![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
317 Cards in this Set
- Front
- Back
|
What is sound? ***
|
propagation of vibratory motion that creates pressure changes in air or other mediums
|
|
|
What is the range of human hearing? ***
|
16 Hz - 20,000 Hz
|
|
|
Ultrasound operates at frequencies above the upper range of human hearing (20,000 Hz)--a range considered ________. ***
|
infrasound
(this doesn't make sense; if above it should be ultra-- infrasound is below 20 Hz) |
|
|
What are some medical uses of ultrasound? ***
|
- radiography - imaging of internal structures
- surgery - destruction of tissue - physical therapy - therapeutic ultrasound |
|
|
How is ultrasound generated? ***
|
110V/60Hz electricity transformed (converted) to higher voltage
higher voltage = higher frequency |
|
|
Describe the crystal used in the ultrasound unit. ***
|
Piezoelectric crystal within a sound head (transducer)
either - natural (quartz) or - synthetic (plumbum zirconium titanate--PZT or barium titanate) most are PZT as it is the least expensive and most efficient |
|
|
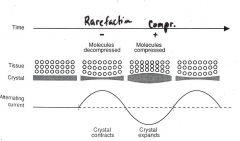
What are piezoelectric properties?
|
material which responds to an alternating current by expanding and contracting at the same frequency at which the current changes polarity
when the crystal expands, it compresses the material in front of it, and when it contracts it rarefies the material in front of it |
|
|
Describe conversion of energy with respect to ultrasound. ***
|
electrical energy is converted to mechanical energy
mechanical energy then may, depending on settings used, be converted to heat (thermal energy) within the tissue through vibrations at the molecular levels |
|
|
Describe how rarefaction and compression of the ultrasound waves affect the crystal and the tissue. ***
|
|
|
|
What is rarefaction? ***
|
the negative phase of the wave, during which the crystal contracts, allowing the tissue molecules to decompress or expand
(actually, it looks like the positive phase of the wave which compresses the crystal but allows the tissue to decompress, so we're speaking of rarefaction from the perspective of the TISSUE, not the crystal) |
|
|
What is compression? ***
|
the positive phase of the wave, during which the crystal expands and the molecules compress
(actually, it looks like the negative phase of the wave which allows the crystal to expand, but compresses the tissue, so we're speaking of compression from the perspective of the TISSUE, not the crystal) |
|
|
What are the frequencies used in therapeutic ultrasound? ***
|
either
- 1 MHz or - 3 MHz |
|
|
How deeply does the energy penetrate for ultrasound using 1 MHz? 3 MHz? ***
|
up to 5 cm (2 inches)
approximately 1-2 cm (0.4 - 0.8 inches) |
|
|
1 Hz =
1 MHz = *** |
1 cycle per second (cps)
1,000,000 cps |
|
|
Which ultrasound frequency has a more divergent beam, 1 MHz or 3 MHz? ***
|
1 MHz
|
|
|
Which ultrasound frequency has a more collimated beam, 1 MHz or 3 MHz? ***
|
3 MHz
|
|
|
What types of wave forms are available for use with therapeutic ultrasound? ***
|
continuous or pulsed
|
|
|
What is a continuous wave form in therapeutic ultrasound? ***
|
delivery of ultrasound energy throughout the entire treatment time
|
|
|
What is a pulsed wave form in therapeutic ultrasound? ***
|
delivery of ultrasound energy during only a portion of the treatment time
|
|
|
What is the ultrasound duty cycle? ***
|
the amount of time the ultrasound is on and delivering energy out of the total treatment time
expressed as a percentage or ratio e.g., a 20% duty cycle has the ultrasound being delivered only 20 percent of the time, usually 2 ms on, 8 ms off Duty cycle == Time on/total time (D = t/T or D = ON/ON + OFF) |
|
|
What is the importance of beam non-uniformity? ***
|
peaks in the energy can cause stinging or burning
|
|
|
What is Spatial Peak Intensity (SPI)? ***
|
the greatest strength (peak) of energy anywhere within the beam
usually greatest at center of beam and lowest at the edges |
|
|
What is Spatial Average Intensity (SAI)? ***
|
the average intensity of ultrasound output
|
|
|
Where is SAI measured? ***
|
at a short distance (about 1/2 cm) from the transducer/sound head
|
|
|
What is Beam Non-uniformity Ratio (BNR)? ***
|
the ratio of SPI to SAI (peak to average)
SPI:SAI |
|
|
What is the minimum acceptable BNR? ***
|
6:1
|
|
|
Who regulates acceptability of BNR? ***
|
the FDA
|
|
|
What is the maximum allowable BNR? ***
|
7:1 (Ms. Stetz was a bit unsure this was absolutely correct)
|
|
|
How can you determine the BNR? ***
|
it should be in the manual or on the machine itself
(The FDA requires the maximum BNR for an ultrasound transducer be specified on the device.) |
|
|
The higher the BNR ratio: ***
|
the less uniform the beam is
thus the beam will be less comfortable, with larger peaks to potentially sting or burn (e.g., if your unit is 5:1 and your intensity is set at 1 W/cm sq, there could be a 5 W/cm sq spike somewhere in the field) |
|
|
Does a better ultrasound machine have a higher or lower BNR? ***
|
lower is better
2:1 is better than 6:1 |
|
|
What is the Effective Radiating Area (ERA)? ***
|
the area of the transducer from which energy radiates
|
|
|
Is the ERA the same size as the transducer? Why? ***
|
no, the ERA is smaller
due to the adhesive used to hold the crystal in place |
|
|
From where does the ultrasound transducer release the most energy? ***
|
from the center
|
|
|
In what three manners may the ultrasound beam be transmitted? ***
|
it may be
- absorbed - refracted - reflected |
|
|
What happens when the ultrasound beam is absorbed? ***
|
the energy continues along a straight line (equal to incidence) into the tissue
|
|
|
What happens when the ultrasound beam is refracted? ***
|
the beam changes direction or course when it comes into contact with the tissue (it is bent)
|
|
|
What happens when the ultrasound beam is reflected? ***
|
the beam is redirected away from the surface of the tissue and does not enter
|
|
|
Where is absorption of ultrasound energy the highest? ***
|
in tissues with high collagen content
(e.g., bone, cartilage, tendon, scar tissue) |
|
|
What would cause the ultrasound energy to be reflected? ***
|
bad contact or a bad medium
ultrasound is also reflected at tissue interfaces, especially where there is greatest difference between acoustic impedance of adjacent tissues (e.g., most--about 35%--occurs at soft tissue-bone interfaces) |
|
|
