![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
121 Cards in this Set
- Front
- Back
|
Breast Cancer Detection Demonstration Project
|
The BCDDP was inplemented in 1973. In this project, 280,000 women underwent annual screening for breast cancer for 5 years at 29 locations throughout the US. Was organized by the American Cancer Society (ACS) and the National Cancer Institute (NCI) and demonstrated that screening, physical examination, mammography and BSE could provide an early diagnosis. Mammography alone found 41% of the cancers and MOST of the early breast cancers.
|
|
|
Justifying Mammogram when a patient is frightened of radiation risk
|
A person is exposed to about the same radiation as she would have gotten walking bare breasted along the beach at noon for 10 minutes. But, that small amount of radiation can detect minute tumors that might save your life if detected early. There is no evidence to suggest that the small doses of diagnostic x-rays used in mammo can induce breast cancer. There are studies supporting LARGE doses increasing cancer such as Hiroshima and Nagasaki.
|
|
|
DIagnosis vs Detection of Cancer
|
Detection is the screening measurements we take to try and find cancer. Detection does not say benign or malignant, just that something is there. This includes breast exams and mammography.
Diagnosis comes with biopsy when specific cells can be identified as cancerous. |
|
|
Two Localization Methods of Lesions in the Breast
|
Free-hand or with a localization device. Can be used with Various techniques for locating tumors, such as angiography, lymphography, hysterography and various scanning methods
|
|
|
Involution
|
Involution is the decrease in size and number of TDLU's over monthly cycles and pregnancies.
|
|
|
Three Major Types of Tissue Variation for Breasts
|
This could be lobules, ducts, and connective tissue
OR This could be fat, fibrous, and glandular. |
|
|
Lobules, Ducts, and Connective Tissue
|
The lobules make the milk and send them through the ducts to the nipple. The connective tissue supports the lobules and ducts and the TDLU system.
|
|
|
TDLU
|
The TDLU consists of the intralobular duct along whose lumen and end protrude blunt or round saccules called ductules, which differentiate into the secretory units or acini during lactation. Individual lobes vary greatly in size and typically about less than half enlarge to become functional during lactation. The TDLUs are embedded in specialized, hormonally responsive connective tissue stroma, the intralobular stroma.
|
|
|
Fat, Fibrous, and Glandular Tissues
|
Fat varies with age and parity and is radiolucent.
Fibrous tissue is the connective/supportive tissue and is radiopaque. Glandular tissues are the ductal tissues and are radiopaque. |
|
|
Xeroradiography
|
A diagnostic x-ray technique in which images are produced electrically rather than chemically, permitting lower exposure times and radiation energies than those of ordinary x-rays. The latent image is made visible with a powder toner similar to that used in a copying machine. Not used today due to high-resolution, fast screen speed film that is not as messy and just as good at showing minute calcifications.
|
|
|
The Five Common Views for Breast Imaging
|
1. Craniocaudal
2. Mediolateral 3. Mediolateral Oblique 4. Microfocus Magnification 5. Coned Compression |
|
|
Craniocaudal Projection
|
The breast is compressed and imaged from top to bottom.
|
|
|
Mediolateral Projection
|
The breast is compressed side to side and imaged from the medial aspect to the lateral aspect.
|
|
|
Mediolateral Oblique Projection
|
The breast is compressed diagonally toward the armpit and imaged from the medial aspect to the lateral aspect.
|
|
|
Microfocus Magnification of the Breast
|
Done when something is seen on the normal views. Uses a very small focal spot with and increased OID to magnify the area of interest. Gives increased resolution, reduces noise, but increases patient dose.
|
|
|
Coned Compression of the Breast
|
This is like a spot film of a small area. A small cone is used to compress the area of interest and then this will decrease scatter, spread the parenchyma out of the way, and give sharp detail of a small area.
|
|
|
Ecklund Technique
|
The Ecklund Technique (also called the Implant Displaced or ID technique) is used to image breasts with implants. The implant is pushed posteriorly against the chest wall so that it is excluded from the image and the breast tissue surrounding the implant is pulled anteriorly and compressed. The CC and MLO positions are usually utilized in the Ecklund technique.
