![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
Fractures
-what is the proper protocol to take when a patient comes into the clinic with a possible fracture? |
-Stabilize the patient
-physical exam -pain control -radiograph |
|
|
Radiographic imaging of a fracture is required in order to....
|
-detect the fracture
-describe the fracture -plan repair of the fracture -evaluate repair -monitor healing -look for complications |
|
|
How are fractures described?
|
-location
-type -complexity -potential complications |
|

Radiograph view
|
DMPLO
|
|

Radiograph view
|
DMPLO
|
|
|
What should you make sure to do when radiographing a fracture?
-why |
-include the cartilage proximal and distal to the fracture
-make sure that there isn't an articular fracture because the prognosis for them is much worse than a regular fracture |
|
|
What are reasons why a fracture would be missed on a radiographic exam, when it showed signs on a physical exam?
|
-poor radiographic technique
-superimposition -not tangential to beam -minimal to no displacement -early cortical stress fractures -physeal fractures (areas of normally lucent lines) |
|
|
What are different options when a fracture cannot be detected by radiograph?
|
-use additional views (different technique, oblique views, compare to the contralateral limb)
-Repeat the study in 1-2 wks -Bone scintigraphy -computed tomography -possibility that there is no fracture |
|
|
Why would a radiograph be repeated in 1-2 wks of the initial?
|
-radiolucent line becomes apparent in 7-10 days
early callous formation in 10-14 days |
|
|
What are some pitfalls to normal fracture detection?
|
-normal radiolucent lines
-superimposed gases (packing defects or gases from within soft tissues) |
|

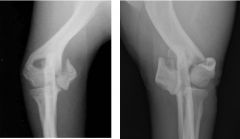
-which one is fractured?
-what kind of fracture is it? |
-left image
-avulsion fracture of the tibial tuberosity |
|
|
How to describe fracture location
|
-right/left
-fore/hind -bone fractured -location in the bone (diaphysis, metaphysis, epiphysis,....) |
|

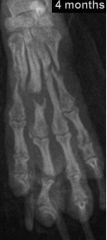
Describe the fracture location
|
-distal diaphysis of the right radius and ulna
|
|
|
How to describe the fracture type
|
-open v. closed
-simple v. comminuted -complete v. incomplete -traumatic v. pathologic -acute v. cronic |
|
|
How to describe fracture orientation
|
-transverse
-short/long oblique -spiral -segmental |
|

What is the fracture type?
|
-open fracture
|
|

What are the fractures types?
|
-left: simple
-right: comminuted |
|
|
Greenstick fracture
-definition |
-only one part of the cortical bone breaks, causing the other to bend
|
|

what type of fracture
|
-incomplete fracture (not through the caudal cortex of the tibia)
|
|

What is the main difference between these two fracture types?
|
-left: traumatic fracture
-right: pathologic fracture |
|
|
How can you tell if a fracture is pathologic?
|
-there is a loss in sharp margin
|
|
|
How can you tell if a fracture is acute or chronic?
|
-acute: sharp margins, well defined, no remodeling
-chronic: rounded margins, remodeling |
|

What is the orientation of this fracture?
|
-transverse
|
|

What is the orientation of this fracture?
|
-long oblique
|
|

What is the orientation of this fracture?
|
-short oblique
|
|

What is the orientation of the fracture?
|
-spiral (due to torsional trauma)
|
|

What type of fracture is this?
|
-segmental fracture (at least 2 breaks on the same bone)
|
|
|
What are different types of fracture alignment?
|
-displacement
-angulation -rotation |
|

Describe the fracture?
|
-comminuted fracture with caudal and medial displacement
|
|

Fracture alignment
|
-overriding cranially
|
|
|
How do you describe angulation in a fracture?
|
-name it according to the direction of the smallest angle between fragments
|
|

