![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
569 Cards in this Set
- Front
- Back
|
The entirety of upper limb function (shoulder girdle, shoulder joint, elbow joint, radio-ulnar joint, wrist joint) is directed toward ***
|
hand function
|
|
|
The joint and muscle structure of the upper limb offers both _______ and ______ to hand function, as well as optimizing the.... ***
|
- stability, mobility
- length-tension of hand muscles (at the wrist) |
|
|
Degrees of freedom at each joint proximal to the hand, combined with the degrees of freedom within the hand allow... ***
|
the hand a (practically) infinite number of positions from which to perform work
|
|
|
Any loss of function at any aspect of the upper limb will decrease... ***
|
the overall function of the hand (mainly because you can’t get the hand where you need it to go)
|
|
|
The hand consists of ____ digits. ***
|
5
(4 fingers and 1 thumb) |
|
|
The hand consists of ____ bones. Name them. ***
|
19
- 5 metacarpals - 14 phalanges |
|
|
Each digit of the hand has ___ metacarpal(s). ***
|
1
|
|
|
Fingers have ___ classifications of phalanges. Name them. ***
|
3
- proximal - middle - distal |
|
|
How are metacarpals designated numerically? ***
|
as 1 through 5, beginning on the radial (thumb) side
|
|
|
Each metacarpal has what landmarks? ***
|
- base
- shaft - head - neck |
|
|
Which metacarpal is the shortest and thickest? ***
|
the first (thumb)
|
|
|
Which metacarpal is generally the longest? ***
|
the second (index finger)
(yes, even though the third/middle finger may be longer overall) |
|
|
The last three metacarpal bones ______ in length from the radial to ulnar portion of the hand. ***
|
decrease
|
|
|
How many joints comprise the hand? ***
|
19 joints
5 carpometacarpal (CMC), 5 metacarpophalangeal (MCP), 4 proximal interphalangeal (PIP), 4 distal interphalangeal (DIP), and 1 interphalangeal (IP) (and, conveniently, 19 bones) |
|
|
How many phalanges does the thumb contain? ***
|
2
proximal and distal only (which is why it only has an IP joint, not PIP/DIP) |
|
|
What four joints comprise digits 2-5 (index, middle, ring, and little fingers)? ***
|
CMC
MCP PIP DIP |
|
|
What is the CMC joint? ***
|
- carpometacarpal
- articulation between distal carpal row and bases of MCs 2-5 (this was how the notes were, but there is a CMC joint at the thumb, although the function and structure are very different) |
|
|
What type of joint is the CMC? ***
|
- plane joint
(minimal to no movement) |
|
|
Motions of CMC joints ***
|
- flexion/extension
- slight abduction/adduction |
|
|
What is the primary function of the CMC joints? ***
|
palmar arching for cupping of the hand
|
|
|
What are the MCP joints? ***
|
- metacarpophalangeal joints
- articulation of heads of metacarpals with bases of proximal phalanges (knuckles) |
|
|
What type of joint are the MCP joints (at least 2-5)? ***
|
- condyloid joints
- biaxial, 2 degrees of freedom |
|
|
Of what types and ranges of motion are the MCP joints (at least 2-5) capable? ***
|
- flexion/extension
- abduction/adduction - 90-110 degrees of flexion (2-5 MCP) |
|
|
What are the PIP joints? ***
|
- proximal interphalangeal joints
- articulation of proximal phalanges with middle phalanges |
|
|
What type of joint are the PIP joints? ***
|
- hinge joints
- uniaxial, 1 degree of freedom |
|
|
Of what types and ranges of motion are the PIP joints capable? ***
|
- flexion/extension
- 80-90 degrees of flexion |
|
|
Which have greater range of motion in flexion, PIPs or DIPs? ***
|
PIPs
|
|
|
How many joints are in the thumb? ***
|
3
- carpometacarpal - metacarpalphalangeal - interphalangeal |
|
|
Describe the CMC joint of the first digit. ***
|
- thumb
- articulation of trapezium and base of first MC - saddle joint, biaxial, 2 degrees of freedom capable of: - flexion/extension - abduction/adduction - permits some rotation which allows for circumduction: which facilitates opposition (a combination of flex/ext, ab/add) |
|
|
Describe the MCP joint of the first digit. ***
|
- thumb
- articulation of first MC and proximal phalanx - hinge joint - uniaxial, one degree of freedom - flexion/extension - 50 degrees of flexion |
|
|
Describe the IP joint of the first digit. ***
|
- thumb
- articulation between proximal phalanx & distal phalanx - hinge joint - 90 degrees of flexion |
|
|
Describe the motions of thumb flexion and extension. ***
|
- flexion is movement of palmar surface of thumb in frontal plane across and parallel with palm (flexion is making 4)
- extension returns thumb back to anatomic position (sticking out) |
|
|
Describe the motions of thumb abduction and adduction. ***
|
- abduction is forward movement of thumb away from palm in a sagittal plane
- adduction returns thumb to plane of hand |
|
|
Describe the retinacular system of the hand. ***
|
- fibrous bands spanning the wrist/proximal hand region, medial-lateral
- located on volar surface (flexor retinaculum) and dorsal surface (extensor retinaculum) - long finger flexor/extensor tendons pass under retinaculum |
|
|
What is the retinacular system of the hand designed to do? ***
|
prevent bowstringing of flexor and extensor tendons
|
|
|
Describe the flexor retinaculum ***
|
- spans the wrist/carpal region to form a carpal tunnel
- structures such as the flexor tendons and median nerve pass through it - when inflammation/edema occur in this area Carpal Tunnel Syndrome develops |
|
|
Describe the extensor retinaculum ***
|
- spans dorsal wrist/carpal area
- long finger extensor tendons pass under it |
|
|
Describe the palmar aponeurois ***
|
- triangular sheet of fibrous tissue covering the long flexor tendons
- protects underlying hand structures - receives tendon of palmaris longus muscle - shrinkage of aponeurosis results in Dupuytren’s contracture |
|
|
Describe the bursae in the hand ***
|
- radial and ulnar bursa
- pad the flexor tendons - flexor tendons pass beneath the flexor retinaculum - decrease friction |
|
|
Describe the flexor (digital) tendon sheaths ***
|
- synovial-like membrane wrapping/covering finger flexor tendons as they pass on to digits
- produce friction-free excursion of tendons |
|
|
Describe the annular pulleys of the hand ***
|
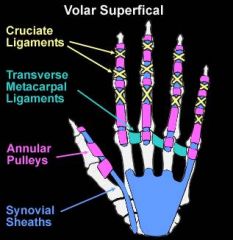
- fibrous tunnels located intermittently on digits
- flexor tendons pass through - prevent bowstringing of tendons during finger flexion |
|
|
Describe the extensor mechanism of the hand ***
|
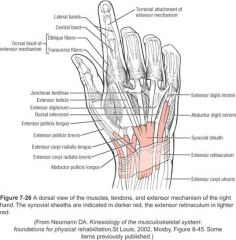
- expansion
- triangular shaped aponeurosis located on dorsum and sides of proximal phalanx of fingers - not on the thumb - finger extensor tendons, lumbricals, and muscles form an attachment to middle/distal phalanges via their attachment to expansion - extensor tendons blend with connective tissue called extensor mechanism; proximally is the dorsal hood, and ultimately the extensor mechanism attaches to the dorsal side of the distal phalanges - by way of attachments to this aponeurosis, these muscles are able to both flex MCP and extend PIP/DIPs to assume the functional position (lumbrical grip/puppet hand) of the hand (as in writing) |
|
|
How do the extrinsic extensors of fingers work with the extensor mechanism? ***
|
- extensor tendons do not attach directly to phalanges but blend with extensor mechanism
- proximal end of extensor mechanism is the dorsal hood, which wraps completely around MCP joint - extensor mechanism serves as primary distal attachment for both extensor muscle tendons and intrinsic muscles of fingers |
|
|
Describe the extrinsic muscles of the hand (in general) ***
|
- extrinsic: muscle origins proximal to wrist
- insertions in hands - assistive actions at wrist - multijoint muscles - exhibit active and passive insufficiency |
|
|
Describe the intrinsic muscles of the hand (in general) ***
|
- intrinsic: muscles having both origins and insertions in hand
- responsible for fine motor control and precision movements of fingers and thumb - fine motor skills take more stability |
|
|
Additional role of the finger flexors ***
|
assist with wrist flexion
|
|
|
Describe the flexor digitorum superficialis ***
|
- divides into 4 tendons
- attaches to middle phalanx - flexes MCP and PIP joints |
|
|
Describe the flexor digitorum profundus ***
|
- runs deep to FDS
- divides into 4 tendons - passes through split of FDS attaches to distal phalanx - flexes all three finger joints |
|
|
Additional role of the extrinsic finger extensors ***
|
assist with wrist extension
|
|
|
Describe the extensor digitorum ***
|
- divides into 4 tendons
- attaches to distal phalanges of fingers 2-5 via extensor expansion - extends all three joints of fingers |
|
|
Describe the extensor indicis ***
|
extends all joints of index finger
|
|
|
Describe the extensor digiti minimi ***
|
extends all joints of the little finger
|
|
|
Describe the flexor pulleys ***
|
- embedded within each fibrous digital sheath
- surround flexor tendons, providing them with nutrition and lubrication - following tendon injury, adhesions may develop between tendon and adjacent digital sheath or between adjacent tendons |
|
|
List the thumb extrinsic muscles and their functions ***
|
- abductor pollicis longus: abducts the thumb at CMC joint
- flexor pollicis longus: flexes all joints of thumb - extensor pollicis longus: extends MCP and IP joints of thumb - extensor pollicis brevis: extends MCP joint of thumb |
|
|
Describe the anatomical snuffbox ***
|
- tendons of EPL,EPB, APL form the borders of the depression
- on dorsolateral aspect of hand at base of thumb when thumb extended - floor of snuffbox is scaphoid bone - radial artery passes through snuffbox |
|
|
What bone forms the floor of the anatomical snuffbox? ***
|
scaphoid bone
|
|
|
What artery passes through the anatomical snuffbox? ***
|
radial artery
|
|
|
List the three groups of intrinsic muscles of the hand. ***
|
- thenar muscles - move thumb
- hypothenar muscles - move little finger - palm muscles - located between thenar and hypothenar muscles |
|
|
Describe the functional position of the hand (a.k.a. lumbrical grip or "puppet hand"). ***
|
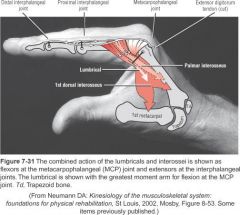
combined action of the lumbricals and dorsal and palmar interossei flex the MCP joints and extend the PIP and DIP joints
|
|
|
List and describe the thenar muscles. ***
|
- opponens pollicis: thumb opposition
- abductor pollicis brevis: abduction of MCP joint - flexor pollicis brevis: flexion of MCP joint |
|
|
List and describe the hypothenar muscles. ***
|
- opponens digiti minimi: opposition of 5th finger
- abductor digiti minimi: abduction of MCP joint - flexor digiti minimi: flexion of MCP joint |
|
|
List and describe the palm muscles. ***
|
- adductor pollicis: adducts thumb
- interossei (dorsal and palmar): --- abduction (dorsal) and adduction (palmar) of fingers --- flex MCP joints and extend PIP/DIP joints - lumbricales --- have no bony attachment (start from the FDP) --- originate on FDP and insert on extensor expansion --- flex MCP joints and extend PIP/DIP joints |
|
|
How do the wrist and hand need to be manipulated for optimal length-tension of the extrinsic finger flexors/extensors? ***
|
- the action of the extrinsic finger flexors/extensors depends upon position of the wrist for optimal length-tension
- the wrist needs to extend for maximal finger flexion or flex for maximal finger extension; if not, the muscles become actively insufficient |
|
|
How are the long finger flexors made
- actively insufficient? - passively insufficient? *** |
- active insufficiency: wrist flexion and finger flexion
- passive insufficiency: wrist extension and finger extension |
|
|
How are the long finger extensors made
- actively insufficient? - passively insufficient? *** |
- active insufficiency: wrist extension and finger extension
- passive insufficiency: wrist flexion and finger flexion |
|
|
What is tenodesis in the hand? ***
|
- use of passive insufficiency of long finger flexors together with wrist extension to get hand flexion
- utilized by patients with SCI who have active wrist extension but no finger flexion - creates a grip |
|
|
How is passive finger flexion achieved via "tenodesis action"? ***
|
- extrinsic flexors of digits cross over anterior side of wrist, and wrist position alters amount of stretch placed on these muscles
- stretching multi-articular muscle at one joint creates passive movement at another joint and is referred to as tenodesis action of muscle |
|
|
List some common injuries and pathologies of the hands. ***
|
- rheumatoid arthritis
- carpal tunnel syndrome - Dupuytren’s contracture - ruptured finger flexor/extensor tendons - compression of neurovascular structures - fractures of metacarpals or phalanges - dislocations of MCP/PIP/DIP joints |
|
|
Describe rheumatoid arthritis effects on the hand(s). ***
|
- inflammation of synovial membrane which erodes articulating joint surfaces
- affects hands bilaterally - can be severely disabling deformities include - palmar dislocation of the MCP joint - ulnar drift - swan-neck deformity - boutonniere deformity |
|
|
Describe the effects of carpal tunnel syndrome on the hand(s). ***
|
- any inflammation that causes compression of the median nerve, including inflammation of flexor retinaculum
- due to repetitive movements of finger flexor tendons through tunnel - leads to inflammation of structures contained within wrist - edema and pressure on median nerve - paraesthesia/pain in distal hand/fingers - motor dysfunction of muscles innervated by median nerve |
|
|
Describe Dupuytren's contracture. ***
|
- shrinkage of palmar aponeurosis resulting in 4th and 5th digits flexion contracture into palm
- etiology unknown |
|
|
What are the signs and symptoms of compression of neurovascular structures in the hand? ***
|
- sensorimotor dysfunction
- deformities - muscle atrophy - distal necrosis of tissue |
