![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back

|
-Normal lungs
-Normal has a big spectrum as these lungs have wear and tear to them |
|
|
Describe the airways of the conducting zone
|
-Trachea
-Bronchi - ciliated and goblet cells, elastic tissue, smooth muscle glands, cartilage -Bronchioles- No cartilage or bronchial glands, ciliated lining, no goblet cells, smooth muscle - The conducting zone protects the gas exchange zone of the lung. The mucociliary elevator traps particles in mucus and clears it out. |
|
|
Describe the cell types of the conducting zone
|
Ciliated cells - Beating of cilia contribute to mucociliary elevator
Goblet cells - mucus secretion Basal cell - Reserve cell Kulchitsky cell - Neuroendocrine cells |
|
|
Describe the branching of the lungs
|
-The trachea breaks into two main stem bronchi
-Then lobar bronchi (5 lobes) -Then segmental bronchi (10 bronchopulmonary segments on right, 9 on left) -Branching continues as airways become bronchioles, then at terminal bronchioles airways transition into respiratory bronchioles -About 20 branch generations from beginning to end -The airways become bronchioles when they no longer have cartilage. The respiratory bronchiole is the beginning of the gas exchange part of the lung. |
|
|
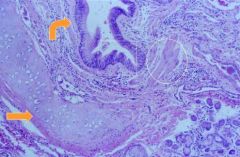
-Normal airway
-The epithelium is pseudostratified ciliated. We often call this respiratory epithelium. -Below the epithelium is the lamina propria. There is cartilage and smooth muscle. -The top arrow points to basement membrane. There is also smooth muscle. |
|
|
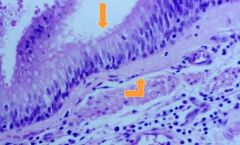
-Normal lung
-There are tall columnar cells. They have a prominent terminal bar and have cilia at the end. -They are sitting on the basement membrane and all the cells touch the basement membrane. -The reserve cells are the likely source of new ciliated cells. -Goblet cells are some of the mucus secreting cells. |
|
|
-This is an example of a chronic airway disease. This is how airways response to chronic injury.
-There are glands underneath the epithelium in the submucosal zone. -Those produce some of the watery and mucoid part of the secretion. -Those are called bronchial glands and they have ducts that go into the lumen. -There are normally very of these glands. -This specimen is full of them, so that is an abnormality of the airway that is seen in chronic bronchitis. -There are many goblet cells as well (another abnormality). |
|
|
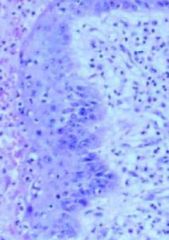
-Squamous metaplasia
-With chronic airway injury the epithelial will no longer look pseudostratified ciliated. It will eventually look stratified squamous. -It doenst have any cilia beating. When you have this much metaplasia there is no longer as much function in terms of mucociliary elevator. -This will lead to mucus accumulation, causing dilitation of the airway. -Bacteria can accumulate and lead to infection and more injury. This can become a chronic and even irreversible process. |
|
|
-Squamous metaplasia
-With chronic airway injury the epithelial will no longer look pseudostratified ciliated. It will eventually look stratified squamous. -It doenst have any cilia beating. When you have this much metaplasia there is no longer as much function in terms of mucociliary elevator. -This will lead to mucus accumulation, causing dilitation of the airway. -Bacteria can accumulate and lead to infection and more injury. This can become a chronic and even irreversible process. |
|
|
Describe the airway respiratory zone
|
Respiratory bronchiole - lined by ciliated cells and Clara cells
Alveolar ducts/sacs -Type I cells - 90% of alveolar surface -Type II cells |
|
|
Describe the cell types of the airway respiratory zone
|
Clara cells - Produce a component of surfactant and are the bronchiolar reserve cells. Clara cells are the reserve cell for this part of the airway. They function in detoxification and in terms of antioxidant and antibacterial secretions.
