![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
116 Cards in this Set
- Front
- Back
|
use r/t drinking |
use- methods for ingesting mind-altering substance
moderate drinking-- men <2 drinks/day, < 10 drinks/wk, 4 drink tolerance women/65+ <1 drink/day, < 7/wk, 3 drink tolerance “at risk” or “hazardous” drinking-- men >4 drinks per occasion, >10 drinks/wk women >3 drinks per occasion, >7 drinks/wk 2+ on CAGE Questions binge-- 5+ drinks within 2 hours heavy-- 5 +drinks on 5+ occasions within 30 days |
|
|
abuse
|
abuse– use of alcohol or drugs for purpose of intoxication
1+ of the following within 12 month period //// -recurrent use, resulting in failure to fulfill major role obligations at work, home, school -recurrent use in situations that are physically hazardous -recurrent substance-related legal problems -continued use despite persistent or recurrent social or interpersonal problems caused or exacerbated by effects of substance |
|
|
dependence
|
dependence- continued substance use despite significant negative consequences
3 or more of the following within 12 month period //// -tolerance -withdrawal -taking the substance in large amounts or over a longer period of time than was intended -persistent desire or unsuccessful efforts to cut down or control use -much time spent in activities necessary to obtain or use the substance -reduction or cessation of important social, occupational, or recreational activities -continued use despite knowledge of persistent or recurrent physical or psychological problems likely caused or exacerbated by the substance |
|
|
intoxication
|
reversible substance- specific syndrome due to recent ingestion of or exposure to a substance
clinically significant maladaptive behavioral or psychological changes due to effect of substance on CNS, developing during or shortly after use of substance symptoms not due to general medical condition, nor better accounted for by another mental disorder |
|
|
withdrawal
|
withdrawal- physical and/or psychological readjustment accompanying discontinuation of mind altering substance
development of substance-specific syndrome due to cessation or reduction in substance use, previously heavy and prolonged syndrome causing significant distress or impairment in social, occupational, or other important areas of functioning symptoms not due to general medical condition, nor better accounted for by another mental disorder |
|
|
tolerance / addiction / detoxification / relapse
|
tolerance- need for increasing amounts of substance to achieve desired effect
addiction- physiological, psychological and behavioral dependence on drugs or alcohol detoxification - process of safely & effectively withdrawing from addictive substance relapse- recurrence of substance dependent behavior following period of abstinence |
|
|
substance abuse etiology
|
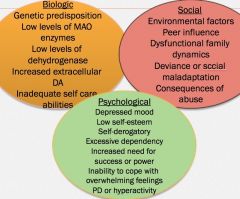
biological--
genetic influence reward pathway- VTA >> nucleus accumbens >> prefrontal cortex psychological-- personality traits, e.g. self-centeredness, inner dishonesty, addictive personality behavioral-- childhood conduct problems social-- family peer use and affiliation environmental |
|
|
addiction severity index (ASI)
|
used to assess substance abuse and related problems, can be administered by MS, RN, or psych tech
|
|
|
alcohol
|
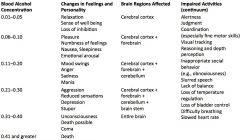
-sedative anesthetic
-liver metabolizes 1 oz of liquor/hour (varies) tolerance & long term abuse-- -rapid metabolism and lower sedation, motor and anxiolytic effects -higher BAL before intoxication -cerebellar degeneration, impaired coordination, unsteady gait, fine tremor, sleep disorders |
|
|
alcohol intoxication
|
blood alcohol level ≥ 0.08%
|
|
|
What affects blood alcohol content?