|
|
Cause and result of ruptured finger flexor/extensor tendons ***
|
- trauma
- results in deformities and dysfunction |
|
|
Joints of the hand are organized into three sets of articulations: ***
|
- carpometacarpal
- metacarpophalangeal - interphalangeal |
|
|
MCP joints form: ***
|
the base of each digit
|
|
|
IP joints are capable of only what types of motion? ***
|
- flexion and extension
(other potential planes of motion are blocked by bony fit of joint and by periarticular connective tissues) |
|
|
Simultaneous extension of all three joints of fingers requires: ***
|
coordinated interplay among muscles
|
|
|
What is the most-used joint in the body? ***
|
the TMJ (temporomandibular joint)
- chewing - talking - swallowing |
|
|
The TMJ opens and closes the mouth ______ times/day ***
|
1500-2000
|
|
|
Describe the articulation of the TMJ. ***
|
- articulation of mandibular condyle of mandible with mandibular fossa of temporal bone; right and left sides of jaw anterior to ear lobes
- each articulation contains an intra-articular disc separating joint space into two distinct compartments: upper and lower |
|
|
The intraarticular disc of the TMJ divides the joint into... ***
|
two distinct compartments
- upper/superior - lower/inferior |
|
|
What type of joint(s) make up the TMJ? ***
|
- it is a synovial joint
- the upper is a plane joint - the lower is a hinge joint (each has their own separate synovial lining) |
|
|
Describe the TMJ capsule. ***
|
- both the upper and lower joints are enclosed in the same capsule
- the capsule is thin and loose anteriorly (more joint dislocations occur anteriorly for this reason) |
|
|
Of what are the articulating surfaces of the TMJ comprised? ***
|
- no hyaline cartilage on the bony articulating surfaces
- fibrocartilage is present instead, as it is necessary to withstand the TMJ's repeated high-stress forces |
|
|
Are the articular surfaces of the TMJ congruent? ***
|
no, they are incongruent and the joint goes off-course frequently
|
|
|
What assists in making the incongruent TMJ more congruent? ***
|
the articular disc
|
|
|
What is the role of the ligaments comprising the TMJ? ***
|
- provide ligamentous support for stability
- attach the mandible to skull and guide movement of mandible against base of skull under the influence of muscular activity - prevent excursion of the mandible |
|
|
What are the three major ligaments of the TMJ? ***
|
- lateral temporomandibular ligament (lateral surface)
- sphenomandibular ligament (medial surface) - stylomandibular ligament (posterior) |
|
|
Of what motions is the TMJ capable? ***
|
- depression (mouth opening – normal ROM is 3 fingerwidths)
- elevation (mouth closing) - protrusion/protraction (jutting chin forward) - retrusion/retraction (sliding teeth backward) - lateral deviation (sliding teeth to either side) |
|
|
What is the normal ROM for TMJ depression? ***
|
3 fingerwidths
|
|
|
What do the muscles of the TMJ provide? ***
|
- power (chewing) and
- intricate control (talking) movement for jaw |
|
|
What muscles act at the TMJ and what do they do? ***
|
- digastric – depression of jaw
- temporalis – elevation and assists protrusion of jaw with posterior fibers - masseter – elevation of jaw and assists only initiation of protrusion - medial and lateral pterygoids – protrusion, lateral deviation, and assists elevation of jaw |
|
|
What issues can cause TMJ disorders? ***
|
- C-spine problems - poor cervical posture (forward head) often directly affects the TMJ
- poor dentition - (teeth positioning, presence/absence of teeth) can result in malocclusions and asymmetrical bite patterns which can cause dislocation of disc, unstable joint - grinding (bruise) and clenching of teeth - can cause tightness of surrounding muscles and muscle spasms, increasing compression of TMJ - injuries or trauma/blows to jaw can cause TMJ dislocation - RA can cause inflammation of the joint capsule and eventual degeneration of the disc and articulating surfaces - OA of TMJ results in degeneration of bony condyle (usually unilateral, usually due to loss of posterior teeth) |
|
|
What are some signs and symptoms associated with TMJ disorders? ***
|
- crepitation, clicking of TMJ (slipping of condyle under/out from under disc during opening and closing)
- jaw pain - decreased range of motion of jaw - asymmetrical opening/closing of mouth - closed or open locking of jaw - tinnitus (ringing in ears) - dizziness - headaches |
|
|
What is the thorax? ***
|
the portion of the trunk between the neck and abdomen
|
|
|
What are the three components of the thorax? ***
|
- ribcage
- diaphragm - abdomen |
|
|
What comprises the ribcage? ***
|
consists of:
- sternum (manubrium, body, xiphoid process) - ribs/costal cartilages - thoracic vertebrae |
|
|
How many ribs does the typical person have, and how are they attached? ***
|
12 pairs of ribs (1-7 true, 8-10 false, 11-12 floating)
ribs attach to sternum anteriorly and thoracic vertebrae posteriorly (this greatly reduces thoracic spine movements) |
|
|
Why is movement in the thoracic spine restricted? ***
|
because of the attachment of the ribs to the vertebrae
|
|
|
What joints does the ribcage have and of what type are they? ***
|
anteriorly – ribs attach to sternum via cartilage:
- costochondral joints--ribs to cartilage (synarthrodial) and - chondrosternal joints--cartilage to sternum (synovial) posteriorly – costovertebral, costotransverse (synovial plane joints) |
|
|
What are the two types of movements by the ribcage during respiration? ***
|
- bucket-handle movement
- pump-handle movement |
|
|
Describe bucket-handle movement during respiration. ***
|
- elevation of lateral aspect of rib cage up and out
- increases mediolateral diameter of thoracic cavity |
|
|
Describe pump-handle movement during respiration. ***
|
- elevation of sternal end of ribs
- increases anterioposterior diameter of thoracic cavity |
|
|
What is the diaphragm? ***
|
dome-shaped, thin musculotendinous sheath which composes the muscular floor of thoracic cavity
|
|
|
How does the diaphragm support respiration? ***
|
- actively contracts during inspirations
- moves caudally, descends or flattens, thereby increasing thoracic cavity space of lung expansion - passively recoils during expirations - ascends into thorax, forming dome shape |
|
|
Name the muscles of the abdominal wall. ***
|
- transverse abdominis
- internal/external obliques - rectus abdominis |
|
|
What are the functions of the abdominal muscles during respiration? ***
|
Two functions:
- increase in muscle tension just before inspiration which increases intra-abdominal pressure (IAP) which forces diaphragm cranially, places it on a slight stretch and insures a stronger diaphragmatic contraction upon inspiration - abdominals also assist during forced expiration |
|
|
1 inspiration + 1 expiration =
_________ *** |
1 respiration
|
|
|
Describe the inspiration process. ***
|
- elevation of ribs and increase in size of thoracic cavity due to descent of diaphragm and expansion of thoracic wall
- pressure within thorax decreases (below atmospheric pressure), air rushes into the lungs - two phases: quiet and forced |
|
|
Describe the expiration process. ***
|
- depression of ribs causing decrease in size of thoracic cavity
- pressure in thorax increases air is forced out of lungs - two phases: quiet and forced |
|
|
What is "quiet inspiration" and what muscles are involved? ***
|
- inspiration with resting or sitting quietly
- diaphragm and external intercostals |
|
|
What is "quiet expiration" and what muscles are involved? ***
|
- passive action occurring through relaxation of diaphragm
- elastic recoil of thoracic wall and lungs - results in depression of ribs - no muscle action is occurring, but external intercostals are involved |
|
|
What is "forced inspiration" and what muscles are involved? ***
|
- occurs when an individual is working very hard and needs a great deal of oxygen (“air hunger”)
- uses muscles of quiet inspiration plus accessory muscles |
|
|
What is "forced expiration" and what muscles are involved? ***
|
- occurs when an individual is working very hard or lacks elastic recoil mechanism due to disease process
- uses accessory muscles to aid in forcing air out of lungs |
|
|
What are the accessory muscles of respiration? ***
|
- muscles which attach to rib cage, shoulder girdle, or vertebral column
- muscles that can assist with inspiration/expiration during situations of stress/forced respirations (exercise, disease) - but not used during quiet respiration |
|
|
What are the accessory muscles of inspiration? ***
|
- those muscles that stabilize and/or elevate shoulder girdle, which indirectly elevate the ribcage, thereby increasing the size of the thoracic cavity
- serratus posterior superior - levator scapula - upper trapezius - rhomboids - pectoralis minor - SCM |
|
|
What are the accessory muscles of expiration? ***
|
those muscles that depress/pull down on ribs
- internal intercostals - serratus posterior inferior those muscles that compress abdomen and force diaphragm upward abdominal muscles - transverse abdominis - external/internal obliques - rectus abdominus |
|
|
What are some effects of aging on respiratory structures? ***
|
ossification of articular cartilages
- fusion of articulation - decreases mobility of rib cage decreased abdominal tone - decreases function of abdominal muscles during forced expiration increased kyphotic posture - decreases overall thoracic cavity space for lung expansion |
|
|
What are some effects of musculoskeletal changes/scoliosis on respiratory structures? ***
|
scoliosis
- abnormal lateral curvature of spine resulting in twisting of the vertebral column rotation of vertebral column - ribs are rotated in thoracic region = ribcage mobility restricted - thoracic cavity space decreased |
|
|
How many bones and intervertebral discs does the vertebral (spinal) column have? ***
|
- 33 (26) short, irregular bones forming long, multijointed rod
(7 cervical, 12 thoracic, 5 lumbar, 5 (fused into 1) sacral, 4 (fused into 1) coccygeal - 23 intervertebral discs |
|
|
What is the function of the vertebral (spinal) column? ***
|
- base of support for head and internal organs
- base for attachment of ligaments, muscle, bones - link between UE/LE - encases and protects spinal cord |
|
|
What are the five regions of the vertebral column? ***
|
1. cervical (7 bones)
2. thoracic (12 bones) 3. lumbar (5 bones) 4. sacral (5 bones, fused) 5. coccygeal (4 bones, fused) |
|
|
How do vertebrae increase and decrease in size? ***
|
- vertebrae increase in size from cervical to lumbar region
- vertebrae decrease in size from sacral to coccygeal region |
|
|
What types of curves are seen in the spinal column? ***
|
- posterior convexity present at birth
- kyphotic curves (thoracic) - lordotic curves (cervical and lumbar) |
|
|
Why is beneficial to have curvature of the spine? ***
|
- curved configuration provides strength and resilience to vertebral column
- 10 times stronger than if straight |
|
|
The vertebral column behaves as a _____ kinematic chain. ***
|
closed
|
|
|
How does being a closed kinematic chain affect the spine? ***
|
- curves are interdependent
- changes in the position of any one segment will result in changes in position of adjacent vertebral joints - not all posture variances are correctable |
|
|
How does the spine achieve its great ROM? ***
|
- motion at the juncture of any two vertebrae is extremely limited and consists of a small amount of movement (some have more than others)
- compound effects of small motions produce a large range of motion for vertebral column as a whole |
|
|
Of what types of motion is the spinal column capable, and in which planes? ***
|
- flexion/extension/hyperextension: sagittal plane
- lateral flexion/bending: frontal plane - rotation: transverse plane |
|
|
What are the major components of a vertebra? ***
|
- body
- neural (vertebral) arch - vertebral foramen |
|
|
What are the characteristics of the body of a vertebra? ***
|
- anterior portion is cylindrical portion
- major weight bearing structure of vertebral column - increase in size cervical to lumbar due to increased load - central portion covered with hyaline cartilage (cartilaginous or vertebral endplates) - spinal roots pass through intervertebral foramina - nutrients pass from cancellous bone through here to cartilaginous intervertebral discs |
|
|
How are the bodies of C1 and C2 formed and how do they articulate? ***
|
- body is absent in C1, poorly formed in C2
- spinous processes are bifid (2-pronged) - they are structurally weak in the anterior portion and fracture - C1 (atlas/yes) - atlantooccipital joint (AO joint) - C2 (axis/no) - atlanto-axial joint (AA joint) dens/odontoid process |
|
|
Describe the neural (vertebral) arch. ***
|
- posterior portion of vertebra, has many parts
- 2 pedicles projecting from body; have inferior/superior vertebral notches which form intervertebral foramina (PNS) - 2 laminae which unite in spinous process - 2 inferior and 2 superior articular processes (facets); form facet joints; orientation of facets determines type of motion occurring at that joint |
|
|
What is a pedicle? ***
|
- structures that project from body of vertebra
- have inferior/superior vertebral notches which form intervertebral foramina (PNS) |
|
|
What is the vertebral foramen? ***
|
- large opening formed by joining of body and neural arch
- spinal cord passes through |
|
|
What passes through the vertebral foramen? ***
|
spinal cord
|
|
|
Characteristics of cervical vertebrae ***
|
- smallest group of vertebrae
- body is small oval; transverse diameter is greater than A/P diameter - vertebral foramen is large - transverse processes have foramina for vertebral artery (if I remember A&P correctly, only the cervical vertebrae have foramina in the transverse process--helps to ID) - spinous process short, bifid - C1 (atlas/yes) has no spinous process or body -- it is shaped like a ring |