Describe
|
-caudal angulation
|
|

Describe alignment
|
-rotation
|
|

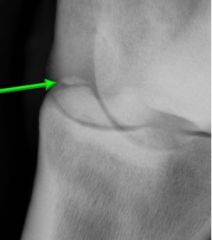
What is the red line pointing to?
|
-fissure
(this is a spiral fracture of the tibia) |
|
|
Why are fissures important?
|
-they can lead to additional damage when repair is attempted
|
|
|
How can you tell when there is soft tissue swelling?
|
-lack of visualization of the fascial planes
(always soft tissue swelling around fractures) |
|
|
Salter-Harris facture
-define |
-a fracture involving the open physis of a young animal
|
|
|
Salter-Harris Fracture
-Complications that it can cause |
-growth disturbance
-joint abnormalities |
|
|
Salter-Harris Fracture Types:
|
-Type I: complete physeal fracture
-Type II: physeal fracture extending through the metaphysis -Type III: physeal fracture extending through the epiphysis -Type IV: fracture of the physis, epiphysis, and metaphysis -Type V: compression fracture of the growth plate |
|
|
Which Salter-Harris fracture is most common?
|
-Type II
|
|

Fracture type
|
-Salter-Harris Fracture type II
|
|

Fracture type
|
-Salter-Harris Fracture Type III
|
|
|
What can result from a Salter-Harris Type V fracture?
|
-angular limb deformity
|
|
|
Avulsion fracture
-cause |
-excessive forces at the attachments of tendons/ligaments/joint capsule
|
|
Fracture Type
|
-chip fracture
|
|

Fracture type
|
-Slab fracture
|
|
|
How to differentiate a chip fracture from a slab fracture
|
Chip Fracture:
-monoarticular Slab fracture: -biarticular -usually a fracture of a cuboidal bone |
|

Fracture type
|
-depression fracture
|
|

Name these condylar fractures (left to right)
|
-lateral condylar fracture
-medial condylar fracture -"Y" Fracture -"T" Fracture |
|
Names these 2 fractures
|
-left: Salter-Harris Fracture Type IV
-right: Condylar "Y" fracture |
|

Name the fracture
|
-Monteggia fracture
-fracture of the proximal 1/3 of the tibia with a luxation of the radial head |
|
|
Types of bone healing
|
-direct
-indirect |
|
|
Most common type of bone healing
|
-Indirect
|
|
|
Indirect bone healing
-cause |
-lack of rigid fixation
|
|
|
Indirect bone healing
-pathogenesis |
-hematoma
-granulation tissue -fibrous connective tissue -fibrocartilage -bone |
|
|
Indirect bone healing
-phases (% of healing time) |
-inflammatory phase (10%)
-repair phase (40%) -Remodeling phase (70%) |
|
|
Tissues needed for bone healing (why)
|
-Periosteum (source of osteoprogenitor cells)
-soft tissues (blood supply) |
|
|
Factors affecting Callus size
|
-stability of the fracture
-fracture configuration -apposition of fracture fragments -vascular supply |
|
|
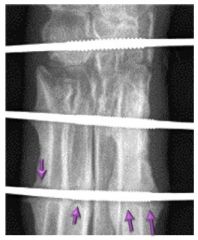
General radiographic timeline f normal indirect healing
|
-widening/decreased distinction of the fracture gap and fracture edges (5-7 days)
-appearance of a bony callus (10-12 days) -disappearance of the fracture line (within 30 days) -bridging cortices soon after -complete remodeling (smooth, opaque, well defined margins) of the callus (90 days after repair) |
|
|
Factors affecting the time required for fracture healing
|
-fracture configuration and location
-stability of repair -status of adjacent soft tissues -patient (age, species, health status) |
|
|
Direct bone healing
-occurs when |
-after rigid fixation results in absolute stability
|
|
|
Direct bone healing
-morphology |
-no callus formed
-difficult to detect radiographically |
|
|
Types of Direct healing
|
-gap healing
-contact healing |
|
|
Size of gap in gap healing
|
< .3 - .5 mm
|
|
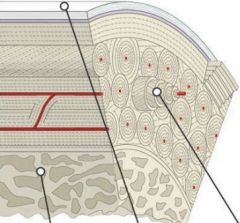
Bone Structure
-name the points |
-cancellous bone
-periosteum -haversian system (functional unit of compact bone) |
|
|
Cutting cone
-process |
-osteoclasts remove old bone
-blood vessel (central vessel) moves in -osteoblasts form osteocytes |
|
|
Factors that can affect bone healing
|
-patient age and breed
-type of fracture -location of fracture -quality of anatomic reduction -stability of repair -vascularity -infection -systemic disease |
|
|
Post-operative imaging
-when to take images |
-after surgery
-4-6 weeks or when needed clinically -repeat until healed |
|
|
ABCDs of Radiographic Evaluation
|
-Alignment/Apposition: fracture ends must have 50% contact; change could indicate instability
-Bone: progression of healing; evidence of complications -Cartilage: evaluation of joints involved in a articular fracture -Device: stable, loosening, bending, breakage, infection -Soft tissue: swelling, mineralization, increased synovial mass |
|
|
How to confirm radiographic union
|
-bone continuity at 4 cortices (2 views)
-complete calcified and ossified bridging callus -no remaining visible fracture line |
|
|
Complications associated with fracture healing
|
-mal-union
-delayed union -non-union -infection -sequestrum formation -disuse osteopenia -joint complications -angular limb deformity -implant failure |
|
|
Malunion
-definition |
-a healed fracture with abnormal anatomical alignment
|
|
|
Malunion
-due to |
-poor initial reduction
-shifting of fragments post reduction -premature removal of fixation device |
|
|
Malunion
-effect |
-may result in lameness
|
|
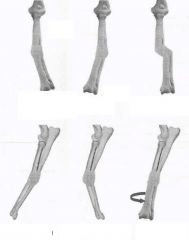
Malunion classifications
-top left to bottom right |
name by direction of distal part of bone
-valgus (lateral) -Varus (medial) -translational -recurvatum (cranial) -antecurvatum (caudal) -torsional |
|
|
Delayed healing
-outcomes |
-should eventually heal if it is stable and there are no complications
-may be a nonunion if it is poorly vascularized and there is a lot of motion |
|
|
Non-union
-how to determine |
-lack of callus progression
-remodeling of the callus at fracture ends with no bridging |
|
|
Main reasons for non-union
|
-excessive motion
-compromised blood supply Others: -distraction of fracture fragments -infection -age, breed, metabolic state,... |
|
|
Nonunion
-types |
-viable (hypertrophic)
-nonviable (atrophic) |
|
|
Viable nonunion
-morphology |
-vascular supply present
-fracture margins are viable |
|
|
Nonviable nonunion
-morphology |
-minimal to no vascular supply
-non-viable fracture margins |
|
|
Hypertrophic nonunion
-definition |
-large callus at the fracture ends with a persistent radiolucent gap
|
|
|
Hypertrophic nonunion
-cause |
-vascularity is present but motion is excessive
|
|
What is this?
|
-atrophic nonunion
|
|
|
Atrophic nonunion
-morphology |
-no callus
-increased fracture gap -Tapered fracture margins |
|

