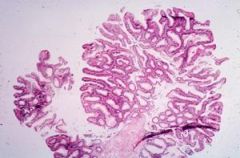
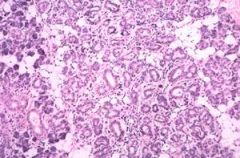
The 6-mm lesion shown in the photomicrograph was removed from the sigmoid colon of a 49-year-old man. A molecular examination of the DNA of the cells of the lesion would show
A. activation of K- B. deletion of DCC C. hypomethylation D. inactivation of RB1 E. loss of p53 |
Option C (hypomethylation) is correct. Hypomethylation of DNA is one of the earliest genetic changes in the development of colonic cancer, and may be present when no histologic abnormalities are detectable. As additional genetic errors occur, the cells will become more atypical.
|
Option A (activation of K-) is incorrect. Although K- is the most commonly activated oncogene in the development of colon cancer, its activation is found in about only 10% of tumors less than 1 cm in diameter.
Option B (deletion of DCC) is incorrect. DCC is no longer believed to play a role in the oncogenesis of colon cancer. It may be a marker for another, as yet uncloned, tumor suppressor gene on the same chromosome. Option D (inactivation of RB1) is incorrect. RB1 is not one of the tumor suppressor genes associated with the development of colon cancer. Option E (loss of p53) is incorrect. In 70\\'9680% of cases of colon cancer, p53 is absent or mutated; it appears infrequently in adenomas. |
|

The gross specimen shows a section of bowel removed from a 16-year-old boy who has had diarrhea and cramping abdominal pain for the past year. The most accurate description concerning these lesions is that they
A. are almost always limited to the colon B. are limited to the mucosa and submucosa C. can occur at any level of the gastrointestinal tract D. typically involve the rectum |
Option C (can occur at any level of the gastrointestinal tract) is correct. The linear ulcerations seen in this specimen are characteristic of Crohn's disease, which can involve any area of the gastrointestinal tract from the oral cavity to the anus.
|
Option A (are almost always limited to the colon), Option B (are limited to the mucosa and submucosa), and Option D (typically involve the rectum) are incorrect. Crohn's disease is associated with increased incidence of colonic adenocarcinoma, but the incidence is about five- to six-fold greater than in patients who do not have the disease. On the other hand, patients with ulcerative colitis have a 20- to 30-fold increase in the incidence of colon cancer. Crohn's disease can occur anywhere in the gastrointestinal tract and may involve multiple areas and all layers of the bowel wall. Ulcerative colitis always involves the rectum.
|
|

The figure shows a gallbladder removed from a 67-year-old woman with a 3-year history of fatty food intolerance. There is no indication of acute cholecystitis. On dissection, there is a firm gray-white infiltrating lesion. The mean 5-year survival rate associated with this neoplasm is
A. 1% B. 10% C. 25% D. 50% E. 75% |
Option A (1%) is correct. Carcinoma of the gallbladder has a poor prognosis. Typically, the cancer is silent and is not discovered until it has already invaded the liver. Gallstones are found in up to 90% of cases. The 5-year survival rate of carcinoma of the gallbladder is about 1%. Option B,Option C , Option D, and Option E are incorrect. Refer to the discussion for Option A.
|
|
|

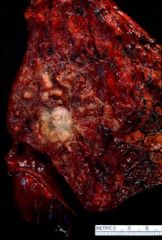
The figure shows a lung removed at autopsy from a 29-year-old man. Which of the following was most likely involved in the initial injury?
A. Alveolar type II pneumonocytes B. Capillary endothelium C. Clara cells D. Pleural mesothelium |
Option B (capillary endothelium) is correct. The photograph shows a lung in the fibrotic stage of adult respiratory distress syndrome (ARDS). In most cases of ARDS, the initial injury involves the capillary endothelium.
|
Option A (alveolar type II pneumonocytes), Option C (Clara cells), and Option D (pleural mesothelium) are incorrect. In a small minority of cases of ARDS, the original injury may involve alveolar type I pneumonocytes.
|
|
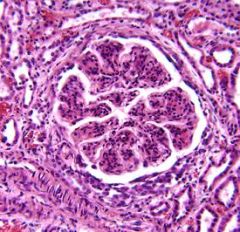
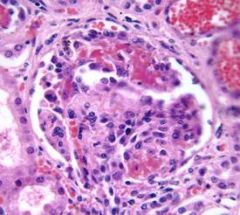
The pronounced glomerular changes shown in the figure occurred in a 24-year-old man with Goodpasture's syndrome. The presence of epithelial proliferation (crescents) in the glomerulus is best interpreted as
A. indication of rapid progression of glomerulonephritis B. loss of foot processes of the podocytes C. result of antiglomerular basement membrane antibodies D. result of deposition of immune complexes E. typical of poststreptococcal glomerulonephritis |
Option A (indication of rapid progression of glomerulonephritis) is correct. The presence of epithelial proliferation (crescents) is an indication of rapid progression of the disease.
|
Option B (loss of foot processes of the podocytes), Option C (result of antiglomerular basement membrane antibodies), Option D (result of deposition of immune complexes), and Option E (typical of poststreptococcal glomerulonephritis) are incorrect. The presence of epithelial proliferation, or crescents, is an indication of rapid progression that is not specific to any particular form of acute glomerulonephritis, and is a grave prognostic sign in any of type of this disease. If the condition is untreated, death from renal failure typically occurs in weeks to months.
|
|
The section shows a subpleural nodule from a primary malignancy of the lung of a 52-year-old woman who has never smoked cigarettes. The histologic classification of this tumor is
A. adenocarcinoma B. bronchoalveolar cell carcinoma C. malignant mesothelioma D. small-cell undifferentiated carcinoma E. squamous cell carcinoma |
Option A (adenocarcinoma) is correct. The most common primary malignancy in the periphery of the lung is an adenocarcinoma; however, other forms of lung cancer can occur in this location. To accurately identify this type of tumor, histologic or cytologic examination is necessary.
|
Option B, Option C, Option D, and Option are incorrect. Refer to the discussion for Option A.
|
|
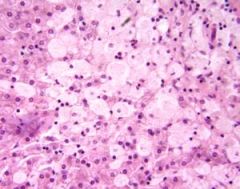
The photomicrograph shows a section of liver from an infant diagnosed with hepatosplenomegaly at 3 months of age. The hepatosplenomegaly progressed to generalized lymphadenopathy and deterioration of psychomotor function, and the infant died at 11 months of age. The large foamy cells show an accumulation of sphingomyelin primarily in which of the following cell structures?
A. Cell membrane B. Cytoplasm, diffusely C. Lysosome D. Mitochondrion E. Nucleus |
Option C (lysosome) is correct. The photomicrograph shows evidence of Niemann-Pick disease, a lysosomal storage disease caused by lack of sphingomyelinase. The net result is the accumulation of sphingomyelin within the lysosomes, which then become enlarged. The process eventually interferes with normal cellular function.
|
Option A, Option B, Option D, and Option E are incorrect. Refer to the discussion for Option C.
|
|
The photomicrograph shows a section of parotid gland taken from a 35-year-old man. Six months ago, he was found to have a stone completely obstructing Stensen's duct. The central portion of the image consists almost entirely of ducts and ductules. The lack of acinar tissue is a result of which of the following pathologic processes?
A. Atrophy B. Dysplasia C. Hyperplasia D. Hypertrophy E. Metaplasia |
Option A (atrophy) is correct. The acinar tissue is entirely absent from the center of the section, and has undergone almost complete atrophy as a result of the increased pressure within the parotid gland caused by the blocked salivary duct. The ducts are more resistant to this insult and are largely intact.
|
Option B (dysplasia) is incorrect. Dysplasia is a premalignant change in which the cells demonstrate atypical changes; it is suggestive of malignant transformation.
Option C (hyperplasia) is incorrect. Hyperplasia is an increase in the number of cells, and is clearly absent in this figure. Option D (hypertrophy) is incorrect. Hypertrophy is an increase in cell size, which is absent in this figure. Option E (metaplasia) is incorrect. Metaplasia is a change from one mature type of cell to another. |
|
The photomicrograph shows a section of myocardium taken from a 56-year-old man who suffered a myocardial infarction. This section of myocardium is an example of which of the following pathologic processes?
A. Coagulation necrosis B. Liquefaction necrosis C. Myocardial atrophy D. Myocardial hypertrophy E. Repair |
Option E (repair) is correct. The micrograph shows a fairly large focus of granulation tissue at an early stage of repair, which will eventually form scar tissue.
|
Option A (coagulation necrosis) is incorrect. Coagulation necrosis preceded the repair reaction that is now occurring. However, the necrotic cells have been removed.
Option B (liquefaction necrosis) is incorrect. Liquefaction necrosis takes place when the primary reaction is mediated by heterolysis from enzymes released by immigrant neutrophils that have migrated to the area Option C (myocardial atrophy) and Option D (myocardial hypertrophy) are incorrect. There is no evident of atrophy or hypertrophy. Granulation tissue occupies virtually all of the section. |
|
The photomicrograph shows a gonadal neoplasm from an 18-year-old man with a 2-month history of painless testicular enlargement. The neoplasm shows characteristics that would best classify it as
A. choriocarcinoma B. embryonal cell carcinoma C. seminoma D. teratoma E. yolk sac tumor |
Option D (teratoma) is correct. The micrograph shows elements derived from all three germ layers, which classifies it as a teratoma. Because all of the elements are mature and no evidence of neoplasia is apparent, this section represents a mature teratoma.
|
Option A (choriocarcinoma) is incorrect. Choriocarcinomas contain syncytiotrophoblastic differentiation (showing the characteristic multinucleated giant cells) and cytotrophoblastic differentiation.
Option B(embryonal cell carcinoma) is incorrect. Embryonal cell carcinomas are composed of nondescript masses of undifferentiated cells growing in a glandular, alveolar, or tubular pattern. Less well differentiated tumors would simply be sheets of cells. Option C (seminoma) is incorrect. Seminomas consist of sheets of large polygonal seminoma cells in an organoid pattern, separated by bands of connective tissue that often contains a dense infiltrate of lymphocytes. Option E (yolk sac tumor) is incorrect. Yolk sac tumors display a lace-like pattern with occasional primitive glomerulus-like Schiller-Duval bodies. |
|

14. The most likely source of the tumor nodules seen in this liver of a patient with painless hepatomegaly is
A. bile ducts B. gallbladder C. hepatic parenchymal cells D. hepatic vasculature E. metastases from a distant site |
Option E (metastases from a distant site) is correct. The innumerable tumor nodules with prominent umbilication suggests origin of circulating malignant cells derived from a primary tumor outside the liver. The most common malignancy in the liver is metastatic.
|
Option A (bile ducts), Option B (gallbladder), Option C (hepatic parenchymal cells), and Option D (hepatic vasculature) are incorrect. Although hepatomas may be multifocal, they tend to form large irregular nodules that resemble the hepatic parenchyma.
|
|
A 51-year-old man who has smoked two packs of cigarettes a day for 35 years has hemoptysis, a chronic cough, and an unintentional weight loss of approximately 14 kg (30 lb) over a period of 8 months. This radiograph of the chest shows a bulky perihilar mass in the upper lobe of the left lung. This tumor would most likely be classified as
A. adenocarcinoma B. giant cell carcinoma C. large cell undifferentiated carcinoma D. poorly differentiated squamous cell carcinoma E. small cell undifferentiated carcinoma |
Option D (poorly differentiated squamous cell carcinoma) is correct. The cells in the center of the section show keratinization as well as occasional prominent "gelatin" rings within the cytoplasm, which suggests squamous differentiation. Intercellular bridges are also evident.
|
Option A (adenocarcinoma) is incorrect. No glandular growth pattern is evident, and there is no evidence of mucin production. A diagnosis of adenocarcinoma cannot be made without finding some glandular feature. Option B (giant cell carcinoma) is incorrect. A giant cell tumor is usually much like large cell undifferentiated carcinoma, but a giant cell tumor contains anywhere from a few to numerous, very large multinucleated tumor cells
Option C (large cell undifferentiated carcinoma) is incorrect. Islands of squamous differentiation are present in large cell undifferentiated carcinoma. Option E (small cell undifferentiated carcinoma) is incorrect. A small cell carcinoma would consist of an irregular mass without discernible architecture consisting of innumerable, approximately lymphocyte-sized cells with scant cytoplasm. |
|
16. The photomicrograph shows histologic changes in the glomerulus of a 24-year-old man who died in acute renal failure from Goodpasture's syndrome. The arrows in the figure point to which of the following pathologic changes?
A. Caseous necrosis B. Coagulation necrosis C. Fat necrosis D. Fibrinoid necrosis E. Liquefaction necrosis |
Option D (fibrinoid necrosis) is correct. The micrograph shows changes characteristic of fibrinoid necrosis. Much of the staining quality comes from insudation of plasma proteins into the interstitium due to injury of the vascular wall. Fibrinoid necrosis is often seen in hypersensitivity disease as well as in malignant hypertension.
|
Option A (caseous necrosis), Option B (coagulation necrosis), Option C (fat necrosis), and Option E (liquefaction necrosis) are incorrect. The characteristic features of caseous necrosis, coagulation necrosis, fat necrosis, and liquefaction necrosis are absent. Refer to the discussion for Option D.
|
|
The photomicrograph shows the lung of a 73-year-old woman. The most common cause of the pulmonary finding shown in the figure is
A. hepatic failure B. ionizing radiation C. left ventricular failure D. nephrotic syndrome E. paraquat exposure |
Option C (left ventricular failure) is correct. The photomicrograph shows the lung of a patient with pulmonary edema. The most common cause of this disease is an increase in hydrostatic pressure within the pulmonary vasculature. Of the listed causes, left ventricular failure would be the most likely possibility.
|
Option A, Option B, Option D, and Option E are incorrect. Refer to the discussion for Option C.
|
|

The liver shown in the figure was removed from a 61-year-old woman at autopsy. Both kidneys showed similar changes, and a berry aneurysm was found in the circle of Willis. The changes are most consistent with which of the following disorders?
A. Adult polycystic kidney disease B. Familial juvenile nephrophthisis C. Infantile polycystic kidney disease D. Medullary cystic disease E. Medullary sponge kidney |
Option A (adult polycystic kidney disease) is correct. Adult polycystic kidney disease is an autosomal dominant disorder, characterized by massive enlargement of the kidneys, cysts in the liver, and frequently with aneurisms of the circle of Willis. Many patients with adult polycystic kidney disease also have cystic disease of the liver, as shown in the figure.
|
Option B (familial juvenile nephrophthisis), Option C (infantile polycystic kidney disease), Option D (medullary cystic disease), and Option E (medullary sponge kidney) are incorrect. Liver cysts and cerebral aneurysms are not expected findings in these diseases. |
|
19. The photomicrograph shows a section from the wall of a 15-cm, multiloculated cystic lesion found on the right ovary of a 37-year-old woman. The left ovary was free of any gross abnormality. The neoplasm would most likely be classified as
A. arrhenoblastoma B. dysgerminoma C. endodermal sinus tumor D. mucinous cystadenoma E. serous cystadenoma |
Option D (mucinous cystadenoma) is correct. The uniform simple mucin-producing epithelium confirms the diagnosis of mucinous cystadenoma. There is no microscopic atypia, and in the gross description, there is no mention of areas of papillary change or solid areas.
|
Option A (arrhenoblastoma), Option B (dysgerminoma), Option C (endodermal sinus tumor), and Option E (serous cystadenoma) are incorrect. Arrhenoblastomas and dysgerminomas are solid tumors and would not be expected to be large and cystic. Endodermal sinus tumors would be very atypical and form a lace-like pattern with occasional Schiller-Duval bodies.The lining epithelium of serous cystadenomas is not mucin-producing.
|
|

The photomicrograph shows a section of liver from a 68-year-old man who died of cor pulmonale. Which of the following serum values would most likely be associated with this hepatic change?
A. Amylase >200 U/L B. Creatinine kinase >500 U/L C. Lactate dehydrogenase >190 U/L |
Option C (lactate dehydrogenase >190 U/L) is correct. The photomicrograph shows central lobular necrosis of the liver produced by the increase in venous pressure, a result of a failing right ventricle. The injury to the hepatic cells allows enzymes, such as lactate dehydrogenase (LDH) and aspartate aminotransferase (AST or SGOT), to be released into the serum.
|
Option A and Option B are incorrect. Refer to the discussion for Option C.
|
|
|
. A 31-year-old woman has a mass on the right side of the neck lateral to the larynx. The mass is determined to be a well-differentiated tumor containing psammoma bodies. The tumor is most likely classified as a
A. follicular adenoma B. follicular carcinoma C. papillary adenoma D. papillary carcinoma |
Option D (papillary carcinoma) is correct. The presence of psammoma bodies is virtually diagnostic of papillary carcinoma, because these bodies are rarely seen in other thyroid neoplasms. Papillary carcinoma occurs most frequently in women between the ages of 20 and 50 years. Papillary carcinoma is the most common thyroid cancer and spreads via the lymphatic system. This type of thyroid cancer is more common in patients with a history of radiation exposure.
|
Option A (follicular adenoma) and Option B (follicular carcinoma) are incorrect. The papillary features of the tumor, such as psammoma bodies and clear nuclei, exclude these diagnoses.
Option C (papillary adenoma) is incorrect. Although some pathologists still use this term, it is now generally believed that all papillary neoplasms of the thyroid should be considered malignant. |
|
|
A total thyroidectomy is performed on a 42-year-old woman with a thyroid mass that appears to be encapsulated. There is evidence of both recent and past hemorrhage and numerous small, follicle-like structures composed of very uniform-appearing cells. Which of the following distinguishing features would suggest that this tumor is malignant?
A. Absence of papillary growth B. Absence of psammoma bodies C. Extension through the capsule D. Microfollicular pattern E. Presence of hemorrhage |
Option C (extension through the capsule) is correct. Invasion through the capsule of the tumor is one of the core characteristics used to determine if a follicular neoplasm of the thyroid is benign or malignant. Another characteristic is invasion of the tumor into the vasculature.
|
Option A (absence of papillary growth) and Option D (microfollicular pattern) are incorrect. These choices would only classify the lesion as a follicular neoplasm. Option B (absence of psammoma bodies) is incorrect. This would confirm that most likely this tumor is not a papillary neoplasm.
Option E (presence of hemorrhage) is incorrect. Hemorrhage is a frequent occurrence in follicular neoplasms of the thyroid, but it would not be a clue in determining if the tumor is benign or malignant. |
|
|
A 61-year-old man with chronic renal failure is being considered for a renal transplant. His serum calcium level is 7.6 mg/dL. Which of the following findings is most likely to be typical in this patient?
A. Bilateral adrenal hyperplasia B. Enlargement of all four parathyroid glands C. Functional parathyroid adenoma D. Hyperplasia of the adenohypophysis E. Hyperplasia of the thyroid follicular cells |
Option B (enlargement of all four parathyroid glands) is correct. The patient has secondary hyperparathyroidism associated with chronic renal failure. In such cases, the hypocalcemia caused by renal retention of phosphate leads to compensatory hyperplasia of the parathyroid glands. Typically, all four parathyroid glands are enlarged.
|
Option A (bilateral adrenal hyperplasia), Option D (hyperplasia of the adenohypophysis), and Option E (hyperplasia of the thyroid follicular cells) are incorrect. Chronic renal failure and low serum calcium level would not cause enlargement of the adrenal glands and neither is associated with hyperplasia of the follicular cells of the thyroid.
Option C (functional parathyroid adenoma) is incorrect. A functional adenoma would cause the other three parathyroid glands to atrophy, resulting in one large gland (with the adenoma) and three atrophic glands. |
|
|
Two months ago, a 19-year-old man was brought to the emergency department following an automobile accident in which he sustained severe lacerations and a ruptured spleen. He immediately received four units of packed red blood cells. He now has developed mild jaundice. Except for vague symptoms of fatigue, he is generally asymptomatic. Both his ALT (alanine aminotransferase) and AST (aspartate aminotransferase) are 40 U/L. His alkaline phosphatase is within normal limits. Which of the following types of hepatitis is most likely to have caused this infection?
A. Hepatitis A (HAV) B. Hepatitis B (HBV) C. Hepatitis C (HCV) D. Hepatitis D (HDV) E. Hepatitis E (HEV) |
Option C (hepatitis C) is correct. HCV has become the major cause of transfusion-related hepatitis since adequate screening methods for HBV have been developed. HCV was previously referred to as non-A, non-B hepatitis or chronic active hepatitis.
|
Option A (hepatitis A) is incorrect. HAV infection is virtually always transmitted through the fecal-oral route.
Option B (hepatitis B) is incorrect. HBV is a blood-borne disease and is no longer a major source of post-transfusion hepatitis since adequate screening methods for HBV have been developed. At present, HBV is transmitted most often by intravenous drug users using shared needles and through intimate sexual contact. Option D (hepatitis D) is incorrect. HDV requires the presence of HBV infection, because the HDV is defective and cannot replicate on its own. Option E (hepatitis E) is incorrect. HEV, an enteric virus, causes hepatitis via the fecal-oral route and is found primarily in developing countries. |
|
|
For the past several weeks, a 39-year-old woman has experienced fatigue, weakness, poor appetite, and weight loss. Physical examination shows hyperpigmentation of the skin and dark patches on the mucous membranes. Laboratory studies show her serum sodium level is 125 mEq/dL, and her serum potassium level is 6.0 mEq/dL. Which of the following is the most likely diagnosis?
A. Atrophic adrenals with dense lymphocytic infiltrate B. Carcinoid tumor of the vermiform appendix C. Functional follicular adenoma of the thyroid D. Granulosa cell tumor of the right ovary E. Hyperplasia of all four parathyroid glands |
Option A (atrophic adrenals with dense lymphocytic infiltrate) is correct. This patient has Addison's disease, as suggested by the fatigue, weakness, poor appetite, and weight loss. Other characteristics include hyperpigmentation of the skin and dark patches on the mucous membranes. In developed countries, the most common cause of Addison's disease is autoimmune destruction of the adrenals, suggested by lymphoid infiltrates in the adrenal glands plus circulating antiadrenal antibodies. In developing countries, tuberculosis would also be a major cause.
|
Option B (carcinoid tumor of the vermiform appendix) is incorrect. A carcinoid tumor limited to the appendix would be clinically silent. In any case, such a tumor does not produce the characteristics associated with Addison's disease.
Option C (functional follicular adenoma of the thyroid) is incorrect. This type of thyroid neoplasm would cause typical hyperthyroidism, not Addison's disease. Option D (granulosa cell tumor of the right ovary) is incorrect. A granulosa cell tumor would produce excess estrogen, not Addison's disease. Option E (hyperplasia of all four parathyroid glands) is incorrect. Hyperparathyroidism would cause hypercalcemia, not the electrolyte and pigmentation changes seen in this patient. |
|
|
For the past 6 months, an 18-year-old woman has had diarrhea, a fever, and cramping and left lower quadrant pain. Flexible sigmoidoscopy shows mucosal ulceration in the sigmoid colon. A biopsy shows transmural inflammation with occasional granulomas. Which of the following would differentiate Crohn's disease from ulcerative colitis?
A. History of fever B. History of prolonged diarrhea C. Involvement limited to the colon D. Presence of gross mucosal ulcerations E. Presence of transmural inflammation with granular formation |
Option E (presence of transmural inflammation with granular formation) is correct. Ulcerative colitis is essentially a disease of the mucosa, whereas Crohn's disease involves all layers of the bowel wall. A biopsy shows that this patient has transmural inflammation with occasional granulomas.
|
Option A (history of fever) is incorrect. Fever is a nonspecific symptom and can be associated with both ulcerative colitis and Crohn's disease.
Option B (history of prolonged diarrhea) is incorrect. Diarrhea is a symptom of both ulcerative colitis and Crohn's disease. Option C (involvement limited to the colon) is incorrect. Although ulcerative colitis is usually limited to the colon, this restriction does not differentiate between ulcerative colitis and Crohn's disease. Involvement of other parts of the gastrointestinal system, such as the small bowel and stomach, point to Crohn's disease. Option D (presence of gross mucosal ulcerations) is incorrect. Both ulcerative colitis and Crohn's disease, as well as some infectious processes such as amebiasis, can cause mucosal ulceration. |
|
|
A 56-year-old man with a history of gastric ulceration and Helicobacter pylori infection has a lesion involving the stomach wall. A biopsy shows that the lesion is a mucosa-associated lymphoid tissue (MALT) lymphoma. Which of the following is the most likely source of this tumor?
A. B cells B. Histiocytes C. Natural killer (NK) cells D. T cells |
Option A (B cells) is correct. Mucosa-associated lymphoid tissue (MALT) lymphomas are low-grade B-cell lymphomas. Gastric MALT lymphoma has a strong association with H. pylori infection.
|
Option B, Option C , and Option D are incorrect. Refer to the discussion for Option A.
|
|
|
. A 18-year-old woman with mildly icteric sclerae has a total bilirubin of 5.5 mg/dL and a direct bilirubin of 0.4 mg/dL. She has no associated symptoms, and no history of exposure to hepatotoxins, blood products, or persons with known hepatitis. A brother is unaffected, but an uncle has a similar condition. This patient most likely has which of the following congenital hyperbilirubinemias?
A. Crigler-Najjar syndrome, type I B. Crigler-Najjar syndrome, type II C. Dubin-Johnson syndrome D. Gilbert syndrome E. Rotor's syndrome |
Option D (Gilbert syndrome) is correct. Patients with this mild, inherited form of conjugated hyperbilirubinemia are healthy and have no functional or structural evidence of liver disease, except for an increase in unconjugated bilirubin.
|
Option A (Crigler-Najjar syndrome, type I) is incorrect. Patients who have this severe, recessively inherited disease generally die within their first year of life, unless they have a liver transplant.
Option B (Crigler-Najjar syndrome, type II) is incorrect. Patients with this form of Crigler-Najjar syndrome generally survive. Affected patients respond to treatment with phenobarbital, which lowers the level of unconjugated bilirubin. The type II form of Crigler-Najjar syndrome is less severe than type I. Option C (Dubin-Johnson syndrome) is incorrect. This form of conjugated hyperbilirubinemia is an autosomal recessive condition that is clinically innocuous. Patients with Dubin-Johnson syndrome will have a darkly pigmented liver. Option E (Rotor's syndrome) is incorrect. This form of conjugated hyperbilirubinemia is an autosomal recessive condition. Rotor's syndrome is clinically innocuous and may be distinguished from Dubin-Johnson syndrome by its lack of pigmentation of the liver. |
|
|
A 37-year-old woman complains of fatigue and intense itching. A physical examination is within normal limits. Laboratory studies show a marked increase in alkaline phosphatase, a slight increase in total bilirubin, and high-normal levels of ALT (alanine aminotransferase) and AST (aspartate aminotransferase). Serologic studies show increased IgM and circulating antimitochondrial antibody. A liver biopsy would most likely show which of the following changes?
A. Bile ducts surrounded predominantly by lymphocytes, some plasma cells, and occasional macrophages B. Deposition of large granules of brown pigment within the cytoplasm of the hepatocytes C. Marked fatty change of the centrilobular hepatocytes D. Piecemeal necrosis of the terminal plate of hepatocytes surrounding the portal tracts |
Option A (bile ducts surrounded predominantly by lymphocytes, some plasma cells, and occasional macrophages) is correct. The patient is suffering from early primary biliary cirrhosis. She has a marked increased in alkaline phosphatase, slight increase in total bilirubin, and high-normal ALT and AST levels. Studies also show an increase in IgM and in circulating antimitochondrial antibody.
|
Option B (deposition of large granules of brown pigment within the cytoplasm of the hepatocytes) is incorrect. This finding is characteristic of Dubin-Johnson syndrome.
Option C (marked fatty change of the centrilobular hepatocytes) is incorrect. This nonspecific finding can occur in reaction to many forms of injury, such as alcoholism. Option D (piecemeal necrosis of the terminal plate of hepatocytes surrounding the portal tracts) is incorrect. This finding is associated with hepatitis virus (HBV) infection. |
|
|
A 51-year-old man with an 8-year history of cirrhosis has a mass lesion in the left lobe of the liver. A needle biopsy determines the lesion is hepatocellular carcinoma (HCC). In the United States, development of HCC is most commonly associated with which of the following?
