![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Linitis Plastica
|

Stomach with leather bottle appearance
Usually adenocarcinoma with submusocal infiltration Radiographic features Barium meal Due to the increased rigidity of the wall, the stomach cannot be adequately distended Narrow lumen seen normal mucosal fold pattern is absent, either distorted, thickened or nodular CT Typically the stomach is diffusely thickened with a small lumen. Evidence of nodal involvement or wide spread metastatic disease should also be sought. Ddx • neoplastic (gastric adenoCA, metastases from tit,lung,lymphoma) • diffuse gastric diverticula (rare) • inflammatory o radiotherapy o eosinophilic enteritis o granulomatous disease Crohn's disease tuberculosis • scarring (e.g. ingestion of corrosives) • gastric amyloidosis |
|
|
Achalasia
|
Achalasia
failure of organized peristalsis with impaired relaxation at the level of LES giving marked dilatation of the oesophagus and food stasis. Present with dysphagia, chest pain / discomfort and eventual regurgitation. Initially symptoms are intermittent. CXR Chest x-ray findings include : right convex opacity behind right cardiac border; occasionally left convex opacity if thoracic aorta tortuous air-fluid level due to stasis in thoracic oesophagus filled with retained secretions and food small / absent gastric air bubble anterior displacement and bowing of trachea on the lateral view The chronic presence of fluid debris in the oesophagus makes patients very prone to aspiration and thus patchy bilateral alveolar opacities representing acute or chronic aspiration pneumonia may be seen. Barium failure of normal peristalsis to clear the oesophagus of barium when the patient is in the recumbent position, with no primary waves identified uncoordinated, non-propulsive, tertiary contractions oesophageal body dilatation, which is typically maximal in the distal esophagus pooling or stasis of barium in the oesophagus when the oesophagus has become atonic or non contractile (late feature in the disease) when barium column is high enough (patient standing) the hydrostatic pressure can overcome the LOS pressure allowing passage of oesophageal content incomplete LOS relaxation that is not coordinated with oesophageal contraction bird beak sign Differential diagnoses achalasia : distal segment of narrowing is less than 3.5 cm central and peripheral neuropathy scleroderma oesophageal malignancy oesophageal stricture |
|
|
Gastric Lymphoma
|
•
TERMINOLOGY Definitions • Gastric metastases from primary cancer • Lymphoma: Malignant gastric tumor of B lymphocytes IMAGING Fluoroscopic Findings o Malignant melanoma metastases Solitary/multiple discrete submucosal masses "Bull's-eye" or "target" lesions: Centrally ulcerated submucosal masses "Spoke-wheel" pattern: Radiating superficial fissures from central ulcer Giant cavitated lesion: Large collection of barium (5-15 cm) communicating with lumen Small or large lobulated masses Mucosal nodularity, spiculation, ulceration o Esophageal squamous cell metastasis Large submucosal masses, central ulceration o Esophageal adenocarcinoma (from Barrett mucosa) Large polypoid/ulcerated mass in gastric fundus Subtle findings of cardia: Small ulcers & nodules CT Findings • Demonstration of lesions facilitated by negative contrast agents (water, gas) • Hematogenous spread of metastases to stomach o Linitis Plastica differential Markedly thickened gastric wall with enhancement, folds preserved, seen in proximal stomach; antrum spared Mimics primary scirrhous carcinoma of stomach • Lymphatic spread of metastases to stomach o Esophageal Ca: Growth in gastric cardia or fundus o Multiple, well-defined, ↓ HU enlarged nodes Characteristic of squamous cell metastases • Direct invasion of stomach o Distal esophageal adenocarcinoma: Barrett mucosa Polypoid, lobulated mass in gastric fundus Indistinguishable from primary gastric carcinoma Ultrasonographic Findings • Grayscale ultrasound o Endoscopic ultrasonography (EUS) Hypoechoic mass disrupting normal wall layers Selective/diffusely thickened echogenic wall layers |
|
|
Esophageal Diverticula
|