|
|
Characteristics of thoracic vertebrae ***
|
- intermediate size vertebrae
- body is squared-off oval - has equal transverse and A/P diameters - vertebral foramen is small - transverse process has facets for rib articulation (big clue for identifying thoracic vertebrae) - spinous process is long, slender, points inferiorly (thus limiting extension); overlap adjacent vertebra |
|
|
Characteristics of lumbar vertebrae ***
|
- largest (greatest amount of force applied in this region of the spinal column)
- body is massive oval with transverse diameter greater than entire diameter (helpful in identifying lumbar vertebrae) - 5th lumbar has a wedge shaped body for articulation with sacral segment (S1) - vertebral foramen is intermediate - spinous process thick, broad, point posteriorly (horizontally) |
|
|
Characteristics of intervertebral discs ***
|
- fibrocartilaginous discs located between each vertebral body of cervical, thoracic, lumbar regions (except C1)
- make up approx 20-33% of length of vertebral column (this is where we lose height when we age) - thickest in lumbar region (9mm) thinnest in thoracic - no independent blood supply; gets nutrients from vertebral endplates covering superior/inferior vertebral surfaces - composed of nucleus pulposis and annulus fibrosis |
|
|
What is the nucleus pulposus? ***
|
- central semi-gelatinous substance
- fluid-filled ball which acts a pivot for intervertebral joints - able to undergo great distortions with loading forces - high water content (80% at birth, < 60% at 60 y/o-- this is why older people get shorter) - can vary morning to night depending on amount of vertebral column loading - people tend to have problems where there is motion (cervical discs and lumbar discs, not generally thoracic |
|
|
How much of the length of the vertebral column is due to the height of the intervertebral discs? ***
|
20 - 33%
|
|
|
Easy ways to distinguish
- cervical vertebrae - thoracic vertebrae - lumbar vertebrae? *** |
- transverse foramina
- facets for rib attachment - size |
|
|
Why do people shrink as they age? ***
|
as we age our intervertebral discs (which comprise 20-33% of the height of our vertebral column) contain less water and compress
|
|
|
What is the anulus fibrosis? ***
|
- outer portion of intervertebral disc
- fibrocartilaginous rings - enclose nucleus pulposus and keep it under pressure - concentrically arranged - thicker anterio-laterally, thinner posteriorly (why it tends to rupture posteriorly) |
|
|
In which direction do intervertebral discs typically rupture, and why? ***
|
- typically posteriorly
- they are thicker anterio-laterally |
|
|
What are the functions of the intervertebral discs? ***
|
- absorb and transmit shock or forces
- increase motion/flexibility of vertebral column - amount of motion at any one disc joint determined by height ratio of disc-- the greater the height the more motion; reduced height reduces ROM - discs height decreases with disc rupture and aging = decreased joint ROM |
|
|
When the intervertebral discs are compressed due to aging/loss of water content, what also happens in addition to compression and loss of height? ***
|
loss of range of motion
(taller discs can bend further and have greater ROM) |
|
|
Name the joints of the vertebral column. ***
|
- atlanto-occipital (AO joint - yes)
- atlanto-axial (AA joint – no) - intervertebral joints - facet joints (zygapophyseal joints) |
|
|
What is another name for a facet joint? ***
|
zygapophyseal joint
|
|
|
What is the atlanto-occipital (AO) joint? ***
|
- articulation between occipital condyles of the skull and C1 vertebra
- synovial, condyloid biaxial joint (flex/ext, lat flex) - supports the weight of the head - protects the spinal cord - many strong ligaments to reinforce the joint, give stability for support of head, protection of SC |
|
|
What is the atlanto-axial (AA) joint? ***
|
- articulation between C1 (atlas/yes) and C2 (axis/no)
- dens (odontoid process) of axis (C2) articulates with anterior arch of atlas (C1) and transverse ligament (posteriorly) - synovial, pivot joint (rotation); 50% cervical rotation |
|
|
What contributes 50% of the total cervical rotation of the neck in each direction? ***
|
- the atlanto-axial (AA) joint between C1 and C2
- it contributes 50% and the other joints combine to make up the rest |
|
|
What are the intervertebral joints? ***
|
- articulation between vertebral bodies (except C1-2, sacral)
- weight-bearing joint of vertebral column - intervertebral discs each joint - cartilaginous, non-synovial joints - each produces a small amount of movement, cumulatively enable great ROM - in vertebral column: the intervertebral joints primarily determine amount of motion and the facet joints primarily determine direction of motion |
|
|
Describe the facet (zygapophyseal) joints. ***
|
- articulation between superior and inferior facets of adjacent vertebrae
- all levels except sacral - synovial plane joints, direction of movement is determined by the orientation of facets - lumbar processes in sagittal plane (primarily flexion/extension) - thoracic processes in frontal plane (primarily lateral bending, some rotation, minimal flexion/extension due to rib attachment and long spinous processes - cervical processes diagonally directed, with motion in all 3 planes - cervical spine is the most mobile--allows for freedom of movement for head/neck |
|
|
At what level(s) of the spinal column are there no facet (zygapophyseal) joints? ***
|
sacral
|
|
|
What is the primary motion permitted by the facet joints at the
- lumbar spine? - thoracic spine? *** |
- lumbar - primarily flexion/extension in the sagittal plane
- thoracic - primarily lateral bending in the frontal plane, some rotation and flexion/extension, but limited by rib attachment and long spinous processes - in vertebral column: the intervertebral joints primarily determine amount of motion and the facet joint primarily determine direction of motion |
|
|
Of all the spinal regions, which is the most mobile/has the most freedom of movement? ***
|
cervical (motion is permitted in all three planes)
|
|
|
What impact may compression forces have on the vertebral column? ***
|
abnormal axial compression forces though long axis of spine primarily affect:
- discs (ruptures), - end plates (fxs) |
|
|
What impact may tensile forces have on the vertebral column? ***
|
abnormal stretching/elongation on structures results in tears of:
- discs, - ligaments, - muscles around vertebral column |
|
|
What impact may shear forces have on the vertebral column? ***
|
abnormal amount of sliding between 2 vertebrae affects
- discs (tears) and - joint spaces/angles (subluxes) occurs primarily at L-S angle and shearing increases as pelvis tilts anteriorally and L-S angle increases |
|
|
What impact may bending over have on the vertebral column? ***
|
- causes compression and tensile (stretching) forces on structures opposite each other
with forward flexion, - anterior structures (discs, ligaments, bones) subject to compression forces and - posterior structures (annulus fibroses, ligaments, muscles) subject to tensile forces |
|
|
What impact may torsion have on the vertebral column? ***
|
- axial rotation, twisting (the worst)
- result in tensile forces which cause stretching and tearing - risk of rupture of disc fibers is increased when torsion, heavy axial compression, and bending are combined Example: lifting a heavy patient in a flexed, twisted posture |
|
|
What is one of the worst things you can do to your spinal column? ***
|
simultaneously twist and bend, then lift something heavy
|
|
|
What is the lumbar-pelvic rhythm? ***
|
- complete lumbar flexion is a coordinated activity of lumbar vertebral flexion and flexion of pelvis (acetabulum) on femur (anterior pelvic tilt)
- as trunk flexes, first portion of lumbar flexion occurs in lumbar intervertebral joint - last portion of flexion occurs as a result of anterior pelvic tilt (hip flexion) - this is the only way the trunk can flex enough to touch fingers to toes |
|
|
What is the sacroiliac joint? ***
|
- articulation between ilia and fused S1,2,3
- part synovial/part fibrous joint; reinforced by strong, massive ligaments - very little motion/mobility; will expand during pregnancy; often fuses in old age |
|
|
Describe the cervical region of the spinal column. ***
|
- most flexible region; movement in all planes
- 50% cervical rotation at atlanto-axial (AA) joint - head nod primarily at atlanto-occipital (AO) joint - greatest amount cervical flex/ext ROM at C4-C6 - stability essential (especially AO and AA) to support of head and protect CC - many muscles/ligaments in C1-C2 region to offer stability |
|
|
What is a cervical facet impingement and how do you treat it? ***
|
"crick in the neck" (mainly due to the loose facet joint capsules in the region)
- flex neck and rotate 45 degrees in the opposite direction to release |
|
|
Where is the greatest amount of cervical flexion/extension ROM? ***
|
C4-C6
|
|
|
Describe the thoracic region of the spinal column. ***
|
less mobility than cervical region due to
- rib cage - inferior orientation of spinous processes - taut facet joint capsules - primary movement is lateral flexion, but some rotation, minimal flex/ext |
|
|
Describe the lumbar region of the spinal column. ***
|
- primary function is to provide support for weight of upper body (HAT – head, arms, trunk)
- primary movement flex-ext - L-S angle: horizontal L5 vertebra articulating with angled S1; the greater the angle the greater the lordosis -- increases with anterior pelvic tilt -- decreases with posterior pelvic tilt - produces increased shearing forces as angle increases |
|
|
Describe the sacral region of the spinal column. ***
|
- fused sacral vertebrae
- designed for -- stability -- supporting loads and -- transmitting forces of HAT (head, arms, & trunk) from vertebral column to hip joint/LE - minimal movement at sacroiliac joint; strong massive ligaments for reinforcement of joint |
|
|
What is the role of trunk flexor muscles during erect posture? ***
|
- flexors: located anteriorally and laterally
- not active during normal erect standing - forward flexion in standing does not require flexors (due to gravity pulling torso down) - lie parallel to vertebral column and this exerts a large compression force during contraction (stability) |
|
|
What is the role of trunk extensor muscles during erect posture? ***
|
- extensors: located posteriorly
- maintain stability of vertebral column in erect posture - control forward flexion in erect posture (eccentric lowering) - lie parallel to vertebral column - exert a large compression force on vertebral column during contraction (stability) |
|
|
What are the general effects of aging and injury on the vertebral column? ***
|
- most common structures affected with aging/injury to vertebral column
-- vertebral bodies (compression fx) -- discs (ruptures) - ligaments (tears, especially PLL) |
|
|
How does the CKC and interrelatedness of spinal column structures affect the structure when one part is damaged? ***
|
deformation of one structure leads to deformation of others
(e.g., decreased disc height due to aging or injury results in: - closer proximity of vertebral bodies, facet joints, spinous processes = loss of mobility - decreased shock absorbency = increased compressive stresses on vertebral body (compression fx) - loss of height of SC = slackened anterior longitudinal ligament (ALL – runs down front)/PLL = decreased stability of SC = Hypermobility of SC) - usually kyphotic posture) -------------------------------------------------------- (e.g., bulging disc due to excessive forces results in: - overstretching of PLL = creep = eventual ligament tissue fails (tearing) = spilling of disc contents into vertebral canal = impingement on spinal nerves) |
|
|
Describe the ligaments of the vertebral column and list the primary ligaments. ***
|
- vertebral column is virtually surrounded by ligaments
- need lots of stability Primary ligaments: - Anterior longitudinal ligament (down front) - Posterior longitudinal ligament (down back) |
|
|
Describe the ALL. ***
|
Anterior longitudinal ligament
- runs down entire vertebral column on anterior surface of vertebral bodies - becomes stretched during extension - limits excessive extension and reinforces intervertebral discs anteriorally - is twice as strong as PLL |
|
|
Describe the PLL. ***
|
Posterior longitudinal ligament
- runs down entire vertebral column on posterior surface of vertebral bodies adjacent to spinal cord - becomes stretched in flexion; limits excessive flexion - reinforces intervertebral discs posteriorly - weaker than ALL - thick in Cx region/thin in Lx region - often tears in lumbar region = possible disc herniation |
|
|
List some of the other ligaments of the vertebral column located in the vertebral arch regions. ***
|
- supraspinal ligament
- interspinous ligament - ligamentum nuchae (nuchal ligament - name for supraspinal ligaments in the cranial/cervical region) - ligamentum flavum - transverse or intertransverse ligament |
|
|
What is the supraspinal ligament? ***
|
extends from C7 to sacrum along tips of spinous processes (tip to tip)
|
|
|
What is the interspinous ligament? ***
|
runs between spinous processes
|
|
|
What is the ligamentum nuchae? ***
|
(nuchal ligament)
- extension of supraspinal and interspinous ligaments in the cervical region |
|
|
What is the ligamentum flavum? ***
|
connects adjacent lamina anteriorly
|
|
|
What is the transverse or intertransverse ligament? ***
|
ligament that runs between two transverse processes
|
|
|
What is often overlooked in therapy in cases of unexplained reduced ROM in thumb?