Is 3 MHz ultrasound considered a deep heating modality? ***
|
yes, although at 1-2 cm, it does not penetrate as deeply as 1 MHz (1-5 cm)
|
|
|
Which means of ultrasound delivery is considered thermal? ***
|
continuous wave
|
|
|
What happens physiologically when thermal ultrasound is administered? ***
|
rapid vibration of molecules in the tissue produce heat
|
|
|
Compare thermal effects of continuous ultrasound vs. hot pack ***
|
continuous US - can increase tissue temperature 4 degrees C at depth of 3 cm
hot pack - can increase tissue temperature 0.8 degrees C at depth of 3 cm (up to 5X more effective) |
|
|
What are the thermal effects of pulsed ultrasound? ***
|
there is a small, brief heating effect during the on time of a pulse
depending on the duty cycle, this heat may or may not dissipate (will dissipate at 20%, less so at 50%--see question, "Can pulsed ultrasound produce heat?") |
|
|
What are some non-thermal effects of pulsed wave ultrasound? ***
|
- acoustic streaming
- cavitation - microstreaming these are thought to alter cell membrane permeability |
|
|
What is acoustic streaming? ***
|
circular flow of cellular fluids induced by ultrasound
constant flow of fluid the wave travels through (can kind of see this in underwater US) |
|
|
What is cavitation? ***
|
formation, growth, and pulsation of gaseous bubbles caused by ultrasound
during compression, bubbles in the tissue are squashed, during rarefaction they expand may be stable or unstable |
|
|
What is microstreaming? ***
|
micro-scale eddying occurring near a small vibrating object (very small movement of fluid)
occurs around the gas bubbles set into oscillation by cavitation |
|
|
What are the effects of thermal (continuous) ultrasound? ***
|
- increased metabolic rate
- increased circulation - increased soft tissue extensibility - decreased pain - nerve conduction velocity changes - decreased muscle spasm |
|
|
What are the effects of non-thermal (pulsed) ultrasound? ***
|
- increased skin and cell membrane permeability
- increased macrophage response - increased protein synthesis - increased intracellular calcium levels - decreased inflammation |
|
|
What are some indications for use of ultrasound? ***
|
- soft tissue shortening (use thermal)
- pain (thermal/subacute or pulsed/acute) - tendon and ligament injuries (thermal/subacute or pulsed/acute) - dermal ulcers (pulsed) - surgical skin incisions (pulsed) - fractures (there is a special US unit that assists in detecting fractures) - reabsorption of calcium deposits (calcific tendinitis/frozen shoulder???) |
|
|
What are some contraindications for use of ultrasound? ***
|
- malignant tumor
- thrombophlebitis - pacemaker - plastic or cement in joint (metal OK) - over exposed CNS tissue (e.g., post-laminectomy) - pregnancy (distal extremities OK) - complete relief of severe pain (nerve block???) - over eyes or reproductive organs - thermal on patients with impaired sensation |
|
|
What are some precautions for use of ultrasound? ***
|
- acute inflammation (pulsed OK)
- over fractures (low-dose/intensity OK) - over growing epiphyseal plates (low-dose/intensity OK) - over bony prominences - over breast implants |
|
|
What size transducer heads do we have available? ***
|
1 cm sq (looks like a penlight)
5 cm sq (medium) 10 cm sq (large) |
|
|
What additional equipment (other than the US machine) is required for application of therapeutic ultrasound? ***
|
a couplant for good contact
gel or polysonic lotion water (submersion) |
|
|
What is the duration of ultrasound treatment? ***
|
treat an area approximately twice the size of the ERA for 5-10 minutes (Cameron)
cover 1" sq every 1-2 minutes (Hayes) |
|
|
What are the intensity parameters for delivery of ultrasound? ***
|
up to 3 W/cm sq
IN GENERAL: - if using 1 MHz use about 1.0-1.5 W/cm sq - if using 3 MHz use about 0.5-1.0 W/cm sq of course, the above also depends upon patient comfort |
|
|
You need to keep the transducer moving, but how do you decide how fast? ***
|
if using unit with good BNR (2:1 to 5:1) you can move more slowly, like 1 cm/second
if using unit with poor BNR (6:1-9:1) you need to move it more quickly due to the higher peaks which may sting or burn; use 4 cm/second |
|
|
What is phonophoresis? ***
|
application of ultrasound with topical drug mixed into the medium
usually a corticosteroid such as hydrocortisone |
|
|
What are some theories behind phonophoresis? ***
|
ultrasound pressure drives the drug through the skin
heating increases vasodilation and absorption increased permeability of the stratum corneum through cavitation enhances absorption (this one is the most credible) |
|
|
Why does 1 MHz penetrate deeper? ***
|
longer wavelengths penetrate deeper
|
|
|
Why do you need to have skin contact with the transducer before you turn the ultrasound machine on? ***
|
if you're aiming it elsewhere, the sound waves can reflect back and crack the crystal
|
|
|
What variables do you control in ultrasound? ***
|
- duty cycle (continuous or pulsed)
- frequency (1 MHz or 3 MHz) - intensity (0.1 - 3.0 W/cm sq) - time (5-10 minute treatment) - size of transducer head |
|
|
When in doubt, what pulsed duty cycle should you use? ***
|
20%
|
|
|
How do the frequencies and intensities relate, in general? ***
|
3 MHz is a bit more superficial, and especially if used on smaller, bonier, less fatty areas you can probably use a lower intensity (start at around 0.5-0.7 W/cm sq)
1 MHz continuous is more likely to be used on a large, muscular area and you can probably start right at 1.0 W/cm sq) |
|
|
What types of tissue is ultrasound especially good at heating?
|
tissues with high collagen content, such as tendons, ligaments, joint capsules, and fascia
|
|
|
Non-thermal effects of ultrasound
|
- facilitate tissue healing
- modify inflammation - enhance transdermal drug delivery |
|
|
What is absorption with respect to ultrasound?
|
conversion of the mechanical energy of ultrasound into heat
highest in tissues with highest collagen content absorption increases in proportion to the ultrasound frequency (this is why we've been starting with lower intensity on 3 MHz--it is absorbed more quickly) |
|
|
Taking into account all tissue types, what is the general relationship between absorption coefficients at 1 MHz and 3 MHz?
|
by doing the math with the absorption coefficient table on page 199 (Cameron), we can see that absorption of 3 MHz ultrasound is about 3 times more efficient than 1 MHz; of course, this should be obvious as 3 is 3 times 1.