|
|
|
Isolation of Non-Palpable Lesions
|
When a non-palpable lesion is found and needs a biopsy, the abnormality must be accurately located so that the smallest amount of tissue is removed for evaluation minimizing trauma to the breast. These lesions can be localized using 3 techniques:
1. Needle-wire localization for open surgical biopsy. 2. Fine-needle aspiration biopsy (FNAB) 3. Large-core needle biopsy (LCNB) |
|
|
Needle-Wire localization
|
Uses a needle that contains a hooked guide wire to lead the surgeon directly to the suspicious tissue.
|
|
|
Fine-Needle Aspiration Biopsy
|
FNAB uses a hollow small-gauge needle to extract tissue cells from a suspicious lesion. FNAB can decrease the need for surgical excisional biopsy by identifying benign lesions.
|
|
|
Large-Core Needle Biopsy
|
LCNB obtains small samples of breast tissue by means of a 9, 11, or 14 gauge needle with a trough adjacent to the tip of the needle. Because larger tissue samples are obtained, clinical support exists for this technique instead of surgical excisional biopsy.
|
|
|
Stereotactic Biopsy
|
Stereotactic intervention (also called stereotaxis) is a minor surgical procedure used to determine whether a lesion is benign or malignant. 3D triangulation is used to identify the exact location of a breast lesion. A digitizer calculates X, Y, and Z coordinates. The X coordinate denotes transverse location, Y depth, and Z height of the lesion. LCNB is the preferred method to use with stereotactic biopsy.
|
|
|
Benefits of Sterotaxis over Surgical Biopsy
|
Less pain, less scarring, shorter recovery time, less patient anxiety, and lower cost.
|
|
|
True Cut Core Biopsy
|
This is actually a stereotactic biopsy. Just another name. The needle is "triggered" to center of the mass and a block of tissue is removed.
|
|
|
Differences in Biopsy Results
|
Fine needle aspiration - Gets cells
True Cut/Stereotactic - Tissue sample Incisional Biopsy - takes a sample Excisional Biopsy - takes the whole mass Brush biopsy - Scrapes cells through the ducts |
|
|
Surgical Techniques - Mutilating Surgeries
|
Standard Radical Mastectomy - Breast, skin, pectoralis muscle, lymph nodes - side effects of edema and depression.
Extended radical Mastectomy - Removes all of above and more tissue. |
|
|
Surgical Techniques - Less Invasive
|
Modified Radical Mastectomy - Breast and Nodes removed
Simple Mastectomy - always leaves tissue and there is no node biopsy Segmental Mastectomy - sections of breast tissue removed Lumpectomy/biopsy - cells or tumor only removed. |
|
|
Breast Specimin Radiography
|
Used to determine that an entire lesion has been removed. The specimin is compressed and magnified. It is usually done while the pt is still under anesthesia so they can go in and take more tissue if needed. Orientation of the tumor, technical factors, and film type must be established and accepted by the whole team to ensure that the tumor is visualized correctly in relation to the breast for localization if more tissue needs to be removed.
|
|
|
Risk Factors Associated with Breast Cancer
|
- Female/getting old
- Genetics - BRCA1 and BRCA 2 - Familial history - Lifestyle to include diet, obesity, alcohol, smoking, physical activity - Reproductive factors to include long menstrual history, never having children, recent use of contraceptives, having 1st child after 30, postmenopausal obesity, HRT therapy, and breast feeding - Prior benign breast disease, hyperplasia - Ionizing radiation - geography/ethnicity - mediations such as tamoxifen/HRT - Underwire bras/Antipersperants |
|
|
The Five Common Views for Breast Imaging
|
1. Craniocaudal
2. Mediolateral 3. Mediolateral Oblique 4. Microfocus Magnification 5. Coned Compression |
|
|
Craniocaudal Projection
|
The breast is compressed and imaged from top to bottom.
|
|
|
Mediolateral Projection
|
The breast is compressed side to side and imaged from the medial aspect to the lateral aspect.
|
|
|
Mediolateral Oblique Projection
|
The breast is compressed diagonally toward the armpit and imaged from the medial aspect to the lateral aspect.
|
|
|
Microfocus Magnification of the Breast
|
Done when something is seen on the normal views. Uses a very small focal spot with and increased OID to magnify the area of interest. Gives increased resolution, reduces noise, but increases patient dose.