|
food; absorption is faster when the stomach is empty
body weight and build; greater body weight provides a greater volume in which alcohol can be distributed gender; females have smaller body mass and a higher proportion of body fat than males |
|
|
progressive effects of alcohol
|
|
|
|
alcohol-induced amnestic DO
|
wernicke’s encephalopathy- degenerative brain disorder caused by thiamine deficiency,
-acute -reversible symptoms -ataxia, confusion, ocular motility abnormalities korsakoff’s amnestic syndrome- inability to acquire new information or retrieve memories -chronic -confabulation; making up stories b/c you can’t remember the truth -irreversible symptoms -follows Wernickes wernicke-korsakoff syndrome is different stages of the same disorder |
|
|
alcohol withdrawal syndrome
|
onset/duration--
within 4-12 hours, symptoms usually peak in intensity during 2nd day of abstinence and improve by 4th/5th day acute anxiety, insomnia, autonomic dysfunction may persist for up to 3-6 months symptoms-- (+)BP, (+)HR, (+)temp diaphoresis mild anxiety/restlessness hand tremors or “shakes” adverse GI effects, e.g. n/v disorientation, confusion, seizures 3 stages-- mild, moderate, & severe (delirium tremens) RN should reorient patient and provide safe environment; previous withdrawals >> more withdrawals every subsequent attempt to quit |
|
|
delirium tremens
|
tachycardia
diaphoresis hypertension confusion tremor disorientation vivid hallucinations seizures resolves in 3-4 days goals for treatment-- -reduce symptoms -hospital stay is needed -anticonvulsant (phenobarbital) -sedatives to offset hallucinations |
|
|
acute treatment for alcohol withdrawal
|
1/ benzodiazepines sedate and reduce anxiety
2/ b vitamins- thiamine & folic acid 3/ magnesium sulfate- administer early, will reduce need for benzo & shorten hospital stay PRNs- antidepressants, sleep aids, antipsychotic |
|
|
non acute treatment for alcohol withdrawal
|
to help sustain AWS recovery--
-campral sedates part of brain that craves alcohol -antabuse- makes taste and smell of alcohol repulsive >> n/v s/p consumption -naltrexone reduces cravings -topamax |
|
|
other depressants
|
sedatives, hypnotics, & anxiolytics
barbiturates- CNS depressants used as anticonvulsants, sedatives, hynotics, and anesthetics; commonly abused and highly addictive benzodiazepines chloral hydrate- synthetic monohydrate of chloral with sedative, hypnotic, and anticonvulsive properties nonbarbiturate hypnotics- anesthetics, sleep aids |
|
|
benzodiazepines
|
valium, ativan, librium, xanax, klonipin
uses include schizophrenia, anxiety, and drug withdrawal **tapering is essential benzo withdrawal-- -anxiety rebound, i.e. tension, agitation tremors, insomnia, anorexia -autonomic rebound, i.e. HTN, tachycardia, sweating, hyperpyrexia -sensory excitement, i.e. paresthesias, illusions -motor excitation, i.e. hyperreflexia, myoclonus, fasciculations, convulsions -cognitive excitation, i.e. nightmares, delirium, hallucinations |
|
|
stimulants
|
cocaine
bath salts amphetamines nicotine ecstacy, meth |
|
|
cocaine effects / intoxication / withdrawal
|
effects--
sudden burst of alertness, energy and self-confidence; high lasts ~10-20 minutes, then let down and cravings intoxication-- CNS stimulation >> depression restlessness >> tremors, agitation >> seizures >> respiratory depression >> cardiac arrest >> death withdrawal-- depletion of neurotransmitters >> (+) sleep >> “crash” dopamine depletion causes “post-coke blues” |
|
|
post-coke blues
|
anxiety
depression anergia decreased libido suicidality anhedonia (-) concentration cocaine craving sleep disturbances with rebound REM |
|
|
cocaine biological effects
|
short term--
(+) dopamine (+) activity in nucleus accumbens (+) body temperature, HR, BP constricted blood vessels dilated pupils long term-- dopamine depletion >> effect on reward system >> anhedonia, can be irreversible |
|
|
cocaine treatment
|
no FDA-approved medications