since 3 MHz comes out of the transducer faster and is absorbed about 3 times faster, we need to start treatment with a lower intensity (approximately 0.5-1.0 W/cm sq) |
|
|
BNR
|
beam nonuniformity ratio
|
|
|
SPI
|
spatial peak intensity
|
|
|
SAI
|
spatial average intensity
|
|
|
What is the absorption coefficient?
|
the amount of absorption that occurs in a tissue type at a specific frequency
determined by measuring rate of temperature rise in a homogeneous tissue exposed to ultrasound at a known intensity |
|
|
What is stable cavitation?
|
the bubbles expand and contract, but do not burst
thought to be the mechanism for nonthermal therapeutic effects of ultrasound |
|
|
What is unstable cavitation?
|
the bubbles grow, then burst, releasing free radicals (OH-, H+)
thought not to occur at the therapeutic ultrasound intensities |
|
|
To operate effectively, transducer crystals must be of an appropriate thickness to resonate with a specific frequency. How are multifrequency transducers made?
|
they use a single crystal of a thickness optimized for only one of the frequencies and they operate with decreased efficiency at the other frequency (variability, reduction of ERA, increased BNR, etc.)
recently, some composite materials have been developed to more accurately and efficiently deliver ultrasound at different frequencies |
|
|
Can pulsed ultrasound produce heat?
|
Yes, there is a small, brief heating effect during the on time of a pulse
Cameron cites a study consisting of a 10-minute treatment at frequency of 3 MHz; one used continuous US at 0.5 W/cm sq; the other used 50% duty cycle at 1.0 W/cm sq they produced equal temperature change at depth of 2 cm note the 50% duty cycle leaves less time for cooling between pulses than a 20% duty cycle |
|
|
Tissues with low ultrasound absorption coefficients generally have
|
a high water content
|
|
|
Is ultrasound effective for treating muscles?
|
generally, no, because they have a relatively low absorption coefficient
most muscles are also larger than the transducers (or twice the transducer area), thus treatment would not be efficient may be suitable for treating/heating small areas of scar tissue within muscles as the scar tissue will have a higher collagen content |
|
|
Does the speed at which the transducer is moved affect the increase in tissue temperature?
|
no
Cameron cites a study where the transducer was moved at 2-3, 4-5, or 7-8 cm/second and all three produced the same temperature elevations |
|
|
Ultrasound at higher frequency + tissue with higher collagen content =
|
higher temperature increase
|
|
|
With 3 MHz ultrasound vs. 1 MHz ultrasound, depth of penetration is _______ but maximum temperature achieved is ______
|
lower
higher |
|
|
An intensity ______ lower should be used when applying 3 MHz ultrasound than when applying 1 MHz ultrasound.
|
3 to 4 times
|
|
|
To increase the total amount of ultrasound energy being delivered, what must be increased?
|
duration or intensity
|
|
|
All other parameters being the same, what variable produces the greatest increase in temperature?
|
(higher) intensity
|
|
|
On average, soft tissue treated with ultrasound at frequency of 1 MHz and intensity of 1 W/cm sq increases in temperature _____ per minute.
|
0.2 degrees Celsius
|
|
|
Where is the highest thermal effect generally produced with ultrasound?
|
at the soft tissue-bone interfaces where reflection is the greatest
|
|
|
What is ultimately used to determine the ultrasound intensity used?
|
patient's report of warmth
thus decreased sensation should be a contraindication for thermal (continuous) ultrasound |
|
|
What will the patient feel if the ultrasound intensity is too high?
|
a deep ache from overheating of the periosteum
intensity must be turned down to avoid burning the tissue |
|
|
Pulsed ultrasound is particularly effective during the inflammatory phase because:
|
it affects macrophage responsiveness and macrophages dominate during inflammatory phase
|
|
|
There is much ambiguous information concerning the effectiveness of ultrasound, but there is one clinical use for which there is strong, high-quality evidence. What is it?
|
use of low-intensity, pulsed ultrasound for healing fractures treated nonoperatively
there is strong evidence that ultrasound promotes fracture healing |
|
|
How does increasing temperature of soft tissue promote its extensibility?
|
increases length gained for same force of stretch, while simultaneously
reduces risk of tissue damage |
|
|
How should stretching be used in conjunction with thermal ultrasound?
|
stretching during heating and maintained 5-10 minutes after application while tissue is cooling
(plastic deformation) |
|
|
Despite conflicting studies, what seems to be the effective ultrasound treatment parameters for wound (dermal ulcer) healing?
|
- 20% duty cycle
- 3 MHz frequency - 0.8-1.0 W/cm sq intensity - 5-10 minutes |
|
|
How are wounds treated with ultrasound?
|
- around the perimeter
- directly on the wound if covered with an ultrasound coupling sheet or done underwater |
|
|
How should ultrasound be applied during the acute phase of tendon inflammation?
|
- pulsed mode
- low intensity (0.5-1.0 W/cm sq) |
|
|
How should ultrasound be applied to assist in resolution of chronic tendinitis?
|
- continuous
- high enough intensity to increase tissue temperature - in conjunction with stretching |
|
|
Based on the few available studies, ultrasound parameters for tendon healing should be:
|
- low-dose (0.5-1.0 W/cm sq)
and - pulsed interestingly, in one study (Warden, et al.) use of NSAIDs cancelled the positive effects of ultrasound on tendon repair |
|
|
What is transosseous ultrasound?
|
application of ultrasound to a fracture via a metal pin inserted in the bone approximately 1 cm from the fracture or with implanted transducers
shown to decrease fracture healing time, increase bone mineral density, and improve lateral bending strength in the healing fracture |
|
|
Parameters for ultrasound facilitation of fracture healing?
|
- very low dose
- 1.5 MHz frequency - 20% duty cycle - 0.15 W/cm sq intensity - 15-20 minutes |
|
|
What form of ultrasound has potential benefit for carpal tunnel syndrome?
|
pulsed
continuous has generally not been recommended for treating carpal tunnel because of the risk of adversely impacting nerve conduction velocity by overheating |
|
|
What advantages does transcutaneous drug delivery have over oral administration or injection?
|
- higher initial drug concentration at delivery site
- avoids gastric irritation - avoids first-pass metabolism by liver - avoids pain, trauma and infection risk of injection - allows delivery to a larger area than injection |
|
|
Drugs delivered by phonophoresis become ________
|
systemic
and any contraindications to systemic delivery also apply |
|
|
How do you select a sound head?
|
choose one that has an ERA approximately half the size of the treatment area
|
|
|
Recommendations for phonophoresis
|
- pulsed 20% duty cycle
- 0.5-0.75 W/cm sq intensity - 5-10 minutes - drug preparation should also effectively transmit ultrasound |
|
|
Reduce ultrasound intensity in areas with ______ _____ or if _______________
|
superficial bone
patient complains of any increase in discomfort |
|
|
How do standing waves affect blood flow?