|
|
|
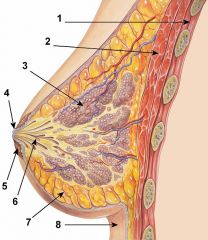
1. Chest wall
2. Pectoralis Muscle 3. Lobules 4. Nipple 5. Areola 6. Lactiferous ducts 7. Fat tissue 8. Inframammary Crease |
|
|
Serratus Anterior
|
Muscle that supports the breast along with the pectoralis major muscle. The base of the breast rests on these muscles.
|
|
|
Axillary Tail of the Breast
|
Extends from the upper lateral base of the breasts into the axillary fossa (armpit)
|
|
|
Cooper's Ligaments
|
Suspensory ligaments that support the breast. Give breasts their firmness or lack of firmness. These separate the lobes.
|
|
|
Lobules
|
Each breast contains 15-20 lobes which contain many lobules, the structural units of the breast.
|
|
|
Acini
|
Each lobule consists of several acini which are the glandular elements of the breast. Each lobule also contains draining ducts and the interlobular stroma or connective tissue.
|
|
|
Mammography 20 years ago VS Today
|
20 Years Ago
- Higher dose - No regulations so machines were often subpar - screen-film - little resolution for detail Today - Moving quickly to digital film - less radiation dose - highly regulated - High resolution |
|
|
Radiation Dose to Breasts in Mammography
|
Entrance Skin Exposure (ESE) - average is 800mR per view.
Glandular Dose is approxamitely 15% of the ESE and should not exceed 100 mR per view. |
|
|
Important Factors affecting Dose in Mammography
|
- Use of grids or not
- Digital vs Film-screen - Number of Views - Technologist Skill/Repeat Rate - Patient Movement |
|
|
Breast Imaging Using MRI
|
MRI imaging of the breast is used to track silicon leaks in breasts and screen for early malignancies. Often done using contrast injected into the veins. Problem is many false positives.
|
|
|
Breast Imaging Using CT
|
Can be used to detect the extent of disease in planning for surgery in those already diagnosed, but MRI does this already. Otherwise, CT is not very good for breast imaging and is too high dose.
|
|
|
Breast Imaging Using PET
|
Notes early tissue changes with the use of isotopes. Looks at activity in tissue instead of structure. Looks at use of glucose in breasts since tumors use a lot of glucose. Drawback is it is expensive.
|
|
|
Breast Imaging Using MIBI
|
This is a nuc med scan. Useful in dertermining benign lumps vs cancer. Not very sensitive to non-palpable lumps and fuzzy. Not good for screening due to radioactive isotope injection.
|
|
|
Breast Imaging Using Thermography
|
The belief is that cancer gives more heat due to blood flow. So a sensor is put on the breast and measures heat in different areas. From this a map is constructed with blue = cold and Red=hot. Hot areas are supposedly the cancerous areas. Not very accurate and has a lot of false positives and negatives!
|
|
|
Breast Imaging Using Transillumination
|
An old technique used before mammography used to determine if a lump was a cyst or solid. Measures amount of light transmitted through the lump. Not a great screening test but can be helpful in conjunction with mammo.
|
|
|
Breast Imaging using Tomosynthesis
|
A 3- dimensional image is created by acquiring images of a stationary compressed breast at multiple angles during a short scan. The individual images are then reconstructed into a series of thin high-resolution slices that can be displayed individually or in a dynamic cine mode.
|
|
|
Breast Imaging Using Sonography
|
High frequency sound waves are sent off in little pulses toward the breast. If something gets in the way of the waves, they bounce back. Can't pick up fine detail of x-ray, but shows other characteristics of a lump and doesn't use radiation. Used mostly to look at a specific area where a lump is already known to be and helps to determine fluid-filled or solid. Also good for distinguishing tissue differences where x-ray is limited.
|
|
|
Prevalence of Cancer
|
Lifetime Risk = 1 in 2 men will develop, 1 in 3 women will develop. Cancer incidence rates have remained relatively steady as have cancer death rates.
|
|
|
Five Year Survival
|
Is used as a means to indicate the severity of cancer in relation to death. A five year survival is considered "cancer survival" and after this point, a person who has stayed cancer "free" is less likely to have breast cancer again.