|
the 1st CMC joint
|
|
|
Which of the following statements is (are) true regarding the normal curvatures of the vertebral column? ***
a. the cervical and lumbar regions are both normally lordotic b. the thoracic and lumbar regions are both normally kyphotic c. the cervical and sacral areas are both normally kyphotic d. the lumbar region is the only region of the spine that is normally lordotic |
a. the cervical and lumbar regions are both normally lordotic
|
|
|
The central fluid-filled portion of the intervertebral disc is called the: ***
a. vertebral end plate b. nucleus pulposus c. annulus fibrosis d. pedicle |
b. nucleus pulposus
|
|
|
Which of the following vertebrae possess transverse foramina? ***
a. cervical b. thoracic c. lumbar |
a. cervical
|
|
|
Which of the following terms is used to describe the second cervical vertebra? ***
a. cauda equina b. pedicle c. atlas d. axis |
d. axis
|
|
|
The lumbar region allows the most motion in the: ***
a. frontal plane b. sagittal plane c. horizontal plane |
b. sagittal plane
|
|
|
The craniocervical region allows the most motion in the: ***
a. frontal plane b. sagittal plane c. horizontal plane |
c. horizontal plane
|
|
|
Which motion of the lumbar spine results in a posterior migration of the nucleus pulposus of an intervertebral disc? ***
a. lateral flexion b. rotation c. flexion d. extension |
c. flexion
|
|
|
An anterior pelvic tilt is naturally accompanied by: ***
a. increased lordosis of the lumbar spine b. decreased lordosis of the lumbar spine c. strong activation of the abdominals d. near maximal elongation of the hip flexors |
a. increased lordosis of the lumbar spine
|
|
|
Which of the following motions decreases the diameter of the intervertebral foramen? ***
a. flexion b. extension |
b. extension
|
|
|
Which of the following statements best describes an anterior spondylolisthesis? ***
a. reduced flexion of the cervical vertebrae b. elongation of the ligamentum flavum c. anterior slippage, or translation, of one vertebra relative to another d. simultaneous elongation of the anterior longitudinal ligament and the rectus abdominis muscle |
c. anterior slippage, or translation, of one vertebra relative to another
|
|
|
Forward flexion of the lumbar spine involves: ***
a. elongation of the anterior longitudinal ligament b. increased diameter of the intervertebral foramen c. posterior migration of the nucleus pulposus d. b and c e. all of the above |
d. b and c
|
|
|
Torticollis is typically caused by: ***
a. tightness of the lumbar erector spinae muscles b. tightness of the sternocleidomastoid c. excessive lateral flexion of the thoracic and lumbar spine d. weakness of the quadratus lumborum |
b. tightness of the sternocleidomastoid
|
|
|
Which of the following statements is true regarding the external oblique muscle? ***
a. activation of the right external oblique produces rotation to the left b. activation of the right external oblique produces rotation to the right c. bilateral activation of the external obliques can produce a posterior pelvic tilt d. a and c e. b and c |
d. a and c
|
|
|
Which of the following muscles or muscle groups is involved with producing an anterior pelvic tilt? ***
a. erector spinae b. hip flexors c. rectus abdominis d. a and b e. b and c |
d. a and b
|
|
|
Which of the following statements is (are) true regarding scoliosis? ***
a. scoliosis refers primarily to a frontal-plane deviation b. scoliosis is named by the concave side of the spinal curve c. scoliosis is named by the convex side of the spinal curve d. a and b e. a and c |
e. a and c
|
|
|
Which muscle is part of the transversospinal muscle group? ***
a. multifidus b. internal oblique c. iliocostalis d. transverse abdominis |
a. multifidus
|
|
|
Lateral flexion of the cervical spine occurs in the: ***
a. frontal plane b. sagittal plane c. horizontal plane |
a. frontal plane
|
|
|
Performing a full sit-up requires strong activation of the: ***
a. quadratus lumborum and erector spinae b. iliocostalis and transversospinal muscles c. iliopsoas and rectus abdominis d. scalenes and suboccipital muscles |
c. iliopsoas and rectus abdominis
|
|
|
The right quadratus lumborum is able to: ***
a. rotate the lumbar spine to the left b. "hike" the left side of the pelvis c. "hike" the right side of the pelvis d. laterally flex the trunk to the left |
c. "hike" the right side of the pelvis
|
|
|
Thoracic outlet syndrome is often the result of tightness or excessive hypertrophy of the: ***
a. iliopsoas muscle b. anterior and middle scalenes c. external obliques d. foramen magnum |
b. anterior and middle scalenes
|
|
|
Which of the following muscles is referred to as the corset muscle owing to its primary function of increasing intraabdominal pressure? ***
a. quadratus lumborum b. erector spinae c. transversus abdominis d. splenius capitis and splenius cervicis |
c. transversus abdominis
|
|
|
A posterior pelvic tilt involves activation of the abdominal muscles? ***
a. true b. false |
a. true
|
|
|
The dens is a bony projection found on the first cervical vertebra? ***
a. true b. false |
b. false
it is found on the 2nd cervical vertebra (axis) |
|
|
The amount of lateral flexion that occurs in the thoracic region is largely limited by the articulation of the ribs with the thoracic vertebrae. ***
a. true b. false |
a. true
|
|
|
The cervical vertebrae have the widest, thickest bodies of all the vertebrae. ***
a. true b. false |
b. false
the lumbar vertebrae have the widest, thickest bodies |
|
|
An individual with an anterior spondylolisthesis in the lumbar region would likely perform hyper-extension exercises as part of a therapeutic regimen. ***
a. true b. false |
b. false
extension would be very bad for anterior spondylolisthesis |
|
|
About one half of the rotation available to the head and neck occurs from motion at the atlanto-axial (AA) joint. ***
a. true b. false |
a. true
|
|
|
The facet (apophyseal) joint surfaces of most lumbar vertebrae are oriented largely in the frontal plane. ***
a. true b. false |
b. false
they are typically oriented in the sagittal plane, although at the caudal end they do return to frontal orientation (e.g., L5-S1) |
|
|
A posterior pelvic tilt typically results in a decreased diameter of the lumbar intervertebral foramina. ***
a. true b. false |
the answer given is "true," however, on page 203 it states that a posterior pelvic tilt:
- flexes the lumbar spine - decreases lumbar lordosis - shifts the nucleus pulposus posteriorly - INCREASES the diameter of the intervertebral foramina |
|
|
The spinal nerves exit the vertebral column through the transverse foramina. ***
a. true b. false |
b. false
the transverse foramina are conduits for vertebral arteries |
|
|
The craniocervical region typically allows 90 degrees of axial rotation to each side. ***
a. true b. false |
a. true
|
|
|
The cervical, thoracic, and lumbar regions of the vertebral column allow what types of movement?
|
they each allow movement in all three planes;
- flexion/extension - lateral flexion - horizontal rotation |
|
|
The amount of motion allowed at any point of the vertebral column depends upon:
|
shapes and functions of local bony, muscular, and ligamentous structures
|
|
|
What can lead to neuromuscular and musculoskeletal problems?
|
- disease
- trauma - aging |
|
|
Type of curvature in the
- cervical region - thoracic region - lumbar region - sacrococcygeal region? |
- lordosis
- kyphosis - lordosis - kyphosis |
|
|
What does the anterior concavity of the thoracic and sacral regions provide?
|
space for vital organs of chest and pelvis
|
|
|
What do the normal curvatures of the spine provide?
|
strength and stability to the entire axial skeleton
|
|
|
Why can a curved vertebral column support more compressive force than a straight one?
|
- curves allow compressive forces to be shared through the tension in the stretched connective tissue and muscles on the convex side of each curve
- they also allow the vertebral column to "give" slightly under a load, rather than support large forces statically |
|
|
What can lead to exaggeration (or reduction) of normal spinal curvature?
|
- disease
- trauma - genetically loose ligaments - habitual poor posture |
|
|
Through which points does the line of gravity pass on a person with ideal posture?
|
- mastoid process
- anterior to 2nd sacral vertebra - slightly posterior to hip - slightly anterior to knee and ankle (just to the concave side of each vertebral region's curvature) |
|
|
How does gravity help maintain spinal curvature?
|
in ideal posture, gravity produces a torque that helps maintain optimal shape of each spinal curvature, allowing one to stand at ease with minimal muscular activation and minimal stress on surrounding connective tissues
|
|
|
Why do people have poor posture?
|
- muscular tightness/weakness
- trauma - poor habits - body-fat distribution - disease - heredity |
|
|
Extension of the vertebral column ______ cervical and lumbar lordosis but _____ thoracic kyphosis.
|
- increases lordosis
- decreases kyphosis |
|
|
Flexion of the vertebral column ______ cervical and lumbar lordosis but _____ thoracic kyphosis.
|
- decreases lordosis
- increases kyphosis |
|
|
Clinicians who treat people with back and neck pain often attempt to correct _______ as a primary component of the rehabilitation process.
|
faulty posture
|
|
|
Name five types of faulty posture.
|
- relaxed faulty posture
- kyphosis lordosis - sway back - flat back - round back |
|
|
What structures form the atlanto-occipital joint?
|
- occipital condyles
- atlas (C1) |
|
|
What is the primary weight-bearing structure of the vertebral column?
|
body of the vertebra
|
|
|
What is the function of the intervertebral disc?
|
shock absorber
|
|
|
What is the interbody joint?
|
formed by the junction of two vertebral bodies and the interposed intervertebral disc
|
|
|
What is the vertebral canal?
|
the hole through each vertebra, through which the spinal cord passes
|
|
|
What are pedicles?
|
- short, thick projections of bone that connect the vertebral body to the transverse process
(the "sides/walls" of the vertebral canal between the body and transverse process; they form notches for the intervertebral foramina) |
|
|
What are laminae?
|
- thin plates of bone that form the posterior wall of the vertebral canal, connecting each transverse process to the base of the spinous process
(the "sides/walls" of the vertebral canal between the transverse and spinous processes) |
|
|
What are the superior and inferior articular processes and facets?
|
- points at which the vertebrae articulate
- the inferior facet of the upper disc articulate with the superior process of the disc below it |
|
|
What do the articular processes and facets form?
|
apophyseal joints
(a.k.a. facet joints) |
|
|
How are the intervertebral foramina formed, and what is their function?
|
- they are formed by the superior and inferior notches on the pedicles and the superior and inferior articular facets)
- they serve as passageways for nerve roots entering or exiting the vertebral column |
|
|
Why does the diameter of the intervertebral foramina sometimes change?
|
because they are formed between two vertebrae (at the pedicles), thus spinal movement (especially flexion and extension) can significantly alter the diameter
|
|
|
What types of forces are intervertebral discs extremely important in absorbing and transmitting?
|
- shear
- compression |
|
|
What three structures comprise an intervertebral disc?
|
- nucleus pulposus
- annulus fibrosus - vertebral end plate |
|
|
Approximately how much of the nucleus pulposus is comprised of water?
|
70-90%
|
|
|
How many rings typically comprise the annulus fibrosus?
|
10-20 concentric rings of fibrocartilage oriented in a crisscross fashion
|
|
|
How are intervertebral discs supposed to function?
|
- two vertebrae are compressed from the pressure of body weight or muscular forces
- the nucleus pulposus of the disc in between them is squeezed outward, producing tension within the annulus fibrosus - this tension stabilizes the spongy disc, converting it into a stable weight-bearing structure |
|
|
What is the function of the vertebral end plate?
|
- connects the intervertebral disc to the vertebrae above and below
- also helps provide the disc with nutrition |
|
|
How are spinal nerves numbered?
|
- cervical spinal nerves exit ABOVE their respective cervical vertebrae (thus there is a C8)
- thoracic and lumbar nerves exit BELOW their respective vertebrae |
|
|
What is a costal facet?
|
a place for rib attachment, and only on the thoracic vertebrae
|
|
|
What is a costotransverse joint?
|
point where a rib articulates with a transverse process (only thoracic)
|
|
|
What is a costovertebral joint?
|
point where a rib articulates with the vertebral body (only thoracic)
|
|
|
Atlas (C1)
- body? - spinous process? - vertebral canal? - transverse processes? |
- no body
- no spinous processes - triangular, largest of cervical region - largest of cervical region |
|
|
Axis (C2)
- body? - spinous process? - vertebral canal? |
- tall with vertical projecting dens
- largest spinous process; bifid - large and triangular |
|
|
C3-C6
- bodies? - spinous processes? - vertebral canal? |
- wider than deep
- bifid - large and triangular |
|
|
C7
- body? - spinous process? |
- wider than deep
- large and prominent, easily palpable (thus often called vertebral prominens) |
|
|
T2-T9
- body? - spinous processes? - vertebral canal? - other features? |
- equal width and depth
- long, pointy, slant inferiorly - smaller than cervical - costal facets for ribs |
|
|
T1, T10-12
- body? - spinous processes? - vertebral canal? - other features? |
- equal width and depth; T1 has full costal facet for rib 1 and partial for rib 2
- long, pointy, slant inferiorly - smaller than cervical - costal facets for ribs, although T10-T12 may lack costal facets |
|
|
L1-L5
- body? - spinous processes? - vertebral canal? |
- wider than deep; L5 is slightly wedged (taller anteriorly than posteriorly)
- stout and rectangular - triangular; contain cauda equina |
|
|
How are the facet joints oriented in the
- cervical spine? - thoracic spine? - lumbar spine? |
- generally about halfway between horizontal plane and frontal plane (45 degrees)
- closest to the frontal plane - upper lumbar are primarily in the sagittal plane but lower lumbar vertebrae transition toward frontal plane |
|
|
Which are the most mobile vertebrae?
|
cervical
|
|
|
Which vertebrae contain transverse foramina? What are they for?
|
- cervical
- passage for vertebral arteries |
|
|
What are the uncinate processes?
|
articulations on the superior posterio-lateral side of cervical vertebrae
(those points that look like vampire fangs) |
|
|
What are the superior facets of C1 for?
|
articulating with the occipital condyles of the skull to form the AO joint
|
|
|
Why do intervertebral discs degenerate/become dehydrated?
|
due to
- excessive wear - arthritis - advanced age |
|
|
What happens when an intervertebral disc degenerates/dehydrates?
|
- bone on bone compression (esp. of uncinate processes of cervical vertebrae)
- compression stimulates growth of osteophytes (bone spurs) which may impinge nerves |
|
|
What is Wolff's Law?
|
a law governing development of osteophytes, which states that, "bone is laid down in areas of high stress and reabsorbed in areas of low stress"
|
|
|
The apophyseal/facet joints of the thoracic vertebrae are oriented.....
|
in the frontal plane, thus promoting lateral flexion primarily
|
|
|
The apophyseal/facet joints of the lumbar vertebrae are oriented.....
|
- primarily in the sagittal plane in the upper lumbar region, thus promoting flexion and extension
- lower (around L5-S1) the orientation switches to frontal, likely to prevent the lower vertebrae from sliding forward |
|
|
What is the role of the sacrum?
|
transmit weight of the vertebral column to the pelvis
|
|
|
What is the sacral promontory?
|
the portion of the sacrum which articulates with L5, forming the lumbosacral junction
|
|
|
What is the lumbosacral junction?
|
the point where L5 articulates with the sacral promontory
|
|
|
What is the sacral canal, and what does it protect?
|
- the vertebral canal of the sacrum
- protects the cauda equina |
|
|
What are the dorsal sacral foramina?