A. Alcoholism B. Exposure to aflatoxin C. Hepatitis C (HCV) infection D. Microvesicular steatosis E. Neonatal hepatitis |
Option C (hepatitis C infection) is correct. HCV infection is most commonly associated with hepatocellular carcinoma. There is a marked reduction of cases of hepatitis B (HBV) in the United States due to the screening of blood used for transfusions.
|
Option A (alcoholism) is incorrect. Although chronic alcoholics with cirrhosis are certainly at risk for the development of hepatocellular carcinoma, individuals who develop hepatocellular carcinoma have a very high prevalence of infection with HBV or HCV.
Option B (exposure to aflatoxin) is incorrect. In less developed countries, hepatocellular carcinoma is associated with exposure to food contaminated with aflatoxin. However, HBV is common in these areas. Aflatoxin is a toxic factor produced by Aspergillus flavus and A. parasiticus, molds containing seedlings of peanut plants. Option D (microvesicular steatosis) is incorrect. This condition is typically found in the liver of children with Reye's syndrome, but it has no relationship to hepatocellular carcinoma. Option E (neonatal hepatitis) is incorrect. This condition has no relationship with the development of hepatocellular carcinoma. |
|
|
A 12-year-old girl has metabolic acidosis and severe ketosis. Her blood glucose level is 460 mg/dL. Serologic studies for antibodies against b cells show a high titer of anti b cell antibodies. Which of the following is most significant concerning the finding of a high titer of these antibodies?
A. Are a serum marker for the destruction of b cells B. Are an indication of the development of type 2 diabetes mellitus C. Have caused the destruction of the b cells in the pancreatic islets D. Form a complex with insulin that causes hyperglycemia |
Option A (are a serum marker for the destruction of b cells) is correct. It is currently thought that anti b cell antibodies arise from antigens released into the blood by the destruction of b cells, probably by cytotoxic T cells. Thus, they are a marker, not a cause, of b cell injury.
|
Option B (are an indication of the development of type 2 diabetes mellitus),
Option C (have caused the destruction of the b cells in the pancreatic islets), and Option D (form a complex with insulin that causes hyperglycemia) are incorrect. There is no relationship between anti b cell antibodies and type 2 diabetes mellitus. |
|
|
A 62-year-old woman with bilateral palpable masses in her abdomen has a creatinine level of 3.7 mg/dL and her blood urea nitrogen (BUN) is 32 mg/dL. During the past year, she has had hematuria with occasional small blood clots in her urine. Which of the following is the most likely diagnosis?
A. Medullary sponge kidney B. Nephronophthisis C. Polycystic kidney disease, autosomal dominant D. Polycystic kidney disease, autosomal recessive E. Renal dysplasia |
Option C (polycystic kidney disease, autosomal dominant) is correct. This clinical scenario of bilateral palpable abdominal masses and marked increase in creatine and BUN represents a fairly classic presentation of autosomal dominant (adult) polycystic disease.
|
Option A (medullary sponge kidney) is incorrect. In this condition, the kidneys are not particularly enlarged.
Option B (nephronophthisis) is incorrect. Kidneys are smaller than normal in a patient with nephronophthisis. Option D (polycystic kidney disease, autosomal recessive) is incorrect. This form of polycystic kidney disease is rare in children. In the perinatal period, it is associated with a mortality of about 75%. Option E (renal dysplasia) is incorrect. Renal dysplasia is the most common cause of a unilateral abdominal mass in newborns. |
|
|
During a routine physical examination and urinalysis, microscopic hematuria is detected in the urine of an asymptomatic 21-year-old man. The hematuria resolves within 10 days, but recurs 1 month later. A needle biopsy of the right kidney shows mesangial hypercellularity. Immunofluorescence staining shows deposits of IgA scattered throughout the mesangial area. Which of the following descriptions of this condition is most accurate?
A. Deposits of IgA are monoclonal and suggest a malignancy in lymphoid organs B. Glomerular damage will proceed at a fast pace, leading to renal failure within 1 year C. IgA is directed against components of the glomerular basement membrane D. The condition is acute and self-limited E. Up to 50% of patients who have this condition eventually require a kidney transplant |
Option E (up to 50% of patients who have this condition eventually require a kidney transplant) is correct. The patient has IgA nephropathy, or Berger's disease. Recurring hematuria, deposits of IgA scattered throughout the mesangial area, and mesangial hypercellularity are all characteristics of Berger's disease.
|
Option A (deposits of IgA are monoclonal and suggest a malignancy in lymphoid organs) is incorrect. Instead, the deposits of IgA are polyclonal and probably represent trapped immune complexes.
Option B (glomerular damage will proceed at a fast pace, leading to renal failure within 1 year) is incorrect. This form of IgA nephropathy, or Berger's disease, is a slowly progressive condition that causes chronic renal failure over a period of about 20 years. Option C (IgA is directed against components of the glomerular basement membrane) is incorrect. In IgA nephropathy, known as Berger's disease, there is no suggestion that the IgA is directed against any particular glomerular structure. Evidence suggests that Berger's disease is an immune complex condition. Option D (the condition is acute and self-limited) is incorrect. Chronic renal failure does not ultimately develop in all patients with Berger's disease (an IgA nephropathy), but the condition tends to recur every few months. |
|
|
A 24-year-old woman has painful urination with frequency and urgency. A physical examination shows an increase in heart rate and a temperature of 39.2\'b0C (102.5\'b0F). She appears ill and somewhat diaphoretic. A urine specimen is grossly red, and red blood cells (RBCs) are seen on microscopic examination. A urinalysis shows bacteria, polymorphonuclear leukocytes, and leukocyte casts. A nitrite test on a urine dipstick is positive. Which of the following is the most likely diagnosis?
A. Acute pyelonephritis B. Acute tubular necrosis C. Cystitis D. Nephrotic syndrome |
Option A (acute pyelonephritis) is correct. Leukocyte casts are formed only in the kidneys, and the presence of these casts is ample evidence of an infection of the renal parenchyma, characteristic of acute pyelonephritis.
|
Option B (acute tubular necrosis) is incorrect. A patient with acute tubular necrosis would present with decreasing urine flow (oliguria) and not with fever, pus in the urine, and white blood cell casts.
Option C (cystitis) is incorrect. Bacteria can be characteristic of both cystitis and acute pyelonephritis, or they can be found in an improperly collected urine specimen from a healthy individual. RBCs can come from the bladder mucosa or the kidney. The presence of polymorphonuclear leukocytes is a nonspecific sign of a urinary tract infection and would not differentiate between bladder and kidney. Option D (nephrotic syndrome) is incorrect. Hematuria would not be found in nephrotic syndrome, but rather a massive loss of protein in the urine is characteristic of this disease. Leukocyte casts would not be present. |
|
|
A urinalysis of an asymptomatic 59-year-old man shows microscopic hematuria and mild prostatic hypertrophy. A CT scan of the abdomen shows a large mass in the left kidney. A needle biopsy confirms a diagnosis of renal cell carcinoma, clear-cell type. Radical nephrectomy indicates that the tumor appears to have invaded the man's left renal vein. If the tumor has metastasized, the most likely site of metastasis is
A. adrenal glands B. bones C. liver D. lungs E. regional lymph nodes |
Option D (lungs) is correct. Renal cell carcinoma is angioinvasive and tends to disseminate via the vascular system early in its history. If metastases occur, the lungs are involved in more than 50% of cases.
|
Option A (adrenal glands), Option B (bones), Option C (liver), and Option E (regional lymph nodes) are incorrect. The bones are the second most common site of metastasis of this tumor, and are involved about 33% of the time. Metastases to the adrenal glands, the liver, and regional lymph nodes do occur, but they are infrequent sites of metastasis.
|
|
|
A 16-year-old girl whose mother was given diethylstilbestrol (DES) during her pregnancy because of threatened abortion wants to be evaluated in anticipation of problems associated with her mother's medical history. Which of the following conditions would represent a risk as a result of maternal use of DES?
A. Adenocarcinoma of the Bartholin's glands B. Adenocarcinoma of the endometrium C. Adenocarcinoma of the vagina D. Squamous cell carcinoma of the cervix E. Squamous cell carcinoma of the vulva |
Option C (adenocarcinoma of the vagina) is correct. A small percentage of female children born to women treated with DES (< 0.14%) eventually develop adenocarcinoma of the vagina. The tumor is usually detected between 15 and 20 years of age. The tumor cells contain abundant glycogen producing a so-called clear-cell carcinoma.
|
Option A (adenocarcinoma of the Bartholin's glands), Option B (adenocarcinoma of the endometrium), Option D (squamous cell carcinoma of the cervix), and Option E (squamous cell carcinoma of the vulva) are incorrect. They have no known association with maternal use of DES. Refer to the discussion for Option C.
|
|
|
A 30-year-old woman fears that she will develop ovarian cancer because of her family history and is tested for the BRCA1 gene. This gene has a strong association with which of the following ovarian neoplasms?
A. Dysgerminoma B. Mixed M\'fcllerian tumor C. Serous cystadenocarcinoma D. Yolk sac tumor |
Option C (serous cystadenocarcinoma) is correct. In women who are positive for the BRCA1 gene, the vast majority of ovarian tumors are serous cystadenocarcinomas. A woman who has a family history of ovarian cancer would be at risk for carrying the BRCA1 gene.
|
Option A, Option B, and Option D are incorrect. Refer to the discussion for Option C.
|
|
|
A 50-year-old woman with an infiltrating ductal carcinoma of the breast has a lumpectomy, followed by adjuvant radiation and chemotherapy. Tissue is sent to the laboratory to determine if any prognostic factors might be present in this woman. Which of the following findings would be associated with an extremely poor prognosis for this patient?
A. Estrogen receptors B. HER-2 neu amplification C. Mutated p53 oncoprotein D. Progesterone receptors |
Option B (HER-2 neu amplification) is correct. Tumors with oncogene amplification (HER-2 neu) tend to have a less favorable prognosis than those without this factor.
|
Option A (estrogen receptors), Option C (mutated p53 oncoprotein), and
Option D (progesterone receptors) are incorrect. The presence of hormone receptors, such as estrogen and progesterone, is a favorable finding. The appearance of mutated p53 oncoprotein is a common genetic error found in many malignancies, but it would not necessarily suggest an unfavorable prognosis. |
|
|
A 55-year-old slightly obese woman has had several bouts of intense right upper quadrant pain and now has scleral icterus. A cholecystectomy shows numerous spongy, laminated brown stones in the gallbladder. Brown gallstones are almost always associated with which of the following conditions?
A. Alcoholic cirrhosis B. Escherichia coli infection of the gallbladder C. History of mild b-thalassemia D. Hypercholesterolemia |
Option B (Escherichia coli infection of the gallbladder) is correct. Brown gallstones are almost always associated with E. coli cholecystitis. Bacteria may secrete b-glucuronidase, which hydrolyzes conjugated bilirubin to unconjugated bilirubin. The increase in concentration of unconjugated bilirubin is believed to produce the stones.
|
Option A (alcoholic cirrhosis) is incorrect. Alcohol is actually somewhat protective against the formation of gallstones.
Option C (history of mild b-thalassemia) is incorrect. This form of anemia is a known precursor of black gallstones. Option D (hypercholesterolemia) is incorrect. Hypercholesterolemia is one of the risk factors for the development of cholesterol (yellow) gallstones. |
|
|
An endometrial biopsy of a 47-year-old woman with a history of irregular vaginal bleeding shows a well-differentiated adenocarcinoma of the endometrium. A hysterectomy confirms tumor involvement of the corpus of the uterus and the cervix. Which of the following is a known risk factor for the development of endometrial carcinoma?
A. History of anovulatory menstrual cycles B. History of cervical human papillomavirus (HPV) infection C. Multiple pregnancies D. Thin body habitus |
Option A (history of anovulatory menstrual cycles) is correct. A history of irregular vaginal bleeding corroborates anovulatory menstrual cycles and is strongly associated with the development of endometrial cancer, probably because of prolonged estrogen stimulation.
|
Option B (history of cervical human papillomavirus infection) is incorrect. There is no known association between HPV and endometrial carcinoma.
Option C (multiple pregnancies) is incorrect. Nulliparity has an association with the development of endometrial carcinoma Option D (thin body habitus) is incorrect. Excess body fat is associated with endometrial carcinoma due to its conversion of androgen precursors into estrogen. |
|
|
A 40-year-old woman has enlarged lymph nodes in the axillae, groin, and cervical triangles. Biopsy of an axillary node shows complete effacement of the architecture of the nodes by nodular aggregates of lymphoma cells. Which of the following is the cell line of origin of this type of lymphoma?
A. B cell B. CD4+ T cell C. CD8+ T cell D. Histiocyte E. Natural killer (NK) cell |
Option A (B cell) is correct. The woman has follicular (nodular) lymphoma, a non-Hodgkin's (NHL) lymphoma that expresses B cell cluster of differentiation (CD) markers. All follicular (nodular) lymphomas are of B cell lineage.
|
Option B (CD4+ T cell), Option C (CD8+ T cell), and Option D (histiocyte) are incorrect. Refer to the discussion for Option A.
Option E (natural killer cell) is incorrect. NK cells comprise 10\'9615% of peripheral blood lymphocytes. They lack both T cell and B cell markers. |
|
|
A 64-year-old woman with a saccular aneurysm of the ascending aorta has ataxia and loss of joint position sense. She confabulates when the physician attempts to obtain a history. Which of the following organisms is capable of producing this constellation of findings?
A. Chlamydia trachomatis B. Haemophilus ducreyi C. Neisseria gonorrhoeae D. Treponema pallidum E. Trichomonas vaginalis |
Option D (Treponema pallidum) is correct. An aortic aneurysm with ataxia and impaired proprioception are characteristic of the tertiary stage of syphilis. The primary stage involves a painless genital ulcer and regional lymphadenopathy, and the secondary stage involves skin and mucosal lesions as well as possible meningeal, hepatic, renal, bone, and joint invasion.
|
Option A (Chlamydia trachomatis) is incorrect. C. trachomatis is an increasingly common agent that transmits sexually transmitted diseases (STDs). It typically causes localized effects, such as scarring of the fallopian tubes.
Option B (Haemophilus ducreyi ) is incorrect. H. ducreyi is a gram-negative bacillus that causes the STD known as chancroid, an acute ulcerative infection of the skin. Option C (Neisseria gonorrhoeae) is incorrect. N. gonorrhoeae is a gram-negative diplococcus that causes gonorrhea and predominantly local effects with acute inflammation and scarring. In addition, the organism can enter the blood stream and cause skin lesions and joint infections. Option E ( Trichomonas vaginalis) is incorrect. T. vaginalis is a protozoal flagellate, a common agent that infects both males and females. It causes mild local effects, such as vaginal discharge. |
|
|
When asked to speak to a women's group about risk factors for the development of breast cancer, the physician should tell the group that the histopathologic finding that carries the strongest risk factor for developing breast cancer is
A. apocrine metaplasia B. atypical lobular hyperplasia C. epithelial hyperplasia D. sclerosing adenosis |
Option B (atypical lobular hyperplasia) is correct. Atypical lobular hyperplasia is a moderate risk factor for the development of breast cancer.
|
Option A (apocrine metaplasia), Option C (epithelial hyperplasia), and
Option D (sclerosing adenosis) are incorrect. At most, these histopathologic findings add only a slight risk for the development of breast cancer. |
|
|
Tumor cells from a 47-year-old woman with invasive carcinoma of the cervix are cultured and used for in vitro testing of potential chemotherapeutic agents. Normal fibroblasts placed in culture as a control at the same time die out after approximately 42 doublings, but the tumor cells have become immortalized. Which of the following best describes the difference in the number of cell doublings between tumor cells and normal fibroblasts?
A. Normal cells are programmed to self-destruct through apoptosis B. Tumor cells are more dependent on anaerobic glycolysis for energy production C. Tumor cells are often motile and can move to more favorable environments D. Tumor cells express telomerase following embryonic life E. Tumor cells lack the cancer suppressor gene RB and can live indefinitely |
Option D (tumor cells express telomerase following embryonic life) is correct. Studies have convincingly shown that many tumor cells express telomerase, which allows them to reproduce indefinitely. The presence of this enzyme, which acts as a reverse transcriptase, enables the cells to reconstitute their chromosomal telomeres. With only a few exceptions, normal cells generally do not express telomerase, and clip a segment of DNA from their telomere with each replication. The limit is about 50 replications.
|
Option A (normal cells are programmed to self-destruct through apoptosis) is incorrect. Apoptosis is the mechanism through which many senescent cells are removed from the body, but it is not involved in longevity in cell culture.
Option B (tumor cells are more dependent on anaerobic glycolysis for energy production) is incorrect. Although any tumor cells use anaerobic glycolysis for energy production, this has no direct effect on their longevity. Option C (tumor cells are often motile and can move to more favorable environments) is incorrect. Tumor cells often show some degree of motility, which helps explain their invasive ability. Because the cell culture is a homogeneous environment, motility is no advantage to survival. Option E (tumor cells lack the cancer suppressor gene RB and can live indefinitely) is incorrect. Cancer cells lack a number of tumor suppressor genes, among which RB might be included. This absence would partially explain their uncontrolled growth, not their longevity. |
|
|
A 51-year-old man has adenocarcinoma of the lesser curvature. Which of the following is the most important prognostic factor when evaluating a patient with this type of tumor?
A. Degree of differentiation B. Depth of invasion C. Gross growth pattern D. Histologic subtype of the carcinoma E. Presence of Helicobacter pylori |
Option B (depth of invasion) is correct. The morphologic feature with the greatest effect on clinical outcome in adenocarcinoma of the lesser curvature is depth of tissue invasion. Patients with carcinoma in the early stages (limited to the mucosa and submucosa) have a far better prognosis (90% survival with surgery) than patients with advanced carcinoma (<10% survival with surgery).
|
Option A (degree of differentiation) is incorrect. The degree of differentiation seems to have little influence on survival.
Option C (gross growth pattern) is incorrect. Exophytic, flat, or depressed growth patterns are apparent in both the early stages and advanced stages of carcinoma. The type of pattern seems to have little influence on prognosis. Option D (histologic subtype of the carcinoma) is incorrect. The histologic subtype of tumor seems to have little influence on prognosis. Option E (presence of Helicobacter pylori) is incorrect. H. pylori seems to be a cofactor in the development of some forms of gastric carcinoma; however, its presence does not influence prognosis. |
|
|
A 49-year-old man with a history of chronic alcoholism suddenly develops severe pain in the midabdominal area, which radiates to the back. Within 24 hours, he goes into shock and develops hypocalcemia. His serum amylase is markedly increased. Despite appropriate care, he dies. Which of the following morphologic changes may account for the hypocalcemia?
A. Hemorrhagic fat necrosis of the pancreas with yellow soap deposits on adjacent adipose tissue B. Impacted gallstones in the ampulla of Vater with acute ascending cholangitis C. Perforation of a gastric ulcer with hemorrhage into the peritoneal cavity and marked chemical peritonitis D. Rupture of the aorta with exsanguination into the retroperitoneal space E. Swollen kidneys with a marked degree of necrosis of the proximal renal tubular epithelium |
Option A (hemorrhagic fat necrosis of the pancreas with yellow soap deposits on adjacent adipose tissue) is correct. With the massive release of enzymes during the necrosis of the pancreas, the triglycerides stored in adipose tissue are digested into free fatty acids, which can react with cations to form soap. Calcium and magnesium soaps are insoluble; as they are formed, they complex calcium removing it from circulation. If sufficient calcium soap is formed, the serum calcium level can be significantly diminished.
|
Option B (impacted gallstones in the ampulla of Vater with acute ascending cholangitis) is incorrect. Impacted gallstones with acute cholangitis would be a source of pain and shock due to gram-negative infection but would not account for the hypocalcemia.
Option C (perforation of a gastric ulcer with hemorrhage into the peritoneal cavity and marked chemical peritonitis) is incorrect. A perforated gastric ulcer is certainly a catastrophic event that can cause severe pain and sometimes shock, but it would not be expected to cause hypocalcemia. Option D (rupture of the aorta with exsanguination into the retroperitoneal space) is incorrect. This condition would indeed be a source of shock, but it would not be expected to cause hypocalcemia. Option E (swollen kidneys with a marked degree of necrosis of the proximal renal tubular epithelium) is incorrect. If the patient had been in shock for a sufficient length of time, he might have exhibited the changes associated with acute tubular necrosis. Although this would cause the electrolyte disturbance, it would not be a cause of acute hypocalcemia. |
|
|
Individuals taking phenobarbital may be more susceptible to free radical injury by toxins such as carbon tetrachloride (CCl4). Phenobarbital induces which of the following subcellular changes?
A. Additional receptor sites for CCl4 on the cell membrane of the hepatocytes B. Atrophy of the Golgi zone within the hepatocytes C. Atrophy of the smooth endoplasmic reticulum (SER) within the hepatocytes D. Increased formation of G proteins within the hepatocytes E. Marked hypertrophy of the SER within the hepatocytes |
Option E (marked hypertrophy of the SER within the hepatocytes) is correct. Phenobarbital induces hypertrophy of the SER and hence a marked increase in cytochrome p450 activity. The conversion of CCl4 into the toxic free radical CCl3 by the cytochrome p450 system causes the injury.
|
Option A (additional receptor sites for CCl4 on the cell membrane of the hepatocytes) and Option D (increased formation of G proteins within the hepatocytes) are incorrect. Refer to the discussion for option E.
Option B (atrophy of the Golgi zone within the hepatocytes) is incorrect. The production of free radicals resulting from CCl4 does not involve the Golgi zone. Option C (atrophy of the smooth endoplasmic reticulum within the hepatocytes). Phenobarbital causes swelling, not shrinking, of the SER. |
|
|
A 67-year-old retired airline pilot slipped on the ice, striking his head on the sidewalk. His history is unremarkable. A CT scan of the head shows no sign of hematoma, but does show atrophy of the cerebral hemispheres. The atrophy is most likely due to
A. decreased daily workload B. diminished blood supply C. inadequate nutrition D. loss of endocrine stimulation E. loss of innervation |
Option B (diminished blood supply) is correct. Atherosclerosis leads to reduced blood flow to the brain and is thought to be the major culprit in the etiology of cerebral atrophy in the elderly.
|
Option A (decreased daily workload) is incorrect. There is no correlation between lack of intellectual activity and loss of neurons.
Option C (inadequate nutrition) is incorrect. Studies have shown that starvation reduces the effects of aging rather than promoting them, so poor nutrition is probably not a significant factor. Option D (loss of endocrine stimulation) is incorrect. The human brain apparently is not under hormonal stimulus for support of its neuronal mass. Option E (loss of innervation) is incorrect. Although studies have described some decrease in the number of neurons and axonal connections over time, this finding is probably not a significant factor. |
|
|
A 50-year-old man who has smoked two packs of cigarettes a day for 30 years has squamous metaplasia of the respiratory epithelium. His physician tells him that smoking is a major cause of metaplasia, but there are other causes for this change. Which of the following may also cause squamous metaplasia of bronchial mucosa?
A. Deficiency of folate B. Deficiency of vitamin A C. Excess vitaminB2 D. Excess vitamin C E. Excess vitamin D |
Option B (deficiency of vitamin A) is correct. Vitamin A and retinoids are necessary in maintaining the differentiation of epithelial cells. Deficiency of vitamin A causes squamous metaplasia of the respiratory tract epithelium as well as impaired vision, night blindness, and xerophthalmia.
|
Option A (deficiency of folate), Option C (excess vitamin B2), Option D (excess vitamin C), and Option E (excess vitamin D) are incorrect. Folate deficiency can cause changes in many cell lines, generally promoting an increase in cell size and asynchronous maturation of the cytoplasm and nucleus. Excess doses of vitamin B2 and vitamin C seem to be relatively harmless. Excess vitamin D influences the metabolism of calcium.
|
|
|
When an acute inflammatory reaction develops in response to an injurious stimulus, endothelial cells and macrophages produce nitric oxide (NO). During acute inflammation, NO functions to
A. cause pain B. induce smooth muscle contraction C. opsonize bacteria D. produce fever E. promote vasodilation |
Option E (promote vasodilation) is correct. NO is produced by nitric oxide synthase and is somewhat cytotoxic. NO causes the relaxation of vascular smooth muscle, leading to vasodilation.
|
Option A (cause pain) and Option D (produce fever) are incorrect. Prostaglandins mediate pain and fever.
Option B (induce smooth muscle contraction) is incorrect. Leukotrienes are responsible for smooth muscle contraction, causing vasoconstriction. Option C (opsonize bacteria) is incorrect. Immunoglobulins opsonize bacteria. |
|
|
A 61-year-old woman with a lengthy history of hypertension dies of an acute myocardial infarction (MI). At autopsy, the heart shows gross hypertrophy of the left ventricle. The adaptive mechanism responsible for the increase in the mass of the ventricle is most likely
A. fusion of individual muscle fibers into larger, stronger units B. increased cycling of cells out of G 0 1 phase C. increased individual cell size, with no mitotic activity D. increased mitotic rate and the production of more cells E. primarily an increase in individual cell size, with normal mitotic activity |
Option C (increased individual cell size, with no mitotic activity) is correct. The increase in cardiac and skeletal mass is due to an increase in the size of individual muscle fibers. These cells are not capable of significant mitotic activity.
|
Option A (fusion of individual muscle fibers into larger, stronger units) is incorrect. Fusion of muscle cells may occur, but this takes place only in unusual myopathies.
Option B (increased cycling of cells out of G 0 phase and into G 1 phase) is incorrect. Cardiac muscle cells are permanent cells that are not capable of significant mitotic activity. Therefore, they do not complete the cell cycle. Option D (increased mitotic rate and the production of more cells) is incorrect. For practical purposes, skeletal muscle and cardiac muscle cells may be considered to be permanent cells and thus incapable of mitosis. Option E (primarily an increase in individual cell size, with normal mitotic activity) is incorrect. Although individual cells do increase in mass, mitosis is not a part of the process. |
|
|
Several weeks after sustaining a gunshot wound, the bullet is surgically removed from the shoulder of a 20-year-old man. Histologically, the lesion resembles a chronic inflammatory infiltrate, with numerous macrophages surrounding the bullet. In the chronic inflammatory response, macrophages are especially important because they are
A. capable of local proliferation B. easily recruited from the circulation C. involved in the production of numerous biologically active substances D. permanently localized to the site of inflammation |
Option C (involved in the production of numerous biologically active substances) is correct. Macrophages produce an abundance of biologically active substances (e.g., toxic free radicals, proteases, cytokines, growth factors, and angiogenesis factor), and all are involved in chronic inflammation.
|
Option A (capable of local proliferation) is incorrect. Macrophages can reproduce locally, but this simply increases their number.
Option B (easily recruited from the circulation) is incorrect. Macrophages are easily recruited from the circulation by various chemotactic factors recruit easily, but many other inflammatory cells can also be attracted similarly. Option D (permanently localized to the site of inflammation) is incorrect. Although some cytokines can immobilize macrophages and are retained in the area of inflammation, this only tends to increase their number. |
|
|
A 30-year-old black woman who resides in North Carolina develops increasing shortness of breath. A physical examination shows lymphadenopathy in the axillae and groin. X-ray film of the chest shows a marked degree of hilar lymph node enlargement. A biopsy of an enlarged axillary lymph node shows numerous noncaseating granulomas. No organisms are identifiable, and acid-fast stains are negative. These findings are most likely caused by which of the following?
A. Coccidioidomycosis B. Cryptococcosis C. Histoplasmosis D. Sarcoidosis E. Tuberculosis |
Option D (sarcoidosis) is correct. Sarcoidosis typically produces noncaseating ("hard") granulomas, rather than lesions characterized by central caseous necrosis. In addition, multisystem involvement, including skin, lungs, lymph nodes, liver, spleen, eyes, and the small bones of the hand and feet, is typical. Sarcoidosis occurs mainly in individuals between the ages of 20 and 40 years; risk is higher in the black population.
|
Option A (coccidioidomycosis) is incorrect. Coccidioides immitis generally produces large, easily identifiable spherules. Some caseous necrosis would occur with coccidioidomycosis. The disease is endemic in the southwestern United States, not North Carolina where this patient resides.
