![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
What are neurodevelopmental disorders?
|
A group of conditions with an onset in the developmental period that produce impairments in personal, social, academic, and occupational functioning.
|
|
|
What are there impairments in for neurodevelopmental disorders?
|
Functioning:
- Personal - Social - Academic - Occupational |
|
|
What are there deficits in for patients with Intellectual Development Disorder (Intellectual Disability)?
|
- Deficits in intellectual functioning such as reasoning, problem solving, planning, abstract thinking, judgment, academic learning, and learning from experience,
- Confirmed by clinical experience and individualized standardized intelligence testing |
|
|
How does an Intellectual Disability affect adaptive functioning?
|
- Failure to meet developmental and socio-cultural standards for personal independence and social responsibility.
- Without ongoing support, the adaptive deficits limit functioning in one or more ADLs, such as communication, social participation, and independent living, across multiple environments such as home, school, work and community |
|
|
When is the onset of Intellectual Disability?
|
Onset of intellectual and adaptive deficits during the developmental period
|
|
|
If you are unable to formally test, what diagnoses can be given for patients thought to have a neurodevelopmental disorder?
|
- Global Developmental Delay (<5 years and unable to test)
- Unspecified Intellectual Disability (>5 years and unable to test d/t associated sensory or physical impairments as in blindness or prelingual deafness, locomotor disability, or presence of severe behavioral disturbance or co-occurring mental disorder) |
|
|
What is Global Developmental Delay?
|
Neurodevelopmental Disorder diagnosis if unable to formally test:
- <5 years and unable to test |
|
|
What is Unspecified Intellectual Disability?
|
Neurodevelopmental Disorder diagnosis if unable to formally test:
- >5 years - Unable to test d/t associated sensory or physical impairments as in blindness or prelingual deafness, locomotor disability, or presence of severe behavioral disturbance or co-occurring mental disorder |
|
|
What are the communication disorder subtypes of neurodevelopmental disorders?
|
- Language disorder
- Speech sound disorder - Childhood onset fluency disorder (stuttering) - Social (pragmatic) communication disorder - Unspecified communication disorder |
|
|
What are the characteristics of a Language Disorder?
|
Persistent difficulties in the acquisition and use of language across ALL modalities (speech, writing, sign language) due to deficits in comprehension or production that include:
• Reduced vocabulary • Limited sentence structure • Impairments in discourse • Language abilities are substantially and quantifiable below expected age level resulting in deficits in functioning • Difficulties not attributable to sensory, motor, medical, neurological, IDD, or global DD. • Onset during the developmental period |
|
|
What are the characteristics of a Speech Sound Disorder?
|
• Persistent difficulty in speech sound production that interferes with speech intelligibility or prevents communication
• Interferes in social, occupational, or academic functioning • Onset during developmental period • Difficulties not attributable to congenital or acquired conditions (cleft palate, cerebral palsy, TBI, medical or neurological conditions) |
|
|
What are the characteristics of Childhood Onset Fluency Disorder (Stuttering)?
|
Disturbances in the normal fluency and time patterning of speech including sound syllable repetitions, sound prolongations, sound pauses within words, word substitutions to avoid problem words, words with tension, monosyllable whole word repetitions ‘I-I-I-I see him’
• Disturbance causes anxiety about speaking or limitations in performance • Onset during developmental period • Not attributable to sensory deficit, neurological, medical condition, or mental disorder |
|
|
What are the characteristics of a Social (Pragmatic) Communication Disorder?
|
• Persistent difficulties in the social use of verbal and nonverbal communication
• Deficits result in functional limitations • Onset during developmental period (maybe late manifestation) • Symptoms not attributable to medical, neurological, poor grammar, and not better explained by ASD, ID/IDD, Global Delay, or another mental disorder |
|
|
What are the characteristics of an Unspecified Communication Disorder?
|
Symptoms characteristic of communication disorder that cause distress or impairment in important areas of functioning but do not meet the criteria for a communication disorder
|
|
|
What are the mandatory criteria for a diagnosis of Autism Spectrum Disorders?