antidepressants dopamine agonists a cocaine vaccine that prevents entry of cocaine into the brain holds great promise for reducing the risk of relapse behavioral interventions-- motivational incentives CBT therapeutic communities |
|
|
bath salts
|
formulation--
one or more synthetic chemicals related to cathinone, an amphetamine-like stimulant found naturally in the khat plant MDPV, mephedrone, and methylone are the chemicals most often found in bath salts onset is 15 minutes; high is 4-6 hours short-term effects-- severe paranoia suicidal thoughts agitation combative/violent behavior confusion hallucinations/psychosis (+) HR, HTN, chest pain death or serious injury |
|
|
amphetamines
|
-block reuptake of norepinephrine and dopamine
-similar to cocaine, affect peripheral nervous system -can be used for ADHD intoxication-- agitation, aggression, psychosis, impaired judgment, elevated HR & BP, dilated pupils, diaphoresis withdrawal-- anxiety, depression, irritability, cravings, insomnia/hypersomnia, psychosis, suicidal ideation |
|
|
nicotine
|
effects--
mental stimulation, muscle relaxant decrease anxiety, the act of smoking ADEs-- chronic lung disease, cardiovascular disease, stroke, cancer, tolerance, addiction, adverse pregnancy outcomes withdrawal-- cravings, irritability, anxiety, difficulty concentrating, increased appetite/weight gain, headaches, insomnia, decreased heart rate |
|
|
opiates
|
opiods of natural origin- opium, morphine, codeine
opiods derivatives- dilaudid, oxycodone, vicodan synthetic- demerol, darvon, fetanyl, talwin effects-- -relieve pain, cough, diarrhea -sedation -euphoria, pleasure -tolerance and physical dependence -withdrawal effects are more severe in children |
|
|
opiates withdrawal symptoms
|
yawning, insomnia, irritability, rhinorrhea, panic, diaphoresis, cramps, nausea, vomiting, diarrhea, muscle aches, bone pain(long bones), piloerection, dilated pupils
|
|
|
opioid substitutes / opioid antagonists
|
substitutes--
buprenorphine methadone antagonist-- narcan naltrexone |
|
|
inhalants
|
-euphoria, disinhibition
-common household products ADEs-- respiratory depression, cardiac arrhythmias, coma, death |
|
|
cannabis
|
euphoria, relaxation, altered consciousness, increased sociability
ADEs-- amotivational syndrome, memory impairments, coordination problems, slows reaction time, increased appetite, paranoia, social withdrawal, visual hallucinations, suicide attempts withdrawal-- restlessness, irritability, insomnia, loss of appetite, depressed mood |
|
|
ecstacy aka MDMA
|
euphoria, ↑ energy, ↑ self-confidence, ↑ sociability
ADEs-- -serotonin syndrome -malignant hyperthermia → muscle breakdown, cardiovascular and renal failure -confusion, depression, sleep disturbance -severe anxiety, paranoia and psychosis -memory impairments, difficulty concentrating withdrawal-- fatigue, loss of appetite, depressed feelings, difficulty concentrating |
|
|
meth
|
↑ activity level used in rural community to increase productivity (e.g. farmers), ↓ appetite, euphoria
ADEs-- (+) wakefulness, dry mouth, nausea, vomiting, diarrhea, loss of appetite, increased physical activity, increased respiration, irritability, confusion, tremors, anxiety, amphetamine psychosis, repetitive behaviors, sensation of insects crawling under the skin, obsessive scratching, violent behavior, CVA, arrhythmia, cardiac arrest, seizures, death withdrawal-- drug craving, depressed mood, disturbed sleep patterns, increased appetite |
|
|
assessment for drug use
|
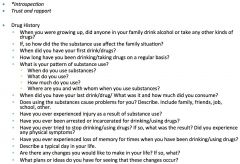
gait disturbance, slurred speech, hyperactivity, poor eye contact, pupil dilation/constriction
defense mechanisms-- denial & projection voluntary v. involuntary intrinsic v. extrinsic |
|
|
bio assessment for drug use
|
-blood alcohol, i.e. toxicology screen, LFTs
-skin changes, i.e. rosacea, rhinophima- capillary damage in your extremity, bruises, spider angiomata -lungs, associated COPD changes -heart, i.e. arrhythmias, tachycardia, cardiomegaly -abdomen, i.e. liver enlargement jaundice, tenderness, ascites -extremities, i.e. vascular changes, nicotine stains, clubbing, track marks |
|
|
nursing diagnoses for drug use
|
risk for...