The ventral sacral foramina? |
- four pairs of holes that allow passage of the dorsal rami of sacral nerves
- four pairs of holes which allow passage of the ventral rami of spinal nerves that form much of the sacral plexus |
|
|
What is the articulation of the sacrum and coccyx called?
|
sacrococcygeal joint
|
|
|
What is the ligamentum flavum?
|
- ligaments that attach between anterior surface of one lamina and the posterior surface of the lamina below
- limits flexion - lies just posterior to spinal cord - thickest in lumbar region |
|
|
What are the supraspinous and intraspinous ligaments?
|
- ligaments between adjacent spinous processes from C7 to the sacrum
- limit flexion - called ligamentum nuchae in the cervical and cranial region - midline structure for muscle attachments and passive support for the head (supraspinous seem to run straight down the back of the spinous processes, while intraspinous seem to run along the lateral sides of the spinous processes) |
|
|
What are the intertransverse ligaments?
|
- those between adjacent transverse ligaments
- limit contralateral lateral flexion - few in the cervical region, in the thoracic are combined with muscle, in the lumbar are thin and membranous |
|
|
What is the PLL?
|
- posterior longitudinal ligament
- from C2 to sacrum, along posterior surfaces of the vertebral bodies - just anterior to spinal cord - stabilizes vertebral column, limits flexion, reinforces annulus fibrosus |
|
|
What is the ALL?
|
- anterior longitudinal ligament
- between base of occipital bone to the sacrum - along anterior surface - adds stability, limits extension or excessive lordosis in cervical/lumbar |
|
|
What is the cauda equina?
|
- "horse's tail"
- end of spinal cord |
|
|
What can damage to the cauda equina do?
Damage to the spinal cord? |
- may cause muscle paralysis, atrophy, altered sensation, and hyporeflexia
- may cause paralysis, altered sensation, spasticity, and hyper-reflexia |
|
|
Where does the adult spinal cord typically end?
|
L1-L2
|
|
|
From what aspect is movement in the spinal column defined?
|
it is described by the direction of motion of a point on the anterior side of the vertebrae
|
|
|
Movements of a particular spinal region are guided primarily by the....
|
spatial orientation of the surfaces within the facet joints
|
|
|
Flexion and extension
- plane - axis of rotation |
- sagittal
- medial-lateral (bending forward and backward) |
|
|
Lateral flexion to right or left
- plane - axis of rotation |
- forntal
- anterior-posterior (bending from side to side) |
|
|
Axial rotation to right or left
- plane - axis of rotation |
- horzontal
- longitudinal/ vertical (twisting, rotating) |
|
|
A vertebra naturally moves in the direction of _____ bony resistance, which is strongly dictated by .....
|
- least
- the articular surfaces of the facet joints |
|
|
The superior facets of C2 are oriented closest to the ____ plane and thus the freest motion is ______.
|
- horizontal
- rotation along the transverse axis |
|
|
The facet surfaces of C3-C7 are oriented ____ and thus the freest motion is ______.
|
- halfway between the horizontal and frontal planes
nearly equal between - lateral flexion along the anterior-posterior axis, and - horizontal rotation along the transverse axis |
|
|
The facet surfaces of the thoracic vertebrae are oriented closest to the ____ plane and thus the freest motion is ______.
|
- frontal
- lateral flexion along the anterior-posterior axis (although ROM is limited by ribs) |
|
|
The facet surfaces of the upper lumbar vertebrae are oriented closest to the ____ plane and thus the freest motion is ______.
|
- sagittal
- flexion and extension along a medial-lateral axis |
|
|
The facet surfaces of the lower lumbar vertebrae are oriented closest to the ____ plane and thus the freest motion is ______.
|
- frontal
- lateral flexion along the anterior-posterior axis (this may be for the "hip hiking" motion needed to walk or run; it also keeps lower lumbar vertebra from sliding anteriorly) |
|
|
Flexion ROM:
- AO joint - AA joint - C2-C7 |
- 5 degrees
- 5 degrees - 35 degrees (total of about 45-50 degrees) |
|
|
Extension ROM:
- AO joint - AA joint - C2-C7 |
- 10 degrees
- 10 degrees - 70 degrees (values are double that of flexion) (total about 85 degrees) |
|
|
Full cervical ROM for flexion and extension?
|
about 130-135 degrees
|
|
|
Axial rotation ROM:
- AO joint - AA joint - C2-C7 - total |
- negligible
- 40-45 degrees - 45 degrees (total about 90 degrees) |
|
|
Lateral flexion ROM:
- AO joint - AA joint - C2-C7 - total |
- about 5 degrees
- negligible - 35 degrees (total about 40 degrees) |
|
|
How do the roll and slide work at the AO joint?
|
opposite directions
(convex on concave) |
|
|
How much of total cervical sagittal plane motion occurs at AO and AA joints?
|
25%
|
|
|
Because of the orientation of the cervical facet joints at C2-C7, what occurs during cervical rotation?
|
the rotation is coupled with a slight amount of cervical lateral flexion
|
|
|
Because of the orientation of the cervical facet joints at C2-C7, what occurs during cervical lateral flexion?
|
the lateral flexion is coupled with a slight amount of cervical rotation
|
|
|
What is full ROM in both directions (combined) for cervical rotation?
|
about 180 degrees
(about 90 degrees each left and right) |
|
|
What does the addition of 150-160 degrees of horizontal plane motion of the eyes do for cervical rotation?
|
enables us to approach 360 degrees of visual field without moving the trunk
|
|
|
The AA joint is responsible for about ____ the rotation in the craniocervical region.
|
half
(about 45 of the 90 degrees) |
|
|
Does the head rotate without atlas?
|
no
(the AO joint strongly resists rotation, thus the AA joint is where it happens) |
|
|
How does flexion affect the size of the intervertebral foramina? Extension?
|
- flexion increases the diameter
- extension decreases the diameter |
|
|
What is one of the most commonly observed faulty postures of the craniocervical region?
|
- "forward-head" posture
- [head is protracted by flexing lower cervical vertebrae and (hyper)extending the upper craniocervical region] |
|
|
How is forward head posturing commonly treated?
|
chin tucks
(retraction of the head) |
|
|
Flexion ROM:
- thoracic - lumbar - total |
- 30-40 degrees
- 50 degrees - (about 85 degrees) |
|
|
Extension ROM:
- thoracic - lumbar - total |
- 20-25 degrees
- 15 degrees - (about 35-40 degrees) |
|
|
What is the total thoracolumbar sagittal ROM (flexion and extension combined)?
|
about 120-125 degrees
|
|
|
The five lumbar vertebrae provide about 50 degrees of flexion. How is this possible? What is the downside?
|
it is due to the near-sagittal plane orientation of the facet joints
(this freedom of motion, however, may also be the cause of the lumbar vertebrae's high incidence of HNP) |
|
|
What limits extension in the thoracic region?
|
- the inferiorly pointing spinous processes of the thoracic vertebrae, and
- the tension in the ALL |
|
|
Rotation ROM:
- thoracic - lumbar - total |
- 30 degrees
- 5 degrees - about 35 degrees |
|
|
Lateral flexion ROM:
- thoracic - lumbar - total |
- 25 degrees
- 20 degrees - about 45 degrees |
|
|
Why is rotation of the lumbar vertebrae so limited?
|
because of the near-sagittal plane orientation of the lumbar apophyseal/facet joints
|
|
|
What are the four categories of disc herniation?
|
- protrusion
- prolapse - extrusion - sequestration |
|
|
What is a protrusion?
|
displaced nucleus pulposus remains within the annulus fibrosus but may create a pressure bulge on the neural tissues
|
|
|
What is a prolapse?
|
displaced nucleus pulposus reaches the posterior edge of the disc, but remains confined within the outer layers of the annulus fibrosus
|
|
|
What is an extrusion?
|
annulus fibrosus ruptures, allowing the nucleus pulposus to completely escape from the disc into the epidural space
|
|
|
Because the nucleus pulposus is mostly fluid, it tends to migrate ____ from the compressed regions of adjacent vertebrae.
|
away
(generally moves opposite spinal motion) |
|
|
Where are HNPs most common?
|
- in the lumbar region
- posteriorly (toward the spinal cord or cauda equina) |
|
|
In which position does the least amount of pressure occur on a lumbar HNP?
|
while lying down
|
|
|
Since treatment of HNPs is often based on mechanics of spinal motion, how are posterior HNPs often treated?
|
with extension exercises to help push the nucleus pulposus anteriorly back toward the center of the disc and away from the spinal elements
|
|
|
What does "scoliosis" mean?
|
curvature
|
|
|
What is scoliosis?
|
deformity of the vertebral column, primarily characterized by abnormal frontal plane curvatures in the thoracolumbar region
|
|
|
Because the motions of the spine are mechanically coupled, scoliosis typically also involves....
|
abnormal curvatures in the horizontal plane and, to a lesser extent, in the sagittal plane
|
|
|
What is the most common pattern of scoliosis?
|
- a single lateral curve, with an apex in the T7-T9 region
- many other patterns involve a compensatory curve, most often in the lumbar region |
|
|
How is the type of scoliosis defined?
|
by the apex of convex side of the curve
|
|
|
In cases of structural (fixed) scoliosis, a characteristic _____ is often evident on forward flexion as a result of the ribs being forced to follow the unwanted rotation of the thoracic vertebrae.
|
"rib hump"
|
|
|
How is scoliosis typically treated?
|
- stretching of the tissues on the shortened (concave) side of each curve
- strengthening of the muscles on the convex side - bracing - soft tissue mobilization - postural education - surgery, when conservative treatment does not arrest progression of the deformity |
|
|
What is an anterior pelvic tilt?
What effect does it have on the lumbar spine? |
- a short-arc anterior rotation of the (top/anterior crest of the) pelvis about the hip joints, with the trunk held upright and stationary
- it extends the lumbar spine and increases lumbar lordosis - tends to shift the nucleus pulposus anteriorly and decrease the diameter of the intervertebral foramina |
|
|
What is a posterior pelvic tilt?
What effect does it have on the lumbar spine? |
- a short-arc posterior rotation of the (top/anterior crest of the) pelvis about the hip joints, with the trunk held upright and stationary
- it flexes the lumbar spine and decreases lumbar lordosis - tends to shift the nucleus pulposus posteriorly and increase the diameter of the intervertebral foramina |
|
|
What is the lumbosacral junction? What occurs here?
|
- the articulation of L5-S1
- the weight of the entire HAT is transferred to the pelvis at this point |
|
|
What is the configuration of the lumbosacral junction? What is this angle called?
|
- aligned so the base of the sacrum is inclined forward about 40 degrees from horizontal
- sacrohorizontal angle |
|
|
Why are the facet joints of L5-S1 oriented close to the frontal plane?
|
to help prevent the lower spine from translating "downhill" in a forward direction relative to the sacrum (anterior spondylolisthesis)
"spondylo" - spine "listhesis" - to slip |
|
|
What forms the SI joints?
|
- articulation between the sacrum and both iliac bones
|
|
|
What is the function of the SI joints?
|
to allow the sacrum to transfer forces of body weight to the pelvis and LE
|
|
|
How much motion do the SI joints allow?
|
- very little
- the rigidity promotes stability, which is required to transfer large forces adequately, such as when walking or running |
|
|
How is the SI joint stabilized?
|
- by many thick ligaments and roughened articular surfaces
- also by muscles such as the piriformis, hamstrings, and abdominals |
|
|
What is the most common pathology causing anterior spondylolisthesis?
|
fracture of the pars interarticularis, a section of the vertebrae midway between the superior and inferior articular processes
|
|
|
What movements are contraindicated for a person with anterior spondylolisthesis?
|
- any exercises promoting full extension or hyperlordosis
- extreme anterior pelvic tilts |
|
|
What are some of the ligaments of the SI joint?
|
- short posterior SI ligaments
- long posterior SI ligaments - sacrospinous ligaments - sacrotuberous ligament |
|
|
What is the typical rotational ROM at the SI joint? Translational distance?
|
- 2 degrees or less
- usually less than 2 mm |
|
|
What is nutation? Counternutation?
|
- means "to nod" (referencing the anterior edge of the sacrum)
- anterior rotation of the sacrum relative to the ilia - posterior rotation of the sacrum relative to the ilia |
|
|
How are the SI joints typically injured? What effects can this have on overall posture?
|
- by a fall on the hip or coccyx
- SI joints become misaligned, which destabilizes the pelvis and results in pain or significant postural compensation |
|
|
Once a spinal nerve exits an intervertebral foramen, it quickly ______.
|
divides into a ventral or dorsal ramus
|
|
|
What are dorsal rami?
|
- form short nerves that innervate most muscles of the posterior neck and posterior trunk
- muscle tissue on the posterior aspect of the vertebral column that courses between T6 and T12 is likely innervated by multiple dorsal rami from spinal nerves T6-T12 |
|
|
What are ventral rami?
|
- form the cervical, brachial, and lumbosacral plexuses
- innervate most of the muscles of the anterior-lateral trunk and neck - muscle tissue of the anterior-lateral trunk spanning T6-T12 would likely be innervated by nerves of the ventral rami of the T6-T12 region (called intercostal nerves) |
|
|
The muscles of the craniocervical region can be divided into what two groups?
|
- anterior
- posterior |
|
|
What motions do anterior craniocervical muscles perform?