|
1. Persistent deficits in social communication and social interaction across multiple contexts, (need all 3):
a. Deficits in social-emotional reciprocity b. Deficits in nonverbal communicative behaviors used for social interaction c. Deficits in developing, maintaining and understanding relationships |
|
|
What are the supportive criteria for a diagnosis of Autism Spectrum Disorders?
|
2. Restricted, repetitive patterns of behavior, interests, or activities (2 of the 4):
a) Stereotyped or repetitive motor movements (most commonly is hand flapping) b) Insistence on sameness, routines, or ritualized patterns c) Highly restricted, fixated interests d) Hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects |
|
|
What are the additional criteria for a diagnosis of Autism Spectrum Disorders (onset? impact? other?)
|
3. Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learning strategies in later life) - usually by 18-24 months
4. Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning. 5. These disturbances are not better explained by intellectual disability or global developmental delay. |
|
|
What are the levels of severity of Autism Spectrum Disorders?
|
- Level I: requires support
- Level II: requires substantial support - Level III: requires very substantial support |
|
|
What are the characteristics of Level I severity of Autism Spectrum Disorders?
|
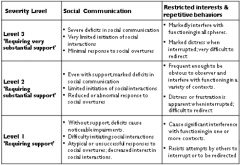
Requires support
|
|
|
What are the characteristics of Level II severity of Autism Spectrum Disorders?
|
Requires substantial support
|
|
|
What are the characteristics of Level III severity of Autism Spectrum Disorders?
|
Requires very substantial support
|
|
|
What kind of disorder is Attention Deficit Hyperactivity Disorder?
|
Neurodevelopmental disorder (no longer classified as a behavioral disorder)
|
|
|
What are the characteristics/criteria of Attention Deficit Hyperactivity Disorder?
|
• Persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development
• Inattention: 6 of 9 criteria for 6 months • Hyperactivity and impulsivity: 6 of 9 criteria for 6 months • Before age 12, several settings, with functional impact • Not from another mental disorder |
|
|
When must Attention Deficit Hyperactivity Disorder be diagnosed by?
|
By age 12
|
|
|
How should you classify a patient's Attention Deficit Hyperactivity Disorder?
|
1. combined
2. predominantly inattentive 3. predominantly hyperactive- impulsive 4. partial remission 5. mild/moderate/severe |
|
|
What is "other specified AD/HD"?
|
Full AD/HD criteria are not met and reason stated
|
|
|
What is "unspecified AD/HD"?
|
Full AD/HD criteria are not met and reason is NOT stated
|
|
|
What are the other diagnostic considerations for neurodevelopmental disorders?
|
• Specific Learning Disorder
• Motor Disorders • Other Neurodevelopmental Disorders • Other specified Neurodevelopmental Disorders • Unspecified Neurodevelopmental Disorders |
|
|
What are the motor disorders?
|
• Developmental Coordination Disorder
• Stereotypic Movement Disorder • Tic Disorder - Other Specified Tic Disorder - Unspecified Tic Disorder |
|
|
What are the criteria for diagnosing Specific Learning Disorder?
|
Difficulty learning and using academic skills (1 of 6 criteria for over 6 months)
1. Inaccurate or slow and effortful word reading 2. Difficulty understanding the meaning of what is read 3. Difficulties with spelling 4. Difficulties in written expression 5. Difficulties in mastering number sense, facts calculation 6. Difficulties in math reasoning • Affected academic skills substantially and measurably below expected norms • Onset during school age years • Not accounted for by ID, sensory impairments, neurological, medical, inadequate educational instruction, psychosocial adversity |
|
|
What do you need to specify about Specific Learning Disorders?
|
• with reading impairment
• with written expression • with math impairments • mild/moderate/severe |
|
|
What are the characteristics of Motor-Developmental Coordination Disorder?
|
- Acquisition and execution of coordinated motor skills is substantially below expected performance-clumsiness, slowness, inaccuracy
- Significant and persistent interference - Impacts activities and productivity - Onset during developmental period - Not better explained by ID, visual impairment, or neurological |
|
|
What are the characteristics of Motor-Stereotypic Movement Disorder?