|
they can cause blood cell stasis (lack of flow)
the plasma and RBCs will separate and band in the vessels, this reverses with cessation of ultrasound however, the endothelial lining of the blood vessels is also damaged, and the damage remains even after treatment stops |
|
|
How are standing waves prevented?
|
keep the transducer moving
|
|
|
When using continuous ultrasound with the goal of heating tissues, the patient should feel it within ______
|
2-3 minutes
but should not feel increased discomfort at any time |
|
|
If using continuous ultrasound in an area with superficial bone, how does that affect the intensity?
|
a slightly lower intensity should produce warmth, as the ultrasound reflected by the bone will cause a greater increase in temperature
|
|
|
What intensity is most often used when applying ultrasound for nonthermal effects?
|
0.5-1.0 W/cm sq
|
|
|
What is the maximum treatment area for ultrasound?
|
approximately 4 times the ERA of the transducer
anything larger than that (like an entire lower back) will have areas cooling while other areas are still being treated or have yet to be treated |
|
|
What is electromagnetic radiation? ***
|
- electric and magnetic fields oriented perpendicular to each other
[electromagnetic energy is one of the 5 forms of energy in nature (along with chemical, mechanical, nuclear, and thermal)] |
|
|
How is the electromagnetic spectrum categorized? ***
|
according to frequency and wavelength
|
|
|
What is the relationship between frequency and wavelength? ***
|
they are inversely proportional
(i.e., the higher the frequency, the shorter the wavelength, and vice versa) |
|
|
Between infrared, ultraviolet, and visible light, which has the longest wavelength? The highest frequency? ***
|
- infrared
- ultraviolet |
|
|
At what speed does visible light move through a vacuum? Ultraviolet light? ***
|
trick question
they both move at the same speed (the speed of light) through a vacuum, as does the rest of the energy in the electromagnetic spectrum |
|
|
What is the speed of light in a vacuum? ***
|
299,792,458 metres per second
186,282 miles per second |
|
|
What does LASER stand for? ***
|
Light
Amplification by Stimulated Emission of Radiation |
|
|
What are the two broad types of medical laser? ***
|
hot or cold
|
|
|
What is a hot laser? ***
|
a laser which is capable of destroying tissue and has surgical applications
|
|
|
What is a cold laser? ***
|
a non-thermal laser which is capable of enhancing tissue
|
|
|
What are some other names for cold laser therapy? ***
|
LLLT - low-level laser therapy
LPLT - low-power laser therapy (also soft laser, therapeutic laser, biostimulating laser, medical laser, and laser acupuncture) |
|
|
What types of lasers are used with LLLT? ***
|
LLLT devices include:
- gallium arsenide (GaAs) - gallium aluminum arsenide infrared semiconductor (GaAlAs) - helium neon (HeNe) |
|
|
What type of laser is ours? ***
|
gallium aluminum arsenide infrared semiconductor (GaAlAs)
|
|
|
Why are lasers given a classification number? ***
|
it tells how much eye damage the laser could potentially cause
|
|
|
What laser classification numbers did we discuss? ***
|
1, 1M, 2
3A - eye damage w/prolonged exposure 3B - eye damage with brief use 4 1 = CD player 2 = low-level pointers, etc. |
|
|
What classification is our laser? ***
|
3B
eye damage with brief use |
|
|
What are the key properties of LLLT? ***
|
- monochromatic
- coherent - collimated |
|
|
Monochromatic =
laser light is _____ color and has _____ wavelength. *** |
one
one |
|
|
Coherent =
all waves are __ _______ *** |
in phase
|
|
|
Collimated (Directional) =
the laser beam is ________ *** |
non-divergent
|
|
|
What is SLD? ***
|
super luminescent diodes
(a.k.a. supraluminous) |
|
|
What is LED? ***
|
light-emitting diodes
|
|
|
What are the differences in light between SLD and LED? ***
|
SLD - high-intensity light
LED - low-intensity light |
|
|
Which operates at a lower frequency, SLD or LED? ***
|
SLD
|
|
|
Are SLD and LED monochromatic? ***
|
no
|
|
|
Which beam is more collimated, SLD or LED? ***
|
SLD (the beam is narrower than LED, but wider than laser)
|
|
|
Which beam is coherent, SLD or LED? ***
|
neither
|
|
|
Which is more powerful, SLD or LED? ***
|
SLD (more powerful than LED, but less than laser)
|
|
|
What are the levels of tissue penetration for laser, SLD, and LED? ***
|
5 cm
2.5 cm 0.5 cm |
|
|
Which has a longer wavelength, SLD or LED? ***
|
SLD penetrates deeper, thus must have the longer wavelength
|
|
|
What type of tissue is SLD used to treat? ***
|
superficial tissue
|
|
|
What type of tissue is LED used to treat? ***
|
very superficial tissue due to its 0.5 cm penetration
|
|
|
What is a cluster probe? ***
|
a laser diode combined with SLDs and/or LEDs to form a cluster
|
|
|
For what type of treatment is a cluster probe used? ***
|
for treating larger areas
|
|
|
How is laser power represented? ***
|
rate of energy flow/production (mW)
(usually fixed and set by manufacturer) |
|
|
How is laser power density represented? ***
|
mW/cm sq
power/cm sq the amount of power per unit area |
|
|
How can one reduce the preset, fixed manufacturer's power setting on a laser? ***
|
use it in a pulsed mode
|
|
|
What is dosage with respect to laser? ***
|
energy delivered per unit area
energy (Joules) = Power (Watts) * Time (sec) J = Ws |
|
|
What is energy density with respect to laser? ***
|
amount of power per unit area
J/cm sq |
|
|
What power and dosage settings do we use for laser? ***
|
we use the manufacturer's preset parameters
manufacturer also sets treatment time |
|
|
What percentage is used for pulsed laser treatment? ***
|
90%
it cannot be further adjusted |
|
|
At what level does cold laser and light energy work? ***
|
photons (light energy) are absorbed at the macroscopic or microscopic level
|
|
|
What is a chromophore? ***
|
at the microscopic level, it is the part of a molecule that absorbs light and gives it color