|
|
|
Breast Cancer Statistics
|
- Breast cancer is 1 in 3 of every cancer diagnosed in women
- 192,000 new cases of invasive breast cancer will be diagnosed each year - 62,000 new cases of carcinoma in situ will be diagnosed each year (CIS is early diagnosis - no spread!) - 40,000 women will die from breast cancer each year. - Lifetime probability of developing breast cancer is 1 in 8. - Excluding skin cancers, Breast cancer is most common cancer in women. |
|
|
Breast Cancer statistics - Men
|
- 1,900 new cases of invasive breast cancer will be diagnosed each year in men (1%)
- 440 men will die from breast cancer each year - Is about 100X less common in men - Lifetime risk of getting breast cancer is 1 in 1000 |
|
|
Breast Cancer Facts
|
- Historically in older women, 77% of new cases and 84% of deaths occur in women 50 years and older
- Most lethal cancer for ages 30-45 - Second leading cause of cancer death in women behind lung cancer - Chance it will be responsible for a woman's death is 1 in 35 (3%) - Death rates declining since 1990. |
|
|
Lifestyle Recommendations for Cancer Risks
|
- No smoking
- No alcohol - Eat healthy (diet) - Exercise (no obesity) - Maintain balance of hormones, energy and immune system |
|
|
Primary Prevention of Disease
|
Primary prevention measures fall into two categories.
- The first category includes actions to protect against disease and disability, such as getting immunizations, ensuring the supply of safe drinking water, applying dental sealants to prevent tooth decay, and guarding against accidents. - General action to promote health is the other category of primary prevention measures. Health promotion includes the basic activities of a healthy lifestyle: good nutrition and hygiene, adequate exercise and rest, and avoidance of environmental and health risks. |
|
|
Secondary Prevention of Disease
|
The goal of secondary prevention is to identify and detect disease in its earliest stages, before noticeable symptoms develop, when it is most likely to be treated successfully. With early detection and diagnosis, it may be possible to cure a disease, slow its progression, prevent or minimize complications, and limit disability. Examples include blood pressure screening or breast cancer screening.
Another goal of secondary prevention is to prevent the spread of communicable diseases. |
|
|
Tertiary Prevention of Disease
|
Tertiary prevention programs aim to improve the quality of life for people with various diseases by limiting complications and disabilities, reducing the severity and progression of disease, and providing rehabilitation. Unlike primary and secondary prevention, tertiary prevention involves actual treatment for the disease.
|
|
|
Staging Purpose
|
Staging is done to determine severity of the cancer and the estimated survival rate to aid in: treatment plan, determining prognosis, evaluating treatment results, exhange of information, and cancer research.
|
|
|
Cure VS Palliation
|
A cure means the disease is comletely irradicated. Palliation means that we treat the symptoms of the disease but cannot cure it.
|
|
|
Screening Program Criteria
|
Due to MQSA (Mammography Quality Standards Act of 1992), a screening program must meet standards in:
- Personnel (qualifications) - Equipment - Reporting and record keeping - quality assurance - infection control - breast imaging to include implant and invasive - consumer complaints - mobile units |
|
|
Personnel Requirements for Mammography Screening - RT
|
- Initial RT licensing from ARRT or ARCERT
- 40 hrs training in mammo with at least 25 monitored exams - minimum of 8 hrs of documented training in any new modality - completion of at least 200 exams in previous 24 month period - minimum of 15 CEU in 36 months with 8 specific to each modality |
|
|
Personnel Requirements for Mammography Screening - MD
|
- Licensed to practice medicine
- either board certified rad or 3 months of formal approved training in interpretation of mammos - minimum of 60 category 1 CEU in each breast imaging modality - interpretation of at least 240 mammo exams in 6 month period under direct supervision - minimum of 15 category 1 CEU's in 36 months with 6 in each modality - interpret or multi-read at least 960 mammos in 24 months. |
|
|
Personnel Requirements for Mammography Screening - Physicist
|
- Qualified medical physicist with active status or licensure
- masters degree or higher in physical science with no less than 10 semester hrs of physics - 40 contact hrs of documented specialized training in conducting mammo surveys - experience conducting at least 1 mammo survey of at least 20 mammo units - 15 CEU's in 36 months - 2 facilities and 6 units every 24 months - maintain valid license. |
|
|
Interdisciplinary Evaluation of Cancer
|
Involves physicians from several disciplines, nurses, social workers, nutritionists, and other members of the health care team. Often provided by a tumor board. Then individual physicians will be in charge of different things such as a radiation oncologist planning treatment area, medical oncologist planning for aplasia and surgery during chemo if necessary, etc... The coordinating physician oversees all of this.