Posterior craniocervical muscles? |
- flex the head/neck
- extend the head/neck (and nearly every muscle in this region also has some potential to laterally flex or rotate the craniocervical regions in the horizontal plane) |
|
|
Name the superficial muscles of the anterior craniocervical region.
|
- sternocleidomastoid
- anterior scalenes - middle scalenes - posterior scalenes |
|
|
What are the functions of the superficial anterior craniocervical muscles?
|
- flex, laterally flex, contralaterally rotate head/neck
- act as "guy wires" to stabilize the region |
|
|
What does the ventral nerve root do?
|
contains primarily outgoing (efferent) axons that provide motor signals to muscle
|
|
|
What does the dorsal nerve root do?
|
- contains mostly incoming (afferent) dendrites that carry sensory information to the spinal cord from the periphery
|
|
|
What are spinal nerves?
|
composed of dorsal and ventral nerve roots
|
|
|
What is a dorsal ramus?
|
posterior branches from the spinal nerve that innervate the deeper posterior musculature of the trunk and craniocervical regions
|
|
|
What is a ventral ramus?
|
- anterior branches from the spinal nerve that innervate the anterior-lateral musculature of the trunk and craniocervical regions
- also form the cervical, brachial, and lumbosacral plexus |
|
|
Sternocleidomastoid OAIN
|
O - sternal head - super manubrium
clavicular head - medial 1/3 I - mastoid process N - Cranial nerve XI (spinal accessory) A - bilateral - flex head/neck unilateral - rotation of head to opposite side; lateral flexion |
|
|
What is torticollis?
|
- a.k.a. wryneck
- tightness of a SCM which results in the head and neck becoming positioned into all of the actions of the SCM (flexion, lateral flexion, contralateral rotation) - typically seen in young children, treated conservatively with stretching and ST mobilization |
|
|
Anterior scalene OAIN
(1413 Ex3) |
O - transverse processes C3-C7
I - first rib N - ventral rami (C3-C7) A - bilateral - flexion of neck; assist inspiration unilateral - lateral flexion |
|
|
Middle scalene OAIN
(1413 Ex3) |
O - transverse processes C2-C7
I - first rib N - ventral rami (C3-C7) A - bilateral - flexion of neck; assist inspiration unilateral - lateral flexion |
|
|
Posterior scalene OAIN
(1413 Ex3) |
O - transverse processes C5-C7
I - external surface of second rib N - ventral rami (C3-C7) A - bilateral - assist inspiration unilateral - lateral flexion |
|
|
How do scalenes assist inspiration?
|
by elevating the ribs
|
|
|
Who may have hypertrophied scalenes?
|
COPD patients, from using them to assist with labored breathing
|
|
|
If either the anterior or middle scalene is significantly tight, what may happen?
|
the patient may experience thoracic outlet syndrome
|
|
|
What passes between the anterior and middle scalenes?
|
- brachial plexus
- subclavian artery (thus if either muscle is tight, they could pinch one of the above and cause thoracic outlet syndrome) |
|
|
Name the deep anterior craniocervical muscles and their function
|
- longus colli
- longus capitis - rectus capitis anterior - rectus capitis lateralis - flex neck and head, dynamically stabilize the craniocervical region |
|
|
Longus colli OAIN
|
O - bodies and transverse processes of C3-T3
I - transverse processes and bodies of C1-C6 N - ventral rami C2-C8 A - flexion of the neck |
|
|
Longus capitis OAIN
|
O - transverse processes of C3-C6
I - anterior to foramen magnum N - ventral rami C1-C3 A - bilateral: flexion of the head and neck |
|
|
Rectus capitis anterior OAIN
|
O - transverse processes of C1
I - just anterior to occipital condyles N - ventral rami C1-C2 A - flexion of the head (AO joint only) |
|
|
Rectus capitis lateralis OAIN
|
O - transverse processes of C1
I - just lateral to occipital condyles N - ventral rami C1-C2 A - unilateral: lateral flexion of the head (AO joint only) |
|
|
Name the deep posterior craniocervical muscles.
What is their function? |
suboccipital muscles
- rectus capitis posterior major - rectus capitis posterior minor - obliquus capitis superior - obliquus capitis inferior - fine control of movements in the AO and AA joints for positioning the head for vision, hearing, and vestibular functions |
|
|
With what is tightness of the suboccipital muscles often associated?
|
"forward head" posture
|
|
|
Rectus capitis posterior major OAIN
|
O - spinous process of C2
I - lateral aspect of inferior nuchal line N - suboccipital nerve (dorsal ramus C1) A - bilateral: extension of AA/AO joints; unilateral: lateral flexion of AO joint, rotation to same side at AA joint |
|
|
Rectus capitis posterior minor OAIN
|
O - posterior tubercle of C1
I - medial aspect of inferior nuchal line N - suboccipital nerve (dorsal ramus C1) A - bilateral: extension of AO joint |
|
|
Obliquus capitis superior OAIN
|
O - transverse process of C1
I - lateral aspect between superior and inferior nuchal lines N - suboccipital nerve (dorsal ramus C1) A - bilateral: extension of AO joint; unilateral: lateral flexion of AO joint |
|
|
Obliquus capitis inferior OAIN
|
O - apex of spinous process of C2
I - inferior margin of the transverse process of C1 N - suboccipital nerve (dorsal ramus C1) A - bilateral: extension of AA joint; unilateral: same-side rotation of AA joint |
|
|
Name the superficial cervical extensors.
What are their function? |
- splenius capitis
- splenius cervicis - work together to extend, laterally flex, and rotate the head and neck to the same side |
|
|
Splenius capitis OAIN
|
O - lower half of ligamentum nuchae and spinous processes of C7-T3
I - mastoid process and lateral 1/3 of superior nuchal line N - dorsal rami (C2-C8) A - bilateral: extension of head and neck unilateral: lateral flexion of head and neck, ipsilateral rotation of head and neck |
|
|
Splenius cervicis OAIN
|
O - spinous processes of T3-T6
I - transverse processes of C1-C3 N - dorsal rami (C2-C8) A - bilateral: extension of neck unilateral: lateral flexion of neck, ipsilateral rotation of neck |
|
|
What is whiplash?
|
result of uncontrolled acceleration of head and neck into flexion, extension, or both
|
|
|
Which type of whiplash generally causes greater strain on muscles and soft tissues?
|
whiplash associated with hyperextension
(partially because maximum extent of cervical flexion is blocked by the chin striking the chest |
|
|
What muscles are particularly vulnerable to hyperextension-associated whiplash?
|
- longus colli
- longus capitis |
|
|
What signs and symptoms does a person with hyperextension whiplash display?
|
- marked tenderness and
- protective spasm in the region of the longus colli/capitis |
|
|
What can a cervical hyperextension (whiplash) injury lead to?
|
- cervical instability
- difficulty shrugging shoulders - without stabilization provided by longus colli and other flexors, upper trapezius loses its stable cranial attachment and thus loses its effectiveness at elevating the shoulder girdle (as part of the upper trapezius, lower trapezius, serratus anterior upward rotation force couple, as well as with the levator scapula and rhomboids in pure elevation, I assume; weakness of upper trapezius also may lead to depressed and downwardly rotated scapula, superior dislocation of the SC joint, and subluxation of the GH joint) |
|
|
Ample control of the head and neck is essential for coordinated alignment of the ________.
|
eyes and ears
(neurologically, many muscles of the head and neck are closely linked to the visual and vestibular systems of the brain) |
|
|
What is the primary function of the deeper craniocervical muscles?
|
- to fine-tune movements of the head and neck
- these muscles (e.g., suboccipitals) are effective at neutralizing secondary (and often undesired) actions that are otherwise dictated by the plane of the facet joint |
|
|
Name the anterior-lateral muscles of the trunk.
|
- rectus abdominis
- external oblique - internal oblique - transverse abdominis |
|
|
What is the main purpose of the anterior-lateral trunk muscles?
|
- provide mobility and stability to the trunk
|
|
|
What does contraction of the abdominal muscles do, and why is this important?
|
- increases intra-abdominal and intrathoracic pressures
- helps in stabilizing the lumbar spine during lifting, coughing, defecation, and childbirth |
|
|
When contracting bilaterally, the abdominal muscles decrease the distance between the _____ and the _____.
|
- xiphoid process of sternum
- pubic bone |
|
|
Bilateral contracting of abdominals is expressed by either _____ or ______ (or ______.)
|
- flexing the thoracic region ("crunches")
- posteriorly tilting the pelvis - or both actions simultaneously |
|
|
Why is the ability to posteriorly tilt the pelvis so important?
|
- it is necessary to neutralize the strong anterior tilting potential caused by contraction of the hip flexor muscles
- this is why clinicians often promote abdominal activation prior to any strong activation of hip flexors (such as straight leg raises) to prevent unwanted lumbar lordosis |
|
|
What is the thoracolumbar fascia?
|
- an extensive, dense sheet of connective tissue that attaches to the spinous processes of all lumbar vertebrae, posterior sacrum, and posterior ilium
- this tissue tightly wraps around several muscles, including the erector spinae, quadratus lumborum, and latissimus dorsi |
|
|
How can contraction of the abdominal muscles help support the lower back?
|
- contraction of the abdominal muscles increases the tension in the thoracolumbar fascia
- this allows the abdominal muscles to transfer force to mechanically support the lower back (maybe why we instinctively contract our abs and hold our breath just prior to a lift) |
|
|
How do we over-stretch the thoracolumbar fascia?
|
- slumped sitting with overly flexed lower back for long period of time
- may reduce the stiffness in the tissue and reduce the effectiveness of the force transfer from the abs and lower back |
|
|
Rectus abdominis OAIN
(1413 Ex3) |
O - crest of pubis
I - xiphoid process and cartilage of ribs 5-7 N- intercostal nerves (T7-T12) A - flexion of trunk, posterior pelvic tilt, increases intra-abdominal and intrathoracic pressure two halves separated by tendinous sheath called linea alba, which mechanically links left and right sets of abdominal muscles; also has three tendinous intersections, which help produce the "six pack" |
|
|
External oblique OAIN
(1413 Ex3) |
O - lateral side of ribs 4-12
I - iliac crest, linea alba N- intercostal nerves (T8-T12) A - bilateral: flexion of trunk, posterior pelvic tilt, increases intra-abdominal and intrathoracic pressure; unilateral: contralateral trunk rotation; lateral flexion largest of lateral abdominal muscles; fibers travel inferior-medial (as your hands travel when putting them into front pockets) primary contralateral rotator of the trunk |
|
|
Internal oblique OAIN
(1413 Ex3) |
O - iliac crest, inguinal ligament, and thoracolumbar fascia
I - ribs 9-12, linea alba N- intercostal nerves (T8-T12) A - bilateral: flexion of trunk, posterior pelvic tilt, increases intra-abdominal and intrathoracic pressure, increases tension in thoracolumbar fascia; unilateral: lateral flexion of the trunk, ipsilateral rotation of trunk deep to the external oblique; courses superior medial (iliac crest to sternum) nearly perpendicular to the external oblique primary ipsilateral rotator of the trunk |
|
|
Transverse abdominis OAIN
(1413 Ex3) |
O - iliac crest, thoracolumbar fascia, cartilages of ribs 6-12, and inguinal ligament
I - linea alba N- intercostal nerves (T7-T12) A - increases intra-abdominal pressure, increases tension in thoracolumbar fascia deepest abdominal muscle; a.k.a. "corset muscle," reflecting its primary function of increasing intra-abdominal pressure; as with internal oblique, contraction pulls on the thoracolumbar fascia, and the resulting tension helps stabilize the lumbar region during lifting activities |
|
|
Other functionally associated muscles (not considered muscles of the trunk, but strongly associated with movement and stability of lumbar region).
|
- iliopsoas (iliacus and psoas major)
- quadratus lumborum (anatomically a muscle of the posterior abdominal wall) |
|
|
Functions of the iliopsoas in the lumbar region
|
- primary hip flexor
- dominant role in other motions of the trunk and pelvis (e.g., sit-ups, anterior pelvic tilt) |
|
|
Functions of the quadratus lumborum in the lumbar region
|
- bilateral activation results in extension of the lumbar spine
|
|
|
Iliopsoas OAIN
|
O - (psoas) transverse processes of T12-L5; (iliacus) iliac fossa
I - lesser trochanter of femur N- femoral nerve A - hip flexion, trunk flexion, anterior pelvic tilt abdominals produce posterior pelvic tilt, while iliopsoas produces anterior pelvic tilt; these muscles can be activated together to firmly stabilize the pelvis within the sagittal plane |
|
|
Quadratus lumborum OAIN
|
O - crest of ilium
I - transverse processes of L1-L4 and 12th rib N- ventral rami (T12-L3) A - bilateral: extension of the lumbar region; unilateral: lateral flexion of trunk clinically, the muscle is known as a "hip-hiker, describing its ability to elevate one side of the pelvis; patients with weak or paralyzed hip flexors can be taught to contract their QL to elevate one side of the pelvis, helping clear the foot from the ground as it is advanced forward during gait |
|
|
What are the two phases of a sit-up?
|
- trunk flexion phase - abdominals (primarily rectus abdominis) bring xiphoid to pubis and flatten lordotic curve of lumbar spine; phase concludes when scapulae clear the surface, however abdominal muscles remain active throughout entire sit-up
- hip flexion phase - hip flexors rotate pelvis and attached trunk anteriorly, drawing the chest closer to the knees |
|
|
How will a person with weak abdominals compensate during a sit-up?
|
- strong contraction of hip flexors, which immediately take over the action
- noted by exaggerated anterior pelvic tilt and increased lumbar lordosis as pelvis and trunk are rotated forward and upward |
|
|
Name the muscles of the erector spinae group.
|
- spinalis (capitis, cervicis, thoracis)
- longissimus (capitis, cervicis, thoracis) - iliocostalis (cervicis, thoracis, lumborum) |
|
|
As a group, the erector spinae....
|
extend and stabilize the entire vertebral column and craniocervical region
|
|
|
The inferior parts of the erector spinae share what common attachment?