-injury e.g. falls -suicide -other-directed violence -deficient fluid volume -imbalanced Nutrition -anxiety -disturbed self-esteem* -disturbed sleep pattern -ineffective coping -ineffective health maintenance -ineffective denial |
|
|
nursing interventions for drug use
|
during detoxification--
monitor vital signs administer medication monitor intake and output fluids, nutrition seizure precautions -maintain accepting attitude and nonjudgmental approach -teach pt and family about substance abuse regarding symptoms, dependence, relapse, dangers -encourage verbalization, expression of feelings -review necessary lifestyle changes -stress management and coping skills |
|
|
drug screening
|
**always screen, important throughout life cycle
screening tools-- AUDIT for detailed direct screening CAGE, T-ACE for further assessment |
|
|
CAGE
|
-have you ever felt you should CUT down on your drinking
-have people ANNOYED you by criticizing your drinking -have you ever felt bad or GUILTY about your drinking -have you ever had a drink in the morning as an EYE-OPENER to get rid of a hangover |
|
|
intermittent explosive disorder
|
**discrete episodes of failing to resist aggressive impulses resulting in serious assaultive acts or property destruction >> followed by a phase of regret for losing control
epileptoid personality- this loss of control is not part of person’s normal personality; patients describe this as episodes of attacks -disregulation of sertononin -degree of aggression grossly out of proportion to provocation or stressor |
|
|
kleptomania
|
**recurrent failure to resist impulse to steal object that is not needed
-increased tension before theft -pleasure, gratification, or relief at time of theft -not done for monetary gain, not planned, and does not involve others -comorbidity w/ head traumas |
|
|
pathologic gambling
|
**persistent and maladaptive gambling behavior
-increased amounts of money needed to achieve excitement -unsuccessful efforts to stop, cut back, or control -restlessness and irritability with attempts to control or cut back -means of escape from problems or mood -lying to family and others to conceal involvement -commission of illegal acts to finance behavior -significant relationships, job, or opportunities jeopardized or lost -reliance on others for relief of poor financial situation DSM5 recategorized this in substance related/addictive disorders; same dopamine release r/t substance related/addictive disorders |
|
|
pyromania
|
**multiple episodes of deliberate and purposeful fire setting
-tension or affective arousal before act -pleasure gratification or tension relief with fire setting, watching its effects or participating in aftermath -not done for monetary gain; expression of ideology, anger, or vengeance; concealing criminal activity; improving living conditions; or as a response to hallucination or delusion -fascination with, interest in, curiosity about, or attractions to fires |
|
|
trichotillomania
|
**recurrent pulling of one’s hair with subsequent hair loss
-increased during stress and relaxation periods -increased tension immediately before act and with attempts to resist urge -gratification, pleasure, or relief with act -treatment w/ dermatology (e.g. topical steroid), hypnotherapy, can be covered up with hair pieces, etc. -women are 4x more likely than men, onset ~age17 |
|
|
personality clusters
|
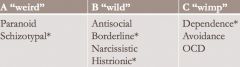
A- odd or eccentric behavior
e.g. paranoid, schizoid, schizotypal B- dramatic, emotional, or erratic behavior e.g. antisocial, borderline, histrionic, narcissistic C- anxious or fearful behavior; insecurity and inadequacy e.g. avoidant, dependent, OCD |
|
|
personality v. personality disorder
|
personality- complex pattern of characteristic outside person’s awareness that influences person’s way of coping, thinking, feeling; stable & predictable
personality disorder-- inflexible, enduring, pervasive, maladaptive personality patterns or traits that cause significant functional impairment or subjective distress |
|
|
maladaptive personality patterns
|
-lack of insight
-does not accept consequences of behavior -want to change environment rather than changing behavior -unable to relate to others |
|
|
egosytonic v. egodystonic
|
egosyntonic- behavior, values, feelings which are in harmony/acceptable to needs/goals of ego; consistent w/ one’s image
egodystonic- opposite, in conflict with needs and goals of ego |
|
|
DSM-IV criteria for personality disorder
|
enduring pattern of inner experience & behavior that deviates markedly from expectations of individual’s culture; manifested in 2+ of the following areas--
cognition- unable to consider consequences of action before acting (e.g. self harm/injury) affect- may have extreme emotional reaction interpersonal functioning- have trouble perceiving events, actions, etc., >> negative misinterpret >> inappropriate reaction impulse control |
|
|
psych eval/testing for personality DO
|
1/ minnesota multiphasic personality inventory-2
2/ millon clinical multiaxial inventory-III *patients should also have toxicology screening |
|
|
personality DO epidemiology
|
10% – 15% of US population; under reported
prevalence gender related -lifelong with onset in adolescence or early adulthood -commonly overlap with other psychiatric disorders |
|
|
paranoid DO
|