Option B (cryptococcosis) is incorrect. Cryptococcus neoformans is a large organism that is usually not difficult to demonstrate. Inflammation associated with C. neoformans is often mild. Option C (histoplasmosis) is and Option E (tuberculosis) are incorrect. In some affected patients (unlike this woman), central nervous system symptoms may develop. Histoplasma capsulatum mimics tuberculosis histologically, and the presence of caseating granulomas is expected. H. capsulatum is endemic to the Ohio-Mississippi river valleys and in areas of northern Maryland, southern Pennsylvania, central New York, and Texas. |
|
|
A 63-year-old man has a history of congestive heart failure due to severe arteriosclerosis of the coronary arteries. He now has pitting edema of the ankles that extends about halfway up the lower part of his legs. The edema in this patient is most likely caused by which of the following mechanisms?
A. Decreased oncotic pressure in the vascular compartment B. Impaired lymphatic drainage of the legs C. Increased hydrostatic pressure in the vascular compartment D. Increased oncotic pressure in the extracellular compartment E. Increased vascular permeability |
Option C (increased hydrostatic pressure in the vascular compartment) is correct. In this patient, the increased pressure is the main cause of dependent edema. The failing right side of the heart (right atrium and ventricle) has led to an increase in intravascular hydrostatic pressure, which eventually causes a net movement of fluid from the vascular space to the extravascular space.
|
Option A (decreased oncotic pressure in the vascular compartment) is incorrect. In some renal diseases, such as minimal change disease, reduced oncotic pressure due to the loss or lack of synthesis of albumin is the mechanism for the development of generalized massive edema (anasarca).
Option B (impaired lymphatic drainage of the legs) is incorrect. This condition can certainly cause edema, but pathology causing the lymphatic obstruction should be evident. Option D (increased oncotic pressure in the extracellular compartment) is incorrect. An increase in oncotic pressure in the vascular compartment would tend to draw in fluid from the extravascular space, rather than move it into the extravascular space. Option E (increased vascular permeability) is incorrect. In inflammatory conditions, increased vascular permeability is the mechanism for the development of edema. |
|
|
An 18-year-old man scheduled to undergo surgery to repair a hernia has a history of easy bruising and a tendency to bleed for an abnormally long time after an injury. Laboratory studies show prolonged bleeding time, normal prothrombin time, and slightly prolonged partial thromboplastin time. Which of the following is the most specific laboratory test that would confirm the suspected diagnosis of von Willebrand's disease?
A. Clot retraction test B. Factor VIII assay C. Ristocetin aggregation test D. Thrombin time |
Option C (ristocetin aggregation test) is correct. Ristocetin binds to platelets, activating von Willebrand's factor (vWF) receptors on the surface. If vWF is present, it forms a bridge between receptors on different platelets, causing platelet aggregation.
|
Option A (clot retraction test) is incorrect. An abnormal result suggests either insufficient fibrinogen or lack of factor XII activity and does not aid in the diagnosis of von Willebrand's disease.
Option B (factor VIII assay) is incorrect. VWF stabilizes factor VIII; thus, in a patient with von Willebrand's disease, factor VIII activity would most likely be somewhat diminished. However, the lack of factor VIII would not cause a prolonged bleeding time. Other diseases, such as hemophilia A, would also cause diminished factor VIII activity. Option D (thrombin time) is incorrect. In a patient with von Willebrand's disease, thrombin time is normal. |
|
|
A 40-year-old man who was involved in an automobile accident is being treated for a fracture of the pelvis. The man is at increased risk of developing pulmonary emboli because of relative stasis of venous flow in his legs. Which of the following most accurately describes these emboli?
A. Most are clinically silent B. They are rare C. They commonly cause chronic pulmonary hypertension D. They typically cause pulmonary infarction E. They usually cause immediate death |
Option A (most are clinically silent) is correct. The majority of pulmonary emboli (60\'9680%) are small; thus, they are clinically silent. Autopsy series are the source of most of the data, and the frequency of finding emboli tends to be related to the diligence of the pathologist.
|
Option B (they are rare) is incorrect. Pulmonary emboli cause more than 50,000 deaths in the United States each year, making them a relatively common occurrence. In a general hospital population, the reported incidence of pulmonary embolism is about 1% at autopsy. One series that uses specialized techniques reports an incidence of 65% of patients.
Option C (they commonly cause chronic pulmonary hypertension) is incorrect. Pulmonary emboli that occur over a lengthy period of time can produce pulmonary hypertension, but multiple episodes are necessary, and the condition is uncommon. Option D (they typically cause pulmonary infarction) is incorrect. Pulmonary emboli often do not cause infarction in patients with normal lungs and normal circulatory systems. Unless some degree of compromise of the pulmonary circulation exists before the event, collateral circulation is effective in preventing infarction. Option E (they usually cause immediate death) is incorrect. To be fatal, pulmonary emboli must involve a large embolus that occludes more than 60% of the total pulmonary vasculature. |
|
|
A 54-year-old woman with severe right upper quadrant pain, fever, and jaundice is in shock when brought to the emergency department. A blood culture grows Escherichia coli. The presumptive diagnosis is acute cholecystitis. The most likely cause of shock is
A. anaphylactic reaction B. cardiogenic shock C. endotoxemia D. hemorrhage E. neurogenic shock |
Option C (endotoxemia) is correct. Endotoxin (lipopolysaccharide), a component of the cell walls of gram-negative bacteria, binds to CD14 receptors. It causes a cascade of events that result in shock, metabolic failure, disseminated intravascular coagulopathy, and eventually multiple organ failure.
|
Option A (anaphylactic reaction) is incorrect. No immunologically mediated event has occurred in this case. Production of an anaphylactic (type I hypersensitivity) reaction requires a history of a prior sensitizing event and then challenge with the sensitizing antigen.
Option B (cardiogenic shock) is incorrect. Although there is an element of myocardial dysfunction in endotoxemia, cardiogenic shock is not the proximate cause. Option D (hemorrhage) is incorrect. Nothing in either the history or presenting physical findings of this patient suggests hemorrhage. Option E (neurogenic shock) is incorrect. Neurogenic shock is an uncommon type of shock and is generally the result of central nervous system injury. No such event has occurred in this case. |
|
|
A 46-year-old woman delivers a newborn with the physical features associated with Down's syndrome (trisomy 21). A FISH (fluorescent in situ hybridization) assay shows the presence of three number 21 chromosomes. The most common mechanism causing trisomy 21 is
A. failure of lyonization B. formation of a ring chromosome C. meiotic nondisjunction of chromosome 21 in the ovum D. mitotic nondisjunction of chromosome 21 early in embryogenesis E. robertsonian translocation of the long arm of chromosome 21 to an acrocentric chromosome |
Option C (meiotic nondisjunction of chromosome 21 in the ovum) is correct. Down's syndrome typically affects children born of women over 35 years of age, and is of maternal origin but of undetermined etiology. The most common mechanism of trisomy 21 (>90% of cases) involves the meiotic nondisjunction of chromosome 21.
|
Option A (failure of lyonization) is incorrect. Lyonization is the random inactivation of one of the two X chromosomes at the blastocyst stage in female embryos.
Option B (formation of a ring chromosome) is incorrect. Ring chromosomes, which result from deletions, do not involve the excess genetic material associated with trisomies. Option D (mitotic disjunction of chromosome 21 early in embryogenesis) is incorrect. This genetic abnormality accounts for about 1% of cases of Down's syndrome. Typically, affected individuals are mosaics who have milder symptoms. Option E (robertsonian translocation of the long arm of chromosome 21 to an acrocentric chromosome) is incorrect. Robertsonian translocation may be a cause of Down's syndrome, but its occurrence tends to be unusual, familial, and may originate from either parent. |
|
|
A 27-year-old man is a diagnosed with a diffuse large cell lymphoma. Genetic analysis of DNA from the lymphoma cells shows rearrangement of the immunoglobulin genes. Which of the following is the most likely origin of this lymphoma?
A. B-cell lymphoma B. Histiocytic lymphoma C. Natural killer (NK) cell lymphoma D. T-cell lymphoma |
Option A (B-cell lymphoma) is correct. Somatic rearrangement of the immunoglobulin genes marks this lesion as a lymphoma of B cell origin. Lymphoma is a monoclonal lesion, so all of the tumor cells exhibit identical patterns of immunoglobulin gene rearrangement.
|
Option B (histiocytic lymphoma) is incorrect. True histiocytic lymphomas are uncommon, and do not show rearrangement of the immunoglobulin genes.
Option C (natural killer cell lymphoma) is incorrect. NK cell lymphoma is a type of lymphoma classified as non\'96B- and non\'96T-cell lymphomas that were originally known as null cell lymphomas. They do not exhibit the gene rearrangement characteristic of T cell or B cell origin. Option D (T-cell lymphoma) is incorrect. Gene rearrangements are characteristic of T-cell lymphomas, but these changes do not involve the immunoglobulin genes. |
|
|
A 37-year-old woman with a 5-year history of Raynaud's phenomenon, increasing dysphagia, and vague abdominal pain undergoes further testing for autoimmune disease. An immunofluorescent antinuclear antibody (ANA) test shows a nucleolar pattern with a high titer. No malar h or joint pathology is evident. The skin on the woman's hands is somewhat shiny, and normal skin markings are indistinct. A biopsy of the skin on the patient's hands would most likely show
A. fibrinoid necrosis of the vasculature B. fibrosis of the dermis, thinning of the epidermis, and thickening of the arterioles C. liquefactive necrosis of the basal layer of the epidermis D. necrotizing inflammation of the small arterioles |
Option B (fibrosis of the dermis, thinning of the epidermis, and thickening of the arterioles) is correct. These pathologic findings are consistent with the diagnosis of progressive systemic sclerosis. The clinical presentation of Raynaud's phenomenon and dysphagia, along with the laboratory finding of a strongly positive ANA with a nucleolar pattern, are also suggestive of progressive systemic sclerosis.
|
Option A (fibrinoid necrosis of the vasculature) is incorrect. This change is more suggestive of systemic lupus erythematosus (SLE), in which an acute necrotizing vasculitis affects small arteries and arterioles, particularly of the skin and muscles.
Option C (liquefactive necrosis of the basal layer of the epidermis) is incorrect. This change is suggestive of SLE. Classically, skin lesions show liquefactive degeneration of the basal epidermal layer. Option D (necrotizing inflammation of the small arterioles) is incorrect. Such involvement suggests polyarteritis nodosa, which affects small- to medium-sized arteries in any organ (e.g., kidneys, heart, liver). |
|
|
An ultrasound examination of a 17-year-old boy with a firm, enlarged right testicle shows a 1-cm cyst. Examination of the testicle after orchiectomy shows a cystic lesion filled with a somewhat cheese-like appearing component that is separated from otherwise normal-appearing tubules by a fairly distinct wall. Microscopic examination shows the wall of the lesion has the appearance of mature skin. This lesion would be classified as a
A. benign germ cell tumor B. benign stromal cell tumor C. germ cell tumor with undetermined malignant potential D. inclusion cyst derived from the overlying scrotal skin |
Option C (germ cell tumor with undetermined malignant potential) is correct. The presence of skin-like tissue in the tumor would determine that the lesion is a mature teratoma, a mass that contains fully differentiated tissue from one or more germ cell layers (e.g., epithelium). Unlike dermoid cysts in the ovary, mature teratomas in the testis are not always benign and have a potential to become malignant; thus, they cannot be considered totally benign. Small foci of undetected malignant components are possible
|
Option A (benign germ cell tumor), Option B (benign stromal cell tumor), and Option D (inclusion cyst derived from the overlying scrotal skin) are incorrect. Teratomas are germ cell tumors that form elements of one or more germ cell layers. Inclusion cysts of the skin are attached to the skin, but do not invade the testis.
|
|
|
A 32-year-old woman has a family history of a high incidence of neoplasia involving multiple organ systems. She undergoes genetic screening for several tumor suppressor genes and oncogenes and is found to have Li-Fraumeni syndrome. The genetic defect associated with this syndrome is loss of one allele of which of the following genes?
A. bcl-2 B. NF-1 C. P53 D. RB E. WT1 |
Option C (P53) is correct. Loss of one of the alleles of the P53 gene is the basis of the Li-Fraumeni syndrome. Patients with this syndrome have an increase in the development of malignant neoplasms arising in various anatomic locations. P53, a tumor suppressor gene that also has oncogene-like properties when mutated, produces an abnormal gene product that is not degraded with normal speed. Patients with a mutated or missing P53 gene have an increased risk of developing malignancies in various tissues.
|
Option A ( bcl-2), Option B (NF-1), Option D (RB), and Option E (WT1) are incorrect. The oncogene bcl-2 is associated with prevention of apoptosis. NF-1, RB, and WT1 are tumor suppressor genes associated with neurofibromatosis, retinoblastoma, and Wilms' tumor of the kidney, respectively.
|
|
|
The mechanism thought to be responsible for the increasingly aggressive behavior of malignant tumors is that they
A. are genetically labile B. cause the production of tumor necrosis factor-a (TNF-a) C. induce angiogenesis D. produce paraneoplastic syndromes |
Option A (are genetically labile) is correct. Malignant tumors are constantly mutating and forming new clones. Many of the clones die, but some will have a selective advantage with regard to growth, invasion, or metastasis.
|
Option B (cause the production of tumor necrosis factor-a is incorrect. Although malignant tumors do cause macrophages to produce TNF-a, it is believed that this causes cachexia.
Option C (induce angiogenesis) is incorrect. Malignant tumors do induce angiogenesis. This allows them to grow larger than about 1 mm (the size limit if they did not develop a blood supply). However, it does not change their potential to become malignant. Option D (produce paraneoplastic syndromes) is incorrect. Malignant tumors may secrete hormones or hormone-like substances that will produce a paraneoplastic syndrome. This capability does not affect the malignant potential of the tumor itself. |
|
|
Studies show that workers in the aniline dye industry are at increased risk for bladder cancer. Similar studies in animals show that many different species exposed to b-naphthylamine develop liver cancer, but not bladder cancer. Which of the following best explains this pattern of human susceptibility to b -naphthylamine?
A. Conjugation of b-naphthylamine with glucuronic acid detoxifies the electrophilic toxic metabolite B. Metabolism of b-naphthylamine into a toxic electrophilic reactant is unique to humans C. Metabolism of b-naphthylamine occurs via the cytochrome p450 system in humans D. b-naphthylamine is directly carcinogenic in humans and does not require metabolic activation E. Urinary glucuronidase reactivates the nontoxic conjugate of b-naphthylamine and glucuronic acid |
Option E (urinary glucuronidase reactivates the nontoxic conjugate of b-naphthylamine) is correct. Humans almost uniquely have b-glucuronidase in their urine, which splits the harmless conjugate into glucuronic acid and the toxic electrophilic metabolite of
b-napthylamine. |
Option A (conjugation of b-naphthylamine with glucuronic acid detoxifies the electrophilic toxic metabolite) is incorrect. This statement describes the detoxification of b-naphthylamine. The harmless conjugate is then excreted into the urine.
Option B (metabolism of b-naphthylamine into a toxic electrophilic reactant is unique to humans) is incorrect. Such metabolism of b-naphthylamine occurs in all animals, not just in humans. Option C (metabolism of b-naphthylamine occurs via the cytochrome p450 system in humans) is incorrect. Such metabolism of b -napthylamine occurs in humans, but many other animal species also metabolize the substance in this manner. Option D (b-naphthylamine is directly carcinogenic in humans and does not require metabolic activation) is incorrect. b-naphthylamine requires metabolic activation to an "ultimate" carcinogen to cause injury. |
|
|
An 18-year-old man with xeroderma pigmentosum would be particularly susceptible to the development of which of the following tumors?
A. Carcinoma of the esophagus B. Carcinoma of the colon C. Carcinoma of the thyroid D. Squamous cell carcinoma of the skin E. Transitional cell carcinoma of the bladder |
Option D (squamous cell carcinoma of the skin) is correct. Xeroderma pigmentosum is an autosomal recessive disease characterized by an inability to repair DNA damage caused by exposure to ultraviolet (UV) light. UV light causes cross-linking of pyrimidine residues, thus preventing normal DNA replication. Such abnormal DNA is repaired by the nucleotide exclusion repair system, and the genes that are normally responsible for this repair mechanism are missing or mutated. Individuals with this disorder subsequently develop tumors related to excessive exposure to the sun, such as squamous cell carcinoma or basal cell carcinoma, at a much earlier age than would be expected. Normally, these tumors are seen after the age of 40 years, depending on amount of sun exposure and genetic factors. Xeroderma pigmentosum occurs less frequently in blacks due to the absorption of UV light and because the melanin in their skin is very protective.
|
Option A (carcinoma of the esophagus), Option B (carcinoma of the colon), Option C (carcinoma of the thyroid), and Option E (transitional cell carcinoma of the bladder) are incorrect. UV damage makes no contribution to the pathogenesis of these tumors, so xeroderma pigmentosum plays no etiologic role.
|
|
|
A 32-year-old man has had vague abdominal discomfort, bloating, and diarrhea since returning from a camping trip 2 weeks ago where he routinely drank mountain stream water. Stool smears show triangular-shaped organisms containing two nuclei. Which of the following is the most likely cause of the diarrhea?
A. Balantidium coli B. Entamoeba histolytica C. Giardia lamblia D. Vibrio cholerae |
Option C (Giardia lamblia) is correct. G. lamblia is the most prevalent pathogenic intestinal protozoan. It attaches to the mucosa rather than invading it; thus, it tends to cause irregular (intermittent) watery diarrhea rather than dysentery. In some patients, it causes constipation; in others, it causes steatorrhea. Symptoms of giardiasis generally occur 1\'963 weeks after infection.
|
Option A (Balantidium coli) is incorrect. This tissue-invasive ciliated protozoan causes colitis and dysentery.
Option B (Entamoeba histolytica) is incorrect. This tissue-invasive parasite causes dysentery, rather than simple diarrhea. Option D (Vibrio cholerae) is incorrect. This organism releases an exotoxin that causes severe, profuse watery diarrhea. |
|
|
A 50-year-old woman who has been taking estrogen daily, without interruption, for a long period of time is at significant risk for the development of
A. endometrial adenocarcinoma B. endometrial atrophy C. enlarged corpora lutea D. ovarian teratoma |
Option A (endometrial carcinoma) is correct. The risk for development of endometrial adenocarcinoma is about 1.7\'962.0 times the normal rate in patients who take unopposed estrogen on a continuous basis, without interruption.
|
Option B (endometrial atrophy) is incorrect. Estrogen is a strong promoter of endometrial growth.
Option C (enlarged corpora lutea) is incorrect. By definition, women who take estrogen replacement therapy (ERT) do not ovulate, so formation of corpus lutea is not possible. Option D (ovarian teratoma) is incorrect. Exogenous estrogen in a postmenopausal woman plays no role in the development of germ cell tumors of the ovary. |
|
|
A 17-year-old girl with Hodgkin's disease was treated successfully with aggressive chemotherapy, and the disease has been in remission for 2 years. She is now at increased risk for the development of a second malignant tumor. Which of the following changes is most likely caused by antineoplastic agents?
A. Depression of immune surveillance B. Depression of the mononuclear phagocyte system C. Induction of nonlethal mutations D. Induction of telomerase E. Promotion of tumor angiogenesis |
Option C (induction of nonlethal mutations) is correct. Most antineoplastic agents act on dividing cells at some specific point in the cell cycle. In damaging the reproductive function of the cell, accumulating nonlethal mutations may occur, which may result in the formation of a second neoplasm.
|
Option A (depression of immune surveillance) is incorrect. The existence of immune surveillance in humans is based on circumstantial evidence, but it is thought to be probable. Once a neoplasm is formed, lack of immune surveillance might augment the chances of it surviving, but it would not be a direct causative factor.
Option B (depression of the mononuclear phagocyte system) is incorrect. Antineoplastic drugs reduce this protective mechanism, but the result would increase opportunistic infections rather than induce a new neoplasm. Option D (induction of telomerase) is incorrect. About 95% of tumors express this gene product, but this alone would not be associated with the production of a new malignancy. Option E (promotion of tumor angiogenesis) is incorrect. If tumors are to grow beyond a minuscule size, angiogenesis is necessary. However, angiogenesis would have no effect on tumor induction. |
|
|
An 18-year-old college student who was seen drinking heavily at a party is found in his room completely unresponsive. When he is admitted to the emergency department, his blood alcohol level is 325 mg/dL. In a nonhabituated drinker, this level of blood alcohol is associated with
A. coma and respiratory collapse B. congestive cardiomyopathy C. development of acute yellow atrophy of the liver D. Korsakoff's syndrome E. Wernicke's encephalopathy |
Option A (coma and respiratory collapse) is correct. Alcohol acts as a central nervous system (CNS) depressant via mechanisms that are still unclear, but possibly by action on GABA receptors. At alcohol levels of 300\'96400 mg/dL, coma and respiratory collapse are likely. Individuals who chronically abuse the substance will tolerate higher levels.
|
Option B (congestive cardiomyopathy) is incorrect. Long-term, rather than acute, alcohol abuse is strongly associated with congestive cardiomyopathy.
Option C (development of acute yellow atrophy of the liver) is incorrect. Although ethanol is a direct hepatic toxin, it would not typically produce such severe damage. Option D (Korsakoff's syndrome) is incorrect. Korsakoff's syndrome, an amnestic syndrome, is a long-term effect of chronic alcoholism due to thiamine deficiency and direct toxicity. Option E (Wernicke's encephalopathy) is incorrect. Wernicke's encephalopathy, which involves confusion, ataxia, and ophthalmoplegia, is a long-term effect of chronic alcoholism due to thiamine deficiency. |
|
|
A 3-year-old boy is brought to the pediatrician suffering from fatigue and delayed mental development. Laboratory studies show anemia with fairly pronounced basophilic stippling of the red cells. A radiograph of the femur shows increased density of the epiphyses. The child's parents mention they had lived in an old house when the child was teething. Which of the following combinations of laboratory studies and results would most likely be found in this patient?
A. Blood analysis, increased serum lead B. Blood analysis, saturated iron-binding capacity, increased serum iron C. Bone marrow aspiration, megakaryocytopenia D. Chromosome analysis, trisomy 21 |
Option A (blood analysis, increased serum lead) is correct. Lead poisoning in children is often a subtle problem generally resulting from ingestion of flakes of paint containing lead. Paint now rarely contains lead, but older homes may have numerous coats of lead-containing paint beneath the top layer of paint. Lead is stored in blood, soft tissue, and bones. It produces anemia due to its interference with heme synthesis such that a zinc (rather than an iron-containing protoporphyrin) is formed. The pathogenesis of the effects of lead on the central nervous system is not entirely understood.
|
Option B (blood analysis, saturated iron-binding capacity, increased serum iron) is incorrect. This finding suggests the possibility of iron overload, not lead poisoning.
Option C (bone marrow aspiration, megakaryocytopenia) is incorrect. Platelet abnormalities would not be expected in lead poisoning. Because blood studies are sufficient for such a diagnosis, bone marrow studies are not indicated. Option D (chromosome analysis, trisomy 21) is incorrect. Unless Down's syndrome is suggested on the basis of physical findings, this analysis is not indicated. |
|
|
A 27-year-old intravenous drug abuser is found dead from an overdose of heroin. Autopsy shows profound pulmonary edema and numerous 3- to 5-mm yellowish-white nodules throughout the lungs. Histologic examination shows granulomas with no suggestion of caseous necrosis. Stains for infectious organisms are negative. An examination under polarized light shows small flecks of birefringent material within macrophages. The cause of these granulomas is most likely
A. activation of angiotensin-converting enzyme (ACE) B. activation of a previously acquired mycobacterial infection C. concomitant HIV infection D. direct toxicity to alveolar macrophages by heroin E. foreign substance in the injected heroin |
Option E (foreign substance in the injected heroin) is correct. To increase profits, drug dealers often dilute ("cut") heroin with foreign substances, which is most likely what the patient used. Usually lactose is used, but any white substance is acceptable; the cleanliness of the "lab" is also doubtful. Talc, a common contaminant, is taken up by macrophages, which then form granulomas as a foreign body reaction. Similar granulomas may often be found in the liver, spleen, and lymph nodes. Profound pulmonary edema is often apparent in individuals who die from heroin overdose.
|
Option A (activation of angiotensin-converting enzyme) is incorrect. An increased level of ACE is a result of granuloma formation, not a cause of it.
Option B (activation of a previously acquired mycobacterial infection) is incorrect. Infection directly associated with intravenous heroin use is frequent, but it is typically pyogenic, rather than mycobacterial. Option C (concomitant HIV infection) is incorrect. HIV infection frequently accompanies intravenous heroin usage due to needle sharing. Activation of previous tuberculosis at a site now "healed" is possible, as is infection de novo by Mycobacterium avium-intercellulare. If this were the case in this patient, the organisms would be readily seen using the appropriate special stains. Option D (direct toxicity to alveolar macrophages by heroin) is incorrect. The lung may exhibit hypersensitivity to heroin by developing severe, often fatal, pulmonary edema, but this would not be a direct cause of granuloma formation. |
|
|
A 47-year-old man is brought to the emergency department after being exposed to an unknown dose of radiation due to malfunction of the industrial radiographic unit he operates. His coworkers think he may have received whole-body radiation exposure. Which of the following would be most sensitive to radiation exposure?
A. Bladder epithelium B. Cartilage C. Hair follicles D. Kidney E. Lymphoid tissue |
Option E (lymphoid tissue) is correct. Lymphoid tissue, hematopoietic tissue, spermatogonia, and ovarian follicles are all highly sensitive to radiation.
|
Option A (bladder epithelium), Option B (cartilage),Option C (hair follicles), and Option D (kidney) are incorrect. Bladder epithelium, hair follicles, and renal tissue is less sensitive to radiation than lymphoid or hematopoietic tissue. Mature cartilage is relatively insensitive to radiation.
|
|
|
A neonate born at 34 weeks' gestation is of appropriate weight and appears to be healthy. About 1 hour after birth, the infant displays retraction of the ribs and grunting sounds are heard during each respiratory cycle. Over the next several hours, the infant experiences breathing difficulties and subsequently develops cyanosis. Rales over both lung fields are heard on auscultation. Blood gases show increased PaCO2 and decreased PaO2. The neonate's respiratory difficulty is primarily caused by
A. aspiration of meconium B. lack of pulmonary surfactant C. in utero infection with cytomegalovirus D. in utero infection with parvovirus E. in utero infection with Toxoplasma gondii |
Option B (lack of pulmonary surfactant) is correct. This is a classic presentation of idiopathic respiratory distress syndrome (RDS) due to lack of formation of pulmonary surfactant by type II pneumocytes. Histologic examination of the lungs at this time would show hyaline membranes lining the alveolar ducts. The increased work of respiration causes exhaustion of the infant, resulting in decreased ventilation and increased PaCO2. Multiple foci of atelectasis produce ventilation/perfusion (V/Q) ratios near 0, which causes venous dilution of oxygenated blood, producing a decline in PaO2
|
Option A (aspiration of meconium) is incorrect. Meconium aspiration is associated with fetal distress. It may cause immediate difficulties with respiration after birth, but it is not expected to cause the usual progression of idiopathic respiratory distress syndrome (RDS).
Option C (in utero infection with cytomegalovirus) and Option E (in utero infection with Toxoplasma gondii) are incorrect. Although pneumonitis is frequently seen with TORCH infections (toxoplasmosis, rubella, cytomegalovirus, herpes simplex), it would not be expected to produce respiratory distress syndrome (RDS). Option D (in utero infection with parvovirus) is incorrect. Parvovirus infection causes hydrops fetalis and spontaneous abortion. |
|
|
A 24-year-old man has a history of fever, weight loss, hypertension, and abdominal pain. Stool and urinalysis are positive for the presence of blood. Several nodular skin lesions are found. A biopsy shows necrotizing arteritis involving medium-sized muscular arteries. This constellation of findings is most suggestive of
A. Kawasaki disease B. polyarteritis nodosa C. syphilis D. systemic lupus erythematosus (SLE) E. Takayasu's arteritis |
Option B (polyarteritis nodosa) is correct. Necrotizing inflammation of affected arteries is characteristic of polyarteritis nodosa, a disease that typically involves medium-sized muscular arteries. This disease may involve fever and weight loss, and hypertension is common. Gastrointestinal lesions are the source of the abdominal pain. The disease may affect individuals of any age.
|
Option A (Kawasaki disease) is incorrect. This condition involves arteries of all sizes. However, it usually occurs in infants and children.