What is this?
|
-osteomyelitis
|
|
|
Osteomyelitis
-causes |
-bone infection
-contamination (open fracture, extended surgery, severe soft tissue damage, foreign object) |
|
|
Osteomyelitis
-radiographic findings |
-periosteal reaction with or without lysis
-indistinct periosteal proliferation -can be confused with a callus (but rougher in appearance) |
|
|
Clinical signs associated with osteomyelitis
|
-pain
-heat -swelling |
|
What is this?
|
-lucency at implants
|
|
|
What can cause lucency at implants?
|
-infection/osteomylitis
-motion -heat necrosis -migration |
|
|
Implant migration
-cause |
-infection
-motion |
|

What is this
|
-sequestrum
|
|
|
Sequestrum
-define |
-fragment of bone that is no longer viable
|
|
|
Sequestrum
-radiographic findings |
-surrounded by pus and granulation tissue
-sclerotic involucrum forms around the pus -draining tract (cloaca) may be present |
|
|
Disuse osteopenia
-radiographic findings |
-thin cortices
-coarse trabeculation -more apparent distal to the fracture |
|
|
Demineralization seen in disuse osteopenia may be due to:
|
-chronic disuse
-limb immobilization -stress protection from orthopedic implants |
|

What is this
|
-disuse osteopenia
|
|
|
Disuse osteopenia
-sequela |
-pathologic fracture
|
|
|
Joint complications from fractures
|
-articular fracture
-(sub) luxation -angular limb deformity -intra-articular implant -septic arthritis |
|

What is this
|
angular limb deformity
|
|
|
Angular limb deformity
-can be due to |
-malunion
-Salter-Harris fracture Type V |
|
|
Angular limb deformity
-most common cause |
-premature closure of the distal ulnar physis
|
|

What is this?
|
septic arthritis
|
|

What is this?
|
Implant failure
|
|
|
Implant failure
-causes |
-broken implant
-bending of implant -loosening of implant -migration |