|
• Repetitive, driven, and purposeless motor behavior (hand shaking, waving, head banging, self biting, self hitting)
• Onset in developmental period • Not attributed to substance, neurological, other mental disorder |
|
|
What do you need to specify about a Motor-Stereotypic Movement Disorder?
|
• With self injurious behavior (SIB)
• Without self injurious behavior • Associated medical, genetic or neurodevelopmental disorder • Mild/moderate/severe |
|
|
What are the characteristics of Tic Disorder - Tourette's Disorder?
|
• BOTH multiple motor and vocal tics present
• Persist for over 1 year – may wax and wane • Onset before age 18 • Not attributed to substance, or medical disorder |
|
|
What are the characteristics of Tic Disorder - Persistent Motor or Vocal Tic Disorder?
|
• Single or multiple motor or vocal tics but NOT BOTH
• Persisted for over 1 year • Onset before age 18 • Not substance related or medical disorder • No prior Tourette’s criteria met |
|
|
What are the characteristics of Tic Disorder - Provisional Tic Disorder?
|
• Single or multiple motor or vocal tics
• Present for less than 1 year • Onset before age 18 • Not related to substance. medical disorder |
|
|
What are the Tic Disorders that don't meet full criteria?
|
Other Specified Tic Disorder
- Impairment without full criteria - Reason given Unspecified Tic Disorder - Impairment without full criteria - No reason given |
|
|
What are the characteristics of Other Specified Neurodevelopmental Disorder?
|
• Symptoms that cause impairment but do not fulfill criteria for specific neurodevelopmental disorder
• Reason given • Ex: neurodevelopmental disorder associated with prenatal alcohol exposure |
|
|
What are the characteristics of Unspecified Neurodevelopmental Disorder?
|
• Symptoms with impairment but do not fulfill criteria for specific disorder
• No reason given • Ex: insufficient information in ER |
|
|
What are the characteristics of Co-Occurring Disorders (neurodevelopmental disorders)?
|
• Increased risk for the presence of other disorders
• Issue of ‘overshadowing’ (the concept of a neurodevelopmental disorder preventing recognition of other disorders) - Ex: person with Intellectual Disability: • 2x medical morbidity • 3x psychiatric disorders • 4x preventable mortality |
|
|
What are the normal fine motor milestones?
|
- 4 months: rattle to mouth
- 6 months: thumb/finger grasp - 12 months: toys in - 18 months: builds/scribble vs stroke - 24 months: grasps small things / draw circle |
|
|
What are the normal gross motor milestones?
|
- 1 month: holds head
- 4 months: sits with support - 6 months: sits and plays - 12 months: walks - 18 months: runs/jumps - 24 months: stairs |
|
|
What are the normal language as communication milestones?
|
- Newborns can recognize voice (but don't understand meaning)
- Verbalizations of a newborn are reflexes of internal state, not intended as communicator - Associate vocalizations with communication and meaning (8-12 months) - Use words to communicate (12-24 months) |
|
|
What are the normal states of expressive language?
|
Stages unfold in order, age range is 6-24 months
- Canonical (ma) - Reduplicated babbling (dada) - First words (relate to person, object, or wants) - Vocabulary develops for period of time - Two wards and grammar - "W" questions and prepositions |
|
|
What are the normal states of receptive language?
|
• Newborn - recognize voice, no meaning
• 1-6 months, turn to voice - attention not comprehension • 6-24 months - stages of comprehension - Single nouns (body parts, general objects) - Rapid increase in vocabulary - One step commands (baby sleep, shoe on) - Two and more step commands |
|
|
What does IQ measure? How does it change?
|
- Measures overall cognition
- Consistent through adulthood |
|
|
What is the major role of PCP during preschool age?
|
Identify potential concern and refer for further evaluation
|
|
|
If you have a concern for a preschool age child's motor and language milestones, what should you consider?
|
• Global developmental delay
• Intellectual disability • Rule out genetic or neurological cause |
|
|
If you have a concern for a preschool age child's language and social milestones, what should you consider?