Option C (syphilis) is incorrect. Syphilis causes an arteritis, but characteristically it is endarteritis with an infiltrate that is rich in plasma cells. Option D (systemic lupus erythematosus) is incorrect. SLE commonly causes a vasculitis that more typically involves the small arteries and arterioles. Option E (Takayasu's arteritis) is incorrect. This granulomatous arteritis usually involves the origin of the great vessels at the aortic arch. |
|
|
A 52-year-old man complains of general malaise. Physical examination shows an enlarged liver, and an MRI shows a mass in the left lobe of the liver. A liver biopsy confirms the mass as an angiosarcoma. The patient most likely has been exposed to which of the following toxins?
A. Carbon tetrachloride (CCl4) B. b-naphthylamine C. Nickel carbonyl D. Organophosphates E. Polyvinyl chloride |
Option E (polyvinyl chloride) is correct. Polyvinyl chloride, a known carcinogen, is associated with the development of hepatic angiosarcoma.
|
Option A (carbon tetrachloride) is incorrect. Although CCl4vis a potent hepatotoxin, it is not associated with the development of angiosarcoma.
Option B (b-naphthylamine) is incorrect. b-naphthylamine is associated with the development of transitional cell carcinoma of the urinary tract. Option C (nickel carbonyl) is incorrect. Nickel carbonyl is associated with the development of squamous cell carcinoma of the sinuses and lung. Option D (organophosphates) is incorrect. Organophosphates are potent cholinesterase inhibitors but are not associated with the development of angiosarcoma. |
|
|
A 48-year-old man comes to the emergency department because of severe chest pain. He is 5 ft 8 in tall and weighs about 90 kg (200 lb). He describes the pain as sudden in onset, producing a sensation of "tearing." Nitroglycerin spray provides no relief. An ECG shows no changes suggestive of an acute myocardial infarction (MI). Angiography shows a dissecting aneurysm of the aorta. The most likely antecedent condition associated with development of a dissecting aneurysm is
A. hypertension B. Marfan's syndrome C. severe atherosclerosis D. syphilis E. systemic lupus erythematosus (SLE) |
Option A (hypertension) is correct. Over 90% of patients who develop a dissecting aneurysm, and who have neither Marfan's syndrome nor a localized connective tissue disorder, are hypertensive.
|
Option B (Marfan's syndrome) is incorrect. Marfan's syndrome, an autosomal dominant disorder of connective tissue, may result in serious cardiovascular abnormalities. Death from aortic dissecting aneurism may occur. However, the physical description of the patient would eliminate Marfan's syndrome as a strong possibility.
Option C (severe atherosclerosis) is incorrect. Atherosclerosis is associated with the development of saccular aneurysms of the descending aorta, generally between the renal arteries and the bifurcation of the aorta into the common iliac arteries. Option D (syphilis) is incorrect. The tertiary stage of syphilis causes saccular aneurysms, most often in the ascending aorta. Option E (systemic lupus erythematosus) is incorrect. Involvement of the cardiovascular system in SLE is manifested primarily in the form of pericarditis, not aortic aneurysm. |
|
|
A 29-year-old woman has a soft midsystolic click on auscultation of the heart. Ultrasound examination shows a mitral valve prolapse. The most likely eventual outcome of this condition is
A. embolism by platelet aggregates B. mitral valve incompetence C. mitral valve stenosis D. normal life |
Option D (normal life) is correct. A mitral value prolapse generally is benign. About 97% of female patients with the condition experience no significant untoward effects.
|
Option B (mitral valve incompetence) is incorrect. Over time, mitral valve incompetence may develop, but this very rarely occurs.
Option C (mitral valve stenosis) is incorrect. Mitral value stenosis generally is the result of scarring due to rheumatic heart disease. Option A (embolism by platelet aggregates) is incorrect. In a very small minority of cases, embolization may occur from leaflet thrombi. |
|
|
As a result of the decreased incidence of patients with chronic rheumatic fever, consequent damage to the cardiac valves has diminished. The most common antecedent condition leading to infectious myocarditis presently is
A. congenital heart disease B. endocardial trauma C. hypercoagulable state D. leukemia E. mucin-producing adenocarcinoma |
Option A(congenital heart disease) is correct. Rheumatic heart disease was once considered the most common condition that could lead to infectious endocarditis. Presently, congenital lesions, particularly those that produce a "jet" effect such as a small ventricular septal defect, are more common and are a risk factor for infective endocarditis.
|
Option B (endocardial trauma), Option C (hypercoagulable state), Option D (leukemia), and Option E (mucin-producing adenocarcinoma) are incorrect. All of these conditions are associated with noninfective endocarditis, which may produce verrucous lesions on the margins of the heart valves. These lesions embolize but are not caused by an infectious organism.
|
|
|
A 63-year-old woman with a history of type 2 diabetes mellitus and an increasing exercise limitation is admitted to the hospital with severe influenza pneumonitis. She subsequently develops adult respiratory distress syndrome (ARDS) and dies 4 days after admission. Autopsy shows the heart encased in a 1-cm dense collagenous scar. Which of the following is the most likely cause of constrictive pericarditis?
A. Cryptococcosis B. Histoplasmosis C. Idiopathic D. Oat cell carcinoma E. Tuberculosis |
Option C (idiopathic) is correct. A well-defined history of a previous suppurative, hemorrhagic, or caseous pericarditis is often absent in the patient who dies of constrictive pericarditis.
|
Option A (cryptococcosis) is incorrect. Cryptococcus,a yeast-like pathogen, usually causes a mild pulmonary infection. Cryptococcosis is not a major cause of pericarditis, but it may lead to meningitis.
Option B (histoplasmosis) is incorrect. Although histoplasmosis can cause constrictive pericarditis, it is not the most common cause of this disorder. Option D (oat cell carcinoma) is incorrect. Oat cell carcinoma can involve the pericardium, but its effects are acute, with formation of a bloody effusion rather than scar tissue. Option E (tuberculosis) is incorrect. Although tuberculosis once was an important cause of constrictive pericarditis, this pulmonary disorder is no longer the most common cause. |
|
|
A 49-year-old man is brought to the emergency department about 6 hours after the onset of crushing chest pain. An ECG is suggestive of acute myocardial infarction (MI), and a troponin-I test is positive. He suddenly develops ventricular arrhythmia and despite appropriate treatment dies 1 hour after admission. At autopsy, the heart shows an area of scarring in the posterior wall of the left ventricle, but no new focus of infarction. For the usual signs of coagulation necrosis to become evident, the patient would have had to survive the recent MI for
A. 20-40 minutes B. 2 hours C. 8-12 hours D. 24-48 hours E. 72 hours |
Option C (8 hours) is correct. The typical signs of coagulative necrosis, including nuclear pyknosis, karyolysis, karyorrhexis, and increased cytoplasmic eosinophilia, appear 8-12 hours after infarction occurs.
|
Option A (20 minutes) is incorrect. The changes that occur in such a short period of time are only ultrastructural (e.g., mitochondrial swelling).Option B (2 hours) is incorrect. In 2 hours, a few "wavy" fibers are visible at the margin of the infarct.
Option D (24 hours) is incorrect. At 24 hours, both the microscopic and gross changes of necrosis would be discernible. At 48 hours, an influx of neutrophils would also be present. Option E (72 hours) is incorrect. At 72 hours, the influx of neutrophils would be at its height, and signs of dissolution of the necrotic heart muscle would be evident. |
|
|
A 72-year-old woman complains of feeling weak. Laboratory studies show a hematocrit of 18%, macrocytosis, hypersegmentation of neutrophils, and occasional giant platelets. Her lactate dehydrogenase (LDH) level is 2950 U/L, and her serum vitamin B12 is 27 pg/mL. Which of the following conditions most likely caused the increase in LDH?
A. Cardiomyopathy B. Hypersplenism C. Ineffective erythropoiesis D. Intravascular hemolysis E. Liver failure |
Option C (ineffective erythropoiesis) is correct. Patients with vitamin B12 deficiency have hyperplasia of the red blood cell (RBC) elements in the bone marrow, but the developing RBCs are destroyed in the marrow before they can be released into the circulation. When RBCs are destroyed, they release their large quantity of LDH into the plasma.
|
Option A (cardiomyopathy) is incorrect. Cardiomyopathy may cause a minor elevation of LDH, but not to the levels seen in the macrocytic anemias.
Option B (hypersplenism) is incorrect. Hypersplenism is not a typical finding in macrocytic anemias. Option D (intravascular hemolysis) is incorrect. In patients with macrocytic anemias, the increased RBC turnover occurs in the bone marrow, not in the circulation. Option E (liver failure) is incorrect. Acute liver necrosis can cause an elevation in LDH, but generally not at the increased levels seen in patients with macrocytic anemias. |
|
|
A 22-year-old medical student volunteers for a hematology research project and is found to be lacking one of four a-globin genes. Previously, he had several hematologic studies that were within normal limits. The significance of this unexpected finding suggests that the student
A. has a moderate degree of erythroid hyperplasia in bone marrow B. has an abnormal hemoglobin concentration C. has numerous target cells in the peripheral blood D. is an asymptomatic carrier of a-thalassemia E. may develop severe hemolytic anemia if exposed to oxidant drugs |
Option D (is an asymptomatic carrier of a-thalassemia) is correct. Deletion of one of the four a-globin genes produces a silent carrier state, and no hematologic abnormalities are evident. One of the chromosome 16 genes carries this deficiency. If such an individual has offspring with another carrier, the children could have the a-thalassemia trait. There are four functional a-globin genes; thus, there are four possible degrees of a-thalassemia (based on the loss or one to four genes). This individual has the mildest form; the most severe form is associated with fetal death in utero.
|
Option A (has a moderate degree of erythroid hyperplasia in bone marrow), Option B (has an abnormal hemoglobin concentration),
Option C (has numerous target cells in the peripheral blood), and Option E (may develop severe hemolytic anemia if exposed to oxidant drugs) are incorrect. Loss of one a-globin allele is silent and results in no hematologic abnormalities, such as hemoglobin Bart's. Sensitivity to oxidant drugs (e.g., antimalarials, sulfonamides, nitrofurantoin, phenacetin, aspirin in large doses, vitamin K derivatives) is associated with glucose-6-phosphate dehydrogenase deficiency, not with a-thalassemia. |
|
|
A 14-year-old boy has a history of prolonged bleeding from minor cuts and trauma. Hematologic studies show normal prothrombin time and normal partial thromboplastin time. An earlobe bleeding time is 14 minutes. Platelet aggregation tests with adenosine diphosphate (ADP), epinephrine, and collagen are normal. Platelets fail to aggregate with ristocetin, even with the addition of normal von Willebrand factor (vWF). A diagnosis of Bernard-Soulier syndrome is confirmed. In a patient with this condition, platelets fail to
A. aggregate B. bind vWF C. degranulate D. form thromboxane A E. release ADP |
Option B (bind vWF) is correct. Bernard-Soulier syndrome is an autosomal recessive disorder characterized by giant platelets with membranes lacking glycoprotein Ib, the locus of the vWF receptor. This prevents the platelets from binding to the subendothelium and interferes with their ability to form a hemostatic plug in a focus of vascular injury.
|
Option A (aggregate) is incorrect. Platelets with an inability to aggregate are characteristic of thrombasthenia. The symptoms of Glanzmann's thrombasthenia, a rare autosomal recessive disorder, include mucosal and postoperative bleeding. Option C (degranulate) is incorrect. Platelets with an inability to degranulate are characteristic of storage pool disease, a group of mild bleeding disorders with defective secretion of platelet granule contents that stimulate platelet aggregation. Option D (form thromboxane A2) is incorrect. Cyclooxygenase inhibitors such as aspirin block the formation of thromboxane A2, a potent platelet-aggregating agent. Option E (release ADP) is incorrect. Platelets with an inability to release ADP are characteristic of storage pool disease, a group of mild bleeding disorders with defective secretion of platelet granule contents (especially ADP) that stimulate platelet aggregation. |
|
|
A 62-year-old woman sees her physician because of "lumps" in her armpits. Physical examination shows small rubbery nodes palpable in the axillae, groin, cervical triangles, and popliteal spaces. Both liver and spleen are palpable. Her leukocyte count is 87,000/mm
with 92% small lymphocytes. Biopsy of the lymph nodes shows an infiltrate of small lymphocytes completely effacing the nodal architecture. No suggestion of follicular pattern is apparent. Which of the following is the most likely diagnosis? A. B-cell lymphoma with no involvement of the bone marrow B. High-grade B-cell lymphoma with a rapidly fatal course C. Low-grade B-cell lymphoma with an indolent course D. Lymphoblastic lymphoma originating in the bone marrow E. T-cell lymphoma induced by human T-cell leukemia virus type 1 (HTLV-1) |
Option C is correct. Small lymphocytic lymphoma, which makes up about 4% of all non-Hodgkin's lymphomas (NHL), is a member of the low-grade group of the Working Formulation Classification. Of the low-grade lymphomas, only small lymphocytic lymphoma does not have a follicular (nodular) architecture.
|
Option A (B-cell lymphoma with no involvement of the bone marrow) is incorrect. Although almost all (>95% of cases) small lymphocytic lymphomas are of a B cell immunophenotype, about 60% of affected patients have involvement of the bone marrow.
Option B (high-grade B-cell lymphoma with a rapidly fatal course) is incorrect. Small lymphocytic lymphoma is an incurable, but generally indolent tumor. Prolonged survival is expected. Option D (lymphoblastic lymphoma originating in the bone marrow) is incorrect. Lymphoblastic lymphoma is a disease of the young population and would be formed of large lymphoid cells with prominent nuclei. Option E (T-cell lymphoma induced by human T-cell leukemia virus type 1) is incorrect. HTLV-1 causes a T-cell lymphoma that is characterized by skin involvement, generalized lymphadenopathy, hepatosplenomegaly, hypercalcemia, and circulating multilobed T lymphocytes. |
|
|
A 36-year-old man has generalized lymphadenopathy. A histologic examination of a lymph node shows a marked degree of follicular hyperplasia. Which of the following findings would best determine that this condition is a benign reactive process rather than neoplastic?
A. Polyclonality on DNA hybridization studies B. Presence of broad increase in IgG on high-resolution electrophoresis C. Presence of surface IgG on the cell membrane of the proliferating cells D. Presence of translocation t (14;18)(q32;q21) |
Option A (polyclonality on DNA hybridization studies) is correct. Polyclonality is a sign of a benign process. Lymphoma is the result of monoclonal expansion of a single cell that has become malignant.
|
Option B (presence of broad increase in IgG on high-resolution electrophoresis) is incorrect. This benign process is too nonspecific to be reliable. If the lymphoma does not produce immunoglobulin, this result has no diagnostic value.
Option C (presence of surface IgG on the cell membrane of the proliferating cells) is incorrect. Surface immunoglobulin is a B cell marker. Option D (presence of translocation t (14;18)(q32;q21)) is incorrect. This translocation is found in most cases of follicular lymphoma. |
|
|
An otherwise healthy 24-year-old woman sees her physician because of "lumps" in her neck. She has no significant family history. Her vital signs are normal, with no suggestion of fever. On palpation of the abdomen, there is no sign of organomegaly. Cervical lymph nodes in the left anterior cervical triangle are large, firm, and not matted. No other site of involvement can be detected by physical examination. A differential diagnosis suggests either Hodgkin's disease or non-Hodgkin's lymphoma. Which of the following is most characteristic of Hodgkin's disease?
A. Almost always involves multiple peripheral groups of lymph nodes B. Typically arises in a single axial group of lymph nodes C. Typically involves extensive extranodal areas D. Typically involves mesenteric lymph nodes and Waldeyer's ring E. Usually skips over groups of nodes |
Option B (typically arises in a single axial group of lymph nodes) is correct. Hodgkin's disease usually arises within a single group of nodes and then spreads contiguously from that point.
|
Option A (almost always involves multiple peripheral groups of lymph nodes), Option C (typically involves extensive extranodal areas),
Option D (typically involves mesenteric lymph nodes and Waldeyer's ring), and Option E (usually skips over groups of nodes) are incorrect. All of these characteristics are more commonly found in patients with non-Hodgkin's lymphoma. |
|
|
A patient has vague symptoms of weakness and fatigue and decreased exercise tolerance. Laboratory studies show a leukocyte count of 11,000/mm with 7% blasts on the peripheral smear. Bone marrow aspirate shows 40% myeloblasts. Acute myeloblastic leukemia is suspected. This patient is most likely between the ages of
A. birth to 2 years B. 2-10 year C. 10-15 years D. 15-40 years E. >40 years |
Option D is correct. Acute myeloblastic leukemia (AML) is primarily a disease of young adults.
|
Option A (birth to 2 years) Option B (2-10 years) Option c (10-15 years), and Option E (>40 years) are incorrect. A young age is more consistent with acute lymphoblastic leukemia (ALL). Acute myeloblastic leukemia (AML) accounts for only 20% of childhood leukemias. Individuals who are more than 40 years of age are more liable to develop chronic myeloid leukemia (CML).
|
|
|
A 67-year-old woman with a 15-year history of severe coronary artery disease and multiple infarcts of the left ventricle and interventricular septum is hospitalized with acute pulmonary edema. Which of the following conditions is the primary physiologic event leading to pulmonary edema?
A. Decreased plasma oncotic pressure B. Left-sided congestive heart failure C. Lymphatic obstruction D. Right-sided congestive heart failure E. Volume overload |
Option B (left-sided congestive heart failure) is correct. Failure of the left ventricle causes increased pressure in the pulmonary circulation, which leads to a net movement of fluid from the vascular to the extravascular compartment (Starling's hypothesis).
|
Option A (decreased plasma oncotic pressure) is incorrect. Reduced oncotic pressure, which is usually due to hypoalbuminemia, can either cause or contribute to movement of fluid from the vascular compartment to the extravascular compartment. It rarely causes pulmonary edema, compared with left-sided heart failure.
Option C (lymphatic obstruction) is incorrect. There is normally a small net movement of fluid from the vascular compartment to the extravascular compartment. Under normal circumstances, this fluid enters the lymphatics and is eventually returned to the blood via the thoracic duct. Although obstruction (e.g., in profound lymphangitic spread of carcinoma) can result in some degree of pulmonary edema, it is not a common cause. Option D (right-sided congestive heart failure) is incorrect. Right-sided ventricular failure would result in peripheral edema, not pulmonary edema. Option E (volume overload) is incorrect. Most often an iatrogenic cause of pulmonary edema, volume overload, can be avoided by careful fluid management. |
|
|
A 19-year-old man suffering from a gunshot wound is brought to the emergency department with rapidly developing profound hypovolemic shock from acute hemorrhaging. The bleeding is controlled, and he is admitted to the intensive care unit. One day after surgery, he appears to be in distress. Arterial blood gas analysis shows a pH of 7.28, PaCO2 of 60 mm Hg, and PaO2 of 70 mm Hg. Moist rales are heard over both lung fields on auscultation. He is using accessory muscles of respiration to aid in breathing, and is subsequently diagnosed with adult respiratory distress syndrome (ARDS). In the pathogenesis of ARDS, the final common pathway primarily involves defective or damaged
A. alveolar capillary endothelium B. Clara cells C. pulmonary surfactant D. type I pneumocytes E. type II pneumocytes |
Option A (alveolar capillary endothelium) is correct. The pathologic equivalent of ARDS is termed diffuse alveolar damage, which is primarily associated with endothelial injury. When the endothelium is injured, protein-rich fluid leaks into the extravascular space, which produces interstitial and intra-alveolar pulmonary edema. Hyaline-like membranes form, and organization of the exudate eventually occurs.
|
Option B (Clara cells) is incorrect. Clara cells are unciliated cells found in the epithelium of the respiratory and terminal bronchioles. These cells do not play a significant role in a patient with ARDS.
Option C (pulmonary surfactant) is incorrect. Lack of surfactant in the newborn causes respiratory distress syndrome (RDS). Although RDS shares some histologic similarities with the acute phase of ARDS, its origin is entirely different, and it does not progress to pulmonary fibrosis. Option D (type I pneumocytes) is incorrect. Toxic gases may damage type I cells and lead to denudation of the alveolar surface. However, this does not account for the leakage of fluid into the extravascular space. Proliferation of type II cells eventually replaces the lost type I cells, resulting in the characteristic "cobblestone" appearance of the alveoli. Option E (type II pneumocytes) is incorrect. Type II cells seem remarkably resistant to injury and account for much of the repair that occurs in the resolution of ARDS. |
|
|
A 53-year-old man with multilobe bronchopneumonia due to Streptococcus pneumoniae infection appears mildly cyanotic. Arterial blood gas analysis shows a PaO2 of 70 mm Hg and a PaCO2 of 42 mm Hg. Which of the following is the most likely explanation for hypoxia in this patient?
A. Edema in many alveoli due to pulmonary infection, preventing adequate gas exchange B. Insufficient ventilation due to pleural pain, preventing adequate oxygenation C. Multiple ventilation/perfusion (V/Q) units approaching zero, producing a physiologic shunt D. Serious reduction of blood flow in the pulmonary circulation due to pulmonary congestion |
Option C (multiple ventilation/perfusion units approaching zero, producing a physiologic shunt) is correct. In this patient, many of the infected areas of the pulmonary parenchyma have blood flowing through them, but the alveoli are filled with fluid or purulent exudate that reduces or prohibits ventilation. This effectively acts as a shunt by combining unoxygenated or poorly oxygenated blood with normally oxygenated blood from the unaffected areas of the lung. Therefore, blood leaving the lung has a reduced PaO2. As a general principle, the most common cause of a reduced PaO2 is the presence of low V/Q units.
|
Option A (edema in many alveoli due to pulmonary infection, preventing adequate gas exchange) is incorrect. This answer addresses only ventilation and does not consider perfusion. The mismatch is between ventilation and perfusion (V/Q ratio).
Option B (insufficient ventilation due to pleural pain, preventing adequate oxygenation) is incorrect. Reduced ventilation primarily tends to increase PaCO2, but does not decrease PaO2 until late in the disease process. Option D(serious reduction of blood flow in of the pulmonary circulation due to pulmonary congestion) is incorrect. With normal circulation, red blood cells are completely oxygenated when they have passed about one-third of the distance through an alveolar capillary. Slowing blood flow through the lungs would neither affect the PaO2 nor reduce the ability of the lungs to fully saturate hemoglobin with oxygen. |
|
|
A 29-year-old man is brought to the emergency department after sustaining third-degree burns over 60% of his body. Twenty-four hours later, he develops adult respiratory distress syndrome (ARDS). Which of the following physiologic features would suggest a diagnosis of restrictive lung disease in this patient?
A. Decreased PaO2 B. Decreased pulmonary elastic recoil C. Decreased total lung volume D. Increased PaCO2 E. Increased pulmonary blood flow |
Option C (decreased total lung volume) is correct. All of the restrictive lung diseases, including ARDS, have a unifying physiologic abnormality\: reduction in total lung capacity. This is often due to parenchymal lung disease, but it can also be the result of neuromuscular disease, skeletal diseases, pleural disease, and acute trauma such as bilaterally fractured ribs that produce a flail chest.
|
Option A (decreased PaO2) is incorrect. Changes in PaO2 would be a secondary phenomenon primarily due to development of an abnormal V/Q ratio.
Option B (decreased pulmonary elastic recoil) is incorrect. Elastic recoil of the lung increases in restrictive lung disease, which results from changes in the pulmonary parenchyma. With other causal conditions, it would not be expected to change significantly. Option D(increased PaCO2) is incorrect. Changes in PaCO2 are a secondary phenomenon. Increasing PCO2 is a grave sign, and is caused by lack of sufficient alveolar ventilation. Option E (increased pulmonary blood flow) is incorrect. Changes in pulmonary blood flow would be a secondary phenomenon. |
|
|
A 12-year-old child develops wheezing and dyspnea after petting a cat. The child is suffering from which of the following forms of asthma?
A. Allergic bronchopulmonary aspergillosis B. Atopic asthma C. Intrinsic nonreaginic asthma D. Intrinsic pharmacologic asthma E. Occupational asthma |
Option B (atopic asthma) is correct. Atopic, or allergic, asthma involves a type I hypersensitivity reaction. The binding of an inhaled specific allergen, such as cat dander, to IgE on the surface of a mast cell induces an attack of typical atopic asthma.
|
Option A (allergic bronchopulmonary aspergillosis) is incorrect. Colonization of the bronchi by Aspergillus with development of hypersensitivity to the fungus is the cause of allergic bronchopulmonary aspergillosis.
Option C (intrinsic nonreaginic asthma). A viral infection, exposure to cold, or inhaled irritants are all associated with intrinsic nonreaginic asthma. The triggering mechanisms are nonimmune. The mechanism is not well understood but thought to be due, at least in part, to unusually reactive airways. Option D(intrinsic pharmacologic asthma) is incorrect. Ingestion of aspirin or a nonsteroidal anti-inflammatory drug generally causes this type of asthma. It is thought that aspirin blocks cyclooxygenase, reducing prostaglandins but not affecting production of leukotrienes. The imbalance causes bronchoconstriction. Option E (occupational asthma) is incorrect. Fumes or inhaled air pollutants usually induce this occupational asthma, which may be mediated by IgG. Often, no specific mechanism can be identified. |
|
|
A 17-year-old boy works for a contractor sandblasting painted concrete surfaces during his summer vacation. In a dusty environment such as this, which of the following sizes of potentially inhaled dust particles has the greatest capacity for causing pulmonary injury?
A. <1 mm B. 1mm C. 5mm D. 10mm E. >20mm |
Option B (1 mm) is correct. Dust particles within the size range of 1mm have great potential for causing pulmonary injury. Bacteria fit nicely into this size range. Shape is also an important factor in considering capacity for pulmonary injury. Although objects such as asbestos fibers are quite long, they can also gain access to the terminal airways and alveoli because they are thin.
|
Option A (<1 mm) is incorrect. Particles of this size usually act more like gases than particles, and although they may enter the alveoli, they usually exit with expiration.
Option C (5mm) is incorrect. Particles of this size tend to impinge on the mucociliary blanket. Here they are trapped and removed as mucus is moved to the oropharynx, where it is swallowed or expectorated. Option D (10 mm) is incorrect. Particles of this size are usually deposited in the nose and do not gain access to the lower respiratory tract. Ottion E (>20 mm) is incorrect. Particles >10mm in size are usually deposited in the nose and do not gain access to the lower respiratory tract. |
|
|
A 67-year-old woman is admitted to the hospital with symptoms of pleuritic chest pain, cough productive of rusty looking sputum containing innumerable neutrophils, and a temperature of 39.2\'b0C (102.5\'b0F). She is an alcoholic. X-ray film of the chest shows that most of the right middle lobe is opacified. Which of the following is the most likely cause of the infection?
A. Haemophilus influenzae B. Klebsiella pneumoniae C. Mycoplasma pneumoniae D. Staphylococcus aureus E. Streptococcus pneumoniae |
Option E 9Streptococcus pneumoniae) is correct. The x-ray film of the chest shows the presence of an intra-alveolar exudate with lobar or segmental consolidation.
S. pneumoniae (pneumococcus) accounts for 90-95% of cases of lobar pneumonia. Alcoholism is a major risk factor for pneumonia and can lead to increased morbidity and mortality. |
Option A (Haemophilus influenzae) is incorrect. This bacterium more commonly produces bronchopneumonia, which has a patchy distribution of inflammation apparent on a chest x-ray film, although it can occasionally produce a lobar pattern.
Option B (Klebsiella pneumoniae) is incorrect. Although this bacterium is the second most common cause of lobar pneumonia, it occurs in a small minority of cases. The exudate in Klebsiella pneumonia tends to be thick, sticky, and often bloody. In addition, this pathogen also tends to be tissue destructive. Option C (Mycoplasma pneumoniae) is incorrect. This bacterium causes atypical pneumonia, which is an interstitial pneumonitis rather than an intra-alveolar infection. Option D (Staphylococcus aureus) is incorrect. This bacterium more commonly produces bronchopneumonia. A chest x-ray film will show a patchy distribution of inflammation, with a tendency to abscess formation. |
|
|
A 58-year-old man who has smoked 2 packs of cigarettes daily for 30 years has a chronic cough and occasionally produces blood-tinged sputum. X-ray film of the posteroanterior chest shows a mass in the region of the hilum of the left lung. His serum calcium level is 12.5 mg/dL; other laboratory studies are within normal limits. Cytology of the sputum is positive for the presence of malignant cells. The most likely cause of the paraneoplastic syndrome in this patient is
A. adenocarcinoma B. bronchial carcinoid tumor C. bronchioloalveolar cell carcinoma D. small cell carcinoma E. squamous cell carcinoma |
Option E(squamous cell carcinoma) is correct. Any histologic type of neoplasm may produce any of the paraneoplastic syndromes associated with lung cancer, but squamous cell carcinoma is most often associated with hypercalcemia.
|
Option A (adenocarcinoma) and Option C (bronchioloalveolar cell carcinoma) are incorrect. Adenocarcinoma or bronchioalveolar cell carcinoma may occasionally produce any of the paraneoplastic syndromes associated with carcinoma of the lung, but they are not associated with hypercalcemia.