|
to the common tendon
- a broad, thick tendon just superficial to the sacrum - blends with the more superficial part of the thoracolumbar fascia |
|
|
spinalis (capitis, cervicis, thoracis) OAIN
|
O -
capitis - blends with semispinalis capitis cervicis - ligamentum nuchae and spinous processes of C7-T1 thoracis - common tendon I - capitis - blends with semispinalis capitis cervicis - spinous process of C2 thoracis - spinous processes of T1-T6 N- dorsal rami of adjacent spinal nerves A - bilateral: extension |
|
|
longissimus (capitis, cervicis, thoracis) OAIN
|
O -
capitis - transverse processes of T1-T5 and near facet joints C3-C7 cervicis - transverse processes of T1-T4 thoracis - common tendon I - capitis - mastoid process cervicis - transverse processes of C2-C6 thoracis - transverse processes of T1-T12 N- dorsal rami of adjacent spinal nerves A - bilateral: extension; unilateral: lateral flexion |
|
|
iliocostalis (cervicis, thoracis, lumborum) OAIN
|
O -
cervicis - angle of ribs 3-7 thoracis - angle of ribs 6-12 lumborum - common tendon I - cervicis - transverse processes of C4-C6 thoracis - angle of ribs 1-6 lumborum - angle of ribs 6-12 N- dorsal rami of adjacent spinal nerves A - bilateral: extension; unilateral: lateral flexion |
|
|
Name the transversospinal muscles
|
- semispinalis
- multifidus - rotators |
|
|
Where are the transversospinal muscles located?
|
- deep to the erector spinae
- run obliquely from transverse processes of one vertebra to the spinous processes of more superior vertebrae |
|
|
How are the transversospinal muscles similar? Different?
|
- similar fiber direction
- length and number of vertebral segments they cross |
|
|
Where are the transversospinal muscles particularly well developed? What is the benefit?
|
- lumbar and craniocervical areas
- extra stability |
|
|
Function of all transversospinal muscles
|
- extend the vertebral column
- oblique fiber direction also gives them a favorable line of pull to produce contralateral rotation |
|
|
The more horizontal (and shorter) the transversospinal muscle, the greater the potential to...
|
produce horizontal plane rotation
|
|
|
How do the transversospinal muscles work with the oblique abdominal muscles?
|
- during trunk rotation
(e.g., rotation to the left is driven primarily by the right external and left internal obliques and reinforced by the right transversospinal muscles |
|
|
Semispinalis (capitis, cervicis, thoracis) OAIN
|
O - transverse processes of C4-T12
I - spinous process 6-8 vertebral segments above the origin; semispinalis capitis attaches just above inferior nuchal line N- dorsal rami of adjacent spinal nerves (C1-T12) A - bilateral: extension; unilateral: rotation to opposite side |
|
|
Multifidus OAIN
|
O - transverse processes of T1-T12
mamillary processes of L1-L5 sacrum I - spinous process 2-4 vertebral segments above the origin; N- dorsal rami of adjacent spinal nerves (C4-S3) A - bilateral: extension; unilateral: rotation to opposite side |
|
|
Rotators OAIN
|
O - transverse processes of all vertebrae
I - spinous process 1-2 vertebral segments above the origin; N- dorsal rami of adjacent spinal nerves (C4-L4) A - bilateral: extension; unilateral: rotation to opposite side |
|
|
What comprises the short segmental group?
|
- intertransversarus muscles
- interspinales muscles |
|
|
Intertransversarus muscles attachment and action
|
- attach between consecutive transverse processes
- unilaterally: laterally flex spine |
|
|
Interspinalis muscles attachment and action
|
- attach between consecutive spinous processes
- extend the spine |
|
|
At what are the intertransversarus and interspinalis muscles particularly effective?
|
- the paired, segmental nature of these muscles allows them to control movement at individual intervertebral junctions, enabling them to provide fine control over the vertical stability of the vertebral column in both sagittal and frontal planes
- they also provide a rich source of sensory feedback, essential for subconscious control of postural alignment |
|
|
The muscles of the posterior trunk have an important function in....
|
- vertically stabilizing the vertebral column
- each muscle group does so in a different manner |
|
|
Which are the most superficial of the posterior trunk muscles?
|
erector spinae
|
|
|
Because of their parallel path, the erector spinae are often referred to as the ______.
|
paraspinals
|
|
|
Each muscular column of the erector spinae crosses many intervertebral segments and is therefore only capable of
|
furnishing gross control over extension and lateral flexion
|
|
|
The transversospinal muscles course obliquely (from nearly vertical to nearly horizontal) across relatively few intervertebral segments, thus...
|
they can exert more refined, multidirectional control over the alignment of the vertebral column
|
|
|
The deep (short) segmental muscles cross only one intervertebral segment, thus...
|
can provide the most precise control over vertical stability
|
|
|
Bending over to touch the toes requires adequate flexibility in both ______ and _____
|
- hips
- low back |
|
|
When observing someone attempting (but unable) to touch their toes, how would tight hamstrings manifest in the lumbopelvic rhythm?
|
- little movement at/flexion of the hip
- excessive lumbar flexion |
|
|
When observing someone attempting (but unable) to touch their toes, how would tight lower back muscles manifest in the lumbopelvic rhythm?
|
- little movement at/flexion of the back
- excessive hamstring flexion |
|
|
What effects can forward flexion compensations (of either the hamstrings or low back) in the lumbopelvic rhythm have?
|
- tightness in one area can place large demands on the other, possibly inducing stress-related pathology
- this is why it's important to visually isolate the components of a particular movement to help determine the origin of a particular limitation |
|
|
Lifting even moderately sized objects can generate large _____ and _____ forces throughout the body, and especially in the base of the spine.
|
compression, shear
|
|
|
Optimal lifting technique allows the forces on the low back to be shared by muscles of the _____, _____, and ______
|
arms, legs, trunk
|
|
|
What are the two sources of stability in the spinal column?
|
- active muscle force (primary)
- ligaments, connective tissue (secondary) |
|
|
What is a neutral spine?
|
- proper spinal alignment with the normal curvatures intact
|
|
|
Core stabilization exercises for the abdominals and posterior trunk are often integral components of ____ rehab programs.
|
back
|
|
|
Core stabilization exercises challenge both _____ and _____ muscular stabilizers.
|
- intrinsic (transversospinal and short segmental groups - attach within the vertebral column to provide fine motor/precise stabilization)
- extrinsic (abdominals, erector spinae, quadratus lumborum, psoas major - attach outside vertebral column to provide gross motor stabilization/movement) |
|
|
What is typically involved in a core stabilization program?
|
- work on extrinsic and intrinsic muscles
- holding a neutral or optimally positioned lumbar spine and pelvis while simultaneously performing movements or dynamic posturing |
|
|
What are the three major requirements of the thoracolumbar region?
|
- protect the organs
- function as a mechanical chamber for breathing - core stability |
|
|
Core stability establishes:
|
- firm base of support for extremities
- mechanical support for vulnerable lumbar/lumbosacral region |
|
|
The most inferior end of the vertebral column is specialized for what two functions?
|
- lumbosacral junction and SI joints must transfer large forces from body weight and activated muscle through the pelvis to the lower extremities
- interacting mechanically with the hip joints (pelvis or femurs) to maximize movement of the trunk |
|
|
Pain with limited ROM anywhere within the vertebral column can originate from:
|
- tight/weak muscles
- torn ligaments - herniated discs - bone spurs compressing nerve roots - inflamed joints - combination of any/all of the above |
|
|
When lifting, why should one attempt to maintain the external load as close to the body as possible?
|
to minimize the external moment arm, thereby reducing the torque and force demands on back muscles
|
|
|
Where is it ideal (although not always possible) to hold the load while lifting?
|
between the knees
|
|
|
Why should one attempt to lift with the lumbar spine as close as possible to a neutral lordotic posture (avoiding extreme flexion and extension)?
|
- vigorous contraction of back extensors with the lumbar spine maximally flexed can damage intervertebral discs
- vigorous contraction of back extensors with the lumbar spine maximally extended may damage facet joints |
|
|
What can lifting with minimal-to-moderate flexion in the lumbar spine do?
|
possibly reduces force demands on extensor muscles
|
|
|
What can lifting with minimal-to-moderate extension in the lumbar spine do?
|
places the apophyseal joints nearer to their close-packed position, providing greater stability
|
|
|
When lifting, what muscles should be used to minimize the force demands on the low back muscles
|
hip and knee extensors
|
|
|
Why should one avoid twisting while lifting?
|
torsional forces on the vertebrae can lead to HNP
|
|
|
Why should one lift slowly and smoothly?
|
to reduce the large peak force generated in the muscles and connective tissues
|
|
|
Why should one lift with a wide base of support?
|
to increase stability and reduce chance of falling or slipping
|
|
|
Which of the following terms best describes anterior translation of the jaw? ***
a. lateral excursion b. elevation c. protrusion d. retrusion |
c. protrusion
|
|
|
Which of the following bones forms the upper jaw? ***
a. mandible b. maxillae c. sphenoid d. temporal |
b. maxillae
|
|
|
Which of the following muscles is primarily involved with opening the mouth? ***
a. temporalis b. masseter c. medial pterygoid d. lateral pterygoid (inferior head) |
d. lateral pterygoid (inferior head)
|
|
|
Widely opening the mount requires ____ of the mandibular condyle. ***
a. anterior translation (protrusion) b. posterior translation (retrusion) c. little movement d. lateral excursion |
a. anterior translation (protrusion)
|
|
|
Activation of the right medial pterygoid and right lateral pterygoid will cause: ***
a. lateral excursion of the mandible to the right b. lateral excursion of the mandible to the left c. simultaneous activation of the infrahyoid muscles d. the hyoid bone to drop 1-2 inches toward the sternum |
b. lateral excursion of the mandible to the left
|
|
|
Which of the following muscles attaches proximally to the zygomatic arch? ***
a. medial pterygoid b. lateral pterygoid c. masseter d. temporalis |
c. masseter
|
|
|
Which of the following bones make up the lower jaw? ***
a. sphenoid b. mandible c. maxillae d. zygomatic |
b. mandible
|
|
|
The total volume of air that can be moved in and out of the lungs on maximal forced inspiration and maximal forced expiration is called: ***
a. tidal volume b. vital capacity c. expiratory reserve volume d. inspiratory reserve volume |
b. vital capacity
|
|
|
Which of the following is considered the most important muscle of inspiration? ***
a. internal intercostals b. diaphragm c. scalenes d. external intercostals |
b. diaphragm
|
|
|
Persons with chronic obstructive pulmonary disease (COPD) often have a barrel-chested appearance because: ***
a. air becomes trapped in the lungs at the end of quiet or forced expiration b. of significant hypertrophy of the abdominal obliques c. of excessive calcium buildup within the rib cage d. of paralysis of the diaphragm |
a. air becomes trapped in the lungs at the end of quiet or forced expiration
|
|
|
According to Boyle's law, as the volume of a system increases: ***
a. the pressure within that system increases proportionally b. the pressure within that system decreases proportionally c. the pressure within that system remains constant |
b. the pressure within that system decreases proportionally
|
|
|
The scalenes are able to assist with inspiration: ***
a. by depressing the upper ribs and superior aspect of the sternum b. by elevating upper ribs and sternum c. by depressing the lower ribs and lower aspect of the sternum d. by lowering the floor of the thoracic cavity |
b. by elevating upper ribs and sternum
|
|
|
Which of the following statements is true? ***
a. quiet expiration is primarily driven by the elastic recoil of the ribs and surrounding connective tissues b. forced expiration involves active contraction of the abdominal muscles c. any muscle that increases intrathoracic volume can be considered a muscle of inspiration d. a and b e. all of the above |
e. all of the above
|
|
|
Expiration is the result of a decrease in intrathoracic volume. ***
a. true b. false |
a. true
|
|
|
The temporalis muscle is primarily involved with depression of the mandible. ***
a. true b. false |
b. false
elevation |
|
|
Contraction of the diaphragm expands intrathoracic volume in three diameters: vertical, medial-lateral and anterior-posterior. ***
a. true b. false |
a. true
|
|
|
The volume of air moved in and out of the lungs during each ventilation cycle is called the tidal volume. ***
a. true b. false |
a. true
|
|
|
Retrusion describes an anterior translation of the mandible. ***
a. true b. false |
b. false
protrusion is anterior, retrusion is posterior |
|
|
The masseter, medial pterygoid, and temporalis muscles are all involved with the action of closing the mouth. ***
a. true b. false |
a. true
|
|
|
Reduction of the intrathoracic volume will cause air to be drawn into the lungs. ***
a. true b. false |
b. false
Reduction of volume would increase pressure and push air out; reduction of intrathoracic pressure will cause air to be drawn in |
|
|
What is mastication?
|
the process of chewing, tearing, and grinding food with the teeth
|
|
|
Each jaw is equipped with ____ of TMJs.
|
a pair/two
|
|
|
Pain originating in the TMJ is often referred to other areas and perceived as:
|
headache or neck pain
|
|
|
Which is the largest facial bone?
|
mandible
|
|
|
How is the mandible attached to the cranium?
|
it is suspended by muscles, ligaments, and the TMJ capsule
|
|
|
What muscles attach at the angle of the mandible?
|
- masseter
- medial pterygoid |
|
|
Which two structures articulate to form the TMJ?
|
- mandibular condyle of mandible
- mandibular fossa of the temporal bone |
|
|
Does the mandible articulate with the maxilla?
|
nope, with the temporal bone
|
|
|
What two processes form the zygomatic arch?
|
the zygomatic process of the temporal bone and the temporal process of the zygomatic bone (cheek bone)
|
|
|
How is the maxilla formed?
|
by the union of the left and right maxillae
|
|
|
The hyoid bone is located at the base of the throat, just anterior to the....