**distrust and suspiciousness toward others based on unfounded beliefs that others want to harm, exploit or deceive the person
-often hostile, irritable, angry; may have legal disputes -neither desires nor enjoys close relationships -blame others for shortcomings and do not take responsibility for their own feelings and behaviors RN diagnosis-- disturbed thought processes interventions-- -brief one on one session -be factual/objective- e.g. when late—apologize rather than give excuse -respect personal space -role-playing -meds include antidepressants and low-dose antipsychotics -psychotherapy, cognitive therapy |
|
|
schizoid DO
|
**emotional detachment, disinterest in close relationships, and indifference to praise or criticism
-appears cold and aloof -exhibits affective flattening -often uncooperative RN diagnosis-- risk for social isolation interventions-- -develop rapport -antidepressants |
|
|
schizotypal DO
|
**odd beliefs leading to interpersonal difficulties
-magical thinking or perceptual distortions that are not clear delusions or hallucinations -paranoid ideation -inappropriate or constricted affect -eccentric appearance -few or no close friends -excessive social anxiety RN diagnosis-- disturbed thought process, risk for social isolation interventions-- -develop rapport -antidepressants and antipsychotics |
|
|
antisocial DO
|
**failure to conform to social norms
-repeated acts that are grounds for arrest -deceitfulness for profit or pleasure -impulsivity -reckless disregard for the welfare of others -consistent irresponsibility -lack of remorse; indifference, e.g. sociopaths RN diagnosis-- risk for other-directed violence interventions-- -set clear and realistic limits -develop rapport; appear calm and in control and speak in a nonprovocative, nonjudgmental tone -guard against being manipulated -avoid confrontations, power struggles -anger management treatment-- **no treatment of choice -group therapy; peer treatment b/c they respect each other -betablockers |
|
|
borderline DO
|
**frantic efforts to avoid real or imagined abandonment
-pattern of unstable, intense interpersonal relationships -dichotomous thinking “splitting” all or nothing -identity disturbance; depersonalizing -impulsivity -recurrent self mutilation and suicidal behavior -chronic feelings of emptiness -inappropriate, intensified affective anger responses -transient psychotic symptoms of paranoia and dissociation |
|
|
borderline DO treatment
|
RN diagnosis--
risk for self-directed violence, risk for self-mutilation, risk for suicide interventions-- -safety -set limits -“no self-harm” contract -behavior modification -SSRI **dialectical behavior treatment- mindfulness technique, social skills training |
|
|
histrionic DO
|
**emotional attention-seeking behavior, in which the person needs to be the center of attention
-inappropriate seductive/sexualized/provocative behavior, rapid shifting, and shallow emotional responses -use of physical appearance to draw attention to self -speech excessively impressionistic -suggestible and easily influenced -relationships considered more intimate than they really are |
|
|
narcissistic DO
|
**arrogance
-grandiose sense of self-importance -need for consistent admiration -consider themselves special and expect special treatment -lack of empathy for others that strains most relationships -sensitive to criticism |
|
|
avoidant DO
|
**social inhibition and avoidance of all situations that require interpersonal contact, despite wanting close relationships
-extreme fear of rejection -anxious in social situations -needs guaranteed signs of acceptance |
|
|
dependent DO
|
**extreme dependency in a close relationship with an urgent search to find a replacement when one relationship ends
**most common in clinical setting -clinging, demanding, submissive -fear, anxiety about losing others -hypersensitivity to rejection, decision making -avoid responsibility -low self-esteem interventions-- -trusting relationship -set limits -self-assessment treatment-- therapy, assertiveness training, medication |
|
|
obsessive-compulsive personality
|
**perfectionism with a focus on orderliness and control to the extent that the individual may not be able to accomplish a given task
-strive to keep the world predictable and organized; life is very regimented **differs from OCD- no obsessions/compulsions |
|
|
personality DO meds
|
A- antidepressants and low-dose antipsychotics
B- anticonvulsant mood stabilizing agents, MAOI’s C- antianxiety agents |
|
|
eating DO epidemiology
|
onset--
AN 14-16; BN 18-24 males account for 5-15% of patients and have later onset than females comorbidities-- depression, substance abuse, anxiety DO OCD is high risk for AN **social obstacles, suicide, death from physical complications, e.g. heart conditions, kidney failures |
|
|
eating DO etiology
|
genetic--
shared familial disposition, perfectionistic temperament; high rates of depression >> AN biological-- (+) endogenous opiods (endorphins from exercise) decrease satiety (-) brain derived neurotropic factor psychological-- -unconscious conflicts -separation issues, e.g. identity formation -regression to pre-puberty, repudiation of sexual development -overcompensation of unmet oral needs -family conflict -control issues |
|
|
anorexia nervosa (AN)
|
**potentially life-threatening
-weight fear -significant weight loss -body image disturbance -strenuous exercising -extreme perfectionism -peculiar food-handling patterns -amenorrhea (-) HR, BP, metabolic rate, and some hormones |
|
|
What are the two types of AN?