Option B (bronchial carcinoid tumor) is incorrect. A bronchial carcinoid tumor is rarely associated with the production of a paraneoplastic syndrome. Option D (small cell carcinoma) is incorrect. Small cell (or oat cell) carcinomas are more likely to be associated with secretion of antidiuretic hormone or adrenocorticotropic hormone. |
|
|
A 69-year-old man sees his physician because of increasing shortness of breath. X-ray film of the chest shows that most of the right lung is encased by a thick layer of moderately dense tissue. Pleural fluid is blood-tinged with numerous atypical cells. The patient is most likely to have a history of occupational exposure to which of the following substances?
A. Asbestos B. Formalin C. Hematite D. Nickel carbonyl E. Silica |
Option A (asbestos) is correct. About 90% of malignant mesotheliomas are related to occupational exposure to asbestos. Individuals who have been exposed to asbestos have an 8% risk of developing malignant mesothelioma. There is a long latent period, with the tumor appearing from about 20-40 years after exposure to the substance.
|
Option B (formalin) is incorrect. Formalin has been attributed to a number of untoward effects; however, pathologists have received extensive exposure to formalin for many years without a strong association with any conditions, except rare hypersensitivity reactions. Formalin has no association with malignant mesothelioma.
Option C (hematite) is incorrect. Exposure to hematite dust may cause siderosis of the lung and perhaps fibrosis. Option D (nickel carbonyl) is incorrect. Nickel carbonyl is associated with development of squamous cell carcinoma of the paranasal sinuses and lung. Option E (silica) is incorrect. Silica exposure is associated with pulmonary fibrosis. |
|
|
A 65-year-old woman is undergoing a physical examination when the physician notices her mucous membranes are somewhat pale and her tongue is beefy red to magenta colored. There is slight cracking of the skin around the angles of her mouth, and her fingernails are slightly spoon-shaped. She has difficulty swallowing. Laboratory studies show a red blood cell count of 12 mL/kg and a hematocrit of 30%. The most likely cause of this patient's condition is a deficiency of
A. iron B. niacin C. pyridoxine D. riboflavin E. vitamin B12 |
Option A (iron) is correct. The history and physical findings suggest that the woman has Plummer-Vinson syndrome, which is characterized by iron-deficiency anemia, glossitis, cheilosis, and dysphagia due to formation of upper esophageal webs.
|
Option B (niacin), Option C (pyridoxine), Option D (riboflavin), and Option E (vitamin B12) are incorrect. Lack of niacin and pyridoxine have been associated with a minor degree of glossitis. Although lack of riboflavin may be associated with glossitis, it is not found with other characteristics of Plummer-Vinson syndrome. Lack of vitamin B12 can cause glossitis and anemia, but not esophageal dysphagia.
|
|
|
A 43-year-old woman sees her physician because of a swollen gland on the left side of her neck. Examination shows a firm mass in the left parotid gland. On palpation, the mass does not move with the overlying skin. The most likely diagnosis is
A. acinic cell carcinoma B. adenoid cystic carcinoma C. mucoepidermoid carcinoma D. pleomorphic adenoma E. Warthin's tumor |
Option D (pleomorphic adenoma) is correct. This benign tumor accounts for about 50% of salivary gland tumors. The location of the tumor (in the left parotid gland) and the sex of the patient (female) increase the likelihood of the tumor being a pleomorphic adenoma.
|
Option A (acinic cell carcinoma), Option B (adenoid cystic carcinoma),
Option C mucoepidermoid carcinoma), and Option E (Warthin's tumor) are incorrect. All of the other salivary gland tumors listed are much less common than pleomorphic adenoma. Acinic cell carcinoma accounts for about 3% of salivary gland tumors. Adenoid cystic carcinoma, which is more common in the minor salivary glands, accounts for about 10% of salivary gland tumors. Mucoepidermoid carcinoma accounts for about 16% of salivary gland tumors. Warthin's tumor affects men more than women and accounts for about 11% of salivary gland tumors. Other tumors account for small percentages of salivary gland tumors, such as squamous cell carcinoma (about 1%). |
|
|
A 54-year-old man with a history of gastroesophageal reflex disease (GERD) is prescribed a proton pump inhibitor. He says he cannot afford the medication and is unable to adhere to the recommended treatment regimen, but instead relies on over-the-counter medications such as antacids and herbal remedies. Brush cytology of the esophagus shows marked reactive changes of the squamous cells as well as the presence of reactive glandular cells consistent with origin in the body of the stomach. This patient is most seriously at risk of developing
A. adenocarcinoma B. esophageal candidiasis C. esophageal stenosis D. esophageal varices E. ulceration of the esophageal mucosa |
Option A (adenocarcinoma) is correct. The presence of glandular cells in the esophageal brushing indicates that the patient has glandular metaplasia of the esophageal mucosa, or Barrett's esophagus (metaplastic columnar epithelium), a complication of chronic GERD. Adenocarcinoma of the esophagus is 30-40 times more likely to occur in patients with Barrett's esophagus.
|
Option B (esophageal candidiasis) is incorrect. Esophageal candidiasis is not a complication of GERD or Barrett's esophagus. It would tend to be found in immunocompromised or debilitated patients.
Option C (esophageal stenosis) is incorrect. Although esophageal stenosis is a frequent complication of GERD and Barrett's esophagus, it is not a life-threatening condition. Option D (esophageal varices) is incorrect. Development of varices is not a complication of GERD. Option E (ulceration of the esophageal mucosa) is incorrect. Although ulceration of the esophageal mucosa is not an uncommon complication of GERD or Barrett's esophagus, it is not life-threatening unless serious bleeding, an unusual event, occurs. |
|
|
A 62-year-old man who has smoked three packs of cigarettes daily for 40 years has shortness of breath on exertion. He is thin with a somewhat expanded barrel-shaped chest and ribs that tend to be somewhat horizontal. He breathes through pursed lips. He is not cyanotic. Forced expiratory volume in 1 second (FEV1) is 16% of predicted value. His oxygen saturation is 80%. Which of the following is the most likely cause of this patient's reduced FEV1?
A. Airway obstruction due to a reduction in elastic recoil of the lung B. Airway obstruction due to severe bronchospasm C. Bronchiolar obstruction due to mucous gland hyperplasia and mucous secretion D. Inability to adequately use accessory muscles of respiration in expiration E. Ventilation/perfusion ratio <1.0 |
Option A (airway obstruction due to a reduction in elastic recoil of the lung) is correct. The patient has emphysema as a result of his history of cigarette smoking for 40 years. Smoking has resulted in the release of an excess of elastase by inflammatory cells (neutrophils and macrophages) in the lungs, causing destruction of the normal architecture of the pulmonary parenchyma. The result is a loss of normal lung elastance and an increase in compliance. Elastic recoil is one of the major sources of energy for movement of air out of the lung during expiration. When it is reduced, the pressure surrounding the small airways becomes greater than the pressure within them, resulting in dynamic collapse of the airway and hence obstruction to airflow in expiration. This normally occurs toward the end of expiration, but in patients with emphysema, it occurs too early, trapping air and increasing residual volume and reducing the FEV1.
|
Option B (airway obstruction due to severe bronchospasm) is incorrect. Bronchospasm is one of the major causes of airway obstruction in bronchial asthma and sometimes in chronic bronchitis. It does not play a role in patients with "pure" emphysema.
Option C (bronchiolar obstruction due to mucous gland hyperplasia and mucous secretion) is incorrect. Excessive secretion of bronchial mucus would cause obstruction in a patient with chronic bronchitis. Option D (inability to use the accessory muscles of respiration in expiration adequately) is incorrect. Such inability might be a cause of respiratory difficulty in a patient with a neuromuscular problem, but would not be a factor in a typical patient with emphysema. Option E (ventilation/perfusion ratio <1.0) is incorrect. A change in V/Q (ventilation/perfusion) would not explain the diminished FEV1, which is a problem with lung mechanics. |
|
|
A 42-year-old man has a boring midepigastric pain and occasional tarry stools. Over-the-counter antacids relieve the pain, and aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) generally aggravate it. X-ray film of the upper gastrointestinal tract shows the presence of a 1- to 2-cm erosion in the duodenal mucosa about 4-cm distal to the pylorus. Which of the following is the most likely cause of this patient's condition?
A. Gastrinoma B. Helicobacter pylori infection C. Insulinoma D. NSAID ingestion E. Vitamin B12 deficiency |
Option B (Helicobacter pylori infection) is correct. Infection with
H. pylori causes the development of most duodenal and many gastric ulcers. The mechanism by which the organism causes peptic ulcer disease is not well understood. |
Option A (gastrinomas) is incorrect. Gastrinomas, which are gastrin-producing tumors, are an unusual cause of peptic ulcer disease, although the hypersecretion they induce can cause intractable ulceration.
Option C (insulinomas) is incorrect. Insulinomas are insulin-secreting islet cell tumors that cause hypoglycemia. They are not significantly associated with ulcer development. These tumors are usually benign. Option D (NSAID ingestion) is incorrect. Because of their COX-1 (cyclooxygenase-1) inhibitory activity, NSAIDs frequently cause ulceration in individuals who take large doses or in those individuals taking them for long periods of time. Option E (vitamin B12 deficiency) is incorrect. Deficiency of vitamin B12 is associated with chronic gastritis, not peptic ulcer disease. |
|
|
An autopsy of a 7-year-old boy who died of irreversible heart failure shows a patchy but focally dense infiltrate of chronic inflammatory cells, predominantly lymphocytes, in the myocardium. Cardiac myocytes in the vicinity of the lymphoid aggregates show focal necrosis. No abnormalities of the cardiac vasculature are evident. Light microscopy shows no organisms. Which of the following is most commonly associated with these findings?
A. Chronic toxoplasmosis B. Corynebacterium diphtheriae C. Lyme disease D. Recent acute viral illness E. Rubella |
Option D (recent acute viral illness) is correct. Infectious myocarditis is most often associated with an acute viral illness of recent occurrence (possibly with the past 5-30 days) involving an organ other than the heart. Offending organisms are typically coxsackievirus, echovirus, poliovirus, and influenza. Diagnosis of the etiologic agent often requires demonstration of a rising titer of antibody against the suspected virus.
|
Option A (chronic toxoplasmosis) is incorrect. Toxoplasmosis is caused by the protozoan Toxoplasma gondii; it is not a recognized cause of infectious myocarditis.
Option B (Corynebacterium diphtheria) is incorrect. The toxin produced by the bacterium causes myocarditis, which results in focal myocardial damage. It does not cause a significant lymphocytic infiltrate. Option C (Lyme disease) is incorrect. Lyme disease is caused by the spirochete Borrelia burgdorferi, which results in myocarditis in as many as two-thirds of affected individuals. The condition is usually transitory. Bacteria sometimes can be found in the myocardium. Option E (rubella) is incorrect. This usually mild systemic viral disease is not a recognized cause of infectious myocarditis. |
|
|
Meckel's diverticulum is an uncommon congenital malformation that is usually a clinically silent condition. In some cases, Meckel's diverticulum can be confused with appendicitis in the presence of
A. heterotopic gastric tissue B. heterotopic pancreatic tissue C. obstruction of the small intestine D. roundworm infestation E. ulcerative colitis |
Option A (heterotopic gastric tissue) is correct. Meckel's diverticulum is a congenital malformation of the small intestine, and occurs in about 2% of the population. It is uncommon, but not rare. If the diverticulum contains heterotopic gastric mucosa, it may ulcerate and cause significant bleeding. It can produce symptoms similar to appendicitis (e.g., right lower quadrant pain).
|
Option B (heterotopic pancreatic tissue) is incorrect. The presence of pancreatic tissue would not cause ulceration and bleeding.
Option C (obstruction of the small intestine) is incorrect. Obstruction may occur if there is intussusception or incarceration of the diverticulum. Option D (roundworm infestation) is incorrect. Roundworms may cause vague abdominal discomfort. Option E (ulcerative colitis) is incorrect. Ulcerative colitis would not be found in the presence of Meckel's diverticulum. Except for a "wash-through" effect to the terminal ileum, ulcerative colitis is a condition that affects the large bowel only. |
|
|
A 4-year-old boy develops hemarthrosis of the right knee with no known preceding traumatic episode. He has not shown any previous abnormal bleeding tendencies associated with the usual childhood trauma. The patient's history suggests an X-linked recessive trait on his mother's side of the family. Which of the following studies would most likely be abnormal?
A. Bleeding time B. Partial thromboplastin time (PTT) C. Prothrombin time (PT) D. Thrombin time |
Option B (partial thromboplastin time) is correct. PTT is a measure of the intrinsic clotting pathway and is abnormal if factor VIII or factor IX activity is reduced. Although PTT is generally adequate to screen for hemophilia, factor VIII or factor IX assay are required to confirm the diagnosis. Hemophilia A and hemophilia B are not clinically distinguishable.
|
Option A(bleeding time), Option C (prothrombin time), and Option D(thrombin time) are incorrect. Bleeding time is primarily a test of platelet function, and in both hemophilia A and hemophilia B, platelet function is normal. PT, which measures the extrinsic pathway, and thrombin time, which depends on the formation of fibrin from fibrinogen, are normal.
|
|
|
A 24-year-old woman in her first trimester of pregnancy complains of heat intolerance. Physical examination shows a slightly enlarged, nontender thyroid gland. Thyroid function studies show a serum thyroxine (T4) level of 14 mg/dL and a serum thyroid-stimulating hormone (TSH) level of 3.0 mU/mL. Which of the following best explains the results of these studies?
A. Decreased thyroid-binding globulin B. Increased synthesis of T4 C. Increased synthesis of triiodothyronine (T3) D. Thyroiditis-induced release of T4 E. Normal finding in pregnancy |
Option E (normal finding in pregnancy) is correct. The total serum T4 level reflects free T4 (unbound and metabolically active) and T4 bound to thyroid-binding globulin (TBG, metabolically inactive). The increase in estrogen that normally occurs during pregnancy stimulates liver synthesis of TBG. Because T4 normally occupies one third of the binding sites on TBG, the additional TBG with its bound fraction increases the total level of T4. The amount of T4 synthesized by the thyroid gland is in balance with the levels of free T4 in the serum; hence the free T4 levels remain the same and the patient is clinically euthyroid. Because free T4 has a negative feedback relationship with TSH, the serum TSH level also remains normal. Thus, an increase in serum T4 in the presence of a normal TSH level indicates that the patient has an increase in TBG, most likely secondary to an increase in estrogen. An enlarged thyroid gland and heat intolerance are normal findings in a pregnant patient.
|
Option A (decreased thyroid-binding globulin) is incorrect. Estrogen increases liver synthesis of TBG.
Option B (increased synthesis of T4) and Option C (increased synthesis of T3) are incorrect. The patient's TSH level is normal, indicating that free hormone levels must be normal. Option D(thyroiditis-induced release of thyroxine) is incorrect. The TSH level is normal, indicating that the patient is euthyroid. Patients with hyperthyroidism have increased free T4 levels and corresponding TSH suppression. |
|
|
A 1-month-old neonate has failure of separation of the umbilical cord. Histologic sections of the surgically removed cord show an absence of neutrophil pavementing and emigration into the interstitial tissue. The clinical and histologic findings in this case are most closely associated with a defect in
A. activation of the complement system B. microtubule polymerization C. respiratory burst mechanism D. synthesis of adhesion molecules E. synthesis of myeloperoxidase |
Option D (synthesis of adhesion molecules) is correct. Neutrophil adhesion to endothelial cells (pavementing) is due to the synthesis of adhesion molecules, which are CD11 /CD18 complexes of glycoproteins. Both neutrophils and endothelial cells synthesize adhesion molecules. Neutrophil adhesion molecule synthesis is stimulated by the complement component C5a and leukotriene LTB4. Synthesis of endothelial cell-derived adhesion molecules is stimulated by interleukin-1 and tumor necrosis factor. Congenital adhesion molecule deficiency can be acquired or genetic. A key feature is failure of separation of the umbilical cord and the absence of neutrophil pavementing and emigration into the umbilical tissue. These patients also have problems with wound healing.
|
Option A (activation of the complement system) is incorrect. Complement deficiencies are more often associated with susceptibility to infections than with adhesion molecule defects.
Option B (microtubule polymerization) is incorrect. This describes a rare autosomal recessive disease called Chediak-Higashi syndrome, which is associated with severe infections related to defects in chemotaxis and phagocytosis. Option C (respiratory burst mechanism) is incorrect. This describes chronic granulomatous disease (CGD) of childhood. CGD is a sex-linked recessive disease characterized by an absence of NADPH oxidase in the cell membranes of neutrophils and monocytes. In a normal neutrophil or monocyte, the presence of NADPH oxidase + NADPH causes the conversion of molecular oxygen into superoxide free radicals (FRs) in phagosomes. The energy released by this reaction is called the respiratory burst. Superoxide FRs then are converted by superoxide dismutase into peroxide. The lysosomal enzyme myeloperoxidase (MPO) then combines peroxide with chloride ions to produce bleach, which is bactericidal to bacteria. Hence, in patients with CGD, who are deficient in NADPH oxidase, there is no respiratory burst, superoxide FRs, peroxide, or bleach to kill bacteria. Option E (defect in the synthesis of myeloperoxidase) is incorrect. The loss of MPO is associated primarily with a microbicidal defect related to the inability to produce bleach in the phagosome. In contrast to CGD, the respiratory burst is intact in MPO deficiency. |
|
|
A 62-year-old man with small cell carcinoma of the lung complains of a headache and visual disturbances. An MRI of the head shows cerebral edema but no evidence of metastatic disease. There is no evidence of pitting edema or volume depletion. The serum Na+ level is 110 mEq/L. Assuming the patient has a normal salt and water intake, which of the following is the most appropriate nonpharmacologic treatment for this patient?
Na+intake H2O intake A. Decrease Decrease B. Decrease No change C. Increase Increase D. No change Decrease E. No change No change |
Option D (no change in Na+; decrease H2O intake) is correct. The patient has the syndrome of inappropriate antidiuretic hormone (ADH), or SIADH, due to ectopic secretion of ADH by a primary lung cancer (small cell carcinoma). ADH is normally involved in the reabsorption of electrolyte free water in the collecting tubules of the kidneys, which concentrates the urine. Therefore, an excess of ADH results in increased reabsorption of water, which enters the extracellular fluid (ECF) compartment and produces a dilutional hyponatremia. Hyponatremia then establishes an osmotic gradient favoring the movement of water into the intracellular fluid (ICF) compartment, which produces cerebral edema. Because pure water is added to both the ECF and ICF compartments, the best nonpharmacologic treatment is water restriction.
|
Option A(decrease Na+ and H2O intake) is incorrect. The hyponatremia is related to the addition of pure water to the ECF and not to a loss of sodium.
Option B (decrease Na+; no change in H2O intake) and Option C (increase Na+ and H2O intake) are incorrect. Refer to the discussion for Option D. Option E (no change in either Na+ or H2O intake) is incorrect. Water must be restricted in the patient. Refer to the discussion for Option D. |
|
|
A 62-year-old man has smoked two packs of cigarettes a day for 30 years. He states that almost every morning during this time, he has coughed up a tablespoon or more of yellow-green sputum. Physical examination shows cyanosis of the skin and mucous membranes, an increased anteroposterior diameter of the chest. On auscultation, scattered sibilant rhonchi and rales are heard in both lung fields. Referring to the figure, which of the following letters, labeled A through F on the curves, represents the expected arterial blood gases in this patient?
A. B. C. D. E. F. |
Option B (decreased arterial pH; increased arterial PCO 2; increased serum HCO3) is correct. The patient has chronic obstructive pulmonary disease (COPD) with cyanosis secondary to hypoxemia (decreased arterial PO2). Chronic bronchitis is the primary type of COPD in a patient who has had a productive cough for the majority of the time he has smoked. Obstruction to airflow secondary to inflammation and increased mucus production is at the level of the terminal bronchioles. Therefore, during expiration, air with high concentrations of CO2 is trapped behind the obstruction. Retention of CO2 in the alveoli increases the arterial PCO2, causing respiratory acidosis. Point B on the graph depicts an acid arterial pH, a PCO2 close to the 60 mm Hg isobar, and an HCO level above the normal of 24 mEq/L. Because the patient has had COPD for most of his life, there has been ample time for the kidneys to reclaim and synthesize HCO, producing metabolic alkalosis to compensate for the respiratory acidosis. Compensation for all acid-base disorders brings the pH close to, but not into, the normal range for arterial pH. This describes a partially compensated acid-base condition. Full compensation rarely occurs because it implies that the arterial pH is brought back into the normal range. The absence of compensation indicates that there has not been enough time for the lungs to compensate for primary metabolic conditions or for the kidneys to compensate for primary respiratory conditions.
|
Option A (decreased arterial pH; increased arterial PCO2 ; increased serum HCO) is incorrect. These findings are most consistent with a partially compensated acute respiratory acidosis. When compared with Option B (a patient with chronic respiratory acidosis), the lack of adequate compensation has done little to raise the arterial pH. Examples of acute respiratory acidosis include depression of the medullary respiratory center (e.g., patient taking barbiturates); paralysis of the muscles of respiration (e.g., polio, Guillain-Barr\'e9 syndrome); and severe pneumonia.
Option C (increased arterial pH; increased arterial PCO2; increased serum HCO) is incorrect. These findings are most consistent with a partially compensated primary metabolic alkalosis (compensation is respiratory acidosis). Examples include diuretics (patient taking primarily loop diuretics and thiazides), vomiting, and mineralocorticoid excess (e.g., primary aldosteronism). Option D (decreased arterial pH; decreased arterial PCO2; decreased serum HCO) is incorrect. These findings are most consistent with a partially compensated primary metabolic acidosis (respiratory alkalosis is compensation). Examples include renal failure, lactic acidosis, ketoacidosis, and renal tubular acidosis. Option E (increased arterial pH; decreased arterial PCO2; decreased serum HCO3 ) is incorrect. These findings are most consistent with a partially compensated primary acute respiratory alkalosis (metabolic acidosis is compensation). Examples include anxiety, a pulmonary embolus, and restrictive lung disease (e.g., sarcoidosis). Option F (increased arterial pH; decreased arterial PCO2; decreased serum HCO ) is incorrect. These findings are most consistent with a partially compensated chronic respiratory alkalosis. Living at high altitudes is the best example of this condition. |
|
|
A 25-year-old woman has not had her menstrual period for the past 8 months. She is 62 inches tall and weighs 41 kg (90 lb). She states that she has been trying to lose weight for her upcoming wedding. A urine pregnancy test is negative. The patient is given an intramuscular injection of progesterone. Ten days later she reports that she has had no withdrawal bleeding. Laboratory studies show the following serum levels:
Prolactin 10 ng/mL Follicle stimulating hormone (FSH) 3 mIU/mL Luteinizing hormone (LH) 2 mIU/mL Thyroid-stimulating hormone (TSH) 4.1 m U/mL Estradiol Low Cortisol (a.m.), 35 mg/dL Growth hormone 10 ng/mL Which of the following is the most likely diagnosis? A. Acromegaly B. Cushing's syndrome C. Hypopituitarism D. Primary ovarian disease E. Weight loss syndrome |
Option E (weight loss syndrome) is correct. When the body fat of a female is less than 15% of normal for her size and weight, hypothalamic secretion of gonadotropin-releasing hormone (GnRH) decreases. This results in decreased stimulation of anterior pituitary release of the gonadotropins FSH and LH. Loss of gonadotropins results in insufficient synthesis of estrogen by the ovaries, with subsequent development of amenorrhea. Amenorrhea may be secondary to disorders involving the hypothalamic/pituitary axis in producing gonadotropins, the ovaries in synthesizing estrogen, or anatomic defects (end-organ disease) that prevent the normal egress of blood out of the vagina (e.g., cervical stenosis, imperforate hymen). A progesterone challenge is an excellent test used to evaluate the cause of amenorrhea once pregnancy is ruled out. Withdrawal bleeding, when progesterone levels decrease, indicates adequate estrogen stimulation of the endometrial mucosa and absence of end-organ disease. Absence of withdrawal bleeding can indicate inadequate levels of estrogen or an end-organ problem. Measuring the levels of serum gonadotropins can help determine which of the three areas is responsible. In hypothalamic-pituitary axis disorders, gonadotropin levels are decreased; in ovarian disorders, gonadotropin levels are increased (loss of the estrogen and progesterone negative feedback on FSH and LH, respectively); and in end-organ disease, gonadotropin levels are normal. This patient's gonadotropin levels are decreased, indicating that the cause of this patient's amenorrhea lies in the hypothalamic-pituitary axis (i.e., excessive weight loss). An important clinical point to remember about weight loss syndromes, including anorexia nervosa, is that there is danger of osteoporosis related to the long-term loss of estrogen and its effect on maintaining normal bone density.
|
Option A (acromegaly) is incorrect. The increase in growth hormone is related to the stress of weight loss. This patient has none of the classic findings of acromegaly (e.g., prominent jaw, enlarged hands and feet).
Option B(Cushing's syndrome) is incorrect. The physical examination shows none of the classic findings of Cushing's syndrome (e.g., truncal obesity). Like growth hormone, cortisol is also a stress hormone that is increased in weight loss syndromes. Option C (hypopituitarism) is incorrect. Levels of cortisol and growth hormone are increased and serum TSH is normal in hypopituitarism. Option D (primary ovarian disease) is incorrect. Gonadotropin levels are low. |
|
|
A 30-year-old man develops an acute onset of confusion, ataxia, nystagmus, and ophthalmoplegia shortly after the administration of an intravenous (IV) solution containing 5% glucose and normal saline. The pathogenesis of this patient's neurologic disorder is most closely related to which of the following conditions?
A. Central pontine myelinolysis B. Purkinje cell atrophy C. Thiamine deficiency D. Viral encephalitis E. Vitamin B12 deficiency |
Option C (thiamine deficiency) is correct. The patient has developed acute Wernicke's encephalopathy, which is a clinical syndrome associated with thiamine deficiency. In the United States, alcoholism is the most common cause of thiamine deficiency. Thiamine is a cofactor in the pyruvate dehydrogenase complex, which catalyzes the conversion of pyruvate into acetyl CoA in the mitochondria. In this reaction, NAD+ is reduced to NADH, which results in the production of 6 ATP in the mitochondria. Decreased levels of acetyl CoA also affect the synthesis of citrate (acetyl CoA + oxaloacetic acid (citrate); hence the amount of ATP produced by the citric acid cycle is reduced. The reduction in ATP synthesis is primarily responsible for the clinical findings in thiamine deficiency (beriberi). In "wet beriberi," congestive cardiomyopathy leads to left-sided and right-sided heart failure; in "dry beriberi," demyelination results in peripheral neuropathies and the Wernicke-Korsakoff syndrome complex. Administering a glucose-containing solution to a patient with subclinical thiamine deficiency results in the consumption of the remaining thiamine in the pyruvate dehydrogenase complex reaction, which precipitates acute Wernicke's encephalopathy. Clinical features of Wernicke's encephalopathy include confusion, ataxia, nystagmus, and ophthalmoplegia. This underscores the importance of administering thiamine intravenously before infusing glucose-containing solutions.
|
Option A (central pontine myelinolysis) is incorrect. This is a demyelination syndrome associated with a rapid IV administration of saline in a patient who has hyponatremia.