|
|
|
Coordinating Pysician Responsibility
|
The physician directing the cancer patient's management will consider how each step in the plan will be evaluated and how the procedures will be carried out to make subsequent treatments easier. They will be the patient's "doctor" and discuss all of the options, treatments, and results with the patient. They will assess impact on the family and provide access to support for that.
|
|
|
Breast Cancer Screening Program
|
Includes:
- Yearly mammo starting at age 40 - Clinical breast exam should be part of a periodic health exam about every 3 yrs for women in 20's and 30's and every yr for women 40 and older. - Women should know how their breasts normally feel and report changes promptly - Screening MRI recommended for women with approximately 20-25% or greater lifetime risk of breast cancer pertaining to family hx, ovarian cancer, and/or women treated for Hodgkin's disease. |
|
|
Breast Cancer Screening Effectiveness
|
Through the BCDDP it was found that by doing the screening program, earlier diagnosis could be made leading to better prognosis for full recovery.
|
|
|
Staging
|
Staging determines the location and spread of cancers. It is TNM - tumor, nodes, metastasis.
|
|
|
Staging TNM System
|
After each (T, N, and M) a modifier is placed to stage the disease. Modifiers are:
x = not assessed (ie can't find it) o = none is = in situ 1-4 = severity in size or location spread |
|
|
Types of TNM Staging
|
1. cTNM or TNM = Clinical staging - based on evidence before treatment from physical exam, rad studies, biopsy, lab tests.
2. pTNM - Pathological Classification - based on information aquired by a surgical procedure. 3. rTNM - Retreatment Classification - used after a disease free interval and when further treatment is planned. 4. aTNM - Autopsy Classification - after death and after complete pathologic study. |
|
|
Staging Examples
|
1. T3, N0, M0 = Larger tumor in a bad location with no nodal involvement and no metastasis.
2. T4, N3, M4 = Large tumor in a bad location, complete regional spread into nodes, and large spread of metastasis. |
|
|
Grading of Breast Cancer
|
Whereas staging determines the location and spread of cancer cells, GRADE describes the differentiation amount of the cells. It looks at the morphology of the tissue as compared to normal. Breast cancer uses regular grading in conjunction with a Scarf-Bloom-Richarson Score
|
|
|
Cancer Grading
|
American Joint Commission on Cancer Guidelines:
GX = Grade cannot be assessed G1 = Well differentiated (low grade) G2 = Moderately well-differentiated (intermediate grade) G3 = Poorly differentiated (High grade) G4 = Undifferentiated (high grade) *These estimate rate of growth as indicated by mitotic rates. |
|
|
Scarf-Bloom-Richardson (SBR) Breast Cancer Scoring
|
Gives a 1, 2, or 3 score in each of the following categories:
- Tubule Formation - how bad the tissue organization looks - Nuclear Pleomorphism - size, shape, variation Mitosis Count - Growth rate |
|
|
SBR Grade
|
The SBR Grade is determined using the score.
Grade 1 - Score of 3, 4, or 5 - shows well differentiated breast cells generally appearing normal and not growing rapidly, arranged in small tubules Grade 2 - Score of 6 or 7 - Moderatley differentiated breast cells with characteristics between 1 and 3 Grade 3 - Score of 8 or 9 - Poorly differentiated breast cells that do not appear normal and tend to grow rapidly and aggressively. * These three grades describe the invasiveness of the tumor |
|
|
Survival Rates Based on SBR Grade
|
Grade 1 - 95% 5 year survival rate
Grade 2 - 75% 5 year survival rate Grade 3 - 50% 5 year survival rate |
|
|
Prognosis of Breast Cancer
|
Depends on grade and staging, but overall prognosis is:
- Infiltrating Ductal - 80% of Breast Cancers - poor prognosis - Lobular (small cell) 10% of Breast Cancers - better prognosis - Various Other Types - 10% of Breast Cancers - best prognosis --includes things such as medullary cancer with is mostly in the left breast and rarely metastasizes. |
|
|
Treatment of Cancer
|
- Surgical Techniques to include mastectomy and lumpectomy
- Radiation - Chemotherapy - Drug Therapy |
|
|
Evolution of Bone Densitometry
|
Initiated in 1930's in historical order from the 30's to today:
1. Radiographic Absorbitometry 2. Radiogammetry 3. Quantitative Computed Tomography 4. Single/Dual Photom Absorptiometry 5. Dual X-ray Absorptiometry (DXA) |
|
|
Radiographic Absorbtiometry
|
Diagnostic radiographs measuring density
|
|
|
Radiogammetry
|
Looked at the digits to measure diameters of the cortex of the distal phalanx. Was used to measure bone density for astronauts.
|
|
|
Quantitative Computed Tomography (QCT)
|
Came about in the 1970's.