|
third cervical vertebra
|
|
|
What is the purpose of the hyoid bone, and what is unique about it?
|
- it serves as an attachment for several muscles involved with moving the tongue, swallowing, and opening the jaw
- it is the only bone in the body that doesn't articulate with any other bone |
|
|
What is the function of the articular disc of the TMJ?
|
- provides joint stability
- reduces joint contact pressure - helps safely guide the condyle across the rough articular eminence of the temporal bone |
|
|
What are the primary motions of the TMJ?
|
- protrusion (protraction)
- retrusion (retraction) - lateral excursion - elevation - depression |
|
|
For what is lateral excursion of the TMJ important?
|
for grinding food between teeth
|
|
|
What provides stability to the TMJ during chewing motions?
|
- fibrous joint capsule and
- lateral ligament |
|
|
How far, on average, can an adult open his/her mouth?
|
slightly more than 2 inches
[given as 3 knuckles (PIP joints)] |
|
|
Fully depressing the mandible requires....
|
- extreme anterior translation (protrusion) of each mandibular condyle relative to its mandibular fossa
- normally the articular disc translates anteriorly along with each mandibular condyle, helping to properly guide the motion |
|
|
What are the primary muscles of the TMJ?
|
- masseter
- temporalis - medial pterygoid - lateral pterygoid |
|
|
What is the shared innervation of all TMJ muscles?
|
cranial nerve V (Trigeminal)
|
|
|
Masseter OAIN
|
O - zygomatic arch
I - external mandible between angle and coronoid process of ramus N - cranial nerve V (trigeminal) A - bilateral: elevation of mandible (closing the mouth) unilateral: ipsilateral excursion |
|
|
Temporalis OAIN
|
O - temporal fossa
I - coronoid process and anterior edge of ramus of mandible N - cranial nerve V (trigeminal) A - bilateral: elevation of mandible (closing the mouth), retrusion unilateral: ipsilateral excursion |
|
|
Medial pterygoid OAIN
|
O - medial surface of lateral pterygoid plate
I - internal surface of the angle and ramus of mandible N - cranial nerve V (trigeminal) A - bilateral: elevation of mandible (closing the mouth) unilateral: contralateral excursion |
|
|
Lateral pterygoid OAIN
|
O - superior head: greater wing of sphenoid
inferior head: lateral surface of lateral pterygoid plate I - near mandibular condyle; superior head also attaches to articular disc of TMJ N - cranial nerve V (trigeminal) A - bilateral: depression of mandible (opening the mouth--inferior head only); protrusion of the mandible unilateral: contralateral excursion |
|
|
Together, how much biting force can the medial pterygoid and masseter produce?
|
almost 100 lbs
|
|
|
Name the suprahyoid muscles
|
- digastric
- geniohyoid - mylohyoid - stylohyoid |
|
|
Name the infrahyoid muscles
|
- omohyoid
- sternohyoid - thyrohyoid - sternothyroid |
|
|
What are the secondary muscles of mastication?
|
- suprahyoids
- infrahyoids |
|
|
Function of the suprahyoid muscles?
|
depression of mandible
|
|
|
Function of infrahyoid muscles?
|
stabilization of hyoid bone
|
|
|
Digastric O, I
Geniohyoid O, I Mylohyoid O, I Stylohyoid O, I |
- anterior belly: internal surface of mandible; posterior belly: mastoid process
- midline of internal mandible - internal surface of body of mandible - styloid process of temporal bone all insert on the hyoid |
|
|
Omohyoid O, I
Sternohyoid O, I Sternothyroid O, I Thyrohyoid O, I |
- superior border of the scapula, near scapular notch
- manubrium and medial clavicle - manubrium - thyroid cartilage all attach to hyoid, except sternothyroid (thyroid cartilage) |
|
|
Conservative treatments for TMD
|
- exercise and postural correction
- biofeedback/relaxation - use of cold/heat - patient education - joint mobilization - ultrasound - behavioral modification - intraoral appliances (splints) |
|
|
Opening the mouth involves:
|
- contraction of inferior head of lateral pterygoid (protrusion)
- assisted by gravity and the suprahyoids (depression) |
|
|
Closing the mouth involves:
|
- strong forces from masseter, medial pterygoid and temporalis
|
|
|
Lateral excursion involves:
|
- masseter (ipsilateral)
- temporalis (ipsilateral) - medial pterygoid (contralateral) - lateral pterygoid (contralateral) |
|
|
What is the average total lung capacity for a normal adult?
|
5 1/2 liters of air
(most of this capacity is unused during normal breathing) |
|
|
What is the average tidal volume for a normal adult?
|
1/2 liter
|
|
|
What is inspiratory reserve volume?
|
the amount of air that can be taken into the lungs (above the tidal volume) upon forced inspiration
|
|
|
What is the expiratory reserve volume?
|
the amount of air that can be pushed out of the lungs (beyond the tidal volume) upon forced expiration
|
|
|
What is vital capacity?
|
the total volume of air that can be moved into and out of the lungs
|
|
|
What is Boyle's law?
|
- the law behind much of the physics governing inspiration and expiration
- states that volume and pressure of a gas are inversely proportional (e.g., larger volume = lower pressure, and vice versa; thus when the ribcage expands, the larger volume forces a drop in pressure and the lungs fill) |
|
|
Is quiet expiration an active or passive process?
|
passive, carried out by the decrease in intrathoracic volume caused by the elastic recoil of the lungs, thorax, connective tissues, etc.
|
|
|
Is forced expiration an active or passive process?
|
active; involves active contraction of expiratory muscles such as the abdominals for coughing, sneezing, forcefully exhaling, etc.
|
|
|
Is quiet inspiration an active or passive process?
|
both quiet and forced inspiration are active processes
|
|
|
How is the intrathoracic volume increased?
|
- elevation of ribs
- elevation and forward expansion of sternum - increasing vertical diameter of the thorax, caused by contraction of the diaphragm |
|
|
What muscles contribute to forced expiration?
|
any that assist with
- depression of the ribs - depression and pulling in on the sternum - decreasing the vertical diameter of the thorax |
|
|
What are the primary muscles of inspiration? Why are they considered primary?
|
- diaphragm
- scalenes - intercostals because they are active during all intensities of breathing (quiet or forced) |
|
|
Diaphragm OAIN
(1413 Ex3) |
O - inner surfaces of ribs 6-12, posterior xyphoid process, bodies of L1-L3
I - central tendon near dome N - phrenic nerve (C3-C5) A - primary muscle of inspiration |
|
|
External intercostals OAIN
|
O & I - inner surfaces of ribs, originating on inferior borders; inserting on superior border of rib below--run obliquely toward midline
N - intercostal nerves (T2-T12) A - assist with inspiration by elevating ribs and expanding thorax |
|
|
Internal intercostals OAIN
|
O & I - inner surfaces of ribs, originating on superior borders; inserting on inferior border of rib above; deep to external intercostals and run perpendicular to them
N - intercostal nerves (T2-T12) A - assist with forced expiration by depressing ribs |
|
|
How do the anterior, middle, and posterior scalenes assist with respiration?
|
they assist inspiration by elevating the upper ribs
|
|
|
What components are incorporated into COPD?
|
- chronic bronchitis
- emphysema - asthma |
|
|
What are the symptoms of COPD?
|
- chronic inflammation and narrowing of the bronchioles
- chronic cough - mucus-filled airways, with over-distention and destruction of alveolar walls |
|
|
What is a significant complication of COPD?
|
- loss of natural elastic recoil within the lungs and collapse of the bronchioles
- as a result, air remains trapped in the lungs at the end of quiet/forced expiration, causing hyperinflation of the lungs and often giving a barrel-chested appearance |
|
|
Persons with COPD often depend upon _____ _____ to breathe.
|
accessory muscles (e.g., scalenes, sternocleidomastoid, pectoralis minor)
|
|
|
What are the muscles of forced expiration?
|
- the four abdominal muscles
- internal intercostals |
|
|
Which of the following joints are most proximal within the hand? ***
a. MCP joints b. PIP joints c. DIP joints d. CMC joints |
d. CMC joints
|
|
|
Which of the following statements is true regarding abduction of the index finger? ***
a. this motion occurs in the frontal plane b. this motion describes the index finger moving away from the middle finger (toward the thumb) c. this motion describes the index finger moving toward the middle finger d. a and b e. b and c |
d. a and b
|
|
|
Flexion of the thumb: ***
a. occurs in the sagittal plane b. occurs in the frontal plane c. occurs in the horizontal plane d. occurs about a longitudinal axis of rotation e. c and d |
b. occurs in the frontal plane
|
|
|
Which of the following joints can perform flexion and abduction? ***
a. CMC joint of the thumb b. DIP joints of digits 2 to 5 c. MCP joints of digits 2 to 5 d. a and b e. a and c |
e. a and c
|
|
|
The motion of touching the thumb to the other fingertips is called: ***
a. abduction b. hypothenar flexion c. opposition d. reposition |
c. opposition
|
|
|
The tendons of the extrinsic finger extensors: ***
a. all course posterior to the medial-lateral axis of rotation of the MCP joints b. all course anterior to the medial-lateral axis of rotation of the wrist c. all blend with a special set of connective tissues called the extensor mechanism d. a and b e. a and c |
e. a and c
|
|
|
Which of the following muscles is not part of the hypothenar eminence? ***
a. flexor digiti minimi b. abductor digiti minimi c. opponens pollicis d. opponens digiti minimi |
c. opponens pollicis
|
|
|
The primary function of the muscles of the thenar eminence is: ***
a. curl the ulnar border of the hand such as when cupping b. position the thumb in varying amounts of opposition to facilitate grasping c. extend the thumb and ulnarly deviate the wrist d. flex the MCP joints of digits 2 to 5 |
b. position the thumb in varying amounts of opposition to facilitate grasping
|
|
|
Which of the following is not an action of the lumbrical muscles? ***
a. flexion of the MCP joints of the fingers b. extension of the DIP joints of the fingers c. flexion of the PIP joints of the fingers d. extension of the PIP joints of the fingers |
c. flexion of the PIP joints of the fingers
|
|
|
The primary function of the dorsal interossei muscles is: ***
a. abduction of the fingers b. adduction of the fingers c. flexion of the PIP and DIP joints d. flexion of the DIP joints |
a. abduction of the fingers
|
|
|
Injury or paralysis of the ulnar nerve will significantly affect the muscles of the hypothenar eminence. ***
a. true b. false |
a. true
|
|
|
Basilar joint osteoarthritis refers to arthritis of the CMC joint of the thumb. ***
a. true b. false |
a. true
|
|
|
Injury or paralysis to the median nerve will likely result in an inability to oppose the thumb. ***
a. true b. false |
a. true
|
|
|
An individual without functional finger flexors may perform a tenodesis grip through activation of the wrist extensors. ***
a. true b. false |
a. true
|
|
|
Paralysis of the radial nerve will primarily result in an inability to oppose the thumb. ***
a. true b. false |
b. false
median nerve |
|
|
The structure of the CMC joint of the thumb is that of a hinge joint. ***
a. true b. false |
b. false
saddle |
|
|
Hyperextension of the MCP joints of the fingers is primarily limited by tension in the palmar (volar) plates. ***
a. true b. false |
a. true
|
|
|
A strong pinching activity such as when cutting with scissors involves strong activation of the adductor pollicis muscle. ***
a. true b. false |
a. true
|
|
|
Extrinsic muscles of the hand have their proximal attachments on the forearm or arm, but attach distally to a structure within the hand. ***
a. true b. false |
a. true
|
|
|
Without activation of the lumbricals and interossei muscles, contraction of the extensor digitorum results in clawing of the fingers. ***
a. true b. false |
a. true
|
|
|
What is a ray?
|
a metacarpal bone and its associated phalanges
|
|
|
What is a common site of fracture in the hand?
|
neck of the metacarpal
|
|
|
How does the position of the thumb's metacarpal differ from that of the other metacarpals?
|
- the thumb's metacarpal is oriented in a different plane
- it is rotated almost 90 degrees medially relative to the other digits; palmar surface faces toward midline of the hand - it is also more anteriorly positioned, which allows it to sweep freely across the palm |
|
|
How do the sides of the thumb face?
|
- dorsal surface faces laterally
- palmar surface faces medially - radial surface faces anteriorly - ulnar surface faces posteriorly |
|
|
Which phalanges have heads?
Tuberosities? |
- proximal and middle phalanges
- distal phalanges only |
|
|
What structures support the arched curvature of the palmar surface of the hand?
|
- proximal transverse arch (distal row of carpal bones; carpal tunnel)
- distal transverse arch (through MCPs) - longitudinal arch (2nd and 3rd rays) |
|
|
How is abduction and adduction described with respect to digits 2-5?
|
as motion away from or toward the middle digit
|
|
|
How are flexion, extension, abduction, and adduction described with respect to the thumb?
|
- palmar surface in frontal plane across palm
- back towards anatomical position - forward movement away from palm - back to anatomical position |
|
|
Where does the basis for all movements within the hand start?
|
CMC joints
|
|
|
What pathology of the hand receives more surgical attention than any other osteoarthritis-related condition of the upper limb?
|
basilar joint osteoarthritis
(common among needlepointers and cow milkers) |
|
|
Supporting structures of the MCP joints
|
- capsule
- radial and ulnar collateral ligaments - cross MCP in oblique palmar direction; limit abduction and adduction, become taut on flexion - fibrous digital sheaths - form tunnels or pulleys for extrinsic finger flexors; contain synovial sheaths to help lubrication - palmar (volar) plates - thick fibrocartilage ligaments that cross palmar side of each MCP; limit hyperextension of MCPs - deep transverse metacarpal ligaments - 3 ligaments that merge into a wide, flat structure that interconnects and loosely binds metacarpals 2-5 |

