![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
What is intimate partner violence?
|
Assaultive behavior that functions to dominate, control, or punish another in an intimate, supposedly peer, relationship
|
|
|
What are the four types of intimate partner violence?
|
- Physical
- Sexual - Property / pet destruction (sends a message that this could be you) - Psychological battering / terrorism |
|
|
How prevalent is physical violence in the a single year?
|
25%
|
|
|
How prevalent is injury from partner violence in a single year?
|
15%
|
|
|
What is the lifetime incidence of physical violence?
|
39%
|
|
|
What is the lifetime incidence of injury from partner violence?
|
25%
|
|
|
What is the relationship between women and the person forcing them to have sex?
|
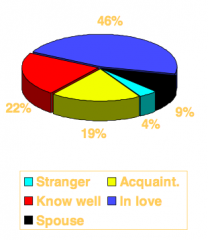
- 46% in love
- 22% know well - 19% acquaintance - 9% spouse - 4% stranger |
|
|
How common is it reported that a woman was forced, by a man, to do something sexual they did not want to do?
|
22%
|
|
|
Your 17 y/o patient tells you she is having unprotected sex. Your task is to:
a) Do a pregnancy test b) Counsel her on contraceptives c) Test her for STIs d) Ask her about IPV e) A, B, and C f) All of the above |
All of the above
- Contraceptive sabotage is sometimes a means of Intimate Partner Violence |
|
|
What is the lifetime incidence of Intimate Partner Violence and Sexual Abuse worldwide?
|
- IPV: 10-50%
- SA: 12-25% |
|
|
How often does interpersonal violence cause death of women age 15-44 years worldwide?
|
Interpersonal violence is the 10th leading cause of death for women 15-44 years old
|
|
|
Men and women are equally victimized by IPV
a) True b) False |
False
- Men in heterosexual relationships are infrequent victims of partner abuse (although hitting may be equal) |
|
|
Men are at most risk for violence perpetrated by whom?
|
- Male friends
- Male acquaintances - Male strangers |
|
|
How does the intentional injury against females and males differ?
|
Violence against women:
- Primarily intimate partner violence - 64% of women who reported rape, physical assault, and/or stalking since age 18 were victimized by a current or former partner Violence against men - Primarily non-intimate partner violence - 84% of men who reported rape and/or physical assault since age 18 were victimized by a non-partner - Only 16% of men who reported rape and/or physical assault by current/former partner |
|
|
What is the risk for men and women in homosexual relationships to experience partner violence?
|
Occurs at a rate comparable to women in heterosexual relationships
|
|
|
Which of the following is NOT a dynamic aspect of IPV
a) relational context b) temporal pattern c) isolation d) anger |
Anger
|
|
|
What are the dynamics of relationships with intimate partner violence?
|
- Temporal pattern (violent episodes do not happen everyday in the vast majority of relationships, instead it occurs on average 6x/year, however psychological battering is more prevalent)
- Injury risk - Fear - Isolation - Dynamics for adolescent girls different than for adult women (adolescent girls hit their boyfriends as much as adolescent boys do) |
|
|
Is there a cycle of violence?
|
- Transgenerational: did the perpetrator grow up in a violent house (seeing it or experiencing it), they are more likely to be an abuser or be a victim (if female)
- Cycle of violence within the relationship (does not happen in most relationships): violent explosion, then regret / apologies / gifts, then another negative cycle begins |
|
|
What are the societal dynamics that contribute to Domestic Abuse?
|
• Institutional/structural sexism (eg, females make less than males so may feel dependent on husband)
• Legislative factors • Law enforcement/criminal justice (required to arrest predominant aggressor) • Social services • Medicine (physicians and other healthcare workers are still not screening enough for partner violence) |
|
|
The most likely cause of face, head, and neck injuries for women is:
a) Car crash b) Athletic injury c) IPV d) Falls |
Intimate Partner Violence
Facial and head injuries more characteristic of blunt intentional trauma (i.e., IPV) than car crashes or falls |
|
|
If a women presents with a facial injury or head injury what are the chances it is due to Intimate Partner Violence?
|
- Facial injury: 5x more likely to be d/t IPV
- Head injury: 1.4x more likely to be d/t IPV |
|
|
What percent of women who are abused struggle with depression? Suicidality?
|
50% MDD
20% suicidality |
|
|
What percent of women who are abused struggle with PTSD?
|
61%
|
|
|
What mental health problems are more common in female victims of IPV?