Is CT of the vertebral bodies. This allowed slices to look at trabecular bodies w/o overlying cortical spinous processes, pedicles, etc... Expensive and high dose though. |
|
|
Single/Dual Photon Absoptiometry
|
Nuclear medicine used with a live radioactive source. Obvious downside is the live radioactive source.
|
|
|
Dual X-ray Absorptiometry (DXA)
|
What we have now. Two energies of x-radiation (ie. x-ray but with filters).
No fine detail, but no live radioactive source and relatively inexpensive. |
|
|
Osteopenia
|
Bone density is lower than peak, but not low enough to be classified as osteoporosis. Often thought of as a precursor to osteoporosis.
- World Health Organization defines osteopenia as anything between 833 (normal BMD) and 648 mg/cm squared. |
|
|
Osteoporosis
|
Severe loss of bone mineral density that can lead to fragility and chance of fragility fractures.
- World Health Organization defines osteoporosis as anything below 648 mg/cm squared. |
|
|
Bone Structure
|
The outside cortical bone is solid bone with only a few small canals. The insides of the bone contain trabecular bone which is like scaffolding or a honey-comb. The spaces between the bone are filled with fluid bone marrow cells, which make the blood, and some fat cells.
|
|
|
Formation of Bone
|
OSTEOCLASTS are large cells that dissolve the bone. They come from the bone marrow and are related to white blood cells. They are formed from two or more cells that fuse together, so the osteoclasts usually have more than one nucleus. They are found on the surface of the bone mineral next to the dissolving bone.
OSTEOBLASTS are the cells that form new bone. They also come from the bone marrow and are related to structural cells. They have only one nucleus. Osteoblasts work in teams to build bone. They produce new bone called "osteoid" which is made of bone collagen and other protein. Then they control calcium and mineral deposition. They are found on the surface of the new bone. |
|
|
Once Osteoblasts have done their work....
|
When the team of osteoblasts has finished filling in a cavity, the cells become flat and look like pancakes. They line the surface of the bone. These old osteoblasts are also called LINING CELLS. They regulate passage of calcium into and out of the bone, and they respond to hormones by making special proteins that activate the osteoclasts.
OSTEOCYTES are cells inside the bone. They also come from osteoblasts. Some of the osteoblasts turn into osteocytes while the new bone is being formed, and the osteocytes then get surrounded by new bone. They are not isolated, however, because they send out long branches that connect to the other osteocytes. These cells can sense pressures or cracks in the bone and help to direct where osteoclasts will dissolve the bone. |
|
|
Prevalence of Low Bone Mass
|
34 Million People in America have Low Bone Mass and 10 Million People have Osteoporosis. 80% (8 million) are women, 20% (2 million) are men.
- 1 out of 2 women and 1 out of 8 men over age 50 will have an osteoporosis related fracture in their lifetime. |
|
|
Risk Factors for Developing Low Bone Mass
|
- Being female
- Aging - Thin and/or small frame - Family hx of osteoporosis - Post menopause - Abnormal/absent menses - Anorexia or Bulimia - Lifestyle - low calcium, high protein diet, sodium, phosphorus, cigarette smoking, caffeine, inactive lifestyle - Vitamin D Deficiency - use of certain meds - low testosterone in men - malabsorption issues - Being caucasian or asian - chronic diseases such as hyperthyroidism, hyperparathyrodism, multiple myeloma, rheumatoid arthritis, Hepatitis C - Prolonged parenteral nutrition |
|
|
Morbidity and Mortality of Low Bone Mass Diseases
|
- 24% of hip fracture patients over the age of 50 die in the year following
- hip fractures are 2-3X higher in women than men - 1/4 of ambulatory fractures lead to long-term care afterward - Cost of therapy, hospitals and nursing homes is estimated at 13.8 billion a year which is about 38 million each day. |
|
|
Levels of Osteoporosis
|
Normal: Bone mineral density(BMD) within 1.0 standard deviation of the average for young adult Osteopenia: BMD within 1.0 to 2.5 standard deviation below the average for young adult
Osteoporosis: BMD with more than 2.5 standard deviation below the average for young adult Severe osteoporosis: BMD with more than 2.5 standard deviation below the average for young adult and one fracture related to osteoporosis |
|
|
Categories of Osteoporosis
|
Osteoporosis is divided into two basic categories: primary and secondary. Primary osteoporosis occurs when bone loss is due to a problem within the bone itself, usually as the result of a disruption in the normal bone remodeling (removal) cycle. Secondary osteoporosis refers to diseases in other parts of the body that also cause bone loss. In this case the bone loss is secondary to some other disease.
