![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
99 Cards in this Set
- Front
- Back
|
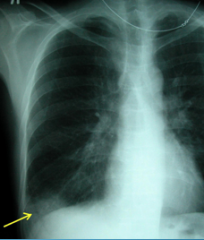
what is a pleural effusion |
Abnormalcollection of fluid in the pleural space |
|
|
classified as a sign of disease but not a disease by itself |
pleural effusion |
|
|
Increasedproduction due to increased hydrostatic or decreased oncotic pressures |
transudate |
|
|
Increasedproduction due to abnormal capillary permeability |
exudate |
|
|
Decreasedlymphatic clearance |
exudate |
|
|
direct infection of the pleural space that is grossly purulent/turbulent |
empyema |
|
|
bleeding into the pleural space |
hemothorax |
|
|
caused by high cholesterol |
chyloform |
|
|
pleural effusions are exudates thataccompany bacterial pneumonias |
Parapneumonic |
|
|
abnormal accumulation of circulatory system fluid results in what |
transudate |
|
|
this accumulation is can be due to what two things |
1. increased hydrostatic pressure 2. decreased oncotic pressure (colloid osmotic pressure) |
|
|
most common cause of transudate |
CHF |
|
|
other causes of transudate |
1. nephrotic syndrome 2. cirrhosis 3. atelectasis |
|
|
what occurs when local factors increase vascular permeability |
exudate |
|
|
the light's criteria are exclusive to what |
exudates |
|
|
what is the light's criteria |
1.Pleural fluid protein/serum protein >0.5 2.Pleural fluid LDH/serum LDH >0.6 or Pleural fluid LDH more than two-thirds normal upper limit for serum |
|
|
5 leading causes of pleural effusions in the US |
1. CHF 2. Pneumonia 3. Cancer 4. pulmonary embolus 5. viral disease |
|
|
of the previous 5, which one can sometimes be either a transudate or an exudate |
pulmonary embolus |
|
|
signs and symptoms of pleural effusion |
dyspnea cough pleuritic chest pain |
|
|
small effusions are normally what |
asymptomatic and have no findings on physical exam |
|
|
physical exam findings of pleural effusions |
1. dullness to percusion 2. decreased breath sounds 3. audible plueral friction rub 4. Egophony 5. bronchial breath sounds |
|
|
what can occur in massive pleural effusions |
lung collapse mediastinal shift to contralateral side |
|
|
lab tests are order depending on what |
the appearance of the pleural fluid |
|
|
what is ordered for bloody fluid |
hematocrit |
|
|
what is ordered for cloudy or turbid fluid |
centrifugation |
|
|
what is ordered for purid odor |
stain and culture could be possible aerobic infection |
|
|
Tovisualize fluid on a standardupright CXR, you need at leasthow much fluid |
75 to 100 CC's |
|

|
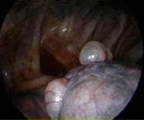
pleural effusion on CT |
|
|
what view is the best choice for detecting smaller effusions, and differentiating loculations & empyema from new effusions or scarring |
lateral decubitus |
|
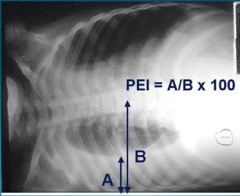
Pleural Effusion index. How is PEI calculated? |
100times the maximum width of the right pleural effusion, divided by the maximalwidth of the hemithorax of the affected side |
|
|
treatment for transudate pleural effusions |
treat underlying condition |
|
|
what is the gold standard treatment for pleural effusions |
thoracentesis |
|
|
pleural fluid must be drain in what case |
empyema |
|
|
lab findings for empyema |
1. pleural fluid PH under 7.2 2. glucose under 40 mg 3. positive gram |
|
|
accumulation of air within the pleural space |
pneumothorax |
|
|
pneumothorax can be either what |
spontaneous or traumatic |
|
|
two types of spontaneous pneumo's |
primary and secondary |
|
|
secondary occurs________. |
as aresult of a complication of preexisting lung disease |
|
|
population group for primary pneumo's |
tall, thin med 20-40 smokers family history |
|
|
can pneumo's be iatrogenic |
yes caused by thoracic needle aspirations, baro trauma, thoracentesis or lung biopsy, or subclavian catheter placement |
|
|
primarny spontaneous is also thought be be a rupture of what |
small blebs |
|
|
clinical manifestations of pneumo's |
unilateral pleuritic chest pain dyspnea palpitations |
|
|
signs can present as_______. |
Respiratorydistress Tachycardia Tachypnea |
|
|
test of choice for pneumo |
CXR |
|
|
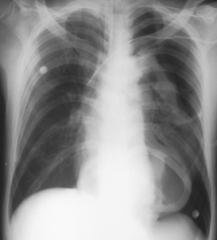
Left side pneumo |
|
|
life threatening pneumo where positive air pressure pushes lungs, trachea, and heart to the contralateral side |