Type I cells - Thin lining cell for gas exchange Type II cells - Surfactant and alveolar reserve cell |
|
|
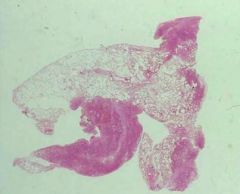
-Organizing pneumonia
-This is a lung section showing regions of alveoli, airways, and vessels. -There is an abnormality here in that the alveoli are filled with fibroblastic plugs. -This zone is probably supplied by 2-3 terminal bronchioles. If you have a disease that affects those 2-3 terminal bronchioles only it will be manifested in a lobular architecture like this histologically. |
|
|
-The terminal bronchiole-respiratory bronchiole transition occurs over a very small distance.
-There are ciliated epithelial cells at one end with smooth muscle which is consistent with a bronchiole of the conducting type. -In the central zone we lose those ciliated epithelial cells. -Instead more cells are cuboidal and are the clara cells. |
|
|
-The terminal bronchiole-respiratory bronchiole transition occurs over a very small distance.
-There are ciliated epithelial cells at one end with smooth muscle which is consistent with a bronchiole of the conducting type. -In the central zone we lose those ciliated epithelial cells. -Instead more cells are cuboidal and are the clara cells. |
|
|
-The distal part/respiratory bronchiole
-Lined by clara cells opens up into the alveolar ducts and alveolar sacs. |
|
|
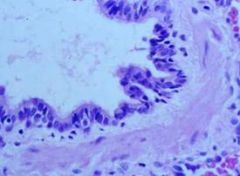
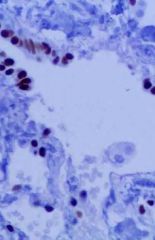
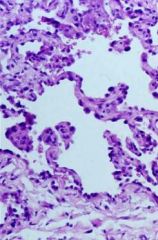
-Alveolar sac
-We see flat cells which are type I pneumocytes which minimize the distance of diffusion for gases. -They are thin and closely apposed to an endothelial cell. -The occasional more prominent cell that is seen are the type II pneumocytes. -The alveolar membrane is structured to be a thin diffusion surface that allows no more than a RBC to pass throughit to allow the gasses in the alveolar space to enter the circulation and gasses that are in the circulation to get into the alveolar space for expiration. -Any thickening of that membrane will cause a problem with diffusion. -The type II pneumocytes are the regenerative cell. |
|
|
-Alveolar sac
-We see flat cells which are type I pneumocytes which minimize the distance of diffusion for gases. -They are thin and closely apposed to an endothelial cell. -The occasional more prominent cell that is seen are the type II pneumocytes. -The alveolar membrane is structured to be a thin diffusion surface that allows no more than a RBC to pass throughit to allow the gasses in the alveolar space to enter the circulation and gasses that are in the circulation to get into the alveolar space for expiration. -Any thickening of that membrane will cause a problem with diffusion. -The type II pneumocytes are the regenerative cell. |
|
|
-Normal alveoli
|
|
|
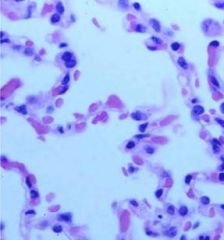
-Abnormal alveoli
-On the right virtually every other cell is a type II cell. This is an injury. -The type I cells have been injured and the regenerative cell has proliferated to line the alveolar space. -This is diffuse alveolar damage. |
|
|
Describe the pulmonary vessels
|
-Arteries/arterioles - Travel and divide with bronchi and bronchioles
-Produce capillary bed in alveoli for gas exchange -Venules collect capillary blood into lobular septa, forming veins and joining at the hilum |
|
|
Describe bronchial vessels
|
-Artery from aorta
-Supplies bronchial tree up to respiratory bronchiole -Venous drainage to azygous/hemiazygous |
|
|
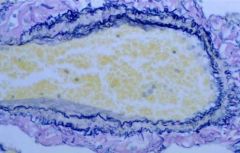
This is an artery with internal and external elastic lamina. There is a normal intima, media, and adventicia.
|
|
|
Here is a normal vein. The veins are in the interlobular septal structures in the lung. They have a thin wall and lack to complex elastic structure.
|
|