Option B (Purkinje cell atrophy) is incorrect. Atrophy of Purkinje cells in the cerebellum is a complication of chronic alcoholism, but does not produce acute Wernicke's encephalopathy Option D (viral encephalitis) is incorrect. The signs and symptoms of encephalitis are primarily headache and mental status abnormalities. Option E (vitamin B 12 deficiency) is incorrect. Vitamin B12 deficiency is associated with subacute combined degeneration in the spinal cord, with demyelination of the posterior column (lack of proprioception, wide-based gait) and lateral corticospinal tract (spasticity, positive Babinski sign). |
|
|
During a routine physical examination of a 13-year-old boy, the physician notices bilaterally enlarged, nontender testicles that do not transilluminate. Additional physical findings include a long face with prominent jaw, high arched palate, and protruding ears. The child has a speech disability and is in a special educational program at school. Which of the following studies would most likely be abnormal in this patient?
A. Buccal smear B. Chromosome study of the father C. DNA analysis of the X chromosome D. Serum gonadotropins E. Testicular biopsy |
Option C (DNA analysis of the X chromosome) is correct. This child has fragile X syndrome (FXS). FXS is thought to be a sex-linked recessive syndrome; however, some patients appear to have a sex-linked dominant inheritance pattern, with a fragile site or gap at the end of the long arm of the X chromosome. At this site, there are triplet repeats of three nucleotides (e.g., CGG-CGG-CGG...). An interesting phenomenon associated with triplet repeat mutations is that there is progressive worsening of the disease in future generations (called anticipation) and signs of mental retardation or impaired learning in carrier females. The disease is exacerbated because more triplet repeats occur in individuals in each succeeding generation, which explains why female carriers may also express the disease. DNA analysis of the X chromosome in lymphocytes identifies the triplet repeats and is considered more sensitive than the fragile X chromosome study.
|
Option A (buccal smear) is incorrect. A buccal smear usually is performed to rule out deficient or extra X chromosomes. Normal females have random inactivation of one of the two X chromosomes. Hence, normal females have one Barr body, and normal males have no Barr bodies. The randomly inactivated chromosome becomes an appendage on the nuclear membrane of cells.
Option B (chromosome study of the father) is incorrect. X-linked conditions are transmitted to males via the carrier female and not by the affected father. Option D (serum gonadotropins) is incorrect. The patient shows no clinical evidence of hypogonadism, as in Klinefelter's syndrome, where the testicles are atrophic. Option E (testicular biopsy) is incorrect. The patient does not have a testicular neoplasm or signs of Klinefelter's syndrome. |
|
|
A 28-year-old man who was hit by a car while crossing the street is immediately taken by ambulance to a nearby hospital. Physical examination shows diminished pulse, cold, clammy skin, and blood pressure of 60/40 mm Hg. Additional findings include an open right femoral fracture and tenderness over the left lower rib cage. The patient is infused with 3 L of 0.9% normal saline and a blood sample is drawn. Which of the following results would be expected from this sample?
A. Low hemoglobin (Hgb) and low hematocrit (Hct) B. Low mean corpuscular volume (MCV) C. Low serum glucose concentration D. Low serum sodium concentration E. Low white blood cell (WBC) count |
Option A (low hemoglobin and low hematocrit) is correct. The patient is in hypovolemic shock secondary to blood loss from the open femoral fracture and a possible ruptured spleen. Initially, loss of whole blood does not alter the Hgb and Hct concentrations because equal amounts of red blood cells (RBCs) and plasma are lost. Within a few hours, however, sodium-containing fluid reabsorbed by the kidneys, along with fluid from the interstitial space, is added to the vascular compartment to restore volume. This uncovers the RBC deficit, leading to a decrease in the Hgb and Hct. If the patient is not transfused with packed RBCs, over the next few weeks to months, the bone marrow replaces the RBC deficit until the Hgb and Hct return to the normal range. However, if a patient with massive blood loss is infused with 0.9% normal saline to increase the blood pressure, the RBC deficit is uncovered immediately and the expected decrease in Hgb and Hct is noted in a complete blood cell count.
|
Option B (low mean corpuscular volume) is incorrect. The size of the RBCs is not altered by the immediate loss of RBCs.
Option C (low serum glucose concentration) is incorrect. The patient received 0.9% normal saline without glucose. Option D (low serum sodium concentration) is incorrect. The concentration of sodium remains the same because 0.9% normal saline is isotonic with plasma. Option E(low white blood cell count) is incorrect. Trauma causes the release of catecholamines, which decrease adhesion molecule synthesis, causing release of the marginating neutrophil pool in the peripheral blood into the circulating pool. This results in an absolute neutrophilic leukocytosis. |
|
|
A febrile 23-year-old woman complains of fatigue, right upper quadrant pain, and difficulty swallowing. Physical examination shows exudative tonsillitis, palatal petechia, tender cervical lymphadenopathy, splenomegaly, and tender hepatomegaly. A complete blood cell count shows mild microcytic anemia, lymphocytic leukocytosis with ~20% of the lymphocytes having atypical features, and a mild thrombocytopenia. Which of the following laboratory findings is expected in this patient?
A. Low total iron-binding capacity B. Normal serum ferritin C. Normal serum transaminases D. Positive hepatitis B surface antigen E. Positive heterophile antibody test |
Option E (positive heterophile antibody test) is correct. The patient most likely has infectious mononucleosis (IM), which is caused by the Epstein-Barr virus (EBV). The virus infects B cells initially by attaching to CD 21 receptors on the cell surface. Circulating T lymphocytes interact with the infected B cells and become antigenically stimulated, resulting in atypical lymphocytosis. The key screening test for IM is the Monospot test, which detects heterophile antibodies in the patient's serum. Heterophile antibodies unique to IM are IgM antibodies directed against horse red blood cells (RBCs). An agglutination reaction against horse RBCs is the basis for a positive Monospot test.
|
Option A (low total iron binding capacity) is incorrect. In young women, iron deficiency anemia secondary to menorrhagia is the most common cause of microcytic anemia. Hence, the total iron-binding capacity should be increased due to increased synthesis of transferrin (binding protein for iron) by the liver whenever iron stores in the bone marrow are decreased.
Option B (normal serum ferritin) is incorrect. The patient most likely has iron deficiency anemia and a low serum ferritin level. Serum ferritin reflects the amount of iron stored in macrophages in the bone marrow. Option C (normal serum transaminases) is incorrect. IM produces an anicteric viral hepatitis. The primary enzymes that are elevated in diffuse liver cell necrosis are serum transaminases, aspartate aminotransferase (AST), and alanine aminotransferase (ALT). Option D (positive hepatitis B surface antigen) is incorrect. The clinical history and physical findings are more compatible with IM-induced hepatitis than hepatitis due to the hepatitis B virus. |
|
|
A 65-year-old man has a history of an elevated red blood cell (RBC) count, frequent headaches, and pruritus after bathing. He now complains of a sudden onset of abdominal pain and bloody diarrhea. Physical examination shows a pulse of 150/min, blood pressure of 80/50 mm Hg, abdominal distention, and absent bowel sounds. Test for occult blood in the stool is positive. Which of the following sets of laboratory data would most likely represent this patient's hematologic disorder?
--------------------------------------------------------------------- RBC Plasma SaO 2 EPO mass volume concentration ---------------------------------------------------------------------- A. Increased Increased Normal Decreased B. Increased Normal Decreased Increased C. Increased Normal Normal Increased D. Normal Decreased Normal Normal EPO = erythropoietin; SaO2 = oxygen saturation |
Option A (increased RBC mass; increased plasma volume; normal SaO2; decreased EPO concentration) is correct. The patient has polycythemia rubra vera (PRV), which is a myeloproliferative disease involving a neoplastic proliferation of trilineage myeloid stem cells in the bone marrow. PRV is an absolute type of polycythemia, meaning there is an increase in the total number of RBCs in the body in mL/kg (RBC mass) as well as an increase in the RBC count (RBCs per L of blood). Unlike other causes of polycythemia, the increase in RBC mass is accompanied by an increase in plasma volume. Because PRV is a stem cell disease, the bone marrow synthesis of RBCs is inappropriate, meaning that the increase in RBC production is not an EPO-mediated response to a hypoxic stimulus. The patient's SaO2 is normal, and the EPO concentration is low. The increase in RBC mass increases the overall O2 content of blood, suppressing EPO release from endothelial cells in peritubular capillaries in the kidneys. The patient's headaches and pruritus are due to histamine released into the blood by increased numbers of peripheral blood basophils and mast cells in skin. The abdominal pain and bloody diarrhea are secondary to thrombosis of the superior mesenteric vein, leading to a hemorrhagic infarction of the small bowel.
|
Option B (increased RBC mass; normal plasma volume; decreased SaO2; increased EPO concentration) is incorrect. This pattern of laboratory findings represents an appropriate type of absolute polycythemia related to a hypoxic stimulus for EPO release. Examples include obstructive and restrictive lung disease, cyanotic congenital heart disease, and living at high altitudes.
Option C (increased RBC mass; normal plasma volume; normal SaO2; increased EPO concentration) is incorrect. This pattern of findings represents an inappropriate type of absolute polycythemia (normal SaO2) related to ectopic or inappropriate secretion of EPO. Examples include renal disease (e.g., cancer, cystic disease, hydronephrosis) and ectopic secretion of EPO from a hepatocellular carcinoma. Option D (normal RBC mass; decreased plasma volume; normal SaO2; normal EPO concentration) is incorrect. This pattern represents a relative type of polycythemia where a loss of plasma hemoconcentrates RBCs in the peripheral blood, increasing the RBC count without affecting RBC mass. Any cause of volume depletion (e.g., excessive sweating, severe diarrhea) leads to this type of polycythemia. |
|
|
A febrile 22-year-old woman complains of crampy right upper quadrant pain. Physical examination shows scleral icterus, right upper quadrant tenderness to palpation, and mild splenomegaly. Laboratory studies show:
Leukocyte count 18,000 Hemoglobin 9.5 g/dL Reticulocyte count, corrected 6% Mean corpuscular volume (MCV) 81 Mean corpuscular hemoglobin concentration (MCHC) 38% Hgb/cell Bilirubin, total //direct 3.6 mg/dL // 0.3 mg/dL Serum alanine aminotransferase (ALT) 20 U/L Many of the red blood cells (RBCs) in the peripheral blood lack central areas of pallor. An ultrasound shows numerous stones in the gallbladder. The patient states that there is a family history of gallbladder disease and anemia at an early age. Which of the following additional studies is most likely to be reported for this patient? A. Abnormal hemoglobin electrophoresis B. Increased RBC osmotic fragility C. Low serum ferritin concentration D. Positive direct Coombs' test E. Positive Heinz body preparation |
Option B (increased RBC osmotic fragility) is correct. The patient has congenital spherocytosis complicated by acute cholecystitis secondary to calcium bilirubinate stones. Congenital spherocytosis is an autosomal dominant disease associated with a spectrin defect in the RBC membrane. Spherocytes are easily recognized because they lack central areas of pallor. Normal RBCs are biconcave disks with a central area of pallor where hemoglobin is less concentrated. Splenic macrophages extravascularly remove spherocytes, which results in anemia and an increase in serum levels of unconjugated bilirubin (end product of hemoglobin metabolism in macrophages). Liver conjugation of excessive unconjugated bilirubin supersaturates the bile, predisposing to the formation of jet-black calcium bilirubinate stones in the gallbladder. The RBC osmotic fragility test will confirm spherocytosis; spherocytes hemolyze earlier than normal RBCs when placed in saline solutions ranging from 0.85% to 0.20% in concentration. Splenectomy is the treatment of choice.
|
Option A (abnormal hemoglobin electrophoresis) is incorrect. The patient does not have a hemoglobinopathy, such as b-thalassemia, where there is an increase in hemoglobins A2 and F, or sickle cell disease, where there is abnormal hemoglobin and sickled RBCs in the peripheral blood.
Option C (low serum ferritin) is incorrect. The patient does not have iron deficiency anemia. Unlike the hemolytic anemias, iron deficiency anemia does not have an elevated, corrected (for the degree of anemia) reticulocyte count. An increased reticulocyte count indicates an appropriate bone marrow response (e.g., increased RBC synthesis) to the anemia, which eliminates bone marrow disease (e.g., aplastic anemia) as the cause of the patient's disorder. Iron deficiency anemia is associated with a low corrected reticulocyte count, because iron is necessary for the synthesis of hemoglobin and proper development of RBCs in the bone marrow. Furthermore, in iron deficiency anemia, the RBCs are microcytic and contain less hemoglobin. This results in a low MCV and a decreased MCHC. In spherocytosis, the MCV is normal and the MCHC is increased, the latter due to increased concentration of hemoglobin in the spherocytes. Option D (positive direct Coombs' test) is incorrect. The patient does not have an autoimmune hemolytic anemia. A direct Coombs' test identifies IgG or complement on the surface of RBCs. The patient has a family history of gallbladder disease and anemia, indicating a genetic rather than acquired basis for RBC hemolysis. Option E (positive Heinz body preparation) is incorrect. The patient does not have glucose-6-phosphate dehydrogenase deficiency, which is a sex-linked recessive disease predominantly seen in males. |
|
|
A 29-year-old Greek medical missionary, who recently returned to the United States after spending 3 months in Africa, is diagnosed with malaria due to Plasmodium vivax. After 4 days of therapy with primaquine, he develops a fever, chills, low back pain, and dark urine. A complete blood cell count shows his hemoglobin is 6 g/dL, leukocyte count is 15,000, and platelet count is 450,000. A corrected reticulocyte count is 12%. The peripheral smear shows polychromasia and numerous red blood cells (RBCs) that are missing parts of their membrane. Urine dipstick is positive for blood. Urine sediment is normal. Which of the following additional laboratory studies would most likely be reported for this patient?
A. Abnormal hemoglobin electrophoresis B. Low mean corpuscular hemoglobin concentration C. Low serum ferritin concentration D. Positive direct Coombs' test E. Positive Heinz body preparation |
Option E (positive Heinz body preparation) is correct. The patient has glucose-6-phosphate dehydrogenase (G6PD) deficiency, a sex-linked recessive disorder. G6PD deficiency leads to decreased synthesis of glutathione (GSH), which is necessary to neutralize peroxide in RBCs. The hemolysis is predominantly intravascular, leading to hemoglobinuria. Infection and therapy with oxidant drugs (e.g., primaquine and dapsone) precipitate hemolysis. In the Mediterranean variant, which is common in individuals of Mediterranean descent, fava beans can precipitate hemolysis. In G6PD deficiency, oxidant damage to RBCs leads to an accumulation of peroxide that cannot be neutralized by GSH. Peroxide damages the RBC membrane (intravascular hemolysis) and denatures hemoglobin, which forms discrete inclusions called Heinz bodies. Splenic macrophages often remove damaged RBC membranes, leaving cells with membrane defects, called "bite cells," circulating in the peripheral blood. The screening test of choice in acute hemolysis is a Heinz body preparation, which requires a special supravital stain to identify the Heinz bodies. Enzyme analysis for G6PD is the confirmatory test and must be performed when active hemolysis has subsided. African Americans have a milder variant of G6PD deficiency.
|
Option A (abnormal hemoglobin electrophoresis) is incorrect. The patient does not have an increase in normal hemoglobin (e.g., hemoglobin A2 or F) or the presence of abnormal hemoglobin (e.g., hemoglobin S). Option B (low mean corpuscular hemoglobin concentration) is incorrect. Patients with G6PD deficiency have normal hemoglobin synthesis, hence a normal MCHC.
Option C (low serum ferritin concentration) is incorrect. The patient does not have iron deficiency anemia, which is associated with an inadequate reticulocyte response to the anemia. Option D (positive direct Coombs' test) is incorrect. Use of primaquine is not associated with an autoimmune hemolytic anemia. |
|
|
An afebrile 72-year-old man has fatigue and substernal chest pain with exertion that is relieved by resting. Physical examination shows a blood pressure of 110/88 mm Hg, pulse of 102/min, pale conjunctiva and palmar creases, and a grade IV systolic ejection murmur heard best in the right second intercostal space. The murmur radiates into the carotid arteries and increases in intensity with expiration. Laboratory studies show:
Hemoglobin 7.0 g/dL Leukocyte count 6,500/mm Mean corpuscular volume (MCV) 77 Platelet count 580,000/mm Partial thromboplastin time (activated, aPTT) normal Prothrombin time (PT) normal Reticulocyte count, corrected 4% Direct Coombs' test negative Urine dipstick positive for blood The peripheral smear shows numerous schistocytes (fragmented red blood cells, RBCs). RBCs are not present in the sediment. Which of the following mechanisms best explains these clinical and laboratory findings? A. Autoimmune destruction of RBCs B. Disseminated intravascular coagulation (DIC) C. Genetic defect in the RBC membrane D. Iron deficiency unrelated to the valvular defect E. Valvular defect leading to intravascular hemolysis |
Option E (valvular defect leading to intravascular hemolysis) is correct. The patient has classic aortic stenosis (systolic ejection murmur with radiation into the carotids) complicated by an intravascular hemolytic anemia due to RBC damage (schistocytes) by the stenotic valve. Chronic loss of hemoglobin in the urine produced iron deficiency (low MCV). Aortic stenosis is the most common cause of intravascular hemolysis associated with schistocytes. Thrombocytosis is secondary to chronic iron deficiency anemia. The classic angina seen in this patient is related to decreased filling of the coronary arteries in diastole due to decreased stroke volume in aortic stenosis plus the moderately severe anemia with concomitant reduced oxygen content of blood.
|
Option A (autoimmune destruction of RBCs) is incorrect. The direct Coombs' test is negative.
Option B(disseminated intravascular coagulation) is incorrect. The aPTT and PT are normal, and the platelet count is elevated. Consumption of coagulation factors and platelets in fibrin clots in the microvasculature prolongs the PTT and PT and lowers the platelet count. Option C (genetic defect in the RBC membrane) is incorrect. Schistocytes are produced by extrinsic damage to the RBC membrane (e.g., stenotic valve, intravascular clots). Option D (iron deficiency unrelated to the valvular defect) is incorrect. The stenotic aortic valve damaged RBCs, leading to hemoglobinuria and loss of iron in the urine. |
|
|
A routine physical examination of an asymptomatic, normotensive 21-year-old African American woman is normal; however, a urinalysis shows red blood cells (RBCs) with no casts. The patient says that she occasionally has had blood in her urine in the past. A urine culture is negative. Laboratory studies show:
Serum blood urea nitrogen (BUN) 10 mg/dL Serum creatinine 1.0 mg/dL Hemoglobin 11.0 g/dL Mean corpuscular volume 78 Reticulocyte count, corrected 2% The peripheral smear shows occasional hypochromatic RBCs. Renal ultrasonography is normal. Which of the following is the next best step in the management of this patient? A. Bone marrow examination B. Cystoscopy C. Renal biopsy D. Sickle cell preparation E. No further investigation is necessary |
Option D (sickle cell preparation) is correct. The patient most likely has sickle cell trait, which causes recurrent microscopic hematuria. Although the percentage of sickle hemoglobin in sickle cell trait is only ~40%, with the remainder representing hemoglobin A, the oxygen tension in the renal medulla is low enough to induce sickling of the RBCs in the peritubular capillaries. This results in microinfarctions in the renal medulla and the potential for renal papillary necrosis and loss of both concentration and dilution of urine.
|
Option A (bone marrow examination) is incorrect. The patient most likely has a mild iron deficiency anemia, which is best diagnosed with a serum ferritin level rather than a bone marrow examination. Furthermore, anemia is not a cause of microhematuria.
Option B (cystoscopy) is incorrect. At this point in the patient's work-up, if the sickle cell screen is negative, a cystoscopy may be necessary to determine the cause of the hematuria. Option C (renal biopsy) is incorrect. If the sickle cell screen is negative, a renal biopsy may be necessary to rule out primary renal disease, particularly IgA glomerulonephritis. Option E (no further investigation is necessary) is incorrect. A recurrent history of microhematuria is always cause for concern and should be evaluated. |
|
|
A normotensive 49-year-old woman complains of fatigue, weight loss, and a dragging sensation in her right upper quadrant. She mentions that she works in a factory where she is exposed to benzene. Physical examination shows generalized, nontender lymphadenopathy and massive hepatosplenomegaly. Laboratory studies show hemoglobin is 6.4 g/dL, leukocyte count is 130,000 and platelet count is 90,000 peripheral smear shows neutrophils at various stages of development, including myeloblasts (1%), mature and immature eosinophils, basophils, and numerous myelocytes, bands, and segmented neutrophils. A bone marrow examination shows hypercellular marrow with a differential count similar to that observed in the peripheral blood. Which of the following additional laboratory findings is most likely in this patient?
A. Auer rods in myeloblasts B. High leukocyte alkaline phosphatase score C. Myeloblasts positive for CD antigen D. Positive Philadelphia chromosome study E. Positive tartrate-resistant acid phosphatase stain |
Option D (positive Philadelphia chromosome study) is correct. The patient has chronic myelogenous leukemia (CML). Like all leukemias, CML is a malignancy arising from stem cells in the bone marrow. Predisposing factors include exposure to radiation or benzene. The classic chromosome abnormality is a t(9;22) translocation of the oncogene (which is responsible for nonreceptor tyrosine kinase activity) from chromosome 9 to chromosome 22 (the Philadelphia chromosome) with fusion at the break cluster region (bcr). The presence of the bcr-c fusion gene is 100% specific for CML, whereas the Philadelphia chromosome has high sensitivity for CML, but it is not 100% specific. CML and acute myelogenous leukemia are the most common leukemias in persons 39\'9660 years of age. CML progresses in ~3 years into a blast crisis, which usually ends in the patient's death. The Philadelphia chromosome is not lost in therapy for CML; t(9;22) is still present.
|
Option A is incorrect. Auer rods are seen only in acute myelogenous leukemias. Auer rods are red, splinter- to rod-shaped inclusions (fused lysosomes) in the cytosol of neoplastic myeloblasts or progranulocytes.
Option B (high leukocyte alkaline phosphatase score) is incorrect. In CML, the leukocyte alkaline phosphatase (LAP) score is usually low. LAP is normally present in nonneoplastic neutrophils from the myelocyte stage to segmented neutrophils. Because the neutrophils of CML are neoplastic, a stain for LAP is usually negative; hence the stain intensity in neutrophils is usually very low or zero. The LAP score is increased in patients whose neutrophil elevations are associated with inflammation. Option C (myeloblasts positive for CD 10 antigen) is incorrect. The CD 10 antigen refers to the common acute lymphoblastic leukemia antigen (CALLA), which is positive in most cases of acute lymphoblastic leukemia. Option E (positive tartrate-resistant acid phosphatase stain) is incorrect. This stain identifies the neoplastic B cells of hairy cell leukemia. |
|
|
A 22-year-old woman complains of fatigue and frequent nose bleeds. Physical examination shows generalized petechiae and ecchymoses, generalized lymphadenopathy, and hepatosplenomegaly. The peripheral smear shows hypergranular blast cells containing numerous Auer rods. Laboratory studies show:
Hemoglobin 7.0 Leukocyte count 50,000 Platelet count 10,000 Prothrombin time 30 sec Partial thromboplastin time (activated, aPTT) 65 sec D-dimer assay positive Treatment with retinoic acid is initiated. Which of the following is the rationale for treating the patient's hematologic disorder with this agent? A. Destroys the blast cells B. Enhances cellular immunity C. Increases maturation of the blast cells D. Prevents infection associated with bone marrow suppression E. Prevents intravascular coagulation |
Option C (increases maturation of the blast cells) is correct. The patient has acute promyelocytic (progranulocytic) leukemia (FAB classification M3). Unique characteristics associated with this form of leukemia include a high incidence of disseminated intravascular coagulation, or DIC (which is present in this patient), a t(15;17) translocation, abnormal retinoic acid metabolism, and an excellent response to treatment with retinoic acid, which matures the promyelocytes.
|
Option A (destroys the blast cells),Option B(enhances cellular immunity),
Option D (prevents infection related to bone marrow suppression), and Option E (prevents intravascular coagulation) are incorrect. Substances released from the granules of the promyelocytes activate the coagulation cascade, leading to intravascular coagulation). D-dimers are fibrin monomers found in a fibrin clot that have been cross-linked by factor XIII (fibrin-stabilizing factor). Their presence indicates that intravascular coagulation has occurred. Refer to the discussion for Option C. |
|
|
A febrile 68-year-old woman with a 40-year history of smoking cigarettes complains of fatigue and weight loss. Physical examination shows generalized nontender lymphadenopathy, hepatosplenomegaly, and petechiae and ecchymoses scattered over the entire body. Laboratory studies show\:
Hemoglobin 8.7 g/dL Leukocyte count 95,000 Platelet count 60,000 Total serum protein concentration 4.5 g/dL The peripheral smear contains predominantly mature-appearing lymphocytes, many of which have a smudged appearance. A blood culture is positive for Streptococcus pneumoniae. A serum protein electrophoresis shows a flat gamma-globulin peak. The pathogenesis for this patient's hematologic condition is most closely associated with which of the following? A. B-cell malignancy arising from the bone marrow B. Hypogammaglobulinemia related to sepsis C. Lymphoid leukemoid reaction secondary to sepsis D. Metastatic lung cancer associated with smoking cigarettes E. T-cell malignancy arising from lymph nodes |
Option A (B-cell malignancy arising from the bone marrow) is correct. The patient has chronic lymphocytic leukemia (CLL). CLL is the most common leukemia; in patients 60 years of age, it is the most common leukemia and the most common cause of generalized lymphadenopathy. Like all leukemias, it arises from stem cells in the bone marrow and can metastasize throughout the body, typically to the lymph nodes, liver, and spleen. Because the B cells are neoplastic, they cannot be antigenically stimulated to produce plasma cells; hence the high incidence of hypogammaglobulinemia and infection in CLL patients.
|
Option B (hypogammaglobulinemia related to sepsis) is incorrect. In this patient, hypogammaglobulinemia did not produce this patient's hematologic condition, however, it is most likely responsible for her sepsis.
Option C (lymphoid leukemoid reaction secondary to sepsis) is incorrect. The patient does not have an exaggerated, benign proliferation of lymphocytes (leukemoid reaction) in response to an infection. In patients with sepsis, expected findings do not include hepatosplenomegaly, generalized nontender lymphadenopathy, lymphocytosis, and hypogammaglobulinemia. These patients have tender lymphadenopathy and neutrophilic leukocytosis. Option D (metastatic lung cancer associated with smoking cigarettes) is incorrect. Although smoking has been implicated in causing leukemia, the clinical and laboratory findings in this patient are totally inconsistent with metastatic lung cancer. Option E (T-cell malignancy arising from lymph nodes) is incorrect. T-cell leukemias are uncommon, usually metastasize to skin, have lytic lesions in bone, and are not associated with hypogammaglobulinemia. |
|
|
A febrile 19-year-old African-American man with sickle cell disease develops pain in the right thigh. A radionuclide bone scan shows a lytic lesion with poorly defined borders in the metaphyseal area of the proximal right femur. The pathogenesis of the femoral bone lesion is most likely associated with which of the following conditions?
A. Aseptic necrosis related to ischemia B. Metastatic cancer from an undetermined site C. Osteomyelitis secondary to Salmonella paratyphi septicemia D. Primary malignancy of bone |
Option C (osteomyelitis secondary to Salmonella paratyphi septicemia) is correct. The most common pathogen causing osteomyelitis in patients with sickle cell disease is Salmonella paratyphi (75% of cases). Staphylococcus aureus septicemia is the most common cause of osteomyelitis in children; however, in patients with sickle cell disease, the loss of splenic function due to repeated infarctions predisposes them to sepsis caused by Salmonella species and not by other pathogens. The metaphysis is the most common location for osteomyelitis associated with sepsis, because it is the most vascular part of bone. A radionuclide bone scan has much greater sensitivity than a routine radiograph in detecting osteomyelitis in its earliest stages. A bone biopsy is the confirming test for osteomyelitis.
|
Option A (aseptic necrosis related to ischemia) is incorrect. Aseptic necrosis most commonly occurs in the femoral head rather than the metaphysis of bone. Furthermore, the bone in aseptic necrosis shows increased density due to reactive bone formation after the ischemic event. Aseptic necrosis of the femoral head is a common complication of sickle cell disease.