|
|
|
What are the effects of cold laser and light therapy? ***
|
- promotes collagen synthesis
- promotes ATP production - decreases inflammation - inhibits bacterial growth - promotes vasodilation - alters nerve conduction velocity (NCV)--some say it increases it, some say decreases - increases production of endogenous opiates, reducing pain (endorphins, enkephalins, etc.) - increases cell proliferation (some WBCs, fibroblasts, osteoblasts, and chondrocytes) - repairs tissue |
|
|
What is the Arndt-Schultz law? ***
|
states that:
- a certain stimulus is needed to initiate a biological process - a slightly stronger stimulus may produce greater effects - beyond a certain point, a stronger stimulus will have a progressively less positive effect - higher levels will become inhibitory (somewhat akin to the law of diminishing returns) |
|
|
What are some indications for use of lasers and light? ***
|
- wounds and fractures
- musculoskeletal disorders (bursitis, tendinitis, etc.) - neurological conditions (neuropathy, neuralgia, etc.) - pain control - arthritis - lymphedema |
|
|
Where should you position the laser to treat for pain control? ***
|
at the acupuncture points
(thus the name "laser acupuncture") |
|
|
What can be done with the laser head if contamination is a concern? ***
|
cover it with saran wrap
the laser can penetrate it and the treatment will still be effective swab the head with alcohol before and after treatment as well |
|
|
What is gridding with respect to laser treatment? ***
|
using laser to treat (an open wound) 1 to 1.5 cm sq sections @ 15 seconds each
|
|
|
What is sweeping with respect to laser treatment? ***
|
using laser to treat (an open wound) along the periphery and within
|
|
|
What are some contraindications for laser and light? ***
|
- malignancy
- after recent radiotherapy (within past 4-6 months) - over hemorrhaging regions - over eyes - over thyroid or other endocrine glands - over abdomen or low back during pregnancy - over epiphyseal plates in children or fontanels of a baby - in photo-sensitive patients |
|
|
How is laser treatment usually administered? ***
|
8-10 treatments, typically
QD (every day) or QOD (every other day |
|
|
Name some sources of electromagnetic radiation. ***
|
natural and manufactured sources
- sun - earth's magnetic field - some electrical appliances - radio, TV, lights |
|
|
What is the inverse square law? ***
|
states that the intensity of waves varies inversely with the square of the distance between the radiant source and the absorbing tissue
at 2X the distance, intensity is 1/4; at 3 feet intensity is cut to 1/9 |
|
|
What is the cosine law? ***
|
states that maximum absorption of radiant energy occurs when the source and target are at right angles to each other
|
|
|
What is the Bensen-Roscoe Law of Reciprocity? ***
|
states that intensity and duration of dose are inversely proportional
(the machine will have preset power; with a lower-power unit, treat longer and with a higher-power unit, treat shorter) |
|
|
How is the velocity of electromagnetic energy measured? ***
|
V = frequency X wavelength
|
|
|
What is the Law of Reflection? ***
|
the phenomenon of throwing back a ray of radiant energy from a surface
|
|
|
What is the Law of Refraction? ***
|
the bending of light rays when the beam passes from one medium into another
|
|
|
What is absorption of electromagnetic energy? ***
|
the taking in and assimilation of the energy
energy must be absorbed before any physiologic changes can take place |
|
|
Describe UV use in physical therapy. ***
|
use of ultraviolet light (electromagnetic energy) for
treatment light source, not a heat source was used some time back, but fell out of favor; is now making a comeback |
|
|
What are some indications for UV therapy? ***
|
- skin disorders (psoriasis, vitiligo, eczema, acne)
- wound healing |
|
|
What are the UV bands? ***
|
UVA - long wave
UVB - medium wave UVC - short wave |
|
|
Describe UVA. ***
|
- long wave
- penetrates deepest - safest and produces less erythema - use with psoralen to increase intensity, but not to the point of UVB |
|
|
Describe UVB. ***
|
- middle wave
- produces most erythema |
|
|
Describe UVC. ***
|
- short wave
- ionizing (can deform cells) - germicidal - too strong for use in PT |
|
|
What is the most common UV treatment modality? ***
|
UVA with psoralen (a.k.a. PUVA)
|
|
|
Is psoralen used with UVB? ***
|
no, the combination would be too strong and produce burns
|
|
|
What are some of the effects of UV radiation? ***
|
- erythema production
- tanning - epidermal hyperplasia - vitamin D synthesis - bactericidal effects |
|
|
What are some contraindications for UV treatment? ***
|
- skin cancer
- most systemic disorders (SLE, TB, renal and hepatic pathology, diabetes) - fever - irradiation of eyes |
|
|
What are some precautions for UV treatment? ***
|
- photosensitivity (very pale skin)
- recent X-ray therapy - photosensitizing medications or supplements (e.g., St. John's Wort) - if previous dose has not disappeared (skin is still pink or red) |
|
|
What are some of the adverse effects of UV? ***
|
- cancer
- eye damage - premature aging of skin - burning |
|
|
What is a strip test? ***
|
used to determine minimal erythemal dose (MED)
strip with 4 holes put on patient's arm, arm under lamp 1st hole uncovered for 120 seconds, then 2nd hole for 60 seconds, then 3rd and 4th for 30 seconds each (total exposure will be 240, 120, 60 and 30 seconds) patient observes for 24 hours to see which area turns pink or red within 8 hours but disappears within 24 hours--this will be the MED |
|
|
What is SED? ***
|
sub-erythemal dose - no change within 24 hours per the strip test
|
|
|
What is MED? ***
|
minimal erythemal dose - the smallest dose producing erythema within 8 hours and disappearing within 24 hours
|
|
|
What is a first-degree erythemal dose (E1)?