|
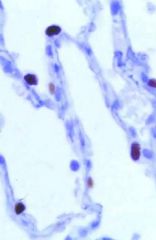
-The lymphatics of the lung are responsible for draining fluid out of the lung, into the thoracic duct, and back into the circulation.
-In this case the lymphatics have been highlighted because there is cancer that has been spread through the lymphatics. -The lymphatics run along interlobular septal structures. |
|
|
-Normal pleura
-As we breathe and expand the lung there needs to be a layer around the last alveolus. The fibroelastic tissue prevents the air from leaving the lung. The lining of that are mesothelial cells. Hyperexpansion is prevented by this layer. The pleura should be very thin. |
|

|
-Abnormal pleura
-This pleura where we can see a white thickening that is almost 2-3 mm is abnormal. This is pleural fibrosis from a patient that was exposed to asbestos. |
|
|
What are the diseases of the conducting airways?
|
-Asthma
-Chronic bronchitis -Bronchiectasis |
|
|
Describe bronchiectasis
|
-Not a single disease, but a manifestation of injury
-Permanent dilation of bronchi and bronchioles, due to destruction of elastic tissue and muscle -Normally what keeps airway tone is a combination of muscle and elastic tissue. If you stretch the airway out it will go back to its origianl shape due to the elastic tissue. In bronchiectasis through chronic injury of the airway wall both the muscle and the elastic tissue become abnormal. -The dilated bronchi are more prominent in the lower lobes. Once there is injury to the airway wall instead of regenerating normally you just develop scar tissue. |
|
|
Describe the causes bronchiectasis
|
-Dilatation of bronchi and bronchioles, usually due to necrosis of wall and obstruction
-Foreign body -Mucoid impaction -Aspergillus -Cystic fibrosis -Immotile cilia -Chronic bronchitis and infection |
|
|
Describe the pathology of bronchiectasis
|
Gross pathology: Dilated bronchi, filled with mucus or pus, lower lobes
Microscopic: Can have acute and chronic inflammation, varying degrees of fibrosis |
|
|
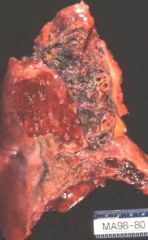
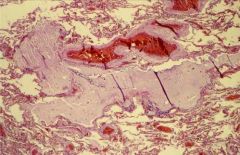
-Bronchiectasis
-These are very dilated bronchi. -They have mucus in them, This is an end stage of the process. -As that airway which supports a section of lung is chronically filled with mucus and chronically getting infected the lung distal to that airway will not function properly and be more prone to infection. -The repeated lung infections lead to lung injury and replacement of scar. -The tan tissue is all fibrous tissue. -This starts as an airway disease and through time you lose lung function. |
|

|
-Bronchiectasis
-These are very dilated bronchi. -They have mucus in them, This is an end stage of the process. -As that airway which supports a section of lung is chronically filled with mucus and chronically getting infected the lung distal to that airway will not function properly and be more prone to infection. -The repeated lung infections lead to lung injury and replacement of scar. -The tan tissue is all fibrous tissue. -This starts as an airway disease and through time you lose lung function. |
|

|
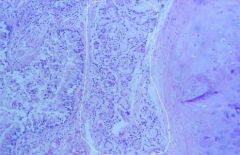
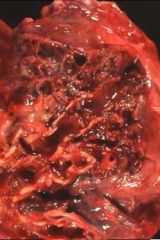
-Bronchiectasis
-We can see marked dilatation of the large airways. The alveolar spaces around them due to repeated injury have been lost. -You shouldn’t be able to see airways this far out. -They are noncontracting. When air goes in them there is no elastic return. -It will fill with mucus and that mucus is prone to infection. |
|
|
-Bronchiectasis
-We can see marked dilatation of the large airways. The alveolar spaces around them due to repeated injury have been lost. -You shouldn’t be able to see airways this far out. -They are noncontracting. When air goes in them there is no elastic return. -It will fill with mucus and that mucus is prone to infection. |
|
|
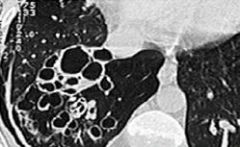
In a CT scan of a bronchiectatic lung you can see the large dilated spaces.
|
|
|
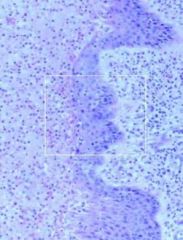
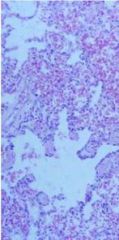
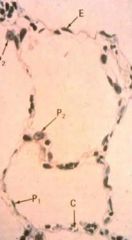
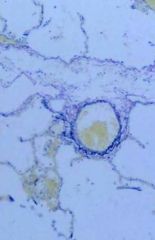
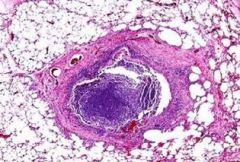
-Bronchiectasis
-The histologic correlate is dilitation of the bronchiole. -The bronchiole and the vessel should be about the same size. -The bronchiole here dwarfs the vessel. -The lumen is blue because it is full of neutrophils. This is pus. |
|
|
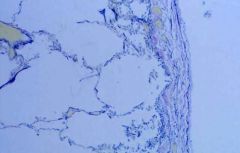
This is a largely dilated bronchiole filled with mucus. The bronchiole is filled with mucus all the way from the distal bronchiole into the alveolar sacs.
|
|
|
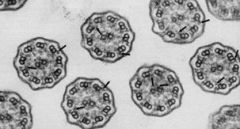
EM of normal cilia
|