Option B (metastatic cancer from an undetermined site) is incorrect. The femoral head is a more common location for metastasis than the metaphyseal area. Furthermore, the clinical presentation of a febrile patient with sickle cell disease and a lytic lesion in bone is more likely to be diagnosed with osteomyelitis than with primary or metastatic cancer. Option D (primary malignancy of bone) is incorrect. The most common bone cancer found in the metaphysis of the femur is an osteogenic sarcoma. As the name implies, it is a bone-producing sarcoma; hence increased density of bone, rather than bone lysis, is expected. |
|
|
A 69-year-old African-American woman complains of fatigue and pain in her lower back and ribs. She states that she has been having problems with voiding urine for the past few days. Physical examination shows percussion tenderness over the lower vertebrae and rib cage. Renal tubular casts are present in the urine sediment. A radiograph of the chest shows generalized osteopenia in the ribs and thoracic vertebral column and multiple lytic lesions in the ribs. Serum protein electrophoresis (SPE) shows an abnormality in the g-globulin region. Laboratory studies show:
Rouleaux Hemoglobin 7.0 g/dL Leukocyte count 6500/mm Platelet count 175,000/mm Serum blood urea nitrogen (BUN) 60 mg/dL Serum creatinine 6 mg/dL Urine dipstick reaction proteinuria (1+); precipitation reaction, sulfosalicylic acid (SSA) 4+ The mechanism responsible for this patient's condition is most closely associated with which of the following? A. Immunoglobulin M-producing lymphoproliferative disorder B. Malignant plasma cell disorder C. Malignant T-cell disorder D. Metastatic disease of undetermined origin E. Renal failure of undetermined origin |
Option B (malignant plasma cell disorder) is correct. The patient has multiple myeloma (MM) complicated by renal failure due to precipitation of Bence Jones (BJ) protein (light chains) in the renal tubules. MM is the most common primary malignancy of bone, and is more common in African Americans than in whites. Lytic bone lesions result from secretion of osteoclast-activating factor (interleukin-1) by malignant plasma cells. In >80% of cases, SPE shows a monoclonal spike in the gamma-globulin region. A single clone of malignant plasma cells produces the predominant immunoglobulin (Ig), usually IgG; hence the sharp spike in the gamma-globulin region of SPE. The immunoglobulin's corresponding light chain (kappa or lambda) BJ protein is spilled into the urine. Because urine dipsticks for protein detect only albumin (whereas the SSA detects both albumin and globulins), a disparity between the urine protein dipstick reaction (trace or +1) and SSA (+3 or +4) excludes albumin as the cause of proteinuria and is highly suggestive of BJ protein in the urine. A bone marrow aspirate showing sheets of malignant plasma cells is mandatory to confirm the diagnosis. Serum immunoelectrophoresis identifies the Ig involved. Renal failure is a common cause of death in MM. Note the increase in serum BUN and creatinine levels and renal tubular casts in this patient.
|
Option A (immunoglobulin M-producing lymphoproliferative disorder) is incorrect. An IgM-producing lymphoproliferative disorder is called Waldenstrom's macroglobulinemia. Unlike MM, this malignant disorder is not associated with lytic lesions and acts more like a malignant lymphoma in that it metastasizes to lymph nodes. Option C (malignant T-cell disorder) and Option D (metastatic disease of undetermined origin) are incorrect. Unlike MM, these disorders are not associated with monoclonal spikes or Bence Jones protein. Option E (renal failure of undetermined origin) is incorrect. This patient's renal failure is a complication of MM, rather than a cause of her skeletal and hematologic problems. |
|
|
A 72-year-old man with a 20-year history of osteoarthritis of the hips and knees develops urinary retention secondary to benign prostatic hyperplasia. A transurethral resection of the prostate is performed to relieve the obstruction. Shortly after the procedure, the patient begins bleeding profusely from the penis. Coagulation studies show the following:
Partial thromboplastin time (activated, aPPT) 38 seconds Prothrombin time (PT) 14 seconds Bleeding time (BT) >15 minutes Platelet count 350,000 mm3 D-dimer assay negative Which of the following mechanisms is most likely responsible for this patient's bleeding disorder? A. Circulating anticoagulant B. Coagulation factor deficiency C. Platelet function disorder D. Secondary fibrinolytic disorder |
Option C (platelet function disorder) is correct. The patient has a qualitative platelet disorder most likely associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs) for his chronic osteoarthritis. NSAIDs block platelet cyclooxygenase, which prevents the synthesis of thromboxane A2 (TXA2). Normally, TXA 2is a potent platelet aggregator and vasoconstrictor of small vessels. It is primarily responsible for producing a temporary hemostatic plug composed of platelets that stop bleeding in injured small vessels. Hence, blocking the synthesis of TXA2 in this patient causes severe bleeding from small vessels that lack platelet plugs. The best test of platelet function is indicated by BT, which evaluates small vessel and platelet function up to the formation of the platelet plug. The BT is prolonged in this patient. The aPTT evaluates the intrinsic coagulation system down to the formation of a fibrin clot, which includes the following factors (in sequence of activation)\: XII, XI, IX, VIII, X, V, II (prothrombin), and I (fibrinogen). The PT evaluates the extrinsic coagulation system down to the formation of a fibrin clot, which includes the following factors (in sequence of activation)\: VII, X, V, II, and I. The platelet count is a quantitative measurement of platelets; however, it does not evaluate platelet function. The most appropriate treatment for this patient is infusion with a few units of platelets, which are functionally capable of forming platelet plugs and participating in the formation of fibrin clots.
|
Option A (circulating anticoagulant) is incorrect. Circulating anticoagulants are antibodies that inhibit specific coagulation factors (e.g., antibodies against factor VIII), thus simulating a coagulation factor deficiency. Normal PTT and PT exclude circulating anticoagulants as a cause of the bleeding.
Option B (coagulation factor deficiency) is incorrect. The PTT and PT in this patient are both normal. Option D (secondary fibrinolytic disorder) is incorrect. The D-dimer assay is negative, and the PT and PTT are both normal in this patient. Secondary fibrinolysis refers to activation of the fibrinolytic system (activation of plasminogen produces plasmin) as a compensatory mechanism to destroy fibrin clots in intravascular coagulation. Plasmin destroys fibrin, fibrinogen, and many of the coagulation factors; therefore, it prolongs the PT and PTT. D-dimers are fibrin monomers in a fibrin clot that have been cross-linked by factor XIII (fibrin-stabilizing factor). Their presence indicates that intravascular coagulation has occurred. |
|
|
A febrile 35-year-old woman complains of a headache, fatigue, and decreased urine output. Physical examination shows bilateral retinal hemorrhages and generalized petechiae and ecchymoses. The peripheral smear shows numerous fragmented red blood cells (RBCs). Laboratory studies show:
Hemoglobin 7.0 g/dL Leukocyte count 9500/mm3\f1 Platelet count 30,000/mm Reticulocyte count, corrected 12% Blood urea nitrogen (BUN), serum 50 mg/dL Creatinine, serum 5 mg/dL Partial thromboplastin time (activated, aPTT) 35 seconds Prothrombin time (PT) 13 seconds Bleeding time (BT) >15 minutes Platelet count 350,000 mm D-dimer assay negative The mechanism most likely responsible for this patient's hematologic disorder is most closely associated with A. circulating anticoagulant B. consumption of coagulation factors C. consumption of platelets D. qualitative platelet disorder E. secondary fibrinolytic disorder |
Option C (consumption of platelets) is correct. The patient has thrombotic thrombocytopenic purpura (TTP), in which a toxin circulating in plasma damages small vessel endothelial cells, resulting in formation of platelet thrombi that occlude the lumen of these vessels throughout the body (e.g., brain, kidneys, heart). Platelets are consumed during this process, which lowers the platelet count and prolongs the BT. The BT primarily evaluates platelet function. Platelet thrombi damage red blood cells, resulting in fragmented cells, called schistocytes, and in an intravascular hemolytic anemia. Renal failure is common, as has occurred in this patient who has a history of oliguria and elevated serum BUN and creatinine levels. Plasmapheresis is the treatment of choice for TTP.
|
Option A (circulating anticoagulant) is incorrect. Circulating anticoagulants are antibodies that inhibit specific coagulation factors (e.g., antibodies against factor VIII), hence simulating a coagulation factor deficiency. Normal PTT and PT exclude circulating anticoagulants from the differential diagnosis.
Option B (consumption of coagulation factors) is incorrect. The thrombi that are formed in the vessel lumen are composed of platelets, not fibrin clots. In other words, TTP is not a variant of disseminated intravascular coagulation (DIC). Option D (qualitative platelet disorder) is incorrect. The problem is consumption of platelets in platelet thrombi, and not a disorder involving platelet adhesion or aggregation. Option E (secondary fibrinolytic disorder) is incorrect. The D-dimer assay is negative, and the PT and PTT are both normal. Secondary fibrinolysis refers to activation of the fibrinolytic system (plasminogen is converted into plasmin) as a compensatory mechanism to destroy fibrin clots in intravascular coagulation. Plasmin destroys fibrin, fibrinogen, and many of the coagulation factors; therefore, it prolongs the PT and PTT. D-dimers are fibrin monomers in a fibrin clot that have been cross-linked by factor XIII (fibrin-stabilizing factor). Their presence indicates that intravascular coagulation has occurred. |
|
|
A 72-year-old man complains of sudden onset of left flank pain and dizziness when he stands up quickly. When he is lying down, his blood pressure is 100/80 mm Hg, and his pulse is 110/min. When he is moved to a sitting position, his blood pressure is 80/60 mm Hg, and his pulse is 160/min. A pulsatile mass is palpated in the abdomen. The pathogenesis of the patient's flank pain and hypotension is most closely attributed to structural weakness of the aorta due to
A. genetic defect in collagen B. genetic defect in fibrillin C. immunocomplex-mediated disease D. normal changes associated with aging E. severe atherosclerosis |
Option E (severe atherosclerosis) is correct. The patient has the classic triad of a ruptured abdominal aortic aneurysm: sudden onset of left flank pain, hypotension, and a pulsatile abdominal mass. Atherosclerotic damage of the abdominal aorta weakens the vessel wall, leading to outpouching of the aorta and the potential for rupture as the expansion increases wall stress.
|
Option A (genetic defect in collagen) is incorrect. Ehlers-Danlos syndrome has multiple inheritance patterns and is characterized by defects in synthesis and structure of collagen. Clinical abnormalities include hyperextensibility, vascular instability, and a predisposition for dissecting aortic aneurysms, the most common cause of death in these patients. Dissecting aortic aneurysms usually are associated with a sudden onset of chest pain radiating into the back. Those extending distally are less likely to rupture than those extending proximally. This patient does not have Ehlers-Danlos syndrome.
Option B (genetic defect in fibrillin) is incorrect. Marfan's syndrome has an autosomal dominant inheritance, and is associated with a defect on chromosome 15 involving the synthesis of a fibrillin component in elastic tissue. Eunuchoid proportions, lens dislocation, arachnodactyly, mitral valve prolapse, and a propensity for dissecting aortic aneurysms are common in these patients. Elastic tissue fragmentation and cystic medial necrosis occur in the wall of the aorta, leading to structural weakness of the vessel. An intimal tear allows blood to dissect through the weak areas. As discussed under Option A, the clinical findings in this patient do not support the diagnosis of a dissecting aortic aneurysm or of Marfan's syndrome. Option C (immunocomplex-mediated disease) is incorrect. Immunocomplex types of vasculitis are more often associated with small vessel vasculitis involving venules, arterioles, or with capillaries and vasculitis involving muscular arteries (e.g., coronary arteries) rather than elastic arteries such as the aorta. Option D (normal changes associated with aging) is incorrect. The aorta is not structurally weakened in older age; it becomes less distensible, but is not prone to rupture. |
|
|
A 28-year-old man has a family history of sudden cardiac death at a young age (<45 years of age). Physical examination shows a systolic murmur that decreases in intensity when the patient is lying down and increases in intensity when he is sitting up. An echocardiogram shows abnormal movement of the anterior mitral valve leaflet against an asymmetrically thickened interventricular septum. The mechanism for sudden cardiac death in this patient's family is most closely attributed to which of the following conditions?
A. Acute myocardial infarction (MI) B. Congenital bicuspid aortic valve C. Conduction system defects D. Dissecting aortic aneurysm E. Mitral valve prolapse |
Option C (conduction system defects) is correct. The patient has hypertrophic cardiomyopathy (idiopathic hypertrophic subaortic stenosis), which is the most common cause of sudden cardiac death in young people. In some cases, there is an autosomal dominant inheritance pattern. Because of asymmetric hypertrophy of the interventricular septum, the anterior leaflet of the mitral valve is closer to the septum than normal. This narrows the outlet channel for blood flow through the aorta. When systole occurs, the anterior leaflet of the mitral valve is drawn against the interventricular septum, thus obstructing blood flow below the level of the aortic valve. This produces a systolic ejection murmur that is easily confused with aortic stenosis. Aberrant myofibers in the hypertrophied septum and conduction system abnormalities also occur; the latter are responsible for fatal ventricular arrhythmia and sudden death. The murmur intensity decreases (less obstruction) whenever left ventricular volume (preload) is increased. Hence, increased venous return to the right-sided heart (lying down) or drugs that decrease cardiac contractility and heart rate (e.g., b -blockers, calcium channel blockers) decrease murmur intensity. Sitting up reduces venous return to the heart (decreases preload) and intensifies the murmur (greater obstruction). Drugs that have an inotropic effect on the heart (e.g., digitalis) or the patient holding his breath against a closed glottis (Valsalva maneuver) have a similar effect.
|
Option A (acute myocardial infarction) is incorrect. Hypertrophic cardiomyopathy is not associated with coronary artery disease. Furthermore, conduction defects do not predispose patients to acute MIs.
Option B (congenital bicuspid aortic valve) is incorrect. This congenital anomaly is the most common cause of aortic stenosis in young to middle-aged patients. It predisposes patients to dystrophic calcification of the valve cusps and subsequent reduction in valve orifice area for blood flow out of the aorta. In aortic stenosis, increasing preload increases the intensity of the murmur (increases obstruction), and reducing preload decreases the intensity (lessens obstruction). Option D (dissecting aortic aneurysm) is incorrect. Dissections do not cause sudden death and are not associated with systolic murmurs. Proximal dissections stretch the aortic valve ring, causing aortic regurgitation, which is a diastolic murmur heard after the second heart sound. Furthermore, the orifice to the left subclavian artery is often occluded, leading to a diminished pulse. Option E (mitral valve prolapse) is incorrect. Mitral valve prolapse (MVP) is associated with a midsystolic ejection click followed by a murmur. Except for MVP associated with Marfan syndrome, MVP is not associated with sudden cardiac death. |
|
|
A 2-day-old neonate with respiratory distress syndrome (RDS) has moderately severe hypoxemia. On auscultation, dry inspiratory crackles are heard in the lungs and a continuous harsh murmur is heard over the entire precordium. Which of the following sets of oxygen saturation (SaO2) values in the cardiac chambers and vessels is most likely present in this patient?
Normal SaO2% Right atrium (RA) 75 Right ventricle (RV) 75 Pulmonary artery (PA) 75 Pulmonary vein (PV) 95 Left ventricle (LV) 95 Aorta (A) 95 ------------------------------------------------ RA RV PA PV LV A ------------------------------------------------ A. 75 80 80 95 95 95 B. 80 80 80 95 95 95 C. 75 75 80 95 95 95 D. 75 75 75 95 80 80 |
Option C (RA 75, RV 75, PA 80, PV 95, LV 95, A 95) is correct. The patient has the classic machinery murmur (continuous murmur) of a patent ductus arteriosus (PDA). Because the neonate has hypoxemia (low arterial PO2) secondary to RDS, the ductus has no stimulus to close. Congenital heart diseases often have shunts between chambers or vessels. The pressure in the chamber or vessel determines the direction of blood flow. When oxygenated blood (SaO2 95%) is shunted into a chamber or vessel with venous blood (SaO2 75%), there is a step-up of SaO2 (~80%) in the venous blood; this is known as a left-to-right shunt. Similarly, when venous blood is shunted into a chamber or vessel with oxygenated blood, there is a step-down of the SaO2 (~80%) leading to clinical evidence of cyanosis; this is known as a right-to-left shunt. In PDA, blood initially flows from the aorta (where pressure is high), through the patent ductus arteriosus, and into pulmonary artery (where pressure is low), a left-to-right shunt; hence there is a step-up of the SaO2 in the pulmonary artery.
|
Option A (RA 75, RV 80, PA 80, PV 95, LV 95, A 95) is incorrect. A step-up of SaO2 in the right ventricle and pulmonary artery is consistent with a ventricular septal defect (VSD, or left-to-right shunt), which is the most common congenital heart disease. If a VSD is left uncorrected, the volume overload in the right side of the heart due to the left-to-right shunt leads to pulmonary hypertension. This is followed by right ventricular hypertrophy and eventual reversal of the shunt (right-to-left), producing clinical evidence of cyanosis, or Eisenmenger's syndrome.
Option B (RA 80, RV 80, PA 80, PV 95, LV 95, A 95) is incorrect. A step-up of the SaO2 in the right atrium, right ventricle, and pulmonary artery is consistent with an atrial septal defect (ASD, or left-to-right shunt), which is most often the result of a patent foramen ovale. Eisenmenger's syndrome also may occur in an ASD (refer to the discussion for Option A). Option D (RA 75, RV 75, PA 75, PV 95, LV 80, A 80) is incorrect. A step-down of the SaO2 in the left ventricle and aorta is consistent with tetralogy of Fallot (right-to-left shunt), which is the most common type of cyanotic congenital heart disease. It consists of an overriding aorta (least common defect), VSD, infravalvular pulmonary stenosis, and right ventricular hypertrophy. The degree of pulmonic stenosis determines the severity of the right-to-left shunt. If the stenosis is not severe, then most of the venous blood enters the pulmonary artery and is oxygenated; hence the patient is often acyanotic. However, when the stenosis is severe, most of the venous blood is shunted through the VSD into the left ventricle (right-to-left shunt), leading to cyanosis. Coexisting PDA and ASD are cardioprotective in a tetralogy. A PDA allows some of the unoxygenated blood in the aorta to reenter the pulmonary artery for oxygenation in the lungs. An ASD allows oxygenated blood from the left atrium to shunt into the right atrium and step-up the SaO2 in the right side of the heart. |
|
|
A febrile 12-year-old boy complains of joint pains and abdominal pain with associated bloody stools, which began 1 week after an upper respiratory infection. Physical examination shows a palpable purpuric h limited to the buttocks and lower extremities. Laboratory studies show occult blood in the stool, red blood cells (RBCs) and RBC casts in the urine, mild proteinuria, and a normal complete blood cell count. Which of the following mechanisms is most closely associated with this patient's condition?
A. Genetic vascular disorder B. Infectious type of vasculitis C. Immunocomplex vasculitis D. Previous group A streptococcal infection E. Type II hypersensitivity vasculitis |
Option C (immunocomplex vasculitis) is correct. The patient has Henoch-Schonlein purpura (HSP), an immunocomplex disease (type III hypersensitivity) involving small vessels primarily in the skin (palpable purpura), gastrointestinal (GI) tract, and glomeruli of the kidneys. HSP is the most common type of vasculitis in children. Increased circulating levels of polymeric IgA and immunocomplexes with IgA and C3 are present in the patient. The immunocomplexes deposit in small vessels and activate the alternative complement system, which produces complement components that are chemotactic for neutrophils. Hence, neutrophils are primarily responsible for tissue damage in this and all other immunocomplex diseases. The glomerulonephritis associated with HSP is similar to IgA glomerulonephritis (Berger's disease) in that IgA immunocomplexes deposit in the mesangium, resulting in hematuria, RBC casts, and proteinuria.
|
Option A (genetic vascular disorder) is incorrect. The most common genetic vascular disorder is Osler-Weber-Rendu disease (hereditary hemorrhagic telangiectasia). It is an autosomal dominant disease associated with dilated vessels (telangiectasia) on the skin, in the mouth, and throughout the mucosa of the GI tract. When found in the GI tract, chronic iron deficiency anemia occurs.
Option B (infectious type of vasculitis) is incorrect. The multisystem involvement and peculiar distribution of the vasculitis on the buttocks and lower extremities favor a diagnosis of HSP. Option D (previous group A streptococcal infection) is incorrect. The patient does not have acute rheumatic fever (ARF) or poststreptococcal glomerulonephritis. In both conditions, neither bloody diarrhea nor vasculitis is part of the clinical presentation. Option E (type II hypersensitivity vasculitis) is incorrect. Most small vessel types of vasculitis are immunocomplex, type III hypersensitivity reactions. Refer to the discussion for Option C. |
|
|
A 45-year old woman develops a fever and dyspnea approximately 24-hours postcholecystectomy for acute gangrenous cholecystitis. Physical examination shows decreased percussion, increased tactile fremitus, and decreased breath sounds in the right lower lobe. The diaphragm is elevated, and there is inspiratory lag on the ipsilateral side. Which of the following is the most likely diagnosis?
A. Atelectasis B. Lobar pneumonia C. Lung abscess D. Pulmonary infarction E. Spontaneous pneumothorax |
Option A (atelectasis) is correct. The most common cause of fever occurring within the first 24-36 hours after surgery is atelectasis, which refers to either a collapse of previously inflated lungs or incomplete expansion of the lungs on inspiration. Postoperatively, mucus plugs develop in the terminal bronchioles, allowing resorption of air out of the distal respiratory unit through the pores of Kohn. The physical findings of atelectasis are those of a lung consolidation, mainly decreased percussion and increased tactile fremitus (vibration of the chest wall when the patient speaks). The loss of lung mass results in ipsilateral elevation of the diaphragm and inspiratory lag, because the lung is not expanding properly on inspiration.
|
Option B (lobar pneumonia) is incorrect. Postoperative pneumonia usually develops 3-10 days after surgery.
Option C (lung abscess) is incorrect. Aspiration of oropharyngeal contents, the most common cause of a lung abscess, does not occur within such a short time (24 h) after surgery. The patient usually has a cough productive of foul-smelling sputum due to the presence of aerobes and anaerobes in the abscess. Option D (pulmonary infarction) is incorrect. Pulmonary embolization usually occurs 5-7 days after surgery. In this patient, there is no history of pleuritic chest pain, which is invariably present in a pulmonary infarction. Most pulmonary emboli originate in the femoral vein. Option E (spontaneous pneumothorax) is incorrect. The physical findings are those of a lung consolidation. In a spontaneous pneumothorax, a portion of the lung collapses, which produces hyperresonance to percussion. Similar to atelectasis, however, a spontaneous pneumothorax shows inspiratory lag, decreased breath sounds, and elevated hemidiaphragm. |
|
|
A 58-year-old man with a 35-year history of cigarette smoking complains of weight loss and cough. Physical examination shows absence of sweating on the left forehead and face and ipsilateral lid lag and constriction of the pupil. On auscultation, sibilant rhonchi that clear with coughing are heard in all lung fields. The anteroposterior diameter of the chest is increased. Which of the following mechanisms best explains the clinical findings in this patient?
A. Destruction of the brachial plexus by a primary lung cancer B. Destruction of the cervical sympathetic plexus by a primary lung cancer C. Extension of a primary lung cancer into the anterior mediastinum D. Uncal herniation secondary to metastatic disease originating in the lung |
Option B (destruction of the cervical sympathetic plexus by a primary lung cancer) is correct. The patient most likely has a primary squamous cell carcinoma in the left superior pulmonary sulcus. The tumor has invaded and destroyed the cervical sympathetic plexus, producing Horner's syndrome. Horner's syndrome is characterized by ipsilateral lid lag (ptosis), pupil miosis (constriction), and absence of sweating (anhidrosis) on the forehead and face.
|
Option A (destruction of the brachial plexus by a primary lung cancer) is incorrect. Tumor invasion of the brachial plexus by superior sulcus tumors usually produces ulnar nerve irritation.
Option C (extension of a primary lung cancer into the anterior mediastinum) is incorrect. The anterior mediastinum contains the thymus and lymphatic tissue. Tumor invasion of the posterior mediastinum, which contains the sympathetic ganglia and nerves, is responsible for producing Horner's syndrome. Option D (uncal herniation secondary to metastatic disease originating in the lung) is incorrect. Uncal herniation refers to herniation of the medial portion of the temporal lobe through the tentorium cerebelli, leading to compression of the midbrain. It is a complication of cerebral edema from any cause, including metastatic disease to the brain. Uncal herniation commonly is associated with compression of the oculomotor nerve (CN III), which produces lid lag, mydriasis (pupil dilatation), and ophthalmoplegia (eyes deviated downward and outward). |
|
|
A 69-year-old man with a 40-year history of cigarette smoking complains of weight loss, a dragging sensation in his right upper quadrant, and crampy left lower quadrant abdominal pain. He states that he has had alternating bouts of constipation and diarrhea over the past 6 months and has noticed blood coating and mixed with his stools. Physical examination shows an enlarged, nodular liver, external hemorrhoids, and occult blood in the stool. Laboratory studies show:
Hemoglobin 9.0 g/dL Leukocyte count 6500 Platelet count 500,000 Mean corpuscular volume (MCV) 75 Ferritin level, serum 3.0 ng/mL Which of the following disorders best explains the positive stool guaiac in this patient? A. External hemorrhoids B. Hepatocellular carcinoma with metastasis to the colon C. Peptic ulcer disease (PUD) D. Primary colon cancer E. Primary lung cancer with metastasis to the colon |
Option D (primary colon cancer) is correct. The patient has primary colon cancer complicated by iron deficiency anemia (microcytic anemia and low serum ferritin) and metastasis to the liver (nodular, enlarged liver). Key points in the patient's history include weight loss, change in consistency of stools, and blood mixed with stools. Thrombocytosis is common in metastatic cancer and in chronic iron deficiency anemia. The most common cause of iron deficiency in a patient over 50 years of age is colon cancer.
|
Option A (external hemorrhoids) is incorrect. Blood coating stools in the presence of external hemorrhoids always requires further investigation, especially in a patient over 50 years of age. As a rule, external hemorrhoids thrombose; internal hemorrhoids bleed.
Option B (hepatocellular carcinoma with metastasis to the colon) is incorrect. Hepatocellular carcinoma (HCC) usually arises from postnecrotic cirrhosis secondary to hepatitis B or hepatitis C. This patient has no history of hepatitis; furthermore, HCC usually metastasizes to the lungs and not to the colon. Option C (peptic ulcer disease) is incorrect. PUD is the most common cause of iron deficiency anemia in men under 50 years of age. Black tarry stools (melena) are more likely to occur than blood coating and mixing with stools. Melena is due to acid conversion of hemoglobin into hematin, a black pigment. PUD alone does not explain the nodular liver in this patient; hence it is not a tenable diagnosis. Option E (primary lung cancer with metastasis to the colon) is incorrect. Metastatic disease to the bowel is more likely to cause signs of obstruction than of bleeding. Although smoking is a risk factor for colon cancer, and primary lung cancer is the most common cause of metastasis to the liver, the overall clinical and laboratory findings do not support lung cancer as the primary diagnosis in this patient. |
|
|
An afebrile 50-year-old man with a 30-year history of cigarette smoking complains of flushing in his face, watery diarrhea, and weight loss over the past 6 months. Physical examination shows an enlarged, nodular liver and a grade 3 pansystolic murmur heard best along the left parasternal border. S3 and S4 heart sounds are present, and the heart sounds and murmur increase in intensity on inspiration. The patient's neck veins are distended, and the jugular venous pulse shows a giant c-v wave. Which of the following laboratory studies would be most useful in confirming the diagnosis of this patient's clinical disorder?
A. Blood cultures B. Complete blood cell count C. Liver function tests D. Serum electrolytes E. Urine test for 5-hydroxyindoleacetic acid (5-HIAA) |
Option E (urine test for 5-hydroxyindoleacetic acid) is correct. The patient has the clinical findings of a carcinoid syndrome complicated by tricuspid insufficiency. To develop a carcinoid syndrome, a carcinoid tumor secreting serotonin must metastasize to the liver. In the liver, the tumor nodules secrete serotonin directly into hepatic vein tributaries and gain access to the systemic circulation, where the tumor produces flushing (due to vasodilatation), diarrhea, and right-sided valvular lesions. All carcinoid tumors are malignant; however, their ability to metastasize to the liver occurs when they are >2 cm. This explains why carcinoid tumors of the appendix (usually <2 cm) rarely metastasize to the liver, whereas those in the terminal ileum have the potential to metastasize; hence their notoriety as the most common primary site for tumors associated with carcinoid syndrome. The classic laboratory finding in carcinoid syndrome is an increase in urine levels of 5-HIAA, which is the liver-derived metabolic end product of serotonin.