|
1/ restricting- without regular binge-eating or purging behavior
2/ binge-eating/purging behavior |
|
|
AN assessment
|
(-) BP
laboratory tests, EKG mental status menses history signs of dehydration and malnutrition--dry skin, flakiness, brittle nails tools-- the eating attitudes test SCOFF CHEAT |
|
|
lanugo
|
fine hair growth; related to hypothermia; can be found in AN--adaptive against cold because body weight is so low
|
|
|
AN hospitalization criteria
|
-rapid weight loss
-persistent bradycardia -systolic BP ≤ 80 mm Hg -hypothermia -electrolyte imbalance -cardiac arrhythmia -suicidal ideation -persistent sabotage or disruption of outpatient treatment -denial of disorder, need for treatment |
|
|
AN nursing diagnoses
|
-imbalanced nutrition
-anxiety -disturbed body image -ineffective coping -disturbed thought processes -interrupted family processes |
|
|
AN interventions
|
-promote weight gain is first priority
-frequent small portions -supervision during and after meals -negotiate adequate food intake -monitor VS, fluid intake/output -cognitive and behavioral strategies, i.e. interoceptive awareness -patient and family education -monitor for suicide |
|
|
AN medications
|
prozac- SSRI, does not work well b/c SSRI is stored in fat; not strong enough to modulate neurotransmitter imbalance in eating disorders; not used in acute phase >> can help with OCD tendency, comorbid depression and anxiety >> **patient must be motivated for treatment
antipsychotic may help w/ disturb processes; ADE include weight gain >> patient wouldn’t be compliant |
|
|
bulimia nervosa (BN)
|
**binge eating- consuming a lot of food in short amount of time
-purging -persistent self-evaluation; person describes as being out of control -high s/p binging more common; not as life threatening, outpatient treatment |
|
|
BN DSM-IV
|
recurrent episodes of binge eating
recurrent inappropriate compensatory behavior in order to prevent weight gain, e.g.-- -self-induced vomiting -misuse of laxatives, diuretics, enemas or other medication -fasting -excessive exercise binge eating and inappropriate compensatory behaviors both occur, on average, at least twice per week for 3 months self-evaluation is unduly influenced by body shape and weight the disturbance does not occur exclusively during episodes of AN |
|
|
What are the two types of BN?
|
1/ purging
2/ non-purging |
|
|
BN assessment
|
-person is not necessarily thin
-worn away teeth enamel due to acid reflux -hand calluses from inducing vomit -nutritional deficiency -dehydration, electrolyte imbalance -coarse voice -impaired gag reflex perform lab tests, EKG, and psychosocial evaluation |
|
|
BN nursing diagnoses
|
imbalanced nutrition
disturbed sleep pattern deficient knowledge disturbed thought processes powerlessness disturbed body image chronic low self-esteem |
|
|
BN interventions
|
-prozac
-therapeutic alliance -identify elimination patterns/cue elimination -promote behavior modifications -encourage recognition and verbalization of feelings -teach patient to keep journal -psychoeducation -assess and monitor for suicide -CCK released by gastric emptying, which decreases overtime after repeated binging; watch level and try to reset |
|
|
binge eating disorder (BED)
|
**like BN but does not have purging/compensations
>>10-30% of obese individuals have BED |
|
|
disordered eating screening
|
How many diets have you been on in the past year?
How often does your weight affect how you feel about yourself? How often do you feel you should be dieting? How often do you feel dissatisfied with your body? |
|
|
SCOFF
|
Do you make yourself SICK because you feel uncomfortably full?