|
|
|
Three Types of Primary Osteoporosis
|
- Type I: Postmenopausal osteoporosis (PMO)
- Type II: Age-related osteoporosis (sometimes called senile osteoporosis) - Type III: Idiopathic osteoporosis: adult and juvenile |
|
|
Type I Primary Osteoporosis
|
Postmenopausal osteoporosis (PMO):
Obviously this affects only women, because it is mainly associated with the loss of estrogen that occurs after menopause. It primarily affects the trabecular (porous, spongy) bone in the vertebrae and in the wrist, where much of the metabolically active trabecular bone is located. It is because of this type of bone loss that many postmenopausal women will have a spine or wrist fracture within five to ten years of their last menstrual period. |
|
|
Type II Primary Osteoporosis
|
Age-related osteoporosis (sometimes called senile osteoporosis):
This affects both men and women. It differs from postmenopausal osteoporosis in that bone loss occurs in the cortical areas of the skeleton as well as in the trabecular areas. Because of the loss in both types of bone, people with Type II osteoporosis also suffer fractures of the hip as well as the wrist and spine. In women, Type II osteoporosis usually shows up about ten years later than Type I, and it is thought to be caused by calcium and vitamin D deficiency as well as by the age-related changes associated with loss of estrogen and the malfunctioning of the remodeling process. |
|
|
Type III Primary Osteoporosis
|
Idiopathic osteoporosis: adult and juvenile:
The word "idiopathic" refers to a disease that arises spontaneously from an unknown or uncertain cause. It is a rare form of primary osteoporosis, and when it occurs in children it is usually around the time of puberty. Fortunately, it often resolves itself after puberty, and the young adult goes on to live a completely bone-healthy life. When idiopathic osteoporosis occurs in adults, the bones become fragile and break, just as they do in people with Type I and Type II osteoporosis. But with these patients, we simply don't know what has caused the disease. |
|
|
Secondary Osteoporosis
|
Secondary osteoporosis is either caused by medications or medical conditions that affect the calcium balance or the microarchitectural integrity of the bones. Fewer than 5% of people with osteoporosis have secondary osteoporosis.
|
|
|
Physics of DXA (DEXA)
|
Dual-Energy X-Ray Absorptiometry:
To quantitate BMD, it is necessary to eliminate soft tissue and measure what is attenuated by bone only. This is accomplished by scanning at two different photon energies and then subtracting out the soft tissue energies. You must have adequate soft tissue to ensure mathematically that you can determine the bone densities accurately. |
|
|
DXA Images
|
The bone density results are calculated from the x-ray attenuation pattern striking the detector, not the image. The images are used for positioning purposes only and cannot be used for diagnosis.
|
|
|
Prevention of Low Bone Mass
|
4 Steps to Prevention:
1. A balanced diet rich in calcium and Vitamin D to include foods and supplements if necessary 2. Weight bearing exercise 3. Healthy lifestyle - no alcohol or smoking 4. Bone density testing/medication appropriately |
|
|
Treatment of Osteoporosis
|
Is usually through medications, diet, and exercise and is also education on how to prevent falls.
|
|
|
Medications for Treating Osteoporosis
|
Medications to reduce resorption or increase formation:
ANTI-RESORPTIVE: - Biphosphonates - Calcitonin - Estrogens - Raloxifene INCREASE FORMATION: - Parathyroid Hormone OTHERS: - Tamoxifen - non-steroidal - Statins - cholesterol treatment |
|
|
Radiographer Accuracy and Precision
|
Important in DXA because the proper amount of soft tissue must be there to properly calculate BMD and there needs to be the proper positioning of bone (the neck for instance) and soft tissue for the machine to calculate properly.