Second-degree (E2)? Third-degree (E3)? *** |
MED * 2 1/2
MED * 5 MED * 10 |
|
|
What factors affect UV penetration of skin? ***
|
- wavelength
- intensity of radiation - power of radiant source - distance between source and skin - angle - thickness of skin |
|
|
Parameters of UV treatment ***
|
- usually begin with lamp approximately 30 inches from skin
- time may be as low as 15 seconds, can increase to 15 minutes - must wear goggles |
|
|
Describe infrared treatment. ***
|
- superficial, dry heat
- no contact - effects same as hot pack |
|
|
What types of infrared are available? ***
|
- luminous (red, amber, or white bulb)
- non-luminous (carborundum core) |
|
|
What are some of the effects of IR treatment? ***
|
- increased temperature
- increased vasodilation - increased metabolism - decreased muscle spasm |
|
|
What are the indications for IR treatment? ***
|
- seeping wounds
- some skin conditions - sub-acute/chronic musculoskeletal conditions (strains, sprains, etc.) |
|
|
What are some contraindications for IR treatment? ***
|
- cancer
- acute inflammatory conditions - fever - active bleeding - cardiac instability - recent X-ray therapy |
|
|
Parameters of IR treatment? ***
|
- lamp approximately 24-36 inches from patient
- perpendicular - treat for approximately 20 minutes - patient feedback important |
|
|
What is radiation? ***
|
process by which energy is transferred from a material with a higher temperature to one with a lower temperature without the need for an intervening medium or contact
|
|
|
What is compression? ***
|
a mechanical force that increases external pressure on the body or a body part
|
|
|
Name three types of compression ***
|
- static (e.g., compression garments)
- intermittent (mechanical) - sequential (distal to proximal, mechanical) |
|
|
What are some indications for external compression? ***
|
- edema (due to venous insufficiency or lymphedema)
- risk of DVT - venous stasis ulcers - post-amputation - risk of hypertrophic scarring |
|
|
How does compression help resolve edema? ***
|
it increases extravascular hydrostatic pressure, reducing outflow from vessels and causing fluid in the interstitial space to return to vessels
|
|
|
What are some causes of edema due to venous insufficiency? ***
|
- obstruction by tumor
- venous valve degeneration - lack of physical activity - phlebitis |
|
|
What are some causes of lymphedema? ***
|
- obstruction by tumor
- degeneration of valves - lack of physical activity - removal of lymph nodes - radiation therapy damage |
|
|
Who is at risk of DVT? ***
|
- immobilized patients
- post-surgical patients - over 50% of all DVTs occur within hospitalized or nursing home patients |
|
|
What is a venous stasis ulcer? ***
|
a tissue breakdown caused by impaired venous circulation
for unknown reasons, frequently occurs on the medial malleolus, accompanied by swelling not necessarily painful |
|
|
How does compression aid a post-amputation patient? ***
|
prevents stretching of soft tissue due to fluid accumulation and
allows shaping of the residual limb |
|
|
Compression can help prevent _______ scarring after severe burns or injuries. ****
|
hypertrophic
|
|
|
What are some contraindications for use of intermittent or sequential compression pumps? ***
|
- heart failure or pulmonary edema
- recent DVT, thrombophlebitis, or embolism - obstructed lymphatic or venous return - severe peripheral artery disease or ulcers from arterial insufficiency - acute local skin infection - acute trauma or fracture - significant hypoproteinemia (low protein/malnutrition) - post vascular surgery - skin graft |
|
|
What are some precautions for use of intermittent or sequential compression pumps? ***
|
- uncontrolled hypertension
- impaired sensation/mentation - stroke - cancer |
|
|
What is one potential adverse effect of external compression? ***
|
too much pressure can impair arterial circulation, causing ischemia
this can impair healing or cause tissue death |
|
|
Name some compression garments. ***
|
- antiembolism stockings
- Thrombo embolic deterrent (TED) hose - velcro-closure devices (adjustable) |
|
|
Setup for intermittent pneumatic compression pump ***
|
appendage covered with stockinette and placed into an inflatable sleeve
elevate limb |
|
|
For how long and how often may a patient be treated with an intermittent pneumatic compression pump? ***
|
treat for 1-4 hours
treat 3X/week to 4X/day |
|
|
What is the on:off cycle for treatment with an intermittent pneumatic compression pump? ***
|
either 3:1 or 4:1
|
|
|
What pressure levels are used for the upper/lower extremities when using an intermittent pneumatic compression pump? ***
|
UE = 30 - 60 mmHg
LE = 40 - 80 mmHg these are only a guide, however, patient comfort should dictate |
|
|
What should the patient not feel during treatment with an intermittent pneumatic compression pump? ***
|
- tingling
- throbbing - numbness - their own pulse |
|
|
Frequency and wavelength are _______ ________
|
inversely proportional
|
|
|
Lower-frequency EMR, including ELF waves, shortwaves, microwaves, IR radiation, visible light and UV has what characteristics?
|
- non-ionizing
- cannot break molecular bonds - cannot produce ions thus can be used for therapy |
|
|
Higher-frequency EMR such as X-rays and gamma rays has what characteristics?
|
- ionizing
- can break molecular bonds - can form ions - can inhibit cell division therefore is usable only in small doses for imaging or in larger doses for tissue destruction |
|
|
The intensity of any type of EMR reaching the body is greatest when:
|
- the energy output is high
- the radiation source is close to the patient - the beam is perpendicular to the surface of the skin |
|
|
Clinical effects of EMR are determined primarily by:
|
the radiation's frequency and wavelength range
|
|
|
Frequencies of EMR used clinically can be in the _______ range.
|
- shortwave
- microwave - IR - visible light - UV |
|
|
Sunlight includes EMR in the ______ ranges
|
- IR
- visible light - UV |
|
|
Most light is ______
|
polychromatic (made up of light of various wavelengths within a wide or narrow range)
|
|
|
How does laser light differ from other forms of light?
|
it is monochromatic (made up of light that is only a single wavelength)
|
|
|
Who introduced the idea of stimulated emission and proposed the possibility of making a powerful light amplifier?
|
Albert Einstein
|
|
|
What is a maser?
|
stimulated emission of radiation in the microwave range
|
|
|
What are the advantages of hot lasers? (Just FYI, as we use cold laser for therapy.)
|
- narrow beam
- selectively absorbed by chromophores, generating heat in and destroying only tissue directly in the beam - doesn't damage surrounding tissues - sterile - allows fine control - cauterizes as it cuts - produces less scarring |
|
|
When and by whom were the first indications of non-thermal effects of tissue healing by low-level HeNe laser discovered?
|
late 60s, early 70s
Endre Mester |
|
|
Gas-tube lasers were eventually superceded by
|
semi-conductor-technology-based photodiodes
|
|
|
What types of diodes are available in laser light therapy probes (applicators)?
|
- LEDs
- SLDs - laser diodes |
|
|
LEDs, SLDs, and laser diodes produce light in the ____ or _____ range of the EM spectrum
|
- visible
- IR |
|
|
What is a cluster probe?
|
use of more than one diode in a probe (applicator)
usually they contain various diodes of different types, wavelengths, and power |
|
|
How is light generated?
|
electricity is applied to excite electrons and move them to a higher valence level
the electrons then spontaneously fall back down to their original level, and as they do, they emit photons of light at various frequencies, depending on how far they fall |
|
|
How are photodiodes constructed?
|
two layers, with P-type material in one layer and N-type material in the other
electrons fall from the N-type to the P-type, photons of various frequencies are emitted if the diode has mirrored ends, it can also be engineered to produce monochromatic laser light |
|
|
What is the difference between spontaneous emission of light (such as with a light bulb) and stimulated emission of light (such as with a laser)?