Serotonin elicits a fibrogenic response in the valvular tissue that may result in tricuspid insufficiency or pulmonic stenosis. This patient has tricuspid insufficiency with the classic pansystolic murmur, giant c-v wave (due to blood entering the right atrium during systole), and S3 and S4 heart sounds (due to volume overload in the right ventricle). Because inspiration increases negative intrathoracic pressures, more blood enters the right side of the heart than is present in the left side. Hence, all abnormal heart sounds and murmurs increase in intensity on inspiration in lesions on the right-side, as opposed to left-sided lesions, which increase in intensity on expiration. Smoking has no relationship with carcinoid tumors or carcinoid syndrome. Bronchial carcinoids rarely produce carcinoid syndrome, and are not associated with smoking. Furthermore, it is not necessary for bronchial carcinoids to metastasize to the liver to produce the syndrome, because serotonin has direct access to the systemic circulation. |
Option A (blood cultures) is incorrect. The patient does not have infective endocarditis (IE) of the tricuspid valve; IE does not explain the nodular liver, flushing, and diarrhea. IE involving the tricuspid valve is most often associated with intravenous drug abuse.
Option B (complete blood cell count) is incorrect. There are no distinct hematologic features that characterize carcinoid syndrome. Option C (liver function tests) is incorrect. Liver function tests are usually normal in patients with liver metastasis due to the focal, rather than diffuse, involvement of the liver parenchyma. Option D (serum electrolytes) is incorrect. Serum electrolytes have no distinct diagnostic profile for carcinoid syndrome. |
|
|
A 58-year-old woman complains of epigastric pain, weight loss, vomiting of coffee ground-like material, and dark black, sticky stools. Physical examination shows epigastric pain on deep palpation and enlarged, nontender left supraclavicular lymph nodes. Both ovaries are enlarged and firm on bimanual pelvic examination. Test for occult blood in the stool is positive. Which of the following clinical scenarios best explains the signs and symptoms in this patient?
A. Primary malignant lymphoma of the stomach with ovarian metastasis B. Primary ovarian cancer with metastasis to the left supraclavicular lymph nodes C. Primary ovarian cancer with metastasis to the stomach D. Primary pancreatic cancer with ovarian metastasis E. Primary stomach cancer with ovarian metastasis |
Option E (primary stomach cancer with ovarian metastasis) is correct. The patient has a primary stomach cancer that has metastasized hematogenously to both ovaries (called Krukenberg tumors). Stomach cancer is the most common primary site for metastasis to the left supraclavicular nodes.
The signet-ring cell type of stomach cancer usually is associated with Krukenberg tumors of the ovaries. This high-grade cancer diffusely infiltrates the wall of the stomach, giving it a firm, nonpliable consistency, hence the term "linitis plastica" or "leather bottle" stomach. Signet-ring cells are malignant cells filled with mucin; the mucin pushes the nucleus to the periphery of the cell, giving the cell a signet-ring appearance. |
Option A (primary malignant lymphoma of the stomach with ovarian metastasis) is incorrect. Gastric lymphomas are uncommon and rarely metastasize to the ovaries.
Option B (primary ovarian cancer with metastasis to the left supraclavicular lymph nodes) is incorrect. This does not explain the patient's epigastric distress and black, tarry stools. Option C (primary ovarian cancer with metastasis to the stomach) is incorrect. Ovarian cancers rarely metastasize to the stomach or to the left supraclavicular lymph nodes. Option D (primary pancreatic cancer with ovarian metastasis) is incorrect. Most pancreatic cancers involve the head of the pancreas and are associated with obstructive jaundice and light-colored stools. Pain usually radiates to the back, because the pancreas is retroperitoneal. Pancreatic cancers do metastasize to the left supraclavicular lymph nodes. |
|
|
A 38-year-old woman with chronic liver disease complains of involuntary, flinging movements of her limbs. She states that other members of her family have had chronic liver disease, dementia, and abnormal body movements. Physical examination shows greenish-brown deposits near the limbus of both eyes, an enlarged, firm liver, and splenomegaly. Which of the following laboratory studies would most likely be abnormal in this patient?
A. Decreased serum ceruloplasmin B. Increased percent iron saturation C. Increased total iron-binding capacity D. Increased total serum copper |
Option A (decreased serum ceruloplasmin) is correct. The patient has Wilson's disease (hepatolenticular degeneration), which is inherited as an autosomal recessive trait. The disease is characterized by a defect in the elimination of copper in bile. Copper accumulates in the liver, producing toxic damage to the hepatocytes, starting as acute hepatitis and progressing to chronic hepatitis and cirrhosis. Serum copper levels reflect the amount of copper bound to ceruloplasmin (90-95% of the total serum copper level) plus free and unbound copper. As expected in any chronic liver disease, protein synthesis is decreased, including synthesis of ceruloplasmin. Hence, the decrease in ceruloplasmin leads to a decrease in the total serum copper level, with a corresponding increase in the circulating level of free copper. The excess copper accumulates in Descemet's membrane of the eyes, producing the Kayser-Fleischer ring. In the brain, copper produces toxic injury in the basal ganglia, particularly in the putamen, where it causes atrophy and visible cavitation. When toxic injury occurs in the subthalamic nucleus, the patient develops hemiballismus (flailing of the limbs). Extrapyramidal signs and dementia also may occur.
|
Option B (increased percent iron saturation) is incorrect. This implies the presence of acquired iron overload disease (hemosiderosis) or hemochromatosis, which is an autosomal recessive disorder. Diseases caused by iron overload are not associated with pigment deposits in the eyes, dementia, or movement disorders.
Option C (increased total iron-binding capacity) is incorrect. This reflects increased synthesis of transferrin in the liver, which primarily occurs in iron deficiency anemia. In chronic liver disease, the total iron-binding capacity is decreased due to decreased synthesis of transferring. Option D (increased total serum copper) is incorrect. The serum ceruloplasmin is decreased in patients with Wilson's disease; total serum copper level is decreased, and the free copper level is increased in serum and urine. Total copper levels are increased in the liver parenchyma. |
|
|
An afebrile 35-year-old sheepherder who is living in a Basque community in southern Arizona complains of recurrent right upper quadrant pain. The sheepherder says that he and his dog spend their days together tending the sheep. A complete blood cell count shows a marked increase in the percentage of eosinophils. An ultrasound of his liver shows a cystic mass with calcifications in the lining of the cyst. Which of the following most accurately describes the epidemiology of this patient's liver disease
A. The dog ate infected sheep B. The dog is an intermediate host C. The sheep is a definitive host D. The sheepherder ate infected sheep E. The sheepherder is a definitive host |
Option A (the dog ate infected sheep) is correct. The patient has echinococcosis due to the tapeworm Echinococcus granulosis or E. multilocularis. In the normal developmental cycle of the Echinococcus species, adult worms mate and lay eggs that develop into larvae. The larvae mature into adult worms, and the cycle repeats. Hosts containing the larval form are called intermediate hosts, while hosts containing the adult worms are called definitive hosts.
|
Option B (the dog is an intermediate host) is incorrect. Adult worms in the dog mate and lay eggs. The sheepherder picks up the eggs by petting the dog, then handling his own food and unknowingly ingesting the eggs. The eggs develop into larvae in the sheepherder. The sheepherder then becomes the intermediate host.
Option C (the sheep is a definitive host) is incorrect. The dog becomes the definitive host. Option D (the sheepherder ate infected sheep) is incorrect. The sheep is the intermediate host. Option E (the sheepherder is a definitive host) is incorrect. The larvae penetrate the wall of the duodenum, transmigrate across the peritoneum, and penetrate the liver to produce a single cyst (E. granulosis ) or multiple cysts (E. multilocularis). The cysts contain numerous scolices with hooklets representing the heads of future adult worms; however, because the sheepherder is the end-stage of the cycle, adult worms are never produced. Cyst walls often become calcified. Rupture of a cyst often results in anaphylactic shock. Treatment with albendazole and percutaneous drainage or surgery is the treatment of choice. |
|
|
A 24-year-old professional weight lifter develops sudden onset of abdominal pain while bench-pressing 550 pounds. Within 10 minutes of the onset of pain, he becomes hypotensive and collapses. During emergency surgery, the surgeon finds clotted and unclotted blood filling the peritoneal cavity. Which of the following best explains the likely origin of the patient's intra-abdominal bleeding?
A. Ruptured abdominal aortic aneurysm B. Ruptured cavernous hemangioma of the liver C. Ruptured liver cell (hepatic) adenoma D. Ruptured splenic artery aneurysm |
Option C (ruptured liver cell adenoma) is correct. Professional weight lifters commonly use anabolic steroids to increase muscle mass and strength. One of the complications of anabolic steroids is the development of liver cell (hepatic) adenomas, which are benign tumors arising from hepatocytes. These tumors tend to rupture and produce intraperitoneal hemorrhage. Women taking estrogen-containing medications are subject to the same complication.
|
Option A (ruptured abdominal aortic aneurysm) is incorrect. The most common mechanism for producing these aneurysms is atherosclerosis. Most abdominal aortic aneurysms occur in men over 50 years of age.
Option B (ruptured cavernous hemangioma of the liver) is incorrect. Cavernous hemangiomas are the most common benign tumor of the liver. Although large cavernous hemangiomas can rupture, the clinical scenario in this case involving a professional weight lifter shifts the differential to a liver cell adenoma as the more likely cause of the intra-abdominal bleeding. Option D (ruptured splenic artery aneurysm) is incorrect. Splenic artery aneurysms are the second most common intra-abdominal aneurysm. They are more commonly found in women and often rupture during pregnancy. |
|
|
An 84-year-old man complains of lower back pain and inability to void urine over the past 24 hours. Physical examination shows point tenderness over the lower lumbar vertebrae and an enlarged bladder extending to the level of the umbilicus. The physician suspects metastatic prostate cancer. Which of the following is indicated as the first step in the management of this patient?
A. Digital rectal examination B. Prostate-specific antigen (PSA) C. Radionuclide bone scan D. Serum alkaline phosphatase E. Transrectal ultrasound with biopsy |
Option A (digital rectal examination) is correct. Prostate cancer is the most common cancer in men. Point tenderness over the vertebral bodies in an elderly patient is highly suggestive of metastatic prostate cancer, especially coupled with clinical evidence of urinary retention. Because prostate cancers develop in the peripheral zone of the prostate, they are palpated easily by digital rectal examination, especially if they have already spread beyond the gland.
|
Option B (prostate specific antigen) is incorrect. Although a serum PSA test is always part of the work-up of prostate cancer, a digital rectal examination is accomplished in a few minutes and provides immediate information. Furthermore, PSA is not 100% specific for prostate cancer, because the level is also increased in benign prostatic hyperplasia (BPH). In the absence of vertebral body tenderness in this patient, BPH would have been the most likely cause of urinary retention. BPH develops in the periurethral zone of the gland; hence enlargement is more likely to cause obstructive uropathy than prostate cancer. Urinary retention secondary to prostate cancer can occur when disease has invaded the bladder neck and obstructed the ureters. Unlike prostatic acid phosphatase, a rectal examination does not falsely increase serum PSA levels.
Option C (radionuclide bone scan) is incorrect. A radionuclide bone scan would be essential for identifying bone metastasis in this patient, however, osteoarthritis and lumbar strain can mimic metastatic cancer to bone. Option D(serum alkaline phosphatase) is incorrect. Prostate cancer is the most common cause of osteoblastic metastases in men. An osteoblastic response in bone results in increased bone density and increased serum alkaline phosphatase. An increased serum alkaline phosphatase lacks specificity, however, because it is also elevated in osteoarthritis (due to reactive bone formation) and cholestatic and metastatic liver disease (due to increased synthesis by bile duct epithelium). Option E (transrectal ultrasound with biopsy) is incorrect. This is the confirmatory test for prostate cancer, not the initial screening test. |
|
|
The mother of an atopic 8-year-old boy notices that her son's face and legs began to swell over the past few days. She assumes that the boy is experiencing a reaction to something he ate, so she immediately takes him to the emergency department. Physical examination shows a normotensive child with generalized pitting edema. Laboratory studies include a normal complete blood cell count, and a urinalysis showing a positive dipstick reaction to protein and a sediment containing numerous fatty casts. Electron microscopy of the glomeruli in this patient would most likely demonstrate
A. fusion of the podocytes B. intramembranous electron-dense deposits C. mesangial electron-dense deposits D. subendothelial electron-dense deposits E. subepithelial electron-dense deposits |
Option A (fusion of the podocytes) is correct. The patient has the classic findings of nephrotic syndrome, which, in children, is usually due to lipoid nephrosis (minimal change disease). Preceding upper respiratory infection, atopy, nonsteroidal anti-inflammatory drugs, and Hodgkin's disease all have been implicated in the pathogenesis of the disease. The gold standard for diagnosis of nephrotic syndrome is a 24-hour urine protein level >3.5 g (<150 mg/24 h). In lipoid nephrosis, a T-cell immune reaction against visceral epithelial cells causes loss of the negative charge of the glomerular basement membrane (called polyanion loss), which results in a selective loss of albumin in the urine. Because the plasma albumin concentration is responsible for 80% of the oncotic pressure, hypoalbuminemia results in leakage of a protein-poor transudate from the vascular compartment into the interstitial tissue (pitting edema) and body cavities (ascites). Furthermore, hypoalbuminemia stimulates increased liver synthesis of cholesterol and subsequent hypercholesterolemia (type II hyperlipoproteinemia). Cholesterol leaks into the urine, producing fatty casts that polarize and often show "Maltese crosses." Lipid stains are positive in the glomeruli and renal tubular cells; however, no proliferative or glomerular basement membrane changes are seen in the glomeruli. Immunofluorescent stains are negative. Electron microscopy shows fusion of the podocytes, which is a universal finding in any nephrotic syndrome. Lipoid nephrosis is not considered an immunocomplex-mediated disease, since no electron-dense deposits are found in the glomeruli. Children respond extremely well to steroid therapy.
|
Option B (intramembranous electron-dense deposits) is incorrect. These findings are consistent with type II membranoproliferative glomerulonephritis ("dense deposit" disease), which produces nephrotic syndrome. An autoantibody against C3, called the C3 nephritic factor, causes continual activation of the alternative pathway, leading to low complement levels.
Option C (mesangial electron-dense deposits) is incorrect. These findings are consistent with IgA glomerulonephritis (Berger's disease), which is the most common type of glomerulonephritis. Children have recurrent macrohematuria (usually following respiratory infections), whereas adults have recurrent microhematuria. Option D (subendothelial electron-dense deposits) is incorrect. These findings are seen in type IV proliferative glomerulonephritis in patients with systemic lupus erythematosus and in type I membranoproliferative glomerulonephritis. Option E (subepithelial electron-dense deposits) is incorrect. These findings are seen in poststreptococcal glomerulonephritis and diffuse membranous glomerulonephritis, which is the most common cause of nephrotic syndrome in adults. |
|
|
A tall, obese 13-year-old boy has bilateral gynecomastia, decreased testicular volume for his age, and sparse axillary and pubic hair. He had the usual childhood infections, except for mumps. A CT scan of the pituitary gland is normal. A buccal smear preparation shows a single Barr body extending off the nuclear membrane of many squamous cells. The results of a chromosome study are pending. Which of the following sets of laboratory studies would be expected in this patient?
--------------------------------------------------- Serum Serum Serum FSH LH testosterone --------------------------------------------------- A. High High Low B. High Normal Normal C. Low Low Low D. Normal High Low --------------------------------------------------- FSH = follicle stimulating hormone LH = luteinizing hormone |
Option A (high FSH; high LH; low testosterone) is correct. The patient has Klinefelter's syndrome, which is a sex-chromosome disorder with 47 chromosomes (XXY). These patients have one Barr body, because one of the two X chromosomes is randomly inactivated. Abnormal numbers of chromosomes are usually due to nondisjunction in the first step of meiosis. Most patients are diagnosed in adolescence, when males fail to show appropriate secondary sex characteristics of puberty. Physical examination shows disproportionately long arms and legs (eunuchoid proportions), decreased testicular volume for age, sparse axillary and pubic hair, and gynecomastia; the last two findings are related to hyperestrinism. Both testicles are atrophic, with atrophy and fibrosis of the seminiferous tubules and no evidence of spermatogenesis (azoospermia). There is hyperplasia of the Leydig cells. The absence of Sertoli cells in the fibrosed seminiferous tubules results in decreased synthesis of the hormone inhibin, which normally has a negative feedback relationship with FSH. Hence, FSH levels in Klinefelter's syndrome are markedly elevated. Because FSH normally increases the synthesis of aromatase in Leydig cells, hyperplasia of the Leydig cells causes an even greater conversion of testosterone into estradiol than normal. Therefore, the patient develops signs of hyperestrinism and hypogonadism, due to low testosterone levels. Decreased synthesis of testosterone, which normally has a negative feedback on LH, leads to an increase in LH.
|
Option B (high FSH; normal LH; normal testosterone) is incorrect. These findings are consistent with pure seminiferous tubule failure. Loss of inhibin leads to an increase in FSH. Because Leydig cells are functional, serum LH and testosterone are normal.
Option C (low FSH; low LH; and low testosterone) is incorrect. These findings are consistent with hypopituitarism, where FSH and LH are decreased, with low LH leading to decreased testosterone synthesis. Option D (normal FSH; high LH; low testosterone) is incorrect. These findings are consistent with a pure Leydig cell failure, where a decrease in testosterone leads to an increase in LH. FSH is normal, because the seminiferous tubules are normal. |
|
|
A 42-year-old woman complains of chronic constipation and progressive weight gain over the past 6 months despite maintaining a pure vegan diet. She takes no prescription or over-the-counter medications. Physical examination shows a pale woman with brittle hair, periorbital puffiness, a symmetrically enlarged, nontender thyroid gland, delayed deep tendon reflexes, and proximal muscle weakness in her lower extremities. Serum creatine kinase level is 350 U/L. Which of the following sets of thyroid function studies is most compatible with this patient's clinical findings?
------------------------------------------------------------- Serum T4 Serum TSH 131I ------------------------------------------------------------- A. Low Low Low B. Low High Normal C. High Low Low D. High Low High ----------------------------------------------------------------- T4= thyroxine; TSH = thyroid-stimulating hormone; 131I = radioactive iodine uptake |
Option B (low T4; high TSH; normaln131I) is correct. The patient has primary hypothyroidism, most likely secondary to Hashimoto's thyroiditis. Hashimoto's thyroiditis is an autoimmune thyroiditis with an increase in antimicrosomal and thyroglobulin antibodies. Along with autoimmune destruction of the gland, an autoantibody directed against the TSH receptor inhibits the gland from synthesizing thyroid hormone. The patient exhibits all of the classic signs of hypothyroidism\: brittle hair, periorbital puffiness, delayed deep tendon reflexes, and primary myopathy of the proximal muscles of the thigh (note the increase in serum creatine kinase). As expected, serum T4 levels are decreased because the gland is being destroyed, and serum TSH is increased due to loss of the negative feedback of T
|
Option A (low T4; low TSH; low 131 I) is incorrect. These findings are most consistent with secondary hypothyroidism, usually due to hypopituitarism. In children, a craniopharyngioma is the most common cause of hypopituitarism; in adults, a nonfunctioning pituitary adenoma is usually responsible for this condition.
Option C (high T4; low TSH; low 131I) is incorrect. These findings are most consistent with a patient whose hyperthyroidism developed from taking an excess amount of thyroid hormone, usually for weight loss. In these patients, the thyroid gland is suppressed and nonpalpable, unlike a gland that produces excessive thyroid hormone. The 131I is decreased, because the gland is inactive and not capable of increasing the uptake of iodine to synthesize thyroid hormone. Option D (high T4; low TSH; high 131 I) is incorrect. These findings are consistent with Graves' disease, which is the most common cause of hyperthyroidism. These patients have an autoantibody against the TSH receptor that increases the synthesis of thyroid hormone. Exophthalmos and pretibial myxedema are unique to the disease. Unlike hyperthyroidism due to exogenous intake of excess thyroid hormone, in Graves' disease, the 131I uptake is high, because the gland requires iodine to synthesize T4 and is diffusely enlarged. |
|
|
A 35-year-old pharmacist complains of recurrent episodes of forgetfulness and tiredness. Physical examination is essentially unremarkable. Laboratory studies show a serum glucose level of 20 mg/dL. Additional studies on the same serum sample show a high serum insulin level and a low C-peptide level. Based on these findings, which of the following is the most likely diagnosis?
A. Benign tumor involving b-islet cells in the pancreas B. Ectopic secretion of an insulinlike factor C. Malignant tumor involving a-islet cells in the pancreas D. Surreptitiously injected human insulin |
Option D (surreptitiously injected human insulin) is correct. Normally, b-islet cells first synthesize preproinsulin in the rough endoplasmic reticulin. Preproinsulin then is delivered to the Golgi apparatus, where proteolytic reactions generate insulin and a cleavage peptide called C peptide. Hence, C peptide is a marker for endogenous synthesis of insulin. In this case, the patient has been injecting himself with insulin. This increases the serum insulin level; however, serum C peptide is decreased due to suppression of the b-islet cells by the exogenously administered insulin.
|
Option A (benign tumor involving b-islet cells in the pancreas) is incorrect. Insulinomas are benign tumors of the b-islet cells that synthesize excess insulin, resulting in severe fasting hypoglycemia. As expected, these patients have increased serum insulin and C-peptide levels, indicating that b -islet cells are synthesizing the insulin.
Option B (ectopic secretion of an insulinlike factor) is incorrect. This lowers both the serum insulin and the C-peptide levels due to hypoglycemia suppressing the b-islet cells from synthesizing insulin. b-islet cells in the pancreas) is incorrect. This describes a glucagonoma, which produces hyperglycemia by stimulating gluconeogenesis. |
|
|
An autopsy performed on a 40-year-old man with dementia shows atrophy of the frontal and temporoparietal lobes of the brain. Histologic examination shows senile plaques. The pathogenesis of the dementia in this patient is most closely related to which of the following?
A. b-amyloid protein B. Decreased dopamine levels C. Slow virus disease D. Triplet repeat mutation |
Option A (b-amyloid protein) is correct. Senile plaques are characteristic of Alzheimer's disease (AD), which is the most common cause of dementia in patients over 65 years of age. Senile plaques contain a core of A-b-amyloid surrounded by neurites. The explanation for the age disparity in this case is that the patient has Down syndrome with three functioning chromosome number 21 (e.g., trisomy 21). Chromosome 21 codes for an Alzheimer precursor protein (APP), part of which is amyloid-b (A- b) protein. This protein is toxic to neurons; hence the extra chromosome 21 codes for more of the protein, which results in AD at an early age.
|
Option B (decreased dopamine levels) is incorrect. This describes Parkinson's disease, where there is degeneration and depigmentation of neurons in the substantia nigra and locus ceruleus and a corresponding decrease in the synthesis of the neurotransmitter dopamine. Patients have extrapyramidal signs and symptoms and occasionally develop dementia.
Option C (slow virus disease) is incorrect. Slow virus diseases include subacute sclerosing panencephalitis (associated with measles), progressive multifocal leukoencephalopathy (associated with papovavirus), and Creutzfeldt-Jakob disease (associated with prions). Although all of these diseases produce dementia, senile plaques are not present in the brain tissue. Option D (triplet repeat mutation) is incorrect. A triplet repeat mutation associated with dementia is Huntington's disease, which is an autosomal dominant disease with triplet repeats of CAG on the short arm of chromosome 4. Atrophy and loss of striatal neurons occur in the caudate nucleus, putamen, and frontal cortex; however, there are no senile plaques in the tissue. Furthermore, patients have chorea and extrapyramidal signs, which are not seen in AD. |
|
|
A 30-year-old woman states that she often burns her hands without feeling any pain. Physical examination shows decreased pain and temperature sensation in the upper extremities, atrophy of the intrinsic muscles of the hands, and abnormal deep tendon reflexes in the upper extremities. The pathogenesis of this patient's neurologic problems is most closely associated with which of the following?
A. Autoimmune destruction of myelin B. Fluid-filled cavity in the cervical spinal cord C. Superoxide free radical destruction of upper and lower motor neurons D. Tumor in the cervical spinal cord E. Vitamin B12 deficiency |
Option B (fluid-filled cavity in the cervical spinal cord) is correct. The patient has syringomyelia, the development of an expanding fluid-filled cavity in the cervical spinal cord. This results in destruction of the crossed lateral spinothalamic tracts (loss of pain and temperature sensation), anterior horn cells (loss of the intrinsic muscles of the hand), and other tracts as the cavity expands. It is often confused with amyotrophic lateral sclerosis (ALS); however, in ALS there are no sensory abnormalities.
|
Option A (autoimmune destruction of myelin) is incorrect. Multiple sclerosis (MS) is the most common demyelinating disease. Symptoms of MS include blurry vision (optic neuritis), intention tremors, nystagmus, ataxia, and scanning speech.
Option C (superoxide free radical destruction of upper and lower motor neurons) is incorrect. This describes the pathogenesis of some cases of ALS where there is a defect in superoxide dismutase on chromosome 21, leading to superoxide free radical damage of upper and lower motor neurons. Option D (tumor in the cervical spinal cord) is incorrect. Although a cervical spinal cord tumor potentially could produce the neurologic findings seen in this patient, the sequence of neurologic defects is more compatible with syringomyelia. Option E (vitamin B12 deficiency) is incorrect. Vitamin B12 deficiency is associated with subacute combined degeneration of the spinal cord. The posterior columns and lateral corticospinal tracts are demyelinated, leading to loss of proprioception (posterior column disease) and upper motor neuron signs and symptoms (lateral corticospinal tract). |
|
|
A 45-year-old woman with a history of mitral stenosis and chronic arrhythmia dies suddenly at her home. At autopsy, a wedge-shaped hemorrhagic lesion is seen at the periphery of the temporal lobe. The mechanism for the temporal lobe lesion is most closely associated with which of the following conditions?
A. Atherosclerosis of the internal carotid artery B. Embolic occlusion of a cerebral artery C. Intracerebral hematoma D. Neoplastic transformation of astrocytes E. Rupture of a congenital aneurysm |
Option B (embolic occlusion of a cerebral artery) is correct. Patients with mitral stenosis develop left atrial dilatation and produce thrombi due to stasis of blood in the chamber. Furthermore, left atrial dilatation predisposes to atrial fibrillation. The combination of a thrombus in the left atrium and atrial fibrillation results in multisystem embolic disease with infarctions. When emboli from the heart disseminate to the brain, they usually enter the middle cerebral artery. Occlusion of the artery results in wedge-shaped infarction extending to the periphery of the brain. When the embolus dissolves, reperfusion of the infarcted area causes a hemorrhagic infarction. An infarction in the brain is an example of liquefactive (not coagulative) necrosis.
|
Option A (atherosclerosis of the internal carotid artery) is incorrect. An atherosclerotic stroke is usually due to a platelet thrombus overlying an atherosclerotic plaque near the bifurcation of the internal carotid artery. This produces a pale infarction of the ipsilateral brain that extends to the periphery of the brain. However, unlike an embolic stroke, reperfusion is less likely to occur, so the infarct remains pale due to the lack of blood flow to the area.
Option C (intracerebral hematoma) is incorrect. Intracerebral hematomas usually are caused by hypertension. Long-standing hypertension leads to the formation of Charcot-Bouchard macroaneurysms of the lenticulostriate vessels, which supply the putamen and thalamus. When these aneurysms rupture, they produce an intracerebral hematoma (not an infarction), most commonly in the basal ganglia area of the brain. Other areas where hematomas can form in a hypertensive bleed are the pons and cerebellar hemispheres. Option D (neoplastic transformation of astrocytes) is incorrect. Astrocytomas are neoplasms arising from astrocytes. Low-grade astrocytomas (grades I and II) are benign; high-grade astrocytomas (e.g., glioblastoma multiforme) are malignant. Glioblastoma multiforme is the most common primary brain tumor found in adults and is characterized by hemorrhagic necrosis. The frontal lobes usually are involved, and the tumor frequently extends across the corpus callosum to the contralateral lobe. Option E (rupture of a congenital aneurysm) is incorrect. Congenital aneurysms in the brain usually develop at the junction of the anterior communicating artery with the anterior cerebral artery or the posterior communicating artery with the posterior cerebral artery. Loss of internal elastic lamina and smooth muscle at the branching points of the vessel occurs, predisposing to berry aneurysm formation. When these rupture, the blood usually enters the subarachnoid space, causing a severe occipital headache and loss of consciousness. |