|
|
|
Dose in Bone Densitometry
|
Doses for Bone Density:
- QCT - 60 mSv - DXA - 1-5 mSv - SXA - Less than 1 mSv - Ultrasound - 0 mSv COMPARISON - Daily Background Radiation - 5-8 mSv - Round trip flight across US - 60 mSv - Lateral Lumbar Spine - 700 mSv - PA Chest - 50 mSv |
|
|
Z- Score VS T-Score
|
Z Score is the # of standard deviations in BMD measurement from the population that is respective of the pt's current age, sex, weight, and race. "Z is me"
T Score is the # of standard deviations in BMD measurement from a young, normal, sex-matched, race-matched individual. Ie. compares to peak bone density. |
|
|
T-Score and Fracture Risk
|
Often used for Fracture Risk:
T-Score: - 0 to -1 SD is normal - -1 to -2.5 SD - Osteopenia - Anything beyond -2.5 SD is osteoporosis |
|
|
Z-Score and Fracture Risk
|
Used less often to determine Fracture Risk.
Z Score: - -1 SD or more would mean a great significance of increased fracture risk compared to peers - Each SD equates to 1.5 to 2.5X increased risk of fragility fracture. |
|
|
Average
|
The mean BMD established and recorded in reference population databases established.
|
|
|
Standard Deviation
|
Is the statistic that tells us how tightly all the various data points are clustered. Ie., a measure of data dispersion. 1 standard deviation is 67% of the data, 2 standard deviations is 95% of the data.
|
|
|
Calculating Standard Deviation
|
1. Find the mean by adding all numbers and dividing by the size of the group (ie. 9 numbers, then add them and divide by 9)
2. Calculate how each number differs from the mean (so, if the first number is 8 and the mean is 9.67, do 8 - 9.67 = -1.67). Do this for all numbers in the set always subtracting the mean. 3. Square each difference you got in step 2 (ie. -1.67 X -1.67 = 2.79). Do this for each number you got in step 2 and then add them all up. 4. Divide the sum you got in step 3 by N-1 where N is the number of values in the set (in this example 9 so you would divide by 8) THIS WILL GIVE YOU: How much each standard deviation is. |
|
|
Pre-Exam/Patient History
|
Scanning Information - is patient pregnant, are they physically able to have exam, have they had recent imaging that could interfere with the exam (such as contrast), fractures with fixations, any known medical conditions.
Patient Information - height, weight, medical hx, medications (especially things like vitamin D, C, etc...), risk factor assessment Past Exams/Labs - CBC, UA, TSH Insurance Information |
|
|
When to be Screened for BMD
|
Bone Mineral Measurement is done to determine whether a person has lost bone mass leading to osteopenia or osteoporosis. This allows us to assess fragility fracture risk.
Screening should be done on: - estrogen deficient women - people with vertebral abnormalities - people undergoing long-term steroid therapy - primary hyperparathyroidism - As response to therapy - should be done every two years in people at risk. * These recommendations are from the Medicare Bone Mass Measurement Coverage Standardization Act. There is no real consensus on what exactly should determine need for screening. |
|
|
Lumbar Spine Method of Bone Density Measurement
|
Spine is centered to sensors to include T12-L4 with equal soft tissue on each side.
- Crests should be included for landmarks - No artifacts should be on the image - Lines are moved to mark the intervertebral areas. |
|
|
Proximal Femur Method of Bone Density Measurement
|
These will predict future hip fractures:
Invert patient foot 15-30° and put the shaft parallel to the long axis of the table. This will give adequate space between ischium and femoral neck. The neck box should go over the femoral neck without getting any ischium in it. Last, no air can be present in the region of interest or it will create inaccurate readings. |
|
|
Quantitative Ultrasound of the Heel
|
QUS uses ultrasound waves laterally through the calcaneous. Measures the speed of sound giving a bone hardness or stiffness reading.
Advantages - less costly, portable, operated by anyone Disadvantages - Accurate, but not precise meaning it cannot be used for monitoring or exact measurements over time, doesn't account for density differences in weight bearing vs non-weigtht bearing, and anyone can operate them. |
|
|
BMC vs BMD
|
BMC - Bone Mineral Content
This is the measurement of bone mineral in the total area of the region of interest. BMD - Bone Mineral Density This is the measurement of bone mineral per unit area of a region of interest. BMD is most widely used because it reduces the effect of body size. |