|
With spontaneous emission, the electrons rise to and fall from various levels, emitting photons of light of various frequencies
with stimulated emission, all electrons are stimulated to move up to the same level, thus when they fall they emit photons all with the same wavelength |
|
|
Laser diodes produce light that is _______, ______, _______, and ____-_____
|
- monochromatic
- coherent - directional - high-intensity |
|
|
LEDs produce light that
|
- may appear to be one color
- is not coherent - is not directional (spreads widely) - low-intensity |
|
|
How does the low power of LED affect treatment time?
|
treatment time is longer
and often there are many (>30) LEDs on the applicator |
|
|
SLDs produce light that
|
- is almost monochromatic
- is not coherent - is not directional (spreads more than laser, but less than LED) - high-intensity |
|
|
How deeply does IR light penetrate soft tissue? Red light?
|
- 2-4 cm
- only a few millimeters (just through and below skin) |
|
|
How is light intensity expressed?
|
watts or milliwatts
|
|
|
What is power density?
|
the amount of power per unit area, expressed as milliwatts per centimeter squared
(mW/cm sq) |
|
|
Laser and other light therapy applicators generally have fixed power, but how can it be reduced?
|
pulsing
|
|
|
The power of most laser diodes used for therapy is between ___ and ____ mW and are thus classified _______
|
between 5 and 500 mW
classified 3B |
|
|
When a laser or light therapy applicator includes a number of diodes, the power of the applicator is equal to _______ and the power density is equal to _______
|
the sum of the power of all its diodes
the total power divided by the total area |
|
|
Which laser application has more pronounced effects:
short-duration, high-power doses, or long-duration, low power doses if they deliver the same total amount of energy? |
short-duration, high-power doses seem to have a more pronounced effect
|
|
|
How is energy expressed?
|
in Joules
energy = power X time J = W * s |
|
|
What is energy density?
|
a.k.a. fluence
amount of power per unit area |
|
|
How is energy density expressed?
|
in Joules per centimeter squared
J/cm sq |
|
|
What treatment dose measurement is preferred for use in laser/light therapy?
|
energy density
J/cm sq |
|
|
Why do we generally not have to select the treatment time for laser/light therapy?
|
it is already included when the therapist selects either
- energy (W * s) or - energy density (J/cm sq) J = power (W) X time (sec) so energy density = W * s/cm sq |
|
|
What is a chromophore?
|
the light-absorbing portion of a molecule that gives it color and that can be stimulated by light energy to undergo chemical reactions
|
|
|
There is evidence that light has a wide range of effects at cellular and subcellular levels, including:
|
- stimulating ATP production
- stimulating RNA production - promoting collagen production - altering synthesis of cytokines involved in inflammation - initiating reactions at the cell membrane by affecting calcium channels and intercellular communications |
|
|
What is thought to be the primary contributor to the clinical benefits of laser and light therapy, particularly in tissue healing?
|
increased ATP production
|
|
|
How is laser and light therapy thought to promote collagen production?
|
by stimulating production of mRNA that codes for procollagen
|
|
|
What is important to remember about use of goggles with laser light treatment?
|
the goggles used need to be opaque to the wavelength of the light emitted from the laser being used
goggles need to be marked with the wavelength range they attenuate and their optical density within that band goggles suitable for one wavelength should not be assumed to be safe at any other wavelength |
|
|
Do eye/retinal damage concerns extend to LED and SLD?
|
no, as these nonlaser light sources are divergent and thus diffuse the light energy so that concentrated light energy would not reach the eye
|
|
|
Why is laser/light therapy contraindicated within 4-6 months after radiotherapy?
|
because radiotherapy increases tissue susceptibility to malignancy and burns
|
|
|
Although photosensitivity is a concern with laser/light treatment, is really only applies to the ____ range.
|
UV
since increased skin sensitivity to light is generally limited to the UV range of the EM spectrum, only UV irradiation must be avoided in sensitive patients |
|
|
What are some noted adverse affects of laser/light treatment?
|
- transient tingling
- mild erythema - skin rash - burning sensation - increased pain or numbness |
|
|
Since the mechanism of therapeutic action of laser and light therapy is not thermal, why do we have to be concerned with possible burns of patient skin?
|
the diodes used to apply laser or other light therapy will get warm if used for prolonged periods of time
this is more likely to occur with low-powered LEDs that take a long time to deliver a therapeutic dose of energy |
|
|
How do you treat an area that does not have intact skin, is painful to touch, or otherwise doesn't tolerate contact with laser/light therapy?
|
applicator may be held slightly above skin but with the light beams still perpendicular to the tissue surface
|
|
|
How is laser/light treatment applied if the treatment area is larger than the applicator?
|
repeat the dose to areas approximately 1 inch apart throughout the entire treatment area
|
|
|
How do you select a particular type of diode for treatment?
|
there is much controversy, since there are few studies directly comparing the effects of coherent (laser) and noncoherent (LED and SLD) light
it is not clear if the differing wavelengths, or degree of coherence or collimation have a clinical impact |
|
|
For what types of treatment might LED be most suitable?
|
since they have the most diffuse light with the widest frequency range and are low power individually they are probably most suitable for treating larger, more superficial areas
|
|
|
For what types of treatment might SLD be most suitable?
|
since they provide light that is less diffuse and of narrower wavelength than LEDs and are more powerful, they are probably most suitable for treating superficial or moderately deep areas, depending on wavelength
|
|
|
For what types of treatment might laser diodes be most suitable?
|
since laser diodes provide light of a single wavelength that is very concentrated, they are probably most suitable for treating small areas and deeper tissues in that small area
|
|
|
Laser light wavelengths:
|
- red (600-700 nm)
- IR (700-1,100 nm) longer wavelength (IR) will penetrate deeper (30-40 mm) while shorter wavelength (red) will not go as deep (5-10 mm) also now blue light which has shorter wavelength than red, and is suitable for surface tissue or exposed soft tissue |
|
|
Laser light diode power:
|
each diode somewhere between 5 mW and 500 mW
|
|
|
LED power:
|
each diode generally somewhere between 1-5 mW but can be as high as 30-40 mW
one probe (applicator) generally will have 20-60 diodes, but may be up to 200+ |
|
|
SLD power:
|
each diode somewhere between 5-35 mW, but may be as high as 90 mW or more
one probe (applicator) generally will have 3-10 diodes |
|
|
In general, low energy densities are thought to be ________, while too high an energy density can be ________ or ________
|
stimulatory
suppressive or damaging |
|
|
Laser/light treatment of acute and superficial conditions should use ______ doses, and for chronic/deeper conditions use ______ doses.
|
lower
higher |
|
|
Why is intermittent compression thought to improve circulation more effectively than static compression?