|
• Communication disorder
• Autism • Rule out genetic or neurological cause |
|
|
How does the age of presentation of an intellectual disability influence the severity of the intellectual disability?
|
• Profound – evident in first 6-12 months
• Severe – evident end of first year • Moderate – evident 1-2 years • Mild – evident by 4-5 years |
|
|
How do we evaluate for Autism?
|
Evaluation by 18-24 months (MCHAT evaluation)
- If they fail that they need to be referred to a specialist - Presents as abnormal social, communication, and play |
|
|
What are the key limitations of Autism Spectrum Disorder in toddlerhood?
|
• Eye contact
• Response to name • Joint Attention • Pointing to express interest • Interest in other children • Gesture • Imitation • Shared enjoyment • Empathic Responding • Displaying range of facial expressions |
|
|
What are some sensitive but not specific symptoms for Autism Spectrum Disorder?
|
• Toe walking / W sitting
• Stereotypies • Sensory sensitivities |
|
|
What are the treatments for Autism Spectrum Disorder?
|
- Best if you get treatment started by 2-2.5 years
- Best if they have still have some language when they start therapy |
|
|
What are the characteristics of a school age child with Autism Spectrum Disorder?
|
As others mature: emotional, behavioral, social, and learning problems “show themselves”
• Articulation errors persist • Cannot learn to read • Cannot retain math facts • Not developing friendships |
|
|
What are the educational issues for a school age child with Autism Spectrum Disorder?
|
• Individual Education Plan versus 504 Plan
• Can the child be educated in regular classroom? • When should the child be excluded from the regular classroom? • Therapy in school versus private therapy |
|
|
What are the characteristics of an Individual Education Plan?
|
Once this is accepted, they are placed in special education program, funding comes from this program
|
|
|
What are the characteristics of a 504 plan?
|
Not as formal or as enforceable, but gets children accommodations with regular education program
|
|
|
How do you treat a school-age child with an Autism Spectrum Disorder?
|
- Therapy and medications
- Access to resources |
|
|
What is the Erikson stage of psychosocial development for adolescence (12-18 years)?
|
Identity vs Role Confusion
- Teens need to develop a sense of self and personal identity. - Success leads to an ability to stay true to yourself - Failure leads to role confusion and a weak sense of self. |
|
|
What are the concerns for an adolescent with Autism Spectrum Disorder?
|
• Increase in mood and anxiety disorders
• Increased awareness in differences from peers • Increase in social complexity • Separation and independence issues • Self management of menstruation |
|
|
What is the Erikson stage of psychosocial development for young adulthood (19-40 years)?
|
Intimacy vs Isolation
- Relationships: young adults need to form intimate, loving relationships with other people. - Success leads to strong relationships, while failure results in loneliness and isolation. |
|
|
What are the transition stage issues for young adults with neurodevelopmental disorders? Resources?
|
• Guardianship: allows parents to talk to medical providers, etc
• Adult community services accessed • Vocational training and employment • School supports until age 21 • Wisconsin Family Care (for adults w/ developmental disabilities) • Social Security Income • Medicaid insurance • Living arrangements |
|
|
What is the Erikson stage of psychosocial development for adulthood (40-65 years)?
|
Generativity vs Stagnation
- Work and parenthood - Adults need to create or nurture things that will outlast them, often by having children or creating a positive change that benefits other people. - Success leads to feelings of usefulness and accomplishment - Failure results in shallow involvement in the world. |
|
|
What are the dimensions of quality of life in adulthood for a patient with a neurodevelopmental disorder?
|
- Satisfaction
- Competence and productivity - Empowerment and independence - Social belonging and community integration - Contribution to the community |
|
|
What are the individual assessment areas for a patient with a neurodevelopmental disorder?
|
• autonomy
• vocational plans • community living opportunities • social networks and supports • intimacy |
|
|
What are the improved quality of life predictors for adults with a neurodevelopmental disorder?
|
• High school graduation
• Paid employment • Parent knowledge of adult services • Parent involvement in transition services • Family coping • Extended family or non-family support |