Do you worry that you have lost CONTROL over how much you eat? Have you recently lost more than ONE stone (14 lb) in a 3-month period? Do you believe yourself to be FAT when others say you are too thin? Would you say that FOOD dominates your life? **each “yes” equals 1 point; a score of 2 indicates a likely diagnosis of anorexia nervosa or bulimia |
|
|
interoceptive awareness
|
the sensory response to emotional/visceral cues
patient do not have good connection w/ emotion >> work with patient to recognize and identify feelings |
|
|
somatic DO etiology
|
psychobiologic theory--
-heightened body sensations -increased autonomic arousal -identification of “patient” -perceived need to be sick, e.g. guilt genetic-- runs in the family CBT theory-- -anxiety expressed through somatization -cognitive distortions of benign symptoms psychoanalytic theory-- psychological source of ego conflict denied displacement of anxiety onto physical symptoms feeling pain is a way of atoning for actions sociocultural-- direct expression of emotions is unacceptable |
|
|
somatization DO / somatic symptom DO
|
DSM-IV- somatization DO
occurs before age 30 and persists for several years; patient presents w/ history of many symptom-- 1 pseudoneurologic, e.g. paralysis, parasthesia, seizure, dysphagia, impaired coordination 2 gastrointestinal, e.g. nausea, bloating, diarrhea, food intolerance 1 sexual erectile dysfunction, e.g. sexual/reproductive pain 4 pain symptoms, e.g. head, joints, chest DSM-5- somatic symptom DO excessive thoughts, feelings, or behaviors related to the somatic symptoms or associated health concerns as manifested by at least one-- -disproportionate and persistent thoughts about the seriousness of one’s symptoms -persistently high level of anxiety about health or symptoms -excessive time and energy devoted to these symptoms |
|
|
hypochondriasis / illness anxiety DO
|
DSM-IV- hypochondriasis
-unrealistic fear of serious illness -preoccupation persists despite medical evaluation and reassurance -physical symptoms may begin with sensitivity to vague physical sensations or mild physical symptoms DSM5- illness anxiety DO -preoccupation with having a serious illness -somatic symptoms not present or ,if so, mild in intensity -performs excessive health related behaviors or maladaptive avoidance **duration of at least 6 months for both DSMs |
|
|
primary v. secondary gains
|
primary- relieve of unconscious psychological conflict, wish, or need; as anxiety increases >> conversion to physical which decreases psychological stress
secondary gain- benefits of sickness (missing work, comfort of others, social obligations) |
|
|
conversion DO
|
-clear, identifiable psychological factor
-symptoms often related to primary gain **characterized by-- sensory dysfunction motor system dysfunction la belle indifference |
|
|
body dysmorphic DO
|
categorized in obsessive-compulsive and related DO
-preoccupation with defect in appearance -frequently check defects, avoid reminders, seek reassurance from others or attempt to improve defect -social isolation, associated with depression and suicidal ideation |
|
|
somatoform nursing diagnoses
|
-fatigue
-pain -insomnia -anxiety -ineffective sexuality patterns -ineffective coping -ineffective therapeutic regimen management -impaired social interactions -risk for caregiver role strain -disabled family coping |
|
|
somatoform interventions
|
-maintain nurse-patient relationship
-encourage identification and expression of feelings -focus on problem solving -assertiveness training -health teaching -avoid reinforcing secondary gains |
|
|
somatoform medications
|
treat comorbidities--
depression- antidepressants anxiety- benzodiazepines |
|
|
factitious DO
|
**deliberate production or exaggeration of symptoms of a physical or mental illness in order to assume sick role
-hospitalization is primary objective -compulsive quality |
|
|
munchausen syndrome
|
**factitious DO imposed on self
-external incentives for behavior are absent, e.g. economic gain, avoiding legal responsibility, or improving physical well-being |
|
|
munchausen syndrom by proxy
|
**factitious disorder imposed on another
intentional production or feigning of physical or psychological symptoms in another person under individual’s care for purpose of indirectly assuming sick role |
|
|
factitious nursing
|
assessment--
chronology of illnesses early childhood experiences family assessment diagnoses-- risk for trauma risk for self-mutilation ineffective individual coping low self-esteem interventions-- -replace dysfunctional, attention-seeking behaviors -accept and value patient -reframe factitious disorder as a cry for help -try to understand patient’s motivations -encourage long-term psychotherapy |
|
|
peds assessment
|
**developmental level frames the assessment and implementation of the management plan
-explain to patient and caretaker the assessment process -questions are more specific, fewer open-ended question -may utilize artistic and play media -interview child and caretaker(s) together and separately evaluation includes-- biopsychosocial history mental status exam additional test, e.g. IQ school records |