|
|
|
Esophageal Filling Defects
|

|
|
|
Esophageal Narrowings
|

|
|
|
Esophageal Strictures
|
|
|
|
Biliary Duct Dilatation
|
|
|
|
Bosniak Criteria
|
|
|
|
Renal Cyst Imaging Features
|
|
|
|
DDX pneumatosis
|
• Pneumatosis is a radiographic finding, not a disease process
o Must correlate with patient history, clinical signs & symptoms to determine its significance Check WBC, lactate, amylase DDx Ischemic Enteritis & Colitis & SBO • Spherical or linear collections of gas in submucosa of affected bowel • Often associated with portal venous gas; SB ischemia usually due to occlusion of SMA or SMV o Colonic ischemia more often due to hypoperfusion; not thrombotic Iatrogenic (Post-Operative or Endoscopy) • Bowel-to-bowel anastomosis. G/J tubes – air to leak from lumen into wall; asymptomatic Drugs (Steroids, Chemo) Pseudopneumatosis (Mimic) • Gas may be trapped against the inner wall of bowel, simulating pneumatosis • Very common in cecum, ascending colon • Lung (Asthma, COPD, pulmonary fibrosis, cystic fibrosis, ventilator) Collagen Vascular Disease • Any "collagen vascular disease" may cause pneumatosis • Intramural gas may result from the bowel disease itself, associated medications (e.g., corticosteroids), or ischemia o Must correlate with clinical & laboratory evidence of disease exacerbation or ischemia Necrotizing Enterocolitis • Common cause of pneumatosis in neonates Pneumatosis Cystoides Intestinalis (like bullae in colon wall) Intestinal Trauma • Serosa of bowel may be avulsed ("degloving injury") • Leads to devascularization & ischemia of bowel Small Bowel Transplantation Inflammatory Bowel Disease • Crohn disease, ulcerative colitis, others • Any disease that causes ulceration of bowel mucosa can cause pneumatosis • Patients are often on steroid medications that may also cause pneumatosis Graft vs. Host Disease • Bone marrow transplant recipients • Clinical triad: Damage to gut, skin, liver • Pneumatosis does not necessarily indicate ischemia o Patients are receiving medications (steroids, immunosuppression) associated with "benign pneumatosis" |
|
|
Cystic Pancreatic Mass
|
Pancreatic Pseudocyst
Pancreatic abscess Neoplastic (Mucinous cystic pancreatic neoplasm, IPMT, pancreatic ductal CA) AD poly cystic kidney VHL Mimics ie Ascites, Duo Tic |
|
|
Adrenal Mass
|
Adenoma (lipid rich,fast washout)
Mets (next most common) 1' Adrenal Cortical CA Adrenal Myelipoma Pheo Hemorrhage Cyst |
|
|
Carcinoid
|
Imaging
Most common primary small bowel tumor beyond ligament of Treitz Appendix > ileum > duodenum > other sites |
|
|
Carcinoid DDx
|
DDX
Sclerosing mesenteritis Infiltrated jejunal mesentery Intestinal metastases and lymphoma Desmoid Mesenteric and small bowel trauma Small bowel carcinoma |
|
|
Carcinoid Findings
|
IMAGING
General Features • Best diagnostic clue: Solitary, well-/ill-defined, enhancing distal ileal mass with mesenteric metastases • Location: Appendix > ileum > duodenum > other sites • Size: Varies from < 1 cm to a few cm • Other general features CT Findings • Submucosal tumors o Solitary or multiple, well-defined enhancing lesion o Better visualization of enhancing mural mass with enteric water as contrast agent o More difficult to detect primary than metastatic foci o Ill-defined, heterogeneous mesenteric mass o Calcification within mesenteric mass (up to 70%) o Occasionally tumor may be of cystic density o Tumor may show spiculation with stellate pattern o ± tethering, fixation, retraction of small bowel loops Due to mesenteric fibrosis and desmoplastic reaction Desmoplastic reaction: Finger-like projections of mass into adjacent mesentery o ± encasement and narrowing of mesenteric vessels • Hypervascular Liver metastases |
|
|
Ddx Pneumoperitoneum
|
Duodenal Ulcer (intra and extraperitoneal is possible)
Gastric Ulcer Diverticulitis (few locules near sigmoid is usual) Intestinal Trauma Iatrogenic Bowel Anastomotic Leak Thoracic pathology may mimic or cause pneumoperitoneum (PTX, Atelectasis, Cystic lung disease) |
|
|
SBO causes
|
CT Findings
Dilated SB loops > 2.5 cm ± air-fluid levels Causes: 1. Extrinsic lesions: Adhesions, Hernia, Peritoneal carcinomatosis, Appendicitis 2. Intrinsic lesions: Adenocarcinoma, Crohn disease, tuberculosis, radiation enteropathy 3. Intraluminal lesions: Gallstones, foreign bodies, bezoars, Ascaris worms |
|
|
Delayed Nephrogram
|
Obstruction of UPJ (calculi, tumour, TCC, RCC, Mets, 1’ bowel or pelvic malignancy, trauma)
Vascular Cause (Renal artery stenosis, vein thrombosis/stenosis) ATN, CIN Shock Pyelonephritis |
|
|
Striated Nephrogram
|
Renal Trauma
Infarct MSK Acute ureteral obstruction Vasculitis M/M Rhabdomyolysis RCC, Mets, Lymphoma |
|
|
Cystic Peritoneal Mass
|
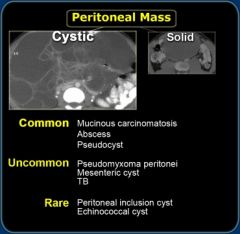
|
|
|
Solid Peritoneal Mass
|
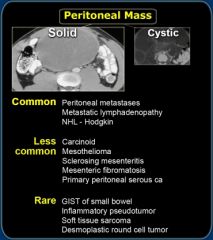
|
|
|
Liver lesions w/ a scar
|
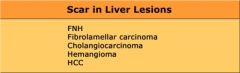
|
|
|
Hemangioma on CT
|
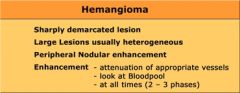
|
|
|
HCC Features on CT
|
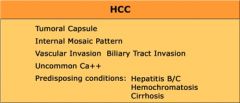
|
|
|
FNH Features on CT
|
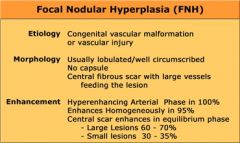
|
|
|
Cystic Hepatic Mass
|
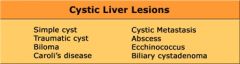
|
|
|
CholangioCA Features
|
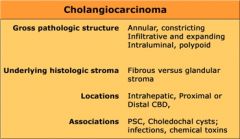
|
|
|
Characterization of Liver Masses
|
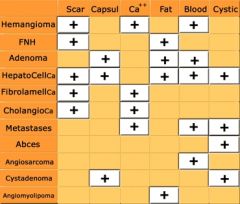
|
|
|
approach to hypervascular mass
|
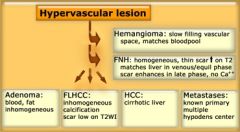
|