|
- PTSD (61%)
- Depression (50%) and Suicidality (20%) - Functional disorders - Anxiety - Alcohol abuse |
|
|
Besides mental health problems, what else are female victims of IPV more likely to have?
|
– Significantly more health problems due to any disease
– More induced abortions – More gynecological disease More hospitalizations for • Trauma • Surgical disorder, non trauma • Gynecological disorder • Induced abortion • Medical disorder • Observation of undefined condition |
|
|
What are the key symptoms of a battered women who has PTSD?
|
• Sleeponsetandinterruptioninsomnia
• Headaches • Nightmares • Cryingspells • Worry • Difficulty concentrating and inability to do her job • Intrusivethoughts • Avoidance of certain situations • Decreasedappetite |
|
|
What are the key symptoms of a battered women who has depression?
|
• Sadness
• Guilt feelings • Sleep interruption insomnia • Overeating and weight gain • Low energy and decreased motivation • Feelings of hopelessness – Not suicidal • Low self-esteem • Frequent crying spells |
|
|
What are the key symptoms of a battered women who has functional disorders?
|
• Somatic complaints
• No pathophysiology identified following comprehensive testing and diagnostic studies |
|
|
What are the key symptoms of a battered women who has anxiety?
|
• Uncontrollable worry and apprehension that
“something bad” was going to happen • Increased muscle tension • Fatigue • Restlessness • Increased absenteeism from work |
|
|
What are the key symptoms of a battered women who has alcohol abuse?
|
• Heavy drinking
• No evidence of tolerance or withdrawal • Occasionally alcohol abuse interferes with responsibilities (eg, taking care of children) • Fighting when she has been drinking |
|
|
What is the financial impact of IPV?
|
Costs millions per year
|
|
|
What is the effect on children living in a family with IPV?
|
80-90% of children directly witnessed assault
|
|
|
What are the ACE studies?
|
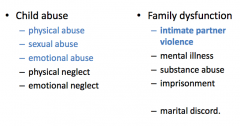
- Ask people about their lifetime experiences with 10 different adverse events
- The more you have experienced, the more likely they are to have certain adult disorders |
|
Exposure to the 10 different adverse events during childhood (ACE study), leads to what lifetime risk?
|
Dose-response relationship between those exposures and adult disorders:
- Smoking - Alcoholism - Drug use / Injected drug use - STIs - # sexual partners - Severe obesity - Depression, anxiety, panic disorder, suicide - Ischemic Heart Disease (IHD) - COPD - Stroke - Idiopathic myocarditis - Myasthenia gravis - Rheumatoid arthritis - Auto-immune hemolytic anemia |
|
|
What are the disguised presentations of IPV?
|
Mental Health:
- Depression, Anxiety - Alcohol/drug abuse Relationship Problem: - Sexual dysfunction - Partner as identified patient Child-related Problem: - Suspected child abuse - Child behavior problem Multiple, stress-related physical complaints |
|
|
How does PTSD mediate between trauma exposure and poor health outcomes?
|

- Elevated symptom reporting
- Medical adherence and coping - Coping strategies for coping with PTSD (risk behaviors, low self-efficacy to change and/or maintain preventive health regimens, increased risk of re-victimization) |
|
|
How does chronic stress / PTSD affect normal physiologic pathways?
|
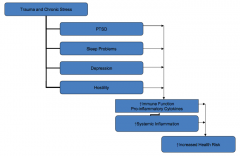
- Disrupts normal neurochemical mechanisms of coping and stress responding
- Affects catecholamine, HPA axis, and immune response - Trauma dysregulates physiologic processes - Increase in pro-inflammatory cytokines (creates wear on system and increases vulnerability to disease) |
|
|
How does chronic stress / PTSD affect sleep?
|
• Negative effects of sleep disruption:
– Immune function – Metabolic changes – Chronic HPA axis activation • Sleep deprived persons have more: – Inflammation – Greater functional disability – Decreased quality of life |
|
|
What are the patient barriers to diagnosing and treating partner violence?
|
• Lack of trust (what will you do with that information)
• Safety jeopardized (ending of a relationship has the greatest risk for homicide, you need to help them get in touch with a shelter) • Financial support jeopardized (might not be able to afford moving out) • Shame & humiliation • Futile resignation |
|
|
What are the barriers health professionals face to diagnosing and treating partner violence?
|
• Lack of knowledge
• Lack of clinical skills & training • Fear of offending the patient (will not offend patient) • Too close for comfort • Pandora’s Box: powerlessness & loss of control |
|
|
What are some questions that can be used to screen for partner violence?