|
|
developmental stages
|

|
|
|
mental retardation (MR)
|
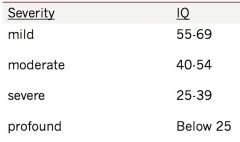
significantly subaverage intellectual functioning: an IQ of approximately 70 or below; affects 2% to 3% of population
**onset must be before age 18 |
|
|
MR etiology
|
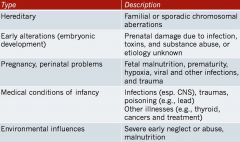
|
|
|
MR diagnoses
|
-risk for injury related to altered physical mobility or aggressive behavior
-self-care deficit related to altered physical mobility or lack of maturity -impaired verbal communication related to developmental alteration -impaired social interaction related to speech deficiencies or difficulty adhering to conventional social behavior -anxiety (moderate to severe) related to hospitalization and absence of familiar surroundings |
|
|
MR treatment
|
**optimal level of functioning, promote independence
-incorporate programs that maximize speech, language, cognitive, psychomotor, social, self-care, and occupational skills -environmental supervision for safety -assess for co-occurring psychiatric disorders -medication used to treat symptoms or comorbidities, e.g. depression -family therapy/support |
|
|
autism spectrum DO / pervasive developmental DO
|
**severe developmental delays in several areas that cannot by attributed to mental retardation
autistic DO asperger’s DO |
|
|
autistic DO
|
**onset is before 3 y/o
-slow or no language development -use of words without attaching meaning to them or communication only by gestures or noises -time spent alone; little interest in making friends -isolation from the world around them; detachment, aloofness -decreased responsiveness to social cues, e.g. smiles, eye contact -sensory impairment, i.e. sensitivity to sight, taste, hearing, touch, or smell -aggressive action, tantrums for no obvious reason -perseveration- showing an obsessive interest in some item or activity and engaging in ritualistic behavior -adherence to routines; inability to tolerate change |
|
|
autistic DO etiology
|
more prevalent in boys
IQ varies widely 1/4 have seizure disorder etiology unknown, areas of research-- genetic brain structure/function abnormalities perinatal factors environmental factors |
|
|
asperger's DO
|
**major difficulties with social interactions and restricted, unusual interests and behaviors; NO clinical delays in speech/cognition
-monotone speech and rigid vocabulary -inability to understand jokes; easily taken advantage of -obsession with facts about circumscribed and odd topics |
|
|
peds red flags >> further eval
|
-avoids/averts gaze
-disinterested in other children/adults -speech/language is either delayed or atypical, e.g. echolalia, scripting -poor and or atypical play skills -labile/moody -repetitive behaviors -delayed and/or atypical motor skills |
|
|
autism diagnostic observation schedule (ADOS)
|
**standardized assessment of-communication, social interaction and play skills and/or use of imaginative materials
-semi-structured presentation -play activities -loosely structured or unstructured -four modules (chosen based on language level), each providing scheduled activities for either children or adults -standard set of social “presses”clinician uses to encourage social responsiveness |
|
|
ADOS scoring guidelines
|
0/ behavior shows no abnormality as specified
1/ behavior is mildly abnormal or slightly unusual 2/ behavior is clearly abnormal or unusual 3/ behavior is markedly abnormal as to interfere with the assessment or very limited 7/ abnormality is not specified in coding 8/ behavior did not occur or is not applicable |
|
|
autistic spectrum treatments
|
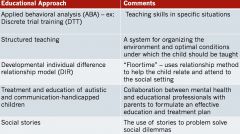
|
|
|
autistic spectrum interventions
|
-physical safety
-management of repetitive behavior -specific behavioral interventions -medication -foster nonverbal social interactions -milieu management -coordination of care -family interventions -teaching self-care skills |
|
|
autistic spectrum drugs
|
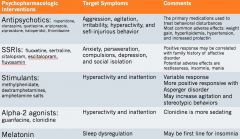
|
|
|
attention deficit / hyperactivity DO (ADHD)
|
inattentive symptoms--
-careless mistakes -attention difficulty -listening problems -loses things -fails to finish what he/she starts organizational skills lacking -reluctant to do tasks that require sustained mental effort -forgetful in routine activities -easily distracted hyperactivity-impulsive symptoms-- -runs/restless -unable to wait for his/her turn -not able to play quietly -fidgets with hands or feet -answers are blurted out -staying seated is difficult -talks excessively -tends to interrupt |
|
|
oppositional defiant DO (ODD)
|
resentful
easily annoyed argues with adults loses temper blames others for misbehavior annoys people deliberately defies rules or requests spiteful |
|
|
conduct disorder (CD)
|
bullying
animal cruelty destroying others’ property fighting out late at night running away from home actively forcing sex being cruel to people using a weapon setting fires not going to school everyday lying or conning stealing while confronting a victim stealing without confronting a victim |