tension |
|
|
what treatment might be required for large pneumo's |

chest tube water seal |
|
|
30% of which type of pneumo has recurrence |
spontaneous |
|
|
pulmonaryhypertension with elevated pulmonary vascular resistance |
pulmonary hypertension |
|
|
it affects what population |
middle age or young women |
|
|
it may present sometimes as what |
Right-side heart failure |
|
|
main cause of secondary pulmonary HTN |
COPD |
|
|
how is pulmonary HTN medically treated |
vasodilators oxygen therapy anticoagulation |
|

|
pulmonary hypertension |
|
|
what is Cor Pulmonale |
RightVentricular hypertrophy |
|
|
it is failure from what |
pulmonary disease |
|
|
most common cause of Cor Pulmonale |
COPD |
|
|
symptoms of Cor Pulmonale |
1. chronicproductive cough 2. exertionaldyspnea 3. wheezingrespirations 4. fatigability 5. weakness |
|
|
signs of Cor Pulmonale |
1. Cyanosis 2. Clubbing 3. Distendedneck veins 4. RVheave or gallop 5. Hepatomegalywith tenderness 6. Dependentedema |
|
|
testing for Cor Pulmonale |
EKG |
|
|
RV function is tested how |
Echocardiogram |
|
|
treatment for Cor Pulmonale |
Treatmentis directed at the underlying pulmonary cause. |
|
|
thrombus in pulmonary artery or branches |
pulmonary embolism (PE) |
|
|
Thirdleading cause of death in hospitalized patients |
PE |
|
|
most common embolus |
thrombus |
|
|
why do thrombi in the leg rarely cause PE's |
because only a small portion of them get above the popliteal or ileofemoral region |
|
|
most patients with PE's will also have what |
DVT |
|
|
classic triad of clinical manifestations for PE's |
1. Dyspnea 2. Pleuritic chest pain 3. Hemoptysis |
|
|
most common symptom of PE |
Tachypnea |
|
|
other signs and symptoms |
Seizures Syncope Abdominalpain Fever Productivecough Wheezing Decreasinglevel of consciousness Newonset of atrial fibrillation |
|
|
70% of patients will have what abnormality on EKG |
Sinustachycardia |
|
|
testing for PE |
arterial blood gases CXR positive d-dimer (high sensitivity, low specificity) |
|
|
arterial blood gas will show what |
respiratory alkalosis |
|
|
what CXR finding is suspicious for PE |
Profoundhypoxia in the setting of normal |
|
|
avascular markings distal to area of embolus |
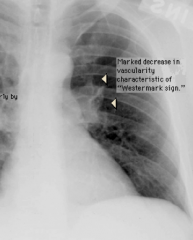
Westermark Sign |
|
|
pleuralbase of increasedmarking. |
hampton's hump |
|
|
what does hampton's hump finding represent |
interparenchymalhemorrhage |
|
|
initial screening and test of choice for PE |
helical CT |
|
|
how is a V/Q scan helpful |
low probability only rules out PE in patients with low clinical suspicion |
|

|
PE CT scan shows a pulmonary embolus within the posterobasal segment of the right lower lobe artery. The artery is enlarged compared with adjacent patent vessels |
|
|
gold standard test for detecting PE |
PulmonaryArteriography |
|
|
test good for detecting proximalextremity thrombosis |
venous ultrasound |
|
|
treatment for PE |
anticoagulation heparin and warfarin (coumadin) |
|
|
heparin treatment |
load80units/kg IV, then maintenance infusion of 18 units/kg/hr Maintain aPTT of1.5-2.5 times normal. Adjustdose based on repeat aPTTvalues. |
|
|
what happens if you don't achieve adequate coagulation level in the first 24 hours |
increases risk 5 fold |
|
|
what does aPTT stand for |
activated partial thromboplastin time |
|
|
which type of heparin has a longer plasma half life |
LowMolecular Weight Heparin |
|
|
how is it administered |
subcutaneously |
|
|
warfarin treatment |
Oraltherapy continued for at least 3 months after PE Startin the hospital with heparin Takesup to 7 days to get to therapeutic state Initialdose stated from 2.5-10mg daily |
|
|
target international normalized ration (INR) |
2.5 |
|
|
INR above what increases risk of bleeding |
4 |
|
|
is warfarin safe to use in pregnancy |
no, category x |
|
|
what doe you use instead |
LMWH |
|
|
risk involved with prolonged therapy for PE |
hemorrhage |
|
|
what PE therapy mustuse in the first 24 hours to be effective |
ThrombolyticTherapy |
|
|
types of thrombolytic therapy |
Streptokinase Urokinase recombinant tissue plasminogen activator |
|
|
Absolutecontraindications for PE therapy |
strokein past 2 months active internal bleeding |
|
|
major contraindications |
uncontrolledHTNsurgery or trauma in last 6 weeks |
|
|
possible treatment for high risk patients |
IVC filter |