|
Ask very specific, behaviorally-oriented questions:
• In my practice I’m concerned about prevention and safety, especially in the family. • Have you been hit, kicked, punched, or otherwise hurt by someone within the past year? If so, by whom? • Do you feel safe in your current relationship? • Is there a partner from a previous relationship who is making you feel unsafe now? |
|
|
What are the characteristics of effective interview questions?
|
• Ask about specific behaviors
• Avoid general, emotionally charged terms like abuse, violence, and victimization • Ask about various types of violence and responses to it: fear; injury; sexual assault; control • Ask about current problems from previous relationships |
|
|
When can you ask about partner violence?
|
• Annual or general exams
• Initial visit with first- time patients • As part of the initial assessment at a specialist • Well child exams • Adolescent & sports physicals • OB visits • Nursing home visits • Whenever you suspect it |
|
|
What are some tips for screening for partner violence?
|
• Screen in private
• Use professional interpreters or health care worker w/ non-English speakers (not a family member) • Discuss limits on confidentiality • Present screening as routine • Be calm, matter of fact and non-judgmental • Obtain behavioral descriptions of what happened, rather than asking why it happened • Begin with open-ended questions, then be specific: “What happens when you fight?” followed by “Has he ever pushed, kicked, or grabbed you?” • Listen! |
|
|
How do you help a patient that is being abused?
|
"S-O-S Doc" intervention
• Support, belief, confidentiality • Safety: Help assess danger • Options: Safety planning & follow-up • Strengths to build upon • Document |
|
|
What are the characteristics of "supporting" a patient who is being abused?
|
• Talk privately
• Make eye contact Say: • I’m sorry you have been treated this way. • Nobody deserves to be hit or hurt. • You have a right to be safe and respected. • The abuse is not your fault. |
|
|
What are the characteristics of assessing the "safety" a patient who is being abused?
|
• Do you feel safe going home? If tonight, what about tomorrow night? What would you do if you stopped feeling safe?
• Are your children safe? |
|
|
What are the indicators for danger to look for in a patient who is being abused?
|
• Increasing frequency or severity
• Weaponsused • Drug and alcohol abuse • Forced or threatened sexual acts • Life transitions: pregnancy; separation; divorce • History of past violence or suicide attempts • Threats to kill |
|
|
What are the "options" for a patient who is being abused?
|
• Local or regional woman's shelters
• Legal advocacy • Police • 911 • Emergency plan |
|
|
What are the "strengths" to validate in a patient who is being abused?
|
• Identify and validate patient strengths
• You are facing a very tough situation with a great deal of courage. • I can see that you care deeply about your children. • You have shown great strength in very tough circumstances. |
|
|
What do you "document" in the subjective of your note from a patient history of a patient who is being abused?
|
• Describe what the patient said using direct quotes
• Add other historical data • Avoid pejorative language – Use “Patient said ‘My husband hit me in the head with a pan.’” – DO NOT use “Patient claimed..” or “Patient alleged...” |
|
|
What do you "document" in the objective of your note from a patient history of a patient who is being abused?
|
- Behavior
- injuries (location and quality, use drawings/body charts/photos, use ruler for scale in photos, include victim's face for identity) |
|
|
What do you "document" in the assessment of your note from a patient history of a patient who is being abused?
|
– “Injury inconsistent with reported mechanism of injury”
– “Injury and history consistent with intentional injury” – Include name of perpetrator if reported by patient |
|
|
How should you follow up with a patient who is being abused?
|
• Encourage and schedule follow-up
appointments • Connect to community resources • Assess barriers to follow-up – Will you have transportation for the next appointment? – Will your partner try to prevent you from returning? |
|
|
What are the potential pitfalls in the treatment of a patient who is being abused?
|
• Not asking when you have the chance
• Trivializing the violence • Overreacting to the violence • Overreacting to the denial (keep asking even if they have said no before) • Summarily recommending “getting out” |
|
|
What are the potential frustrations of treating a patient being abused?
|
• “Revolving door” syndrome
• Dealing with denial • “Bad” victims – Alcohol and drug abusers – Maltreating parent – “Other side of the tracks” • Magnitude of the problem and sense of helplessness • Excessive outrage |
|
|
What are the ethical issues involved with treating a patient being abused?
|
• Denial of services (I don’t want to talk about the issue)
– Too tired – Too helpless – Not my area – Opening Pandora’s Box • Duty to warn/protect • Confidentiality • Send home without a follow-up plan |