|
the varying pressure is thought to milk fluids from the distal to the proximal vessels
|
|
|
How is it thought that compression helps control scar tissue formation?
|
it is proposed that the warmth produced by compression garments increases the activity of temperature-sensitive enzymes that break down collagen, such as collagenase
|
|
|
How is normal balance of fluids maintained in tissues?
|
hydrostatic and osmotic pressure remain in proportion (with hydrostatic pressure just slightly higher)
|
|
|
What is hydrostatic pressure?
|
the pressure that pushes fluids out of the blood vessels
|
|
|
What is osmotic pressure?
|
the pressure that keeps fluids inside the vessels
|
|
|
What determines hydrostatic pressure?
|
blood pressure and effects of gravity
|
|
|
What determines osmotic pressure?
|
concentration of proteins inside and outside the vessels
|
|
|
Why, under normal circumstances, is hydrostatic pressure slightly higher than osmotic pressure?
|
to produce the small amount of fluid leakage into the tissues that eventually becomes lymph
|
|
|
What variables help ensure appropriate amount of leakage into tissues to produce lymph?
|
- healthy diet
- healthy vascular system - muscular contraction |
|
|
What are the major causes of edema?
|
- venous or lymphatic obstruction
- venous or lymphatic insuffficiency - increased capillary permeability - increased plasma volume due to sodium and water retention |
|
|
Edema may also occur following what events?
|
- exercise
- trauma - surgery - burns - infection |
|
|
Why may edema also occur after exercise, trauma, surgery, burns, or infection?
|
acute inflammation associated with these events causes increased vascular capillary permeability
|
|
|
Why may pregnancy cause edema?
|
- increased blood volume
- altered venous smooth muscle tone - increased pressure within veins caused by gravid uterus reducing venous return from the lower body, leading to venous insufficiency |
|
|
What other diseases and medical conditions can cause edema?
|
- congestive heart failure
- cirrhosis - acute renal disease - diabetic glomerulonephritis - malnutrition - radiation injury |
|
|
Should edema caused by congestive heart failure, cirrhosis, acute renal disease, diabetic glomerulonephritis, malnutrition, or radiation injury be treated with compression? Why or why not?
|
no
in these cases compression is not likely to reduce the edema and may in fact worsen the overall health of the patient |
|
|
What is the primary factor propelling both lymphatic and venous flow?
|
muscle contraction
healthy skeletal muscle activity such as with walking or running or rhythmic isometric muscle contraction provides a milking action to propel blood in the veins back to the heart |
|
|
What can cause venous insufficiency?
|
- lack of physical activity
- dysfunction of venous valves - mechanical obstruction of veins by tumor or inflammation |
|
|
What is the most common cause of venous insufficiency?
|
phlebitis
|
|
|
If limbs are in a dependent position, edema will ______
|
worsen further because of increased hydrostatic pressure caused by gravity
|
|
|
Where are lymph nodes concentrated?
|
- axillary
- throat - groin and - paraaortic areas |
|
|
Why does fluid flow into the lymphatic system?
|
because concentration of proteins inside lymphatic vessels is generally higher than in the interstitial space
|
|
|
Upon what does flow of lymphatic fluid depend?
|
as with other fluids, it depends on muscle activity
|
|
|
What factors can cause lymphedema?
|
- decreased levels of plasma proteins (especially albumin)
- mechanical obstruction in the lymphatic system - abnormal distribution of lymphatic vessels or nodes (e.g., some removed after surgery) - reduced physical activity |
|
|
How does decreased levels of plasma protein cause lymphedema?
|
the osmotic pressure that normally keeps fluid in the lymphatic vessels is reduced
|
|
|
What are normal plasma protein levels?
|
6-8 gm/dL
3.3 gm/dL for albumin |
|
|
When lymphedema is caused by hypoproteinemia, what should be done?
|
the underlying problem needs to be addressed first to prevent further edema
|
|
|
Lymphedema can be _____ or ______
|
primary
secondary |
|
|
What is primary edema?
|
congenital disorder of the lymphatic vessels
(e.g., Milroy's disease in which the lymphatic vessels are hypoplastic, aplastic, or varicose and incompetent) |
|
|
What causes secondary lymphedema?
|
- blockage or insufficiency of the lymphatics
- infection - neoplasm - radiation therapy - trauma - surgery - arthritis - chronic venous insufficiency - lipedema |
|
|
What are the most common causes of secondary lymphedema worldwide? In the U.S.?
|
- filariasis - filarial worms
- result of cancer treatment with lymph node removal or radiation, both of which can cause fibrosis (also mechanical obstruction, dysfunction of valves, accidental damage during surgery) |
|
|
What are some of the adverse consequences of edema (of any origin)?
|
- impaired ROM
- limitations of function - pain |
|
|
Persistent chronic edema, particularly lymphedema, can cause
|
collagen to be laid down in the area, leading to subcutaneous tissue fibrosis and hard induration of the skin
this may eventually cause disfiguring and disabling contractures and deformities |
|
|
Chronic edema also increases the risk of ______ because________.
|
infection
tissue oxygenation is reduced this risk is further elevated with lymphedema because of the protein-rich environment for bacterial growth |
|
|
Advanced chronic lymphatic or venous obstruction may result in:
|
- cellulitis
- ulceration - partial limb amputation if unmanaged |
|
|
When are the more serious sequelae (cellulitis, ulceration, partial amputation) of chronic lymphatic/venous obstruction more likely to occur?
|
if the pressure of the excess fluid accumulated in the interstitial extravascular spaces causes arterial obstruction
|
|
|
Chronic venous insufficiency often causes:
|
- itching due to stasis dermatitis
- brown pigmentation due to hemosiderin deposition these are commonly seen on the medial lower leg |
|
|
Blood flowing slowly can:
|
coagulate and form a thrombus
|
|
|
Which has been found to be more effective in preventing DVTs, heparin or intermittent pneumatic compression?
|
compression has been found to be at least as effective as heparin, if not more so
combining the two may be best of all |
|
|
What is postthrombotic syndrome?
|
characterized by pain, swelling and skin changes in the area of the thrombus
|
|
|
What are venous stasis ulcers?
|
areas of tissue breakdown and necrosis that occur in areas of impaired venous circulation
|
|
|
What is the mechanism for causing venous stasis ulcers?
|
it is unknown, but possible that the elevation in venous pressure caused by impaired venous circulation leads to endovascular and inflammatory changes which provide the setting for ulcer formation
skin changes associated with inflammation can then cause fibrosis, impaired wound healing, and ulceration tissue oxygen levels in the area are typically normal |
|
|
What is the treatment of choice for venous stasis ulcers?
|
compression
|

